TL;DR
Venous thromboembolism (VTE) is a condition where a blood clot (thrombosis) forms in a deep vein, usually in the leg (deep vein thrombosis) or pelvis, and can travel to the lungs, causing a pulmonary embolism. This is a serious condition that can be life-threatening if not treated promptly.
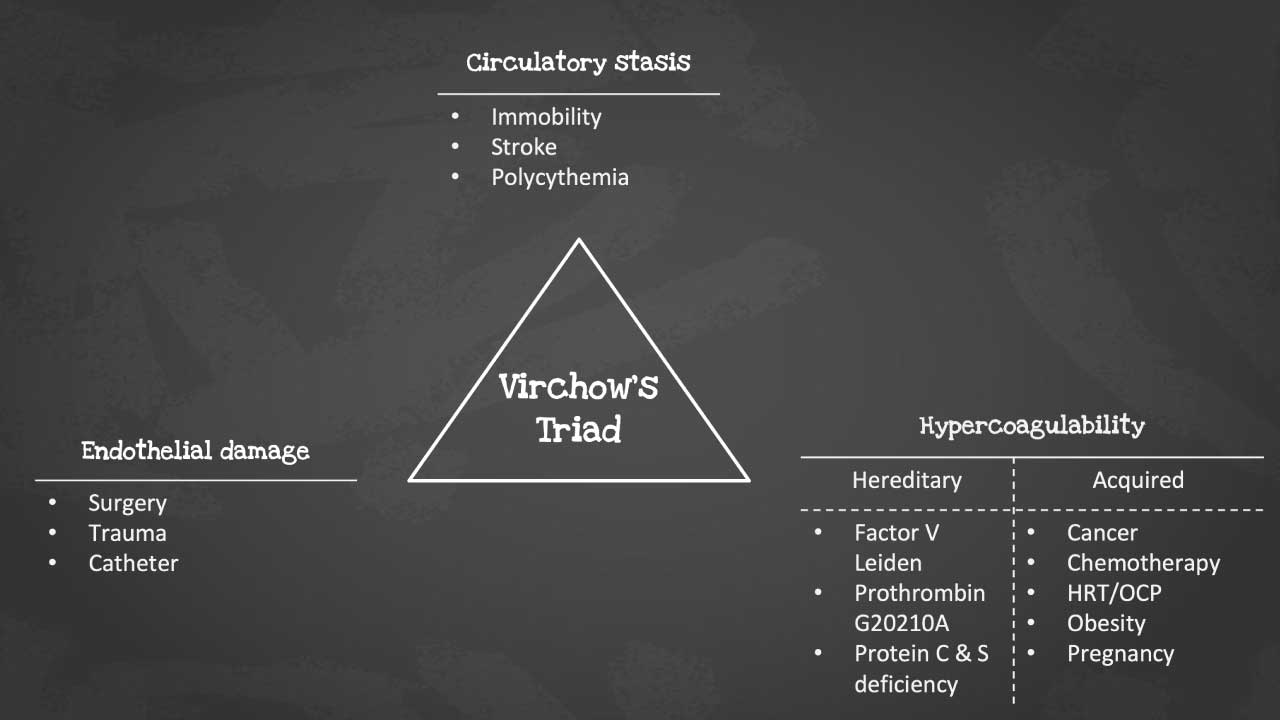
- Virchow’s Triad ▾: endothelial injury, stasis, and hypercoagulability – explains the underlying mechanisms of clot formation, but various other individual risk factors play a role.
- Symptoms ▾: Early symptoms like leg pain, swelling, and warmth can raise suspicions, while shortness of breath and chest pain could signify a life-threatening PE.
- Related disorders ▾: DVT, PE, chronic venous insufficiency & post-thrombotic syndrome.
- Investigation ▾: D-dimer testing and compression ultrasound are essential investigative tools, though specific situations might require CT scans, MRIs, or V/Q scans.
- Treatment ▾: Anticoagulants, the mainstay of treatment, come in various forms like heparin, warfarin, and DOACs, while thrombolysis and mechanical interventions are reserved for specific cases.
- Prevention ▾: Prophylaxis with compression stockings and low-dose anticoagulants is vital for high-risk patients undergoing surgery or facing prolonged immobilization.
