Introduction
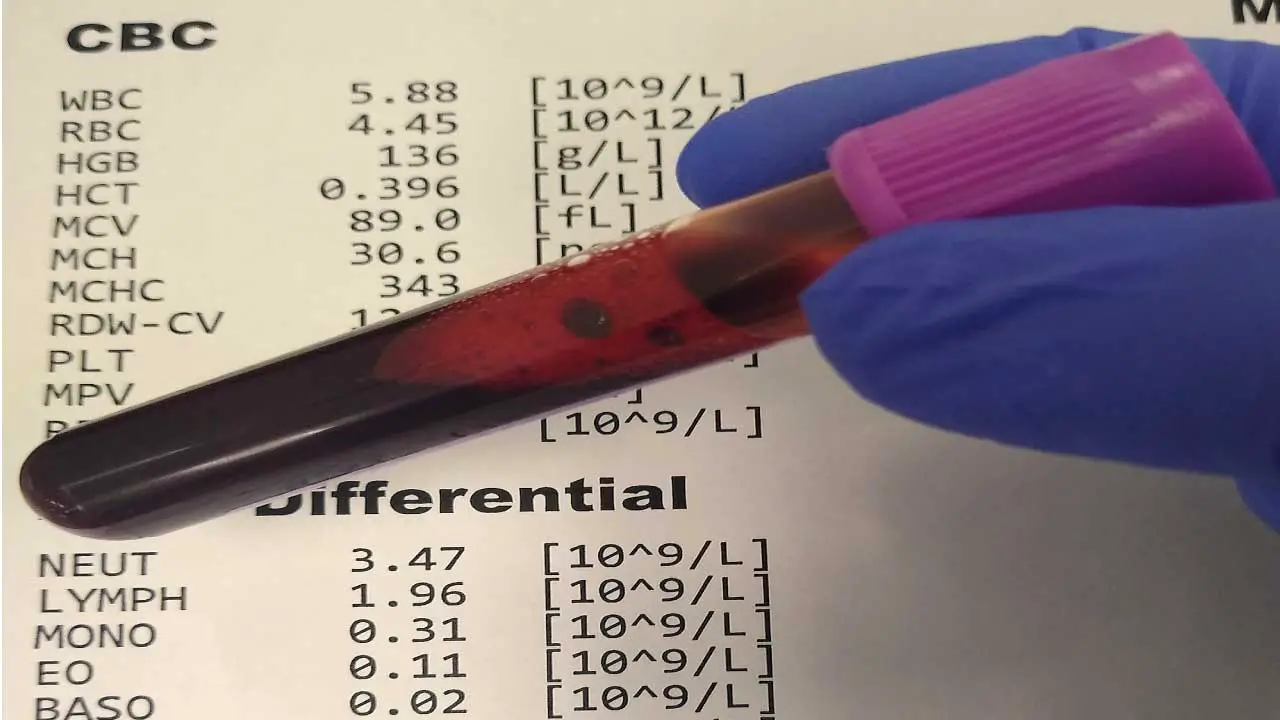
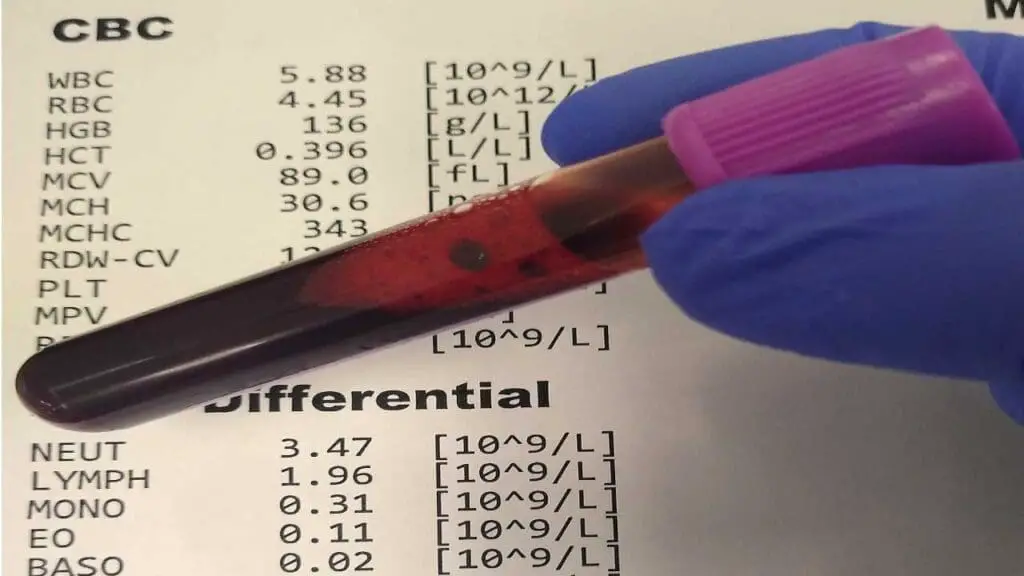
Complete blood count (CBC) with differential or complete blood picture is a routine blood test that provides a comprehensive picture of the body’s blood cells. It measures the number, size, and maturity of various types of blood cells, including:
- Red Blood Cells (RBCs): These cells carry oxygen throughout the body. The CBC with differential measures the number of RBCs, the amount of hemoglobin they contain (protein that binds oxygen), and the percentage of blood volume occupied by RBCs (hematocrit).
