TL;DR
Thrombocytosis or high platelet count is defined as elevated platelet count above the normal range (typically >450,000/μL).
- Reactive Thrombocytosis ▾: More common, caused by underlying conditions like infection, inflammation, iron deficiency, splenectomy, malignancy, etc. Platelet count usually normalizes with treatment of the cause.
- Essential Thrombocythemia ▾: A myeloproliferative neoplasm with autonomous platelet overproduction due to genetic mutations (JAK2, CALR, MPL).
- Symptoms ▾: Reactive is often asymptomatic. Essential can cause vasomotor symptoms, thrombosis, bleeding, and splenomegaly.
- Diagnosis ▾: CBC, peripheral blood smear, inflammatory markers, iron studies, bone marrow biopsy (for primary), and molecular testing.
- Treatment & Management ▾: Reactive: treat underlying cause. Essential: risk stratification and treatment with aspirin, cytoreductive agents (hydroxyurea, anagrelide, interferon-alpha, ruxolitinib).
- Complications ▾: Thrombosis, hemorrhage, rare transformation to myelofibrosis/leukemia in essential thrombocythemia.
- Prognosis ▾: Reactive is generally good. Essential is chronic but manageable with monitoring.
*Click ▾ for more information
Introduction
Thrombocytosis is defined as an elevated platelet count (high platelet count) in the peripheral blood, typically above the upper limit of the normal reference range.
What are platelets?
Platelets, also known as thrombocytes, are small, anucleated (lacking a nucleus) cell fragments in the blood that originate from large cells in the bone marrow called megakaryocytes. They are disc-shaped in their inactive state and are essential for normal blood clotting.
Why are platelets important?
Platelets play a crucial role in both hemostasis (the physiological process of stopping bleeding) and thrombosis (the pathological formation of blood clots within blood vessels).
Hemostasis (Coagulation)
- Adhesion: When a blood vessel is injured and the underlying collagen is exposed, platelets adhere to this damaged surface via specific receptors (e.g., glycoprotein Ib/IX/V complex binding to von Willebrand factor).
- Activation: Upon adhesion, platelets become activated. This activation triggers a change in their shape (they become more spherical with pseudopods), and they release various substances from their granules, including:
- ADP (adenosine diphosphate) and Thromboxane A2 (TXA2): These are potent platelet activators and attract more platelets to the site of injury (positive feedback).
- Growth factors: Involved in tissue repair.
- Coagulation factors: Contribute to the coagulation cascade.
- Aggregation: Activated platelets express glycoprotein IIb/IIIa receptors on their surface, which bind to fibrinogen (a plasma protein). Fibrinogen acts as a bridge, linking adjacent platelets together to form a platelet plug (primary hemostasis).
- Stabilization of the Clot: Platelets provide a negatively charged phospholipid surface that is essential for the activation of coagulation factors in the coagulation cascade. This leads to the generation of thrombin, which converts fibrinogen into fibrin. Fibrin forms a mesh that reinforces and stabilizes the platelet plug, forming a more definitive blood clot (secondary hemostasis).
Thrombosis (Pathological Clot Formation)
While the mechanisms are similar to hemostasis, in thrombosis, platelets are inappropriately activated and aggregate within intact blood vessels. This can be triggered by:
- Endothelial damage: Damage to the inner lining of blood vessels (e.g., due to atherosclerosis, inflammation) can expose collagen and activate platelets.
- Abnormal blood flow: Stasis or turbulent blood flow can promote platelet activation and adhesion.
- Hypercoagulable states: Certain conditions can increase the propensity for platelet activation and coagulation.
The resulting thrombus (blood clot) can obstruct blood flow, leading to serious consequences such as myocardial infarction (heart attack), stroke, or deep vein thrombosis.
In essence, platelets are vital for maintaining vascular integrity and responding to injury by forming a hemostatic plug. However, their uncontrolled activation and aggregation contribute significantly to the development of pathological thrombi.
Platelet Count
The normal reference range for platelet count in adults is generally accepted to be between 150,000 and 450,000 platelets per microliter (μL) of blood, or 150 to 450 x 109/L.