*Click ▾ for more information
What is venous thrombosis (VTE)?
When we talk about thrombosis, we usually focus on arteries because their high-pressure flow makes them prone to sudden, dangerous blockages also known as arterial thrombosis. But don’t underestimate the veins! Venous thrombosis (VTE) is when a clot forms in one of these slower-moving vessels, typically in the legs or pelvis.
VTE is often used interchangeably with a broader term, venous thromboembolism (VTE). What’s the difference?
- Venous thrombosis is the formation of the clot itself within the vein.
- Venous thromboembolism refers to the potential consequence of a venous clot – when the clot breaks free, becomes and embolus and travels through the bloodstream to another location, usually the lungs.
So, VTE encompasses both the initial clot formation (venous thrombosis) and the potential for that clot to travel (venous thromboembolism). This distinction is crucial for accurately diagnosing and managing the condition.
What is Thrombosis?
Thrombosis is the formation of a blood clot (called a thrombus) inside a blood vessel. Think of it like a traffic jam within your circulatory system, where blood cells get stuck together instead of flowing smoothly. These clots can partially or completely block the vessel, disrupting the delivery of oxygen and nutrients to vital organs.
Now, let’s dissect the thrombus itself. It’s like a tangled web with three main components:
- Platelets: Platelets clump together at the site of injury to form a plug and stop bleeding. But sometimes, they get overzealous and build up even where they’re not needed, leading to a thrombus.
- Fibrin: Fibrin solidifies the platelet plug into a dense mesh that traps red blood cells. Imagine fibrin strands acting as scaffolding for the clot to grow.
- Red blood cells: These oxygen-carrying cells get caught in the fibrin web, adding bulk and further restricting blood flow.
The balance between these elements is crucial. When the clotting process goes haywire, a thrombus forms, posing a serious threat to health. Remember, while clotting is essential for healing wounds, uncontrolled clotting can cause major problems.
VTE Risk Factors
Venous thromboembolism (VTE) lurks in the shadows, waiting for the perfect storm of risk factors to brew. Understanding these factors, and how they fit into Virchow’s Triad, is key to identifying and preventing this potentially life-threatening condition.
Virchow’s Triad
- Endothelial injury: This is the “trigger” that sets the whole clotting cascade in motion. Think of it as a tear in the vessel lining, inviting platelets and clotting factors to the site of injury. Examples include:
- Inflammation: From infections to autoimmune diseases, inflammation can damage the endothelium.
- Trauma: Surgery, fractures, and even vigorous exercise can cause internal injuries.
- Radiation therapy: This can damage the vascular lining, particularly in the treated area.
- Vascular catheters: These tubes, used for various procedures, can irritate and injure the endothelium.
- Stasis: This is the “slow-down” factor, where sluggish blood flow allows clotting factors to cozy up and form a thrombus. Examples include:
- Prolonged immobilization: Bed rest, casts, and long-distance travel can all lead to stasis.
- Obesity: Excess weight increases pressure in the veins, especially in the legs.
- Pregnancy: Hormonal changes and compression of veins by the growing uterus contribute to stasis.
- Heart failure: This weakens the heart’s pumping capacity, leading to blood pooling in the veins.
- Hypercoagulability: This is the “overdrive” factor, where the body’s natural clotting system goes into overdrive, producing too many clotting factors or not enough inhibitors. Examples include:
- Inherited thrombophilia: Conditions like Factor V Leiden and Protein C deficiency make individuals prone to clotting.
- Acquired thrombophilia: Certain cancers, infections, and autoimmune diseases can trigger hypercoagulability.
- Hormonal factors: Birth control pills and hormone replacement therapy can increase clotting risk.
- Medications: Some drugs, like corticosteroids and tamoxifen, can promote clotting.
While Virchow’s Triad provides a solid framework, other factors can also play a role:
- Age: The risk of venous thrombosis (VTE) increases with age, particularly after 60 years old.
- Previous VTE: Having had a previous venous thromboembolism (VTE) significantly increases the risk of future events.
- Family history of VTE: Genetic predisposition can also play a role.
- Smoking: This damages the endothelium and increases platelet activity.
- Medical conditions: Certain conditions like inflammatory bowel disease and cancer can increase venous thromboembolism (VTE) risk.