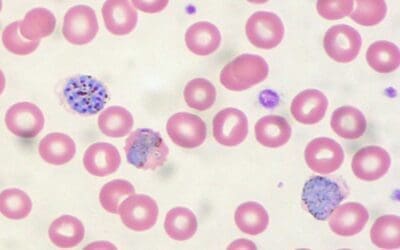
- White Blood Cells (WBCs): These cells are part of the immune system and fight infection. However, a differential count, often included in a CBC with differential, takes things a step further. It provides a breakdown of the five main types of white blood cells:
- Neutrophils – Fight bacterial infections.
- Lymphocytes – Part of the immune system, fighting viruses and other pathogens.
- Monocytes – Play a role in chronic infections and immune response.
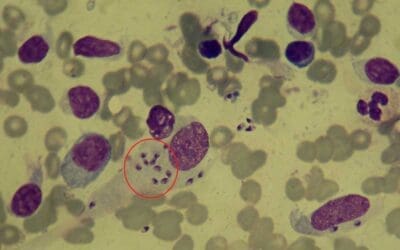
- Eosinophils – Involved in allergic reactions and parasitic infections.
- Basophils – Involved in allergic reactions and inflammation.
- Platelets: These are cell fragments involved in blood clotting.
Importance of CBC with differential
- Overall Health Assessment: A CBC with differential or complete blood picture acts as a baseline for your blood cell health. It can identify potential issues like anemia, infection, inflammation, or blood clotting disorders.
- Diagnosis and Monitoring: Abnormal values in a CBC with differential can point towards various conditions. It can also be used to monitor the effectiveness of treatment for existing blood disorders.
- Early Detection: Changes in blood cell counts can be early indicators of health problems, allowing for timely diagnosis and intervention.
Reference ranges are important because they provide a baseline for interpreting laboratory test results. By comparing a patient’s test results to the reference range, healthcare providers can identify any values that fall outside of the normal range. This can help them to diagnose diseases, monitor the effectiveness of treatment, and identify potential complications.
Reference ranges are established by testing a large group of healthy people and determining the range of values that includes 95% of the results. This means that 2.5% of healthy people will have test results that fall outside of the reference range. This does not necessarily mean that they are sick, but it may indicate a need for further testing or evaluation.
Reference ranges can vary depending on a number of factors, including age, sex, race, ethnicity, and pregnancy status. This is why it is important to use a reference range that is appropriate for the patient’s population group.
Here are some specific examples of how reference ranges are used in hematology:
- A complete blood count (CBC) with differential or complete blood picture is a common hematology test that measures the levels of different types of blood cells in the blood. The reference ranges for CBC with differential vary depending on the patient’s age and sex. For example, the reference range for the white blood cell count is higher in children than in adults.
- A prothrombin time (PT) test is used to measure how long it takes for the blood to clot. The reference range for the PT test is different for people who are taking blood thinners and for those who are not.
- A platelet count is used to measure the number of platelets in the blood. Platelets are involved in blood clotting. A low platelet count can increase the risk of bleeding. The reference range for the platelet count is the same for both men and women.
Reference ranges are an important tool for healthcare providers in the diagnosis and management of hematologic diseases.
