TL;DR
Polycythemia vera is a chronic blood disorder characterized by an increased production of red blood cells. It is caused by genetic mutations in the bone marrow particularly JAK2 mutations.
- Symptoms ▾: May include fatigue, headache, dizziness, itching, and enlarged spleen.
- Complications ▾: Increased risk of blood clots (DVT, stroke, heart attack) due to thicker blood.
- Investigations ▾
- Complete Blood Count (CBC) with Differential: Red blood cell count and hemoglobin are typically elevated.
- Hematocrit: Elevated in PV.
- Erythrocyte Sedimentation Rate (ESR): Often low in PV, but not specific to the condition.
- Bone Marrow Examination: Increased cellularity.
- Molecular Mutation Testing: Mutations in JAK2, CALR, or MPL genes are common.
- Serum Erythropoietin (EPO) Level: Usually low in PV due to excess red blood cell production.
- Imaging Studies: X-rays, ultrasounds, or CT scans may be used to assess spleen size or rule out other conditions.
- Diagnostic Criteria ▾: Either all 3 major criteria or first 2 major plus the minor criterion according to the MPN WHO 2022 Diagnostic Criteria.
- Treatment and Management ▾: Aims to reduce red blood cell count through phlebotomy or medications. Aspirin is used to prevent blood clots.
- Prognosis ▾: With proper management, most individuals with polycythemia vera (PV) can live long and fulfilling lives. Early diagnosis and treatment are crucial to minimize complications.
*Click ▾ for more information
What is Polycythemia Vera (PV)?
Polycythemia vera (PV) is a chronic myeloproliferative neoplasm (MPN) characterized by an uncontrolled increase in red blood cell production by the bone marrow, thereby causing en elevated red blood cell count. This overproduction leads to thickening of the blood, which can significantly impact blood flow and increase the risk of serious complications like blood clots (thrombosis) and bleeding.
What is Polycythemia?
Polycythemia refers to a condition in which there is an abnormally high number of red blood cells in the blood. The term “polycythemia” is sometimes used interchangeably with “erythrocytosis,” which specifically refers to an increase in red blood cells. However, “polycythemia vera” is a specific type of myeloproliferative neoplasm where there is an increase in all blood cell lines (red blood cells, white blood cells, and platelets), with the increase in red blood cells being the most prominent feature.
Polycythemia can be broadly classified into two main categories:
Absolute Polycythemia (True Erythrocytosis)
This involves an actual increase in the total red blood cell mass in the body. It can be further divided into:
- Primary Polycythemia: This is caused by a problem within the bone marrow itself, leading to the overproduction of red blood cells. Polycythemia vera is the most common type of primary polycythemia and is often associated with a JAK2 gene mutation. In primary polycythemia, erythropoietin (EPO) levels are typically low or normal.
- Secondary Polycythemia: This occurs as a result of an underlying condition that stimulates the body to produce more red blood cells. EPO levels are usually elevated in secondary polycythemia. Causes of secondary polycythemia include:
- Hypoxia-related: Conditions causing low oxygen levels in the body, such as chronic lung disease (COPD), sleep apnea, high altitude, smoking, and certain heart defects.
- EPO-producing conditions: Tumors (e.g., renal cell carcinoma, hepatocellular carcinoma), kidney problems (e.g., renal artery stenosis), and certain medications (e.g., anabolic steroids, testosterone).
- Genetic conditions: Some inherited conditions can cause increased red blood cell production for example Hb Chesapeake which has an abnormally high oxygen affinity. This condition leads to increased RBC production due to the body’s response to perceived or actual hypoxia.
Relative Polycythemia (Apparent/Spurious Polycythemia)
In this condition, the increase in red blood cell concentration is not due to an actual increase in red blood cell mass, but rather a decrease in plasma volume (the liquid part of the blood). This can be caused by dehydration, stress, diuretic use, or conditions like Gaisböck syndrome (often seen in obese, hypertensive men who smoke). The total red blood cell mass is normal in relative polycythemia.
Pathogenesis and Pathophysiology
Bone Marrow Overproduction
In healthy individuals, the bone marrow tightly regulates the production of different blood cells, including red blood cells, white blood cells, and platelets. However, in polycythemia vera, this regulation goes awry, leading to uncontrolled overproduction of all three cell lineages.
- Red blood cells: The most prominent feature of polycythemia vera (PV) is a significant increase in red blood cell production. This leads to a condition called erythrocytosis, which literally translates to “excess of red blood cells” with an elevated red blood cell count.