Remember, venous thromboembolism (VTE) is often a multifactorial condition, with several risk factors working together to tip the scales towards clot formation. By understanding these factors, you can better identify at-risk individuals, implement preventative measures, and ultimately save lives.
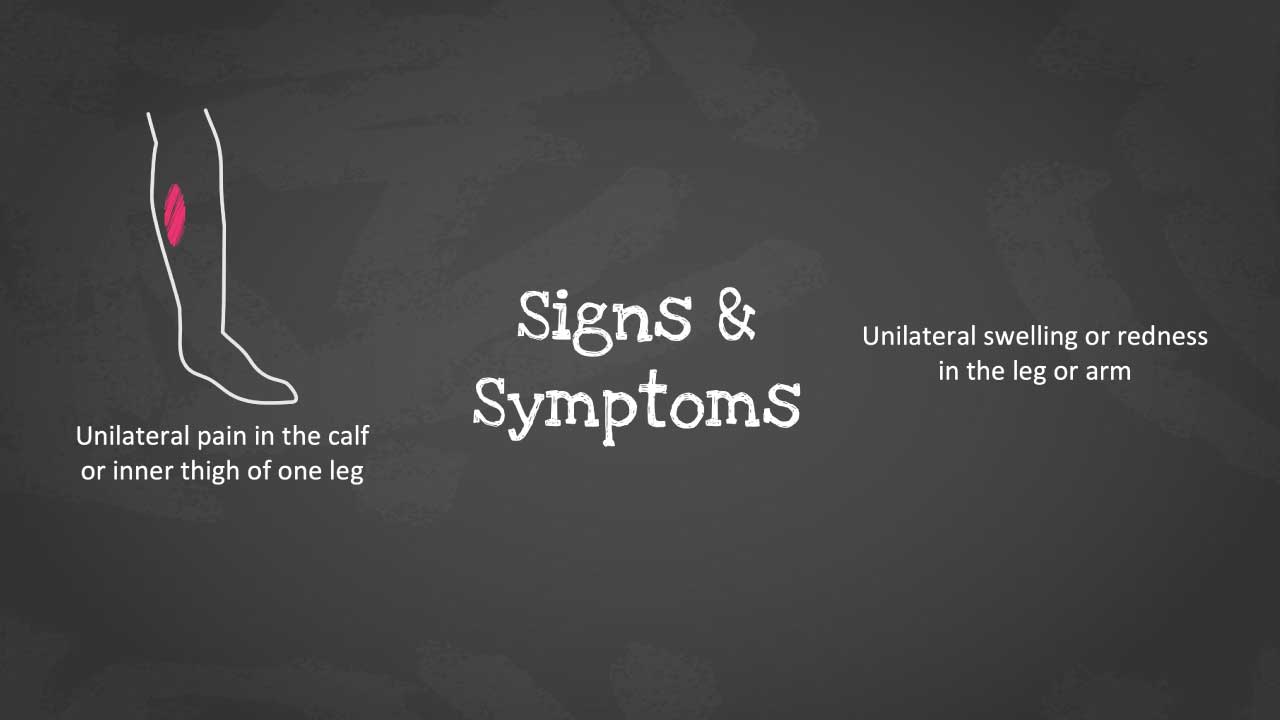
VTE Symptoms and Signs
Venous thromboembolism (VTE) can be a sneaky villain, often lurking in the shadows without throwing up obvious red flags. However, knowing its telltale signs and symptoms can be the key to early diagnosis and preventing potentially life-threatening complications like pulmonary embolism (PE). Let’s delve into the world of VTE symptoms, differentiating between typical and atypical presentations and understanding the significance of each.
Typical Presentation
- Unilateral leg pain: This is the most common clue, with a throbbing or aching sensation often localized to the calf or thigh.
- Swelling: The affected leg appears puffier than the other, sometimes significantly so.
- Tenderness: Pressing on the swollen area elicits pain, like stepping on a hidden bruise.
- Warmth: The affected leg feels warmer to the touch compared to the other leg. Imagine holding a mug of coffee against your skin.
- Skin changes: Discoloration like redness or darkening may appear, especially in later stages. Think of a bruised banana starting to turn brown.