A platelet count above 450,000 platelets per microliter (μL) of blood (or 450 x 109/L) is generally considered as thrombocytosis or high platelet count.
Causes of Thrombocytosis (High Platelet Count)
Thrombocytosis (high platelet count) is broadly categorized into two main types based on its underlying cause.
Reactive (Secondary) Thrombocytosis
This is the more common type of thrombocytosis (high platelet count). It occurs when the elevated platelet count is a reaction to another underlying medical condition. The bone marrow is stimulated to produce more platelets due to various factors.
Causes of Reactive Thrombocytosis
- Infections: Acute and chronic infections caused by bacteria, viruses, or fungi. This is a particularly common cause in children.
- Inflammation: Chronic inflammatory diseases such as rheumatoid arthritis, inflammatory bowel disease (Crohn’s disease, ulcerative colitis), Kawasaki disease, sarcoidosis, and other connective tissue disorders. Acute inflammation due to surgery, trauma, or burns can also lead to a temporary increase in platelets.
- Iron Deficiency Anemia: The link is not fully understood but may involve increased erythropoietin levels stimulating megakaryocytes (platelet precursors).
- Splenectomy or Hyposplenism: The spleen normally removes old and damaged platelets. Its absence or reduced function leads to a higher circulating platelet count.
- Malignancy: Various cancers, including solid tumors (lung, gastrointestinal, breast, ovarian), lymphomas, and other hematologic malignancies, can be associated with high platelet count. Sometimes, it can be the first sign of cancer.
- Hemorrhage and Blood Loss: Following significant blood loss, the body may temporarily increase platelet production to aid in hemostasis.
- Hemolytic Anemia: Increased destruction of red blood cells can sometimes lead to reactive thrombocytosis.
- Rebound Thrombocytosis: This can occur after recovery from thrombocytopenia (low platelet count) caused by conditions like severe infections or chemotherapy.
- Medications: Certain drugs, such as epinephrine, corticosteroids, and some growth factors, can cause an increase in platelet count.
- Other Stressful Conditions: Severe trauma, burns, and major surgery can trigger a transient increase in platelets.
Essential (Primary) Thrombocythemia (ET)
This is a myeloproliferative neoplasm (MPN), a type of blood cancer. It is characterized by the autonomous (unregulated) overproduction of platelets by abnormal megakaryocytes in the bone marrow. This means the high platelet count is not simply a reaction to another condition but arises from a problem within the bone marrow itself.
Causes of Essential Thrombocythemia
The exact cause is often unclear, but it is associated with acquired genetic mutations in hematopoietic stem cells.
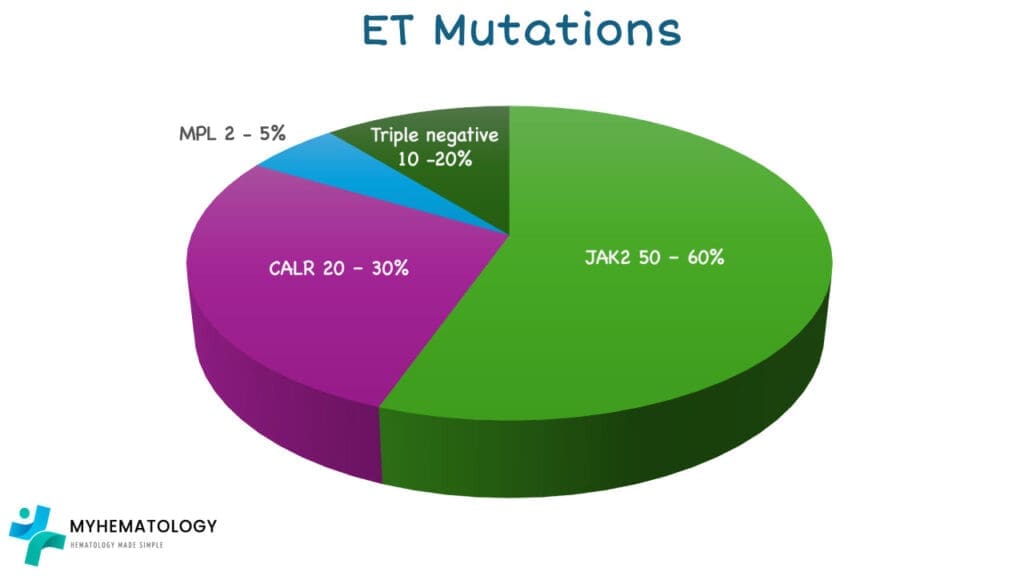
- JAK2 (Janus Kinase 2) gene: This mutation is found in approximately 50-60% of ET patients. It leads to increased signaling in pathways involved in blood cell production.