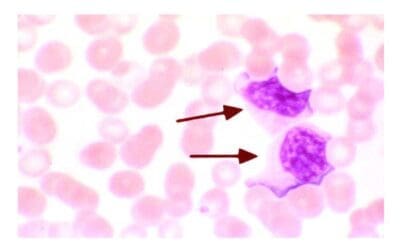
- White blood cells: While the increase in white blood cells (leukocytosis) may be moderate in polycythemia vera, it can sometimes be significant.
- Platelets: Similar to white blood cells, the rise in platelet count (thrombocytosis) can be variable in polycythemia vera patients.
The Role of the JAK-STAT Pathway
The JAK-STAT pathway is a critical signaling pathway involved in normal blood cell production.
In healthy individuals, specific hormones bind to cell surface receptors, activating JAK proteins. These activated JAKs then phosphorylate (activate) STAT proteins, which translocate to the nucleus and turn on specific genes responsible for normal blood cell development (hematopoiesis) and maturation.
This pathway ensures controlled and regulated production of blood cells based on the body’s needs.
Mutations and Dysregulation
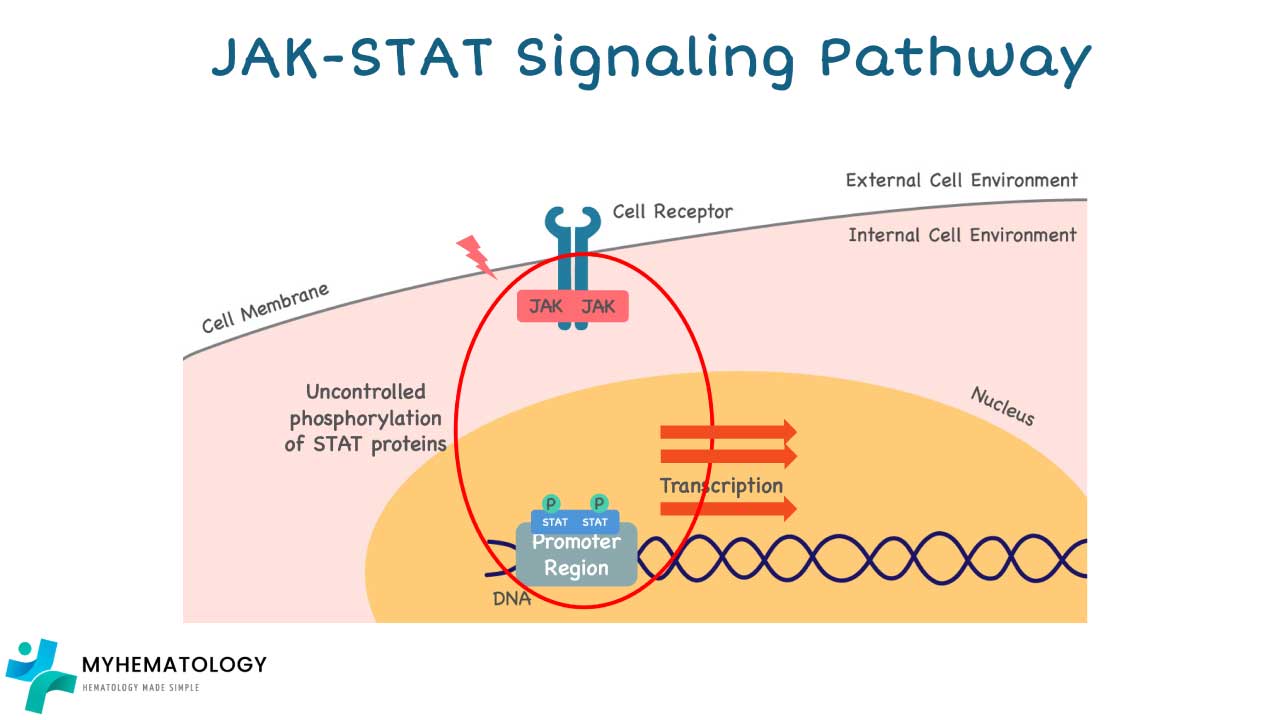
In polycythemia vera (PV), specific mutations occur in genes encoding proteins involved in the JAK-STAT pathway, leading to its dysregulation:
The primary mutation associated with Polycythemia Vera is in the JAK2 gene, specifically:
- JAK2 V617F mutation: This is found in approximately 95% of PV patients. This mutation leads to a constantly active JAK2 protein, which promotes the uncontrolled growth and division of blood cells, particularly red blood cells, but also white blood cells and platelets.