Atypical Presentation
But venous thromboembolism (VTE) isn’t always so obvious. In some cases, it lurks behind the scenes, causing:
- Vague discomfort: Dull ache or tightness in the leg that’s easily mistaken for muscle strain or fatigue.
- Minimal swelling: Noticeable only on close comparison with the other leg.
- Generalized symptoms: Fatigue, fever, and loss of appetite, mimicking various other illnesses.
Dyspnea and Chest Pain
Sometimes, venous thromboembolism (VTE) takes a dramatic turn, sending an embolus traveling to the lungs, causing a potentially life-threatening pulmonary embolism (PE). Watch out for these warning signs:
- Sudden dyspnea (shortness of breath): Difficulty catching your breath, even at rest, is a major alarm bell.
- Sharp chest pain: A stabbing or pleuritic pain that worsens with deep breaths or coughing is another worrying sign.
- Coughing up blood: This is a rare but ominous symptom, indicating a severe PE.
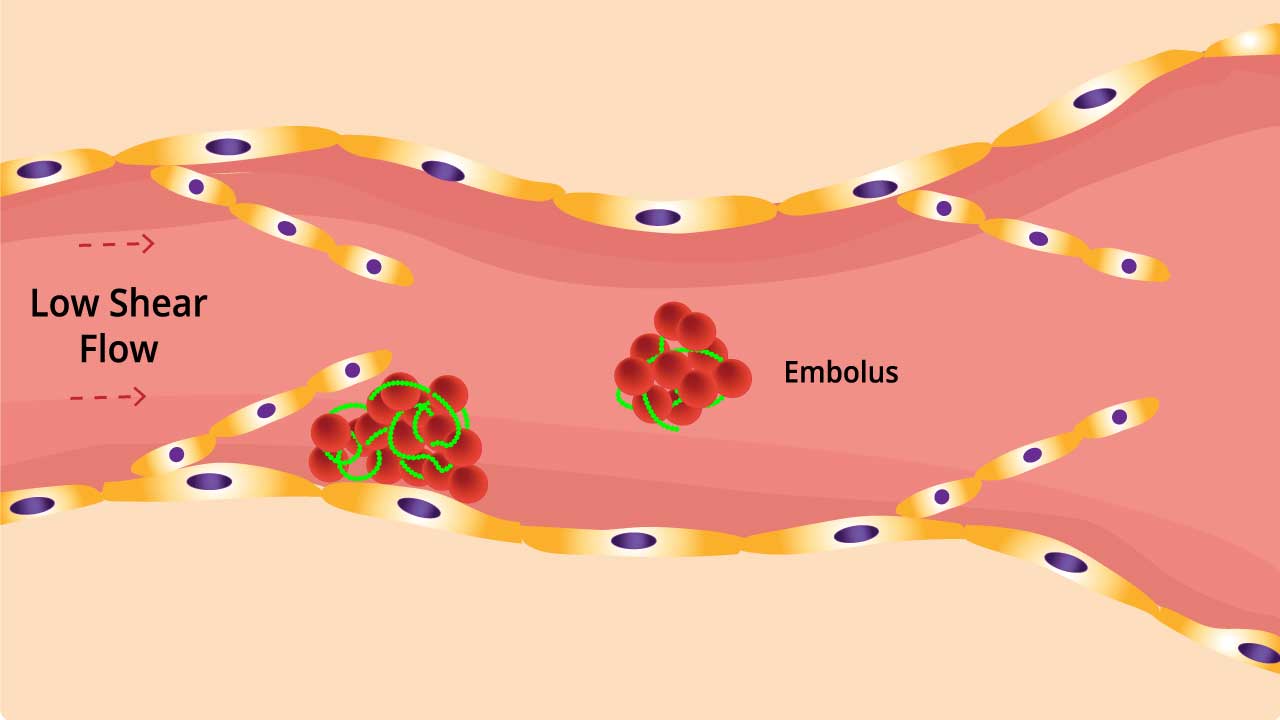
Pathophysiology of VTE
Venous thrombosis tends to occur in areas with decreased or mechanically altered blood flow such as the pockets adjacent to valves in the deep veins of the leg.