Complete blood count (CBC) with differential for adults
Red blood cells (RBCs) are the workhorses of the oxygen transport system in your body. They carry hemoglobin, a protein that binds oxygen in the lungs and delivers it to tissues throughout the body. The complete blood picture or the CBC with differential evaluates various aspects of RBCs to identify potential issues like anemia or abnormal RBC production.
- RBC Count: This measures the number of RBCs per microliter of blood in a CBC with differential. A low count can indicate anemia, while a high count may suggest dehydration or certain blood cancers.
- Hemoglobin: This measures the total amount of hemoglobin in the blood, typically expressed in grams per deciliter (g/dL) in a CBC with differential. Low hemoglobin is a hallmark of anemia, potentially caused by iron deficiency, blood loss, or vitamin deficiencies. High hemoglobin can be linked to dehydration or certain blood disorders.
- Hematocrit: This represents the percentage of the blood volume occupied by RBCs. A low hematocrit reflects anemia, while a high hematocrit can suggest dehydration or specific blood conditions.
- Mean Corpuscular Volume (MCV): This reflects the average size of RBCs.
- Microcytosis (MCV < 80 fL): Suggests small RBCs, potentially indicating iron deficiency anemia.
- Macrocytosis (MCV > 96 fL): Indicates larger RBCs, seen in vitamin B12 or folate deficiency anemia.
- Normocytic (MCV within normal range): RBC size is normal.
- Mean Corpuscular Hemoglobin (MCH): This measures the average amount of hemoglobin present in each RBC.
- Hypochromia (MCH < 27 pg): Indicates low hemoglobin content per RBC, often seen in iron deficiency anemia.
- Normochromia (MCH within normal range): Hemoglobin content per RBC is normal.
- Mean Corpuscular Hemoglobin Concentration (MCHC): This reflects the concentration of hemoglobin within an RBC.
- Hypochromia (MCHC < 32 g/dL): Indicates low hemoglobin concentration, often seen in iron deficiency anemia.
- Normochromia (MCHC within normal range): Hemoglobin concentration is normal.
- Red Cell Distribution Width (RDW): This measures the variation in the size of your RBCs. Increased RDW indicates greater variation in RBC size, potentially suggesting a nutritional deficiency or other blood disorders.
- Reticulocyte Count: This measures the percentage of immature RBCs (reticulocytes) in your bloodstream.
- Increased reticulocyte count: May indicate the body is attempting to increase RBC production in response to anemia.
- Decreased reticulocyte count: May suggest bone marrow suppression, hindering RBC production.
- Total WBC Count: This measures the total number of WBCs per microliter (mcL) of blood.
- Elevated WBC count (Leukocytosis): Can indicate infection, inflammation, or certain blood cancers.
- Decreased WBC count (Leukopenia): May suggest bone marrow problems, autoimmune disorders, or viral infections.
- Neutrophils (Reference Range: 40-70%): These are the most abundant WBCs, acting as the body’s first responders against bacterial infections. They engulf and destroy invading bacteria.
- Lymphocytes (Reference Range: 20-40%): These come in two main types:
- T lymphocytes (T cells): Orchestrate the immune response by coordinating the attack on infected cells and directing other immune cells.
- B lymphocytes (B cells): Produce antibodies, specialized proteins that target and neutralize specific pathogens.
- Increased lymphocytes can suggest a viral infection or immune system activation.
- Monocytes (Reference Range: 2-10%): These are large phagocytic cells that engulf debris from dead cells, bacteria, and other foreign materials. They also play a role in chronic infections and inflammation.
- Eosinophils (Reference Range: 1-4%): These are involved in allergic reactions and parasitic infections. They release chemicals to combat these conditions. Increased eosinophils can indicate allergies or parasitic infections.
- Basophils (Reference Range: 0-1%): These are the least common WBC type and are involved in allergic reactions and inflammatory disorders. They release histamine, a chemical that triggers allergic reactions. Increased basophils can be linked to certain allergic conditions or mast cell disorders.
- Platelet Count (Reference Range): This measures the number of platelets per microliter (mcL) of blood in the CBC with differential.
- Thrombocytosis (Platelet count > 450,000/mcL): An elevated platelet count can increase the risk of blood clots, potentially leading to strokes, heart attacks, or deep vein thrombosis. It may be caused by inflammatory conditions, certain cancers, or iron deficiency.