- CALR (Calreticulin) gene: Mutations in this gene are found in about 20-30% of ET patients, often mutually exclusive with JAK2 mutations.
- MPL (Myeloproliferative Leukemia Virus Oncogene) gene: Mutations in this gene, which encodes the thrombopoietin receptor, are found in a smaller percentage (around 2-5%) of ET patients.
- Triple-Negative ET: Some patients with ET do not have mutations in JAK2, CALR, or MPL. The underlying genetic drivers in these cases are less well understood.
In essential thrombocythemia, the platelets produced may not always function normally, which can paradoxically lead to both thrombotic (clotting) and hemorrhagic (bleeding) complications.
Understanding the distinction between reactive and essential thrombocytosis is crucial for diagnosis and management, as the underlying causes and treatment approaches differ significantly. Reactive thrombocytosis often resolves once the underlying condition is treated, while essential thrombocytosis is a chronic condition requiring ongoing management.
Signs and Symptoms of Thrombocytosis
The signs and symptoms of high platelet count can vary significantly depending on the underlying cause (whether it’s a primary bone marrow disorder like essential thrombocythemia or secondary to another condition) and the degree of platelet elevation.
Primary Thrombocytosis (e.g., Essential Thrombocythemia)
Many individuals may be asymptomatic, especially initially. When symptoms occur, they can include:
- Vascular (related to blood clots or impaired blood flow)
- Headache
- Dizziness
- Changes in vision
- Chest pain
- Shortness of breath
- Weakness
- Numbness or tingling in hands and feet
- Burning, throbbing pain, redness, and warmth in hands or feet (erythromelalgia)
- Transient ischemic attacks (TIAs) or stroke
- Heart attack (less common)
- Blood clots in unusual locations (e.g., hepatic or mesenteric veins)
- Hemorrhagic (related to bleeding, especially with very high platelet counts)
- Easy bruising
- Nosebleeds
- Bleeding gums
- Heavy menstrual periods
- Gastrointestinal bleeding (less common)
- Others
- Fatigue
- Enlarged spleen (splenomegaly), causing discomfort or fullness in the upper left abdomen
Secondary (Reactive) Thrombocytosis
Often, individuals with secondary thrombocytosis are asymptomatic, and the high platelet count is discovered during tests for the underlying condition. If symptoms occur, they are often related to the condition causing the thrombocytosis (high platelet count).
In some cases of very high platelet counts due to secondary causes, there can be a slightly increased risk of clotting or bleeding, but this is less common than in primary thrombocytosis. Potential symptoms, when present, can include:
- Symptoms related to the underlying condition (e.g., fever and signs of infection, joint pain in inflammatory conditions, unexplained weight loss in cancer).
- Less commonly, symptoms similar to those seen in primary thrombocytosis, such as:
- Headache
- Dizziness
- Weakness
- Easy bruising
- Nosebleeds
- In rare cases of extreme thrombocytosis, there might be a slightly increased risk of thrombotic events.
It can be challenging to distinguish between primary and secondary thrombocytosis based on symptoms alone. Further laboratory tests and clinical evaluation are crucial to determine the underlying cause of the high platelet count.
Laboratory Investigations for Thrombocytosis
The laboratory investigation of thrombocytosis is crucial for confirming the diagnosis and, most importantly, distinguishing between primary (clonal) and secondary (reactive) causes. This distinction guides prognosis and treatment.