While valves help to promote blood flow through the venous circulation, they are also potential locations for venous stasis and hypoxia. Multiple postmortem studies have demonstrated the propensity for venous thrombi to form in the sinuses adjacent to venous valves.
As blood pools, activation products of the coagulation system accumulate locally leading potentially to local hypercoagulability. Activation products of clotting and fibrinolysis can induce endothelial damage which in turn leads to further activation of the hemostasis system. Endothelial damage may also result from distension of the vessel walls by the pooling blood.
Blood flow is further decreased by hyperviscosity due to elevated fibrinogen levels and dehydration. The clot can break off and travel to another part of the body as an embolus. The embolus is dangerous as it can lodge itself in the lungs preventing blood from reaching the lungs and this can be fatal.
Related Disorders of VTE
Venous thrombosis (VTE), the formation of blood clots in veins, isn’t just a standalone condition. It’s a gateway to a cascade of related disorders, each with its own set of complications and potential long-term effects. Let’s delve into some of the most common disorders associated with venous thromboembolism (VTE).
Deep Vein Thrombosis (DVT)
This is the initial formation of a clot in a deep vein, typically in the legs or pelvis. It’s the culprit behind many other venous thromboembolism (VTE)-related issues. Symptoms include leg pain, swelling, warmth, and redness. Left untreated, DVT can lead to:
- Pulmonary embolism (PE): When a DVT breaks free, becomes an embolus and travels to the lungs, it can block a pulmonary artery, causing sudden shortness of breath, chest pain, and even death.
- Post-thrombotic syndrome (PTS): Even after the clot dissolves, damage to the vein can lead to chronic leg pain, swelling, and skin changes.
Pulmonary Embolism (PE)
This is the life-threatening complication of DVT, where an embolus travels to the lungs and blocks an artery. Symptoms include sudden shortness of breath, chest pain, coughing up blood, and rapid heart rate. PE requires immediate medical attention and can be fatal if not treated promptly.
Chronic Venous Insufficiency (CVI)
This condition arises when weakened or damaged veins struggle to pump blood effectively back to the heart. It’s often a consequence of untreated DVT or PTS. Symptoms include chronic leg swelling, fatigue, skin discoloration, and leg ulcers. While not life-threatening, CVI can significantly impact quality of life and requires long-term management.
Post-thrombotic Syndrome (PTS)
This chronic condition develops after a DVT dissolves, leaving behind damaged valves and weakened veins. Symptoms include leg pain, swelling, skin discoloration, and varicose veins. PTS can significantly impact mobility and quality of life, requiring ongoing management and, in some cases, surgical intervention.
Understanding the interconnectedness of these disorders is crucial for:
- Early diagnosis and treatment of venous thromboembolism (VTE): Prompt intervention for DVT can prevent PE and minimize the risk of developing CVI and PTS.
- Effective management of related complications: Each disorder has its own treatment strategies, and understanding the connection helps tailor care to individual needs.
- Preventing future venous thromboembolism (VTE) events: By addressing underlying risk factors and implementing preventive measures, we can break the cycle and reduce the risk of recurrence.