- JAK2 exon 12 mutations: These are found in most of the remaining 5% of PV patients who do not have the JAK2 V617F mutation.
While CALR (calreticulin) and MPL (myeloproliferative leukemia virus oncogene) mutations are also associated with other myeloproliferative neoplasms like essential thrombocythemia (ET) and primary myelofibrosis (PMF), they are rarely found in PV. Recent research indicates that CALR mutations can be associated with JAK2-negative PV in very rare cases, but the JAK2 mutations are the defining genetic characteristic for the vast majority of PV diagnoses.
These mutations essentially act like a “stuck accelerator” in the JAK-STAT pathway, constantly stimulating blood cell production regardless of the body’s actual needs.
Consequences of Increased Blood Cell Production
The overproduction of all three blood cell types in PV has several consequences, primarily affecting blood viscosity and blood flow
- Increased blood viscosity: With an elevated red blood cell count, platelets, and even white blood cells, the blood becomes thicker and stickier.
- Impeded blood flow: Thicker blood flows less easily through narrow blood vessels, potentially leading to ischemia (reduced oxygen supply) in tissues and organs.
Risk Factors and Polycythemia Vera (PV) Causes
While the exact cause of polycythemia vera (PV) remains unknown, several risk factors are associated with an increased chance of developing the disease.
- Age: PV is primarily diagnosed in older adults, with the average age of diagnosis being around 60-65 years. The risk increases significantly after the age of 40.
- Family history: Having a close relative (parent, sibling, child) with polycythemia vera (PV) slightly increases the risk compared to the general population. However, the majority of polycythemia vera (PV) cases occur in individuals with no family history.
- Smoking: Smoking is considered a potential risk factor for polycythemia vera (PV), although the exact link is not fully understood.
Polycythemia Vera Symptoms and Signs
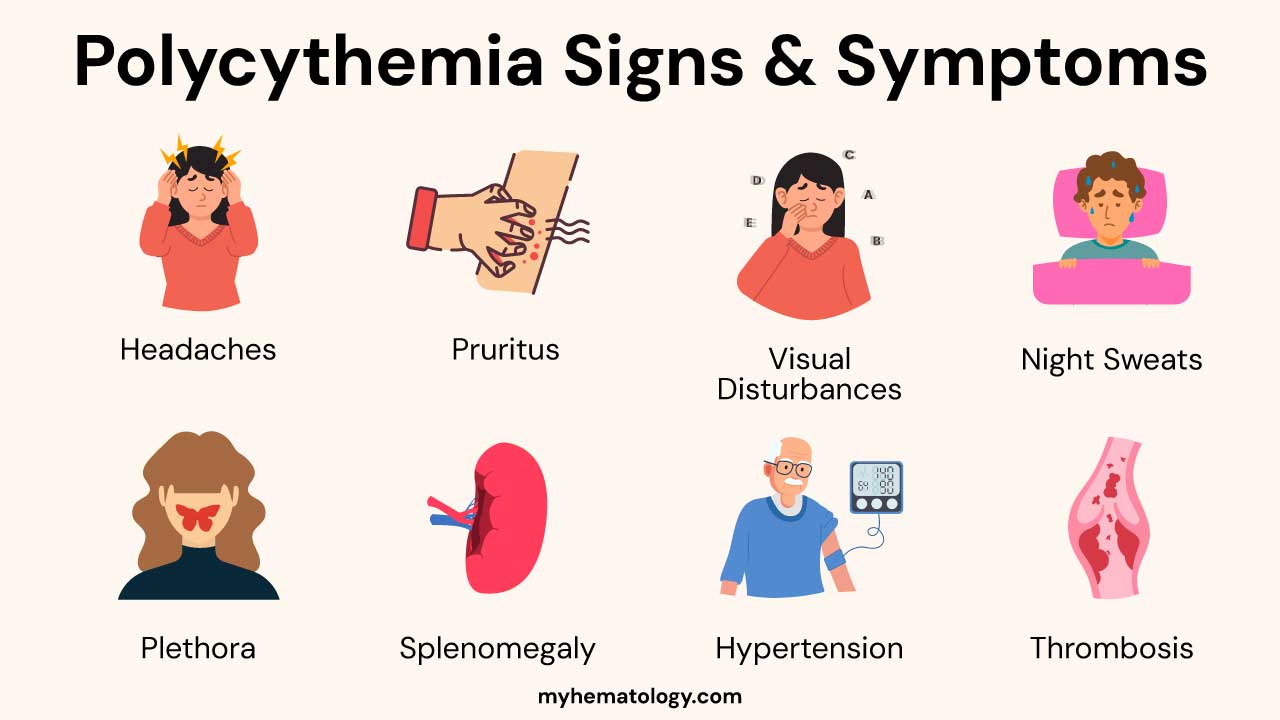
Polycythemia Vera (PV) symptoms and signs arise primarily from the increased red blood cell mass and the resulting hyperviscosity (thickening of the blood). This sluggish blood flow can affect various organs and systems. Additionally, the overproduction of other blood cell lines (white blood cells and platelets) and the underlying myeloproliferative disorder can contribute to certain symptoms.