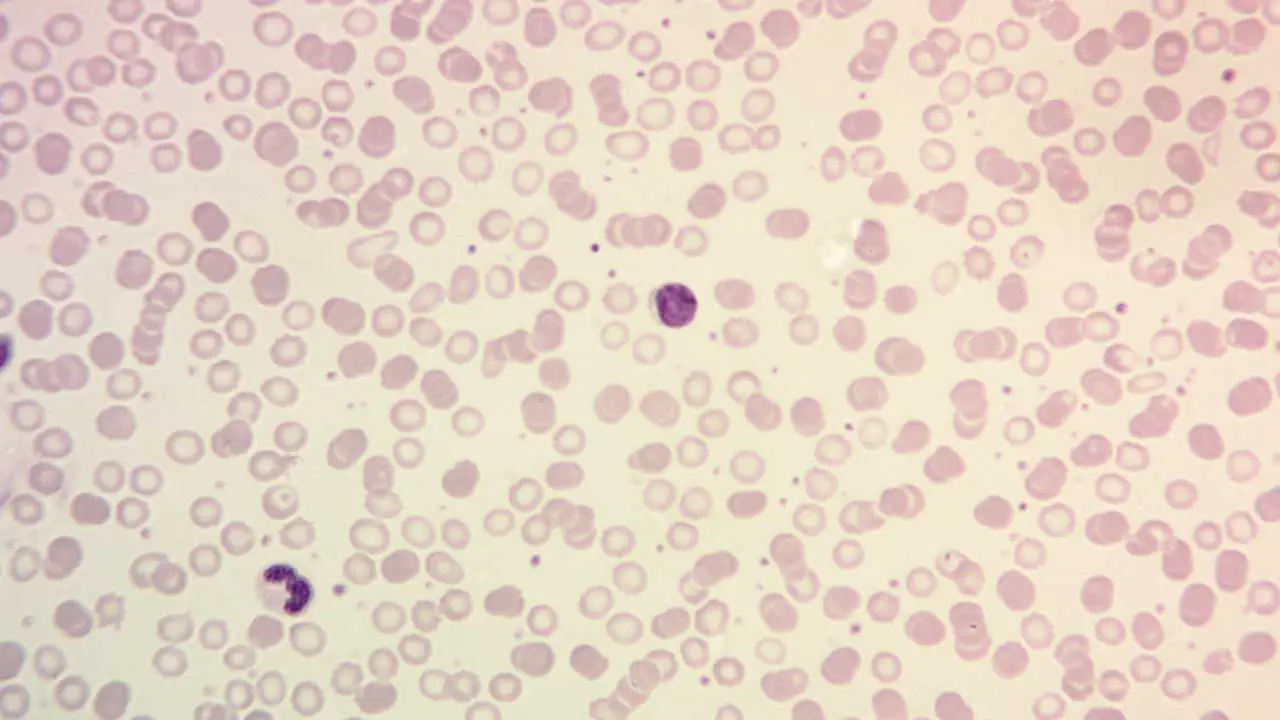
Complete Blood Count (CBC) and Peripheral Blood Smear
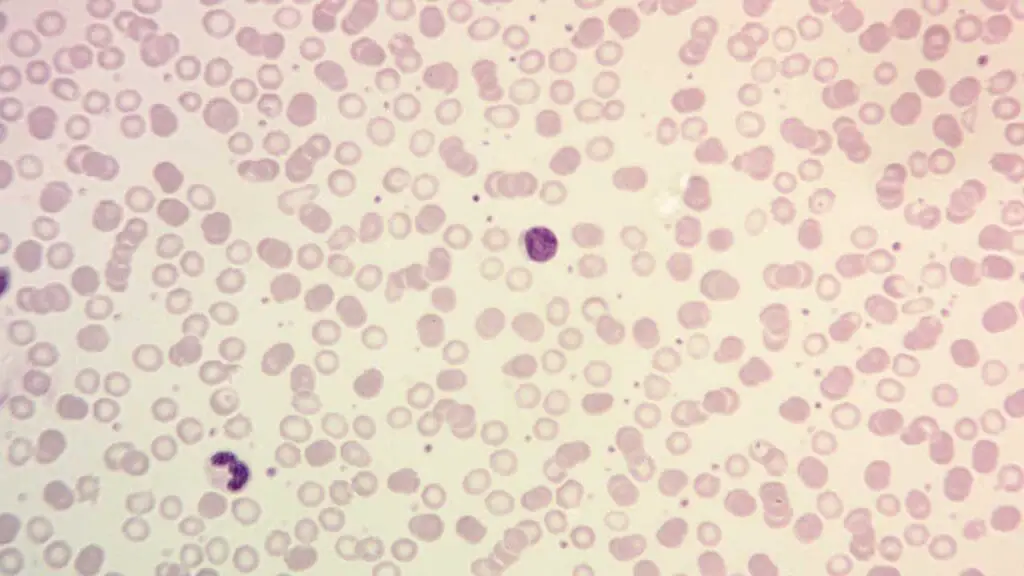
- Platelet Count: A sustained elevation above 450 x 109/L is the hallmark. In primary thrombocytosis, it can be significantly higher (>1000 x 109/L). Secondary thrombocytosis usually shows a less extreme elevation, often below 1000 x 109/L, and may be transient.
- Red Blood Cell (RBC) Indices: Mean corpuscular volume (MCV) and other RBC parameters are important. Iron deficiency (a common cause of reactive thrombocytosis) is often associated with a low MCV. Elevated hemoglobin/hematocrit may suggest Polycythemia Vera (PV), another myeloid neoplasm.
- White Blood Cell (WBC) Count: Usually normal or mildly elevated in primary thrombocytosis. In secondary thrombocytosis, it can be normal, elevated (due to infection or inflammation), or decreased (in some infections). Markedly elevated WBC with immature forms suggests Chronic Myeloid Leukemia (CML).
- Peripheral Blood Smear: Examination of the blood film can reveal large or abnormally shaped platelets in primary thrombocytosis. It can also show signs of underlying conditions causing secondary thrombocytosis (e.g., fragmented RBCs in hemolysis) or suggest other diagnoses (e.g., blast cells in leukemia, teardrop cells in myelofibrosis).
Exclusion of Secondary Causes
- Iron Studies: Serum ferritin, iron, and total iron-binding capacity (TIBC) are essential to rule out iron deficiency anemia, a common cause of reactive thrombocytosis (high platelet count). Low ferritin with high TIBC is indicative of iron deficiency.