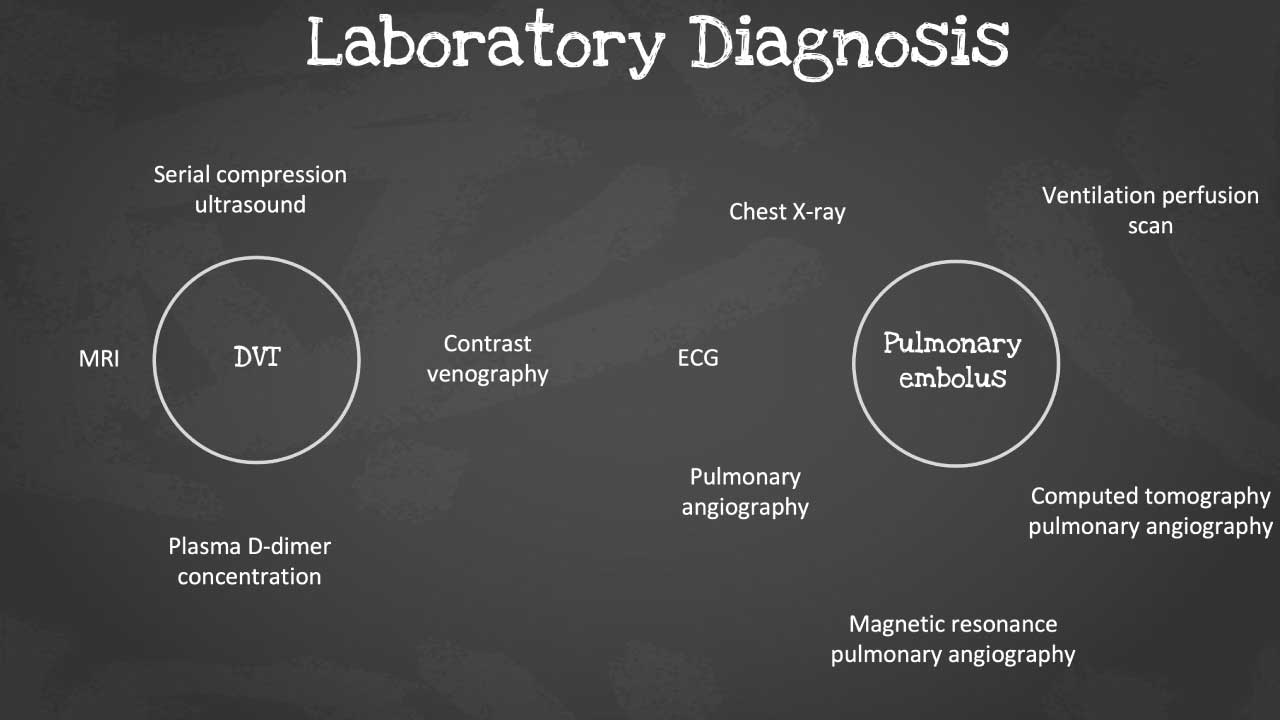
General Laboratory Investigations of VTE
D-dimer Testing
When a clot forms, it breaks down over time, releasing D-dimer into the bloodstream. This test measures the level of D-dimer, providing a quick and non-invasive initial assessment of venous thromboembolism (VTE) risk. High D-dimer levels suggest a recent clot formation, raising suspicion for venous thromboembolism (VTE). Normal D-dimer levels make venous thromboembolism (VTE) less likely, but not entirely ruled out.
D-dimer is a sensitive test, but not specific. Other conditions like infections or recent surgery can also elevate D-dimer levels.
Compression Ultrasound
This is the gold standard for diagnosing deep vein thrombosis (DVT), the most common type of venous thromboembolism (VTE). Using sound waves, it creates a detailed image of the veins, revealing any blood clots obstructing the flow. It accurately identifies or excludes DVT in the legs, arms, or other areas. It is safe and non-invasive with minimal discomfort for the patient.
Additional Investigations
While D-dimer and compression ultrasound are the mainstays, other investigations may be needed in specific scenarios.
- Venography: This X-ray-based technique uses contrast dye to visualize the veins, offering a more comprehensive view but with higher radiation exposure.
- Blood Tests: Specific tests for inherited thrombophilias or other underlying conditions contributing to venous thromboembolism (VTE) risk may be ordered.
- CT Scan: For suspected pulmonary embolism (PE), a CT scan of the lungs can reveal blockages caused by clots traveling from the veins.
- Ventilation-Perfusion (V/Q) Scan: This specialized nuclear medicine test helps assess PE probability by looking at both air flow and blood flow in the lungs. It can be helpful in inconclusive cases.
- Pulmonary angiography: A special type of X-ray test that requires insertion of a large catheter (a long, thin hollow tube) into a large vein (usually in the groin) and into the arteries within the lung, followed by injection of contrast material (dye) through the catheter.
- Magnetic resonance imaging (MRI): Uses radio waves and a magnetic field to provide images of the lung, but this test is usually reserved for certain patients, such as for pregnant women or in patients where the use of contrast material could be harmful.
- Computed tomographic pulmonary angiography (CTPA): A special type of X-ray test that includes injection of contrast material (dye) into a vein.
General Treatment and Management of VTE
Anticoagulants: The Mainstay of Treatment
These medications work by preventing further clot formation and promoting gradual breakdown of existing clots.