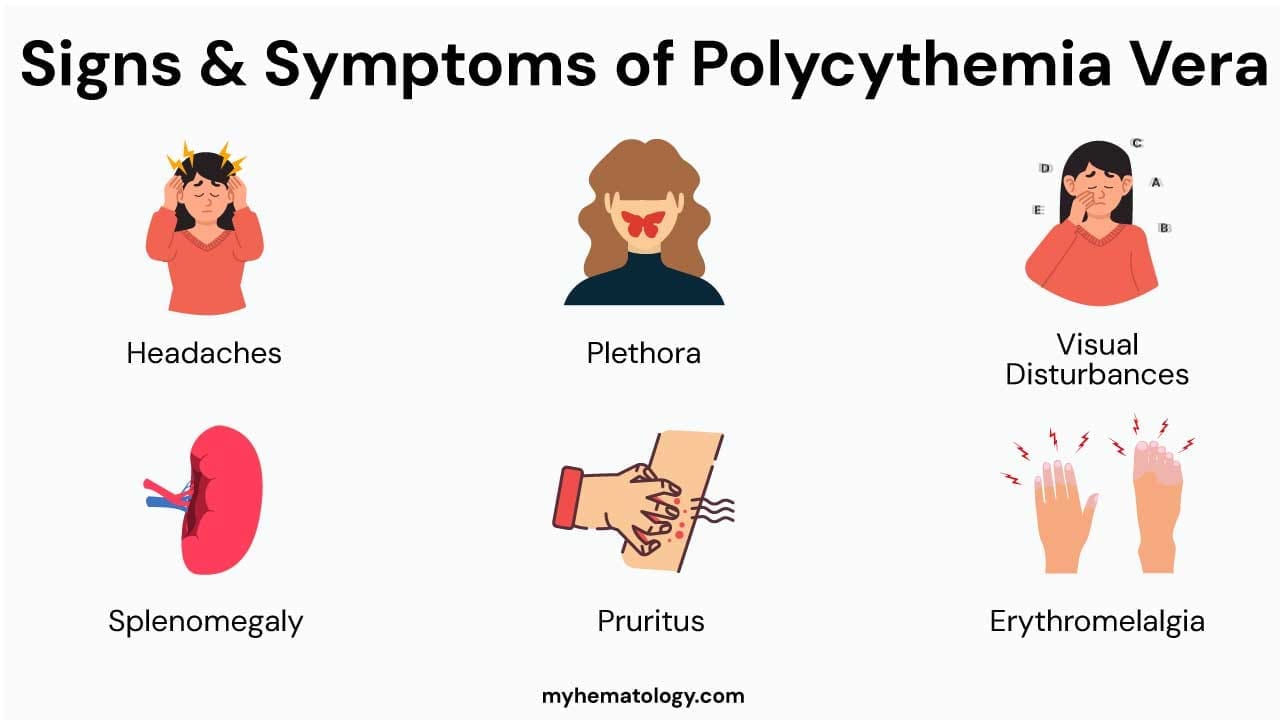
Polycythemia Vera Symptoms Related to Hyperviscosity and Reduced Blood Flow
- Headache: Often described as a dull, throbbing, or persistent ache. The increased blood volume and viscosity can lead to increased intracranial pressure and affect cerebral blood flow.
- Dizziness and Lightheadedness: Impaired blood flow to the brain can cause feelings of imbalance, spinning sensations, or a near-fainting feeling.
- Fatigue: A common and often debilitating symptom. While counterintuitive (more oxygen-carrying capacity), the increased blood viscosity can reduce efficient oxygen delivery to tissues, leading to fatigue. The underlying myeloproliferative process can also contribute.