- Inflammatory Markers: Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are often elevated in inflammatory conditions causing secondary thrombocytosis (high platelet count).
- Renal and Liver Function Tests: Abnormalities may point to underlying conditions causing reactive thrombocytosis (high platelet count).
- Testing for Underlying Conditions: Depending on the clinical suspicion, further tests for infection, autoimmune diseases, and malignancy may be necessary.
Genetic Studies (for suspected primary thrombocytosis)
- JAK2 V617F Mutation Analysis: This is the most common mutation in primary MPNs and is found in about 50-60% of Essential Thrombocythemia (ET) cases.
- CALR Mutation Analysis: If JAK2 is negative, testing for CALR mutations (present in 20-30% of ET).
- MPL Mutation Analysis: If both JAK2 and CALR are negative, testing for MPL mutations (present in 2-5% of ET).
- BCR-ABL1 Detection: To rule out CML, especially if the WBC count is elevated.
Bone Marrow Aspiration and Biopsy (for suspected primary thrombocytosis or diagnostic uncertainty)
- Cellularity: Helps assess if the thrombocytosis. (high platelet count) is due to autonomous proliferation in the bone marrow.
- Megakaryocyte Morphology: In Essential Thrombocythemia (ET), the bone marrow typically shows increased numbers of large, mature megakaryocytes with hyperlobulated nuclei.
- Assessment for Fibrosis: Increased reticulin or collagen fibrosis suggests Primary Myelofibrosis (PMF) rather than ET.
- Detection of Dysplasia: Can point towards Myelodysplastic Syndromes (MDS) with high platelet count.