- Heparin: This fast-acting injectable works by blocking the activity of clotting factors, particularly thrombin. It’s often the first line of defense, administered intravenously or subcutaneously.
- Warfarin: This classic oral anticoagulant interferes with vitamin K metabolism, indirectly affecting several clotting factors. Also known as Coumadin, it is a long-term player, requiring regular monitoring of blood clotting time (INR) to ensure proper dosage.
- Direct oral anticoagulants (DOACs): These newer medications target specific clotting factors directly, offering convenience with fewer dietary restrictions and less frequent monitoring. They come in various brands, each with its own administration schedule.
Mechanism of Action
Heparin and DOACs block the action of clotting factors, while warfarin affects vitamin K production, which is necessary for clot formation.
Administration Routes
- Heparin can be given intravenously, subcutaneously, or even topically in some cases.
- Warfarin and DOACs are taken orally.
Beyond Anticoagulants
In some cases, additional measures might be needed:
- Thrombolysis: This involves using clot-busting medications like tPA to dissolve existing clots, often used in severe cases or those involving pulmonary embolism (PE).
- Mechanical interventions: Inferior vena cava (IVC) filters can be placed in certain high-risk patients to prevent clots from traveling to the lungs.
Prevention
For high-risk patients undergoing surgery, pregnancy, or other situations, prophylaxis plays a crucial role.
- Compression stockings: Improve blood flow and prevent clot formation.
- Early mobilization: Getting patients moving helps keep blood flowing smoothly.
- Blood thinners: Low-dose anticoagulants can be used in specific cases.
Remember
- Timely diagnosis and prompt treatment are essential for optimal outcomes.
- The choice of treatment depends on the type and severity of venous thromboembolism (VTE), individual risk factors, and patient preferences.
- Close monitoring and follow-up are crucial to ensure successful clot resolution and prevent recurrence.
Frequently Asked Questions (FAQs)
What is the difference between DVT and VTE?
DVT (Deep Vein Thrombosis) is a specific type of VTE (Venous Thromboembolism).
- DVT is when a blood clot forms in a deep vein, usually in the leg or pelvis.
- VTE is a broader term that encompasses both DVT and pulmonary embolism (PE). PE occurs when a clot from a deep vein breaks off and travels to the lungs.
Essentially, all DVT cases are VTE, but not all VTE cases are DVT.
Which 2 conditions are forms of VTE?
Deep vein thrombosis (DVT) and pulmonary embolism (PE) are the two forms of VTE (Venous Thromboembolism).
What is the main cause of VTE?
The main cause of VTE (Venous Thromboembolism) is a combination of factors that disrupt normal blood flow and clotting. These factors include:
- Injury or surgery: Damage to veins can trigger clot formation.
- Immobility: Lack of movement allows blood to pool, increasing the risk of clots.
- Inflammation: Conditions like infections or inflammatory bowel disease can contribute to clot formation.
- Other risk factors: Obesity, age, certain medications, and genetic predispositions also play a role.
What happens if VTE is not treated?
If VTE is left untreated, it can lead to serious complications:
- Pulmonary embolism (PE): A portion of the clot can break loose and travel to the lungs, blocking blood flow and potentially causing death.
- Post-thrombotic syndrome: Damage to the veins caused by the clot can lead to long-term swelling, pain, and skin ulcers.
- Heart problems: A large PE can put significant strain on the heart, leading to heart failure.
What surgeries are high risk for VTE?
Surgeries with a high risk of VTE include:
- Orthopedic surgeries: Hip and knee replacements, femur fractures
- Major abdominal surgeries
- Pelvic surgeries
- Brain and spinal surgeries
- Major trauma
These surgeries often involve extended periods of immobility, which increases the risk of blood clots forming
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Saba HI, Roberts HR. Hemostasis and Thrombosis: Practical Guidelines in Clinical Management (Wiley Blackwell). 2014.
- DeLoughery TG. Hemostasis and Thrombosis 4th Edition (Springer). 2019.
- Keohane EM, Otto CN, Walenga JM. Rodak’s Hematology 6th Edition (Saunders). 2019.
- Kaushansky K, Levi M. Williams Hematology Hemostasis and Thrombosis (McGraw-Hill). 2017.