- Thrombocytopenia (Platelet count < 150,000/mcL): A low platelet count can increase your risk of excessive bleeding, even from minor injuries. It can be caused by various factors, including decreased platelet production, increased platelet destruction, or enlarged spleen trapping platelets.
| Parameters | Male | Female | Unit |
| White blood cell (WBC) Count | 4.1 – 10.34 | 4.3 – 11.68 | x 10^9/L |
| Red blood cell (RBC) count | 4.44 – 5.97 | 3.89 – 5.25 | x 10^12/L |
| Hemoglobin (Hb) level | 13.02 – 17.16 | 11.25 – 15.19 | g/dL |
| Haematocrit | 39.8 – 51.02 | 34.7 – 45.35 | % |
| Mean cell volume (MCV) | 80.72 – 96.93 | 78.63 – 97.22 | fL |
| Mean cell hemoglobin (MCH) | 27.43 – 32.46 | pg | |
| Mean cell hemoglobin concentration (MCHC) | 31.77 – 35.21 | g/dL | |
| Platelet count (PLT) | 155.45 – 389.87 | x 10^9/L | |
| Red cell distribution width (RDW) | 11.7 – 14.43 | % | |
| Neutrophil count (NEUT#) | 1.87 – 6.92 | 1.94 – 7.44 | x 10^9/L |
| Lymphocyte count (LYMPH#) | 1.15 – 3.77 | x 10^9/L | |
| Monocyte count (MONO#) | 0.22 – 0.84 | x 10^9/L | |
| Eosinophil count (EO#) | 0.04 – 0.65 | x 10^9/L | |
| Basophil count (BASO#) | 0.01 – 0.1 | x 10^9/L | |
| NEUT%* | 40.86 – 72.08 | % | |
| LYMPH% | 19.94 – 47.59 | % | |
| MONO% | 4.03 – 11.8 | % | |
| EO% | 0.55 – 8.59 | % | |
| BASO% | 0.13 – 1.73 | % | |
| Reticulocyte count (RET#) | 35.75 – 107.5 | x 10^9/L | |
| RET% | 0.48 – 2.07 | % |
Lymphocyte subsets
Lymphocyte subsets are a specific group of white blood cells (WBCs) within the lymphocyte category that play a critical role in the adaptive immune system. A CBC with differential count doesn’t typically provide a detailed breakdown of lymphocyte subsets. However, some advanced hematology tests can measure these subsets using markers like CD3, CD4, CD8, and calculate the CD4/CD8 ratio.
- CD3 Positive (CD3+): This marker identifies mature T lymphocytes, a major component of the adaptive immune system. A low CD3+ count may suggest immunodeficiency or malnutrition.
- CD4 Positive (CD4+): These are T helper cells, vital for directing and regulating the immune response. They activate other immune cells and help B cells produce antibodies. A low CD4+ count is a hallmark of HIV infection and can also be seen in some autoimmune diseases.
- CD8 Positive (CD8+): These are cytotoxic T lymphocytes (CTLs) that directly target and kill virus-infected cells or abnormal cells like cancer cells. An increased CD8+ count can be seen in viral infections or chronic inflammatory conditions.
- CD4/CD8 Ratio: This compares the number of CD4+ helper T cells to CD8+ cytotoxic T cells.
- A low ratio (less than 1.0): May suggest HIV infection, immunosuppression, or certain autoimmune diseases.
- A high ratio (more than 3.0): Less common, but can be seen in some viral infections or immune system disorders.
| Parameter | Reference Range | Unit |
| CD3# | 694 – 2362 | cell/uL |
| CD4# | 391 – 1548 | cell/uL |
| CD8# | 185 – 1049 | cell/uL |
| CD3% | 51.19 – 81.65 | % |
| CD4% | 26.38 – 54 | % |
| CD8% | 12.89 – 40.69 | % |
| CD4/8 ratio | 0.77 – 3.93 |
Erythrocyte sedimentation rate (ESR)
The Erythrocyte Sedimentation Rate (ESR) is a simple and inexpensive blood test that measures the rate at which red blood cells (RBCs) settle at the bottom of a test tube over a period of time. While not a specific diagnostic tool, an elevated ESR can be a valuable indicator of inflammation or other underlying conditions in the body.
| Parameter | Male | Female | Unit |
| 17 – 50 yr | 1 – 7 | 3 – 9 | mm/hr |
| 51- 60 yr | 2 – 10 | 5 – 15 | mm/hr |
Hemoglobin Subtypes
Hemoglobin subtypes themselves are not routinely measured in a CBC with differential. However, understanding their importance lies in their role in diagnosing specific blood disorders like sickle cell disease and thalassemia. Identifying the type of abnormal hemoglobin helps guide treatment decisions and manage these conditions effectively.