- Iron Stores: Can be assessed directly in the bone marrow.
Other Specialized Tests (less commonly used)
- Red Blood Cell Mass Study: To definitively exclude polycythemia vera in cases where the hemoglobin/hematocrit is borderline.
- Platelet Function Tests (e.g., Platelet Aggregation Studies, PFA-100): May be considered in cases of unexplained bleeding despite high platelet counts, but are not typically used for routine diagnosis of thrombocytosis .
- Serum Erythropoietin (EPO) Level: Usually normal or low in primary thrombocytosis and high in thrombocytosis (high platelet count) secondary to hypoxia or anemia.
The interpretation of these laboratory investigations requires careful consideration of the clinical context to accurately diagnose the cause of thrombocytosis (high platelet count) and guide appropriate management.
Treatment and Management
The treatment and management of high platelet count depend heavily on the underlying cause (primary vs. secondary) and the patient’s risk of developing complications, primarily thrombosis (blood clots) and, less commonly, bleeding.
Treatment of Secondary (Reactive) Thrombocytosis
- Identify and Treat the Underlying Cause: The primary focus is on addressing the condition that is driving the increased platelet count.
- Treating infections with antibiotics or antivirals.
- Managing inflammatory conditions with anti-inflammatory medications.
- Correcting iron deficiency anemia with iron supplementation.
- Treating underlying malignancies.
- Discontinuing causative medications.
- Allowing recovery after surgery or trauma.
- Low-Dose Aspirin: May be considered in patients with very high platelet counts (>1,000,000/µL) and additional cardiovascular risk factors, but the evidence for routine use in secondary thrombocytosis is limited.
- Cytoreductive Therapy (Platelet-Lowering Medications): Generally not indicated for secondary thrombocytosis unless the platelet count is extremely high and causing symptomatic thrombotic or hemorrhagic complications, which is rare. The platelet count usually normalizes once the underlying condition is resolved.
- Monitoring: Regular monitoring of the platelet count and the underlying condition is important.
Treatment of Primary (Clonal) Thrombocytosis (e.g., Essential Thrombocythemia)
Management is based on risk stratification for thrombotic events, as outlined previously for ET.
- Low-Risk Patients
- Low-Dose Aspirin (75-100 mg daily): Usually recommended.
- Observation: May be considered in very low-risk individuals with close monitoring.
- Intermediate-Risk Patients
- Low-Dose Aspirin: Usually recommended.
- Cytoreductive Therapy (e.g., Hydroxyurea or Anagrelide): Often considered if platelet count is persistently high (>1000 x 109/L) or if other vascular risk factors are present.
- High-Risk Patients
- Low-Dose Aspirin: Generally recommended (unless contraindicated).
- Cytoreductive Therapy (e.g., Hydroxyurea, Anagrelide, or Interferon-alpha): Usually indicated to lower the platelet count.
General Considerations for Primary Thrombocytosis
- Platelet Count Target: The target platelet count for cytoreductive therapy is generally <400 x 109/L, but this can be individualized.
- Symptom Management: Address any symptoms like erythromelalgia, headaches, or fatigue.
- Cardiovascular Risk Factor Management: Control hypertension, diabetes, hyperlipidemia, and advise smoking cessation.
- Pregnancy: Requires specialized management with low-dose aspirin and potentially interferon-alpha.
- Surgery: Risk of thrombosis and bleeding needs to be assessed, and platelet-lowering therapy may be adjusted.
- Monitoring: Regular monitoring of blood counts and for signs of complications or disease progression is essential.
Potential Complications
The potential complications of high platelet count primarily revolve around an increased risk of thrombosis (blood clots) and, paradoxically, bleeding (hemorrhage), especially in cases of very high platelet counts or dysfunctional platelets. The likelihood and severity of these complications depend on whether the high platelet count is primary or secondary, the degree of platelet elevation, the presence of other risk factors, and the underlying cause.