- Weakness: General lack of physical strength and energy, possibly due to impaired tissue perfusion.
- Visual Disturbances: Blurred vision, double vision (diplopia), transient visual loss (amaurosis fugax) can occur due to reduced blood flow to the eyes or retinal vasculature.
- Tinnitus: Ringing, buzzing, or other sounds in the ears, potentially related to altered blood flow in the inner ear.
- Neurological Symptoms: In severe cases of hyperviscosity, patients might experience more serious neurological issues like transient ischemic attacks (TIAs) or even strokes. Paresthesias (numbness, tingling, or burning sensations, especially in the extremities) can also occur due to impaired microcirculation.
Polycythemia Vera Symptoms due to Increased Blood Volume and Plethora
Plethora (Reddened Face): The increased number of red blood cells circulating near the skin surface gives the face, lips, and mucous membranes a characteristic flushed, ruddy, or even purplish appearance. This is a hallmark sign.
Polycythemia Vera Symptoms Related to Splenomegaly
- Left Upper Abdominal Fullness or Discomfort: The enlarged spleen can press on other abdominal organs, causing a feeling of fullness, pressure, or mild pain in the left upper quadrant.
- Early Satiety: The enlarged spleen can compress the stomach, leading to feeling full quickly after eating only a small amount of food.
- Abdominal Pain: Can occur due to splenic enlargement or, less commonly, splenic infarction.
Polycythemia Vera Symptoms Related to Thrombocytosis and Endothelial Dysfunction
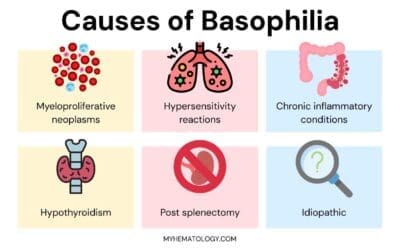
- Pruritus (Itching), Especially After a Warm Bath (Aquagenic Pruritus): This is a very characteristic symptom of polycythemia vera, although the exact mechanism is not fully understood. It’s thought to involve the release of histamine or other pruritogenic substances from basophils or mast cells, potentially exacerbated by changes in skin blood flow or nerve endings after exposure to warm water.
- Erythromelalgia: A burning pain, redness, and warmth in the extremities (hands and feet), often triggered by warmth or exercise. This is thought to be related to platelet activation and microvascular disturbances.
- Transient Ischemic Attacks (TIAs) and Other Microvascular Disturbances: Increased platelet activity and endothelial dysfunction can contribute to transient neurological symptoms or other microcirculatory issues.
Polycythemia Vera Symptoms Related to Increased Cell Turnover and Metabolic Changes
- Gout: Increased breakdown of blood cells leads to elevated uric acid levels, which can precipitate gout attacks (sudden, severe joint pain, redness, and swelling, often in the big toe).
- Night Sweats: Can occur, although less prominent than in some other hematological malignancies. The underlying myeloproliferative process can contribute to systemic symptoms.
- Unexplained Weight Loss: Less common in early polycythemia vera but can occur as the disease progresses or transforms.
Bleeding Tendencies (Paradoxical)
While the increased blood viscosity might intuitively suggest a higher risk of clotting, some PV patients can also experience increased bleeding tendencies (e.g., nosebleeds, easy bruising, gum bleeding, heavy menstrual periods). This is thought to be due to acquired von Willebrand factor deficiency or platelet dysfunction in some cases.
Asymptomatic Presentation
A significant number of individuals, especially in the early stages of PV, may be asymptomatic. The diagnosis is often made incidentally based on abnormal blood test results obtained during routine checkups or investigations for other reasons.
Polycythemia Vera Symptoms due to Complications
- Blood clots (thrombosis): Elevated blood cell production and thickening of the blood can significantly increase the risk of blood clots forming in arteries and veins. Depending on the location of the clot, symptoms can vary widely, ranging from:
- Deep vein thrombosis (DVT): Pain, swelling, and redness in the legs, often affecting one leg more than the other.
- Pulmonary embolism (PE): Sudden shortness of breath, chest pain, coughing, and rapid breathing.
- Bleeding: While less common than blood clots, PV can also increase the risk of bleeding, particularly from areas like the nose or gums, due to alterations in platelet function or abnormalities in the blood vessel walls.
Complications of Polycythemia Vera