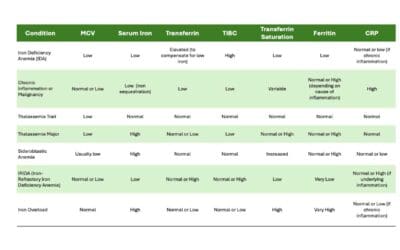
Hematology-related biochemical parameters
These biochemical parameters offer valuable insights into iron status, vitamin deficiencies, and red blood cell production. They are often used in conjunction with a CBC with differential or complete blood picture to diagnose and manage various blood disorders.
Iron Status
- Serum Iron: Measures the amount of iron circulating in the blood attached to a protein carrier called transferrin. Low serum iron can suggest iron deficiency, while high levels might indicate iron overload.
- Total Iron Binding Capacity (TIBC): Reflects the total amount of iron that transferrin can bind. High TIBC with low serum iron suggests iron deficiency, while a low TIBC with high serum iron might indicate inflammation or liver disease.
- Transferrin Saturation: Indicates the percentage of transferrin sites occupied by iron (serum iron divided by TIBC). A low transferrin saturation suggests iron deficiency, while a high saturation could indicate iron overload or inflammation.
- Ferritin: Stores iron in the body, primarily in the liver. Low ferritin is a more reliable indicator of iron deficiency compared to serum iron alone. High ferritin can suggest iron overload or inflammation.
Vitamin Deficiencies
- Serum Vitamin B12: Essential for DNA synthesis and red blood cell production. Deficiency can cause megaloblastic anemia with large, immature red blood cells.
- Serum Folate: Another crucial vitamin for red blood cell production. Deficiency can also lead to megaloblastic anemia.
- Red Cell Folate: Measures folate levels directly within red blood cells, potentially providing a more accurate picture of folate status. Low red cell folate can confirm folate deficiency even if serum folate levels appear normal.
Red Blood Cell Production
- Serum Soluble Truncated Transferrin Receptor (sTfR): Released by bone marrow when iron is deficient to increase iron uptake for red blood cell production. High sTfR levels suggest iron deficiency, while normal or low levels may indicate adequate iron stores or other causes of anemia.
- Serum Haptoglobin: Binds to free hemoglobin released from damaged red blood cells. Low haptoglobin can suggest ongoing hemolysis (destruction of red blood cells).
- Serum Erythropoietin: A hormone produced by the kidneys that stimulates red blood cell production in response to low oxygen levels. High erythropoietin levels can be a sign of anemia due to various causes, including iron deficiency, vitamin deficiencies, or bone marrow problems.
| Parameter | Reference range | Unit |
| Serum iron | 11.5 – 30.5 | umol/L |
| TIBC | 45.5 – 75 | umol/L |
| Transferrin saturation | 15 – 47.5 | % |
| Ferritin | 20 – 325 | ug/L |
| Serum vitamin B12 | 180 – 1000 | pg/mL |
| Serum folate | 7 – 45 | nmol/L |
| Red cell folate | 300 – 1000 | nmol/L |
| Serum soluble truncated transferrin receptor (sTfR) | 9 – 28 | nmol/L |
| Serum haptoglobin | 30 – 200 | mg/dL |
| Serum erythropoietin | 4 – 19 | mU/mL |
Coagulation profile
The coagulation profile, also known as a clotting profile, is a series of blood tests that assess the blood’s ability to form clots and prevent excessive bleeding. It plays a crucial role in diagnosing and managing bleeding and clotting disorders.
- Prothrombin Time (PT): Measures the time it takes for blood to clot after adding tissue factor and calcium. An abnormal PT can indicate deficiencies in factors involved in the extrinsic clotting pathway, such as Factor VII, Factor X, or prothrombin itself. This could increase bleeding risk.