Thrombotic Complications
The high platelet count can make the blood “stickier,” increasing the propensity for clot formation in arteries and veins throughout the body. The consequences of these clots vary depending on where they occur:
- Arterial Thrombosis: Can lead to serious events like stroke, transient ischemic attacks (TIAs), myocardial infarction (heart attack), and peripheral arterial thrombosis (potentially causing limb ischemia).
- Venous Thrombosis: Can result in deep vein thrombosis (DVT), pulmonary embolism (PE) (a life-threatening condition), and clots in less common sites like the splenic vein, hepatic vein (Budd-Chiari syndrome), or mesenteric veins.
- Microvascular Thrombosis: Can cause symptoms like erythromelalgia (burning pain, redness, and warmth in extremities), headaches, dizziness, and visual disturbances.
Hemorrhagic Complications (Paradoxical Bleeding)
In some cases, particularly with very high platelet counts (often >1,000,000/µL) or in primary thrombocytosis where the platelets may be inherently abnormal, the platelets can be dysfunctional and unable to effectively contribute to blood clotting. This can lead to an increased risk of bleeding, manifesting as:
- Easy bruising
- Nosebleeds (epistaxis)
- Bleeding gums
- Heavy menstrual periods (menorrhagia)
- Gastrointestinal bleeding
- Rarely, more serious bleeding events like intracranial hemorrhage.
Complications Specific to Primary Thrombocytosis (e.g., Essential Thrombocythemia)
- Transformation to Other Myeloproliferative Neoplasms (MPNs): Over time, essential thrombocythemia can, in a small percentage of cases, evolve into other MPNs like Polycythemia Vera (PV) or Primary Myelofibrosis (PMF).
- Transformation to Acute Leukemia: A rare but serious complication where ET transforms into acute myeloid leukemia (AML).
Pregnancy Complications
Women with high platelet count, especially primary thrombocytosis, have an increased risk of complications during pregnancy, including miscarriage, preeclampsia, placental insufficiency, and thrombotic events.
Factors Influencing the Risk of Complications
- Underlying Cause: Primary thrombocytosis generally carries a higher risk of thrombotic and hemorrhagic complications compared to secondary thrombocytosis, especially at very high platelet counts.
- Degree of Platelet Elevation: Very high platelet counts (significantly above 1,000,000/µL) can increase the risk of both thrombosis and bleeding.
- Age: Older individuals tend to have a higher baseline risk of vascular events.
- Prior History of Thrombosis or Bleeding: Patients with a previous history of these events are at higher risk of recurrence.
- Presence of Other Risk Factors: Cardiovascular risk factors (hypertension, diabetes, smoking, hyperlipidemia) increase the risk of thrombotic complications.
- Underlying Medical Conditions: The condition causing secondary thrombocytosis can also have its own set of complications.
- Genetic Mutations (in primary thrombocytosis): Certain mutations, like JAK2 V617F, have been associated with a potentially higher thrombotic risk in some studies.
Prognosis
The prognosis of high platelet count is highly dependent on whether it is primary or secondary.
Secondary (Reactive) Thrombocytosis: The prognosis is generally good, as the high platelet count is usually transient and resolves once the underlying condition (e.g., infection, inflammation, iron deficiency) is successfully treated. In most cases, it does not lead to significant long-term complications related to blood clots or bleeding. The prognosis is primarily determined by the underlying cause.
Primary Thrombocytosis (e.g., Essential Thrombocythemia): The prognosis is more variable. While ET is a chronic condition with no current cure, many patients can live for a long time, often with a near-normal life expectancy, especially with appropriate management.
The main risks are thrombotic and hemorrhagic complications, which can be serious or even life-threatening.
Factors influencing prognosis in ET include age, prior history of thrombosis, presence of cardiovascular risk factors, and specific genetic mutations.
With careful monitoring and treatment (including low-dose aspirin and cytoreductive therapy in higher-risk individuals), the risk of these complications can be significantly reduced, leading to a favorable long-term outlook for many patients. However, there is a small risk of transformation to myelofibrosis or acute leukemia over time, which can impact the prognosis negatively.
Frequently Asked Questions (FAQs)
What are the red flags of thrombocytosis?
Recognizing the “red flags” of high platelet count is crucial for prompting further investigation and appropriate management. These red flags often suggest a higher likelihood of primary thrombocytosis or an underlying condition with significant potential for complications.
Clinical Red Flags (Symptoms and Patient History)
- Thrombotic Events: A history of unexplained blood clots, especially in unusual locations (e.g., mesenteric vein thrombosis, hepatic vein thrombosis, cerebral venous sinus thrombosis) or at a young age. Arterial events like stroke or transient ischemic attacks (TIAs) and myocardial infarction are also concerning.
- Bleeding Episodes: Paradoxical bleeding (e.g., nosebleeds, easy bruising, gastrointestinal bleeding) despite a high platelet count. This can occur due to acquired von Willebrand factor deficiency at very high platelet count or dysfunctional platelets.
- Vasomotor Symptoms: Recurrent or persistent symptoms like headaches, dizziness, lightheadedness, visual disturbances (e.g., transient blurring or flashing lights), and paresthesias (tingling, numbness, burning sensations, especially in the hands and feet). Erythromelalgia (painful redness and warmth of the extremities) is also a significant red flag.
- Splenomegaly: Palpable enlargement of the spleen on physical examination.
- Unexplained Systemic Symptoms: Fatigue, night sweats, unintentional weight loss, and low-grade fever without an obvious infectious cause can sometimes be associated with myeloproliferative neoplasms.
- Family History: A family history of myeloproliferative neoplasms or unusual blood clotting disorders might raise suspicion.
- Lack of Obvious Reactive Cause: Thrombocytosis (high platelet count) without a clear underlying inflammatory condition, infection, iron deficiency, recent surgery, or other typical triggers for reactive thrombocytosis should prompt consideration of a primary cause.
- Progressive or Markedly Elevated Platelet Count: A persistently high platelet count over time or an initial platelet count that is very high (e.g., >1,000,000/μL) is more suggestive of a primary disorder.
Which cancers cause high platelets?
Thrombocytosis (high platelet count) can be associated with various cancers through a phenomenon known as paraneoplastic thrombocytosis. This occurs when cancer cells release substances that stimulate the bone marrow to produce more platelets.
Cancers more commonly associated with high platelet counts include
- Solid Tumors
- Lung Cancer
- Colorectal Cancer
- Ovarian Cancer
- Gastric Cancer
- Esophageal Cancer
- Kidney Cancer (Renal Cell Carcinoma)
- Breast Cancer
- Endometrial Cancer
- Other solid tumors can also be associated.
- Hematological Malignancies (Blood Cancers)
Can stress cause high platelets?
Yes, stress can indeed cause high platelet count, a condition known as reactive thrombocytosis or secondary thrombocytosis.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Vannucchi AM & Barbui T. Thrombocytosis and thrombosis. Hematology Am Soc Hematol Educ Program (2007) 2007 (1): 363–370.
- Clarke C, Hamilton W, Price S, Bailey SE. Association of non-malignant diseases with thrombocytosis: a prospective cohort study in general practice. Br J Gen Pract. 2020 Nov 26;70(701):e852-e857. doi: 10.3399/bjgp20X713501. PMID: 33199294; PMCID: PMC7679146.
- Almanaseer A, Chin-Yee B, Ho J, Lazo-Langner A, Schenkel L, Bhai P, Sadikovic B, Chin-Yee IH, Hsia CC. An Approach to the Investigation of Thrombocytosis: Differentiating between Essential Thrombocythemia and Secondary Thrombocytosis. Adv Hematol. 2024 Feb 12;2024:3056216. doi: 10.1155/2024/3056216. PMID: 38375212; PMCID: PMC10876298.
- Skoda RC. Hematology Am Soc Hematol Educ Program (2009) 2009 (1): 159–167.
- Bleeker JS, Hogan WJ. Thrombocytosis: diagnostic evaluation, thrombotic risk stratification, and risk-based management strategies. Thrombosis. 2011;2011:536062. doi: 10.1155/2011/536062. Epub 2011 Jun 8. PMID: 22084665; PMCID: PMC3200282.