- Activated Partial Thromboplastin Time (APTT): Measures the time it takes for blood to clot after adding a phospholipid and an activator that bypasses the initial steps of clotting. An abnormal APTT suggests deficiencies in factors involved in the common clotting pathway, including Factors VIII, IX, XI, XII, or abnormalities in platelets or clotting proteins. This could also indicate an increased risk of bleeding.
- Thrombin Time (TT): Measures the time it takes for fibrin to form after adding thrombin, the enzyme responsible for converting fibrinogen to fibrin (the clot). An abnormal TT suggests issues with fibrinogen or thrombin activity, potentially leading to impaired clot formation.
Markers for Blood Clot Formation and Breakdown
- D-Dimer: A fragment produced during fibrin breakdown. Elevated D-Dimer levels can suggest increased clotting activity or ongoing clot breakdown, potentially helpful in diagnosing deep vein thrombosis (DVT) or pulmonary embolism (PE). However, other conditions can also elevate D-Dimer.
- Fibrin Degradation Products (FDP): Similar to D-Dimer, these are fragments of fibrin degradation. Elevated FDP levels indicate ongoing clot breakdown, but they are not as specific as D-Dimer.
Tests for Specific Clotting Factors
- Proteins C & S, Antithrombin: These are natural anticoagulants that regulate clot formation. Deficiencies in these proteins can increase the risk of blood clots.
- Factors II (Prothrombin) through XII: These are individual proteins involved in the various clotting pathways. Testing for specific factors helps pinpoint the exact cause of abnormal PT or APTT results, allowing for targeted treatment of clotting factor deficiencies.
Platelet Function Tests
- Platelet Aggregation Test: Measures the ability of platelets to clump together and form a plug at the site of injury, triggered by various agents like collagen, arachidonic acid, ADP, and epinephrine. Abnormal platelet aggregation suggests impaired platelet function, potentially leading to increased bleeding risk. This can be caused by various factors such as medications, inherited disorders, or certain diseases.
- Platelet ATP Release: Measures the release of adenosine triphosphate (ATP) from platelets upon activation, which plays a role in platelet aggregation and signaling. Reduced ATP release can indicate abnormal platelet function.
| Parameter | Reference range | Unit |
| Prothrombin time | 12 – 14 | Seconds (s) |
| Activated partial thromboplastin time (APTT) | 24 – 35 | s |
| Thrombin time (TT) | 12 – 17 | s |
| D-Dimer for DVT/PE | <400 | ng/mL |
| Protein S | 65 – 140 | % |
| Protein C | 70 – 140 | % |
| Antithrombin | 80 – 120 | % |
| Factor II | 50 -150 | % |
| Factor V | 50 -150 | % |
| Factor VII | 50 -150 | % |
| Factor VIII | 50 – 200 | % |
| Factor IX | 50 – 150 | % |
| Factor X | 50 – 150 | % |
| Factor XI | 50 – 150 | % |
| Factor XII | 50 -150 | % |
| Willebrand factor activity | 60 – 200% | % |
| Willebrand factor antigen | 50 – 160 | % |
| Factor VIII-inhibitor | 0 – 0.5 | Bethesda unit |
| alpha2-antiplasmin | 80-120 | % |
| Plasminogen | 80-120 | % |
| Fibrin degradation products (latex particles) | <20 | ug/mL |
| Platelet Aggregation (in platelet-rich plasma) | ||
| with collagen (2ug/mL) | 70-95 | % |
| with arachidonic acid (0.5mM) | 70-100 | % |
| with ADP 5uM | 70-90 | % |
| with ADP 10uM | 70 – 90 | % |
| with epinephrine (5uM) | 75-90 | % |
| with ristocetin (1.0 mg/mL) | 60 -80 | % |
| Platelet ATP release (in blood) | ||
| with thrombin (1 unit) | >0.5 | nmoles of ATP |
| with collagen (2 mg/mL) | 0.5 – 1.7 | nmoles of ATP |
| (5mg/mL) | 0.9 – 1.7 | nmoles of ATP |
| with arachidonic acid (0.5mM) | 0.56 – 1.4 | nmoles of ATP |
| ADP (5mM) | 0 – 0.7 | nmoles of ATP |
| ADP (19mM) | 0.38 – 1.71 | nmoles of ATP |
Disclaimer: This article is intended for informational purposes only and is specifically targeted toward medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. This article does not provide exhaustive information on all aspects of the discussed hematological disorders, and new research and understanding may emerge over time. See additional information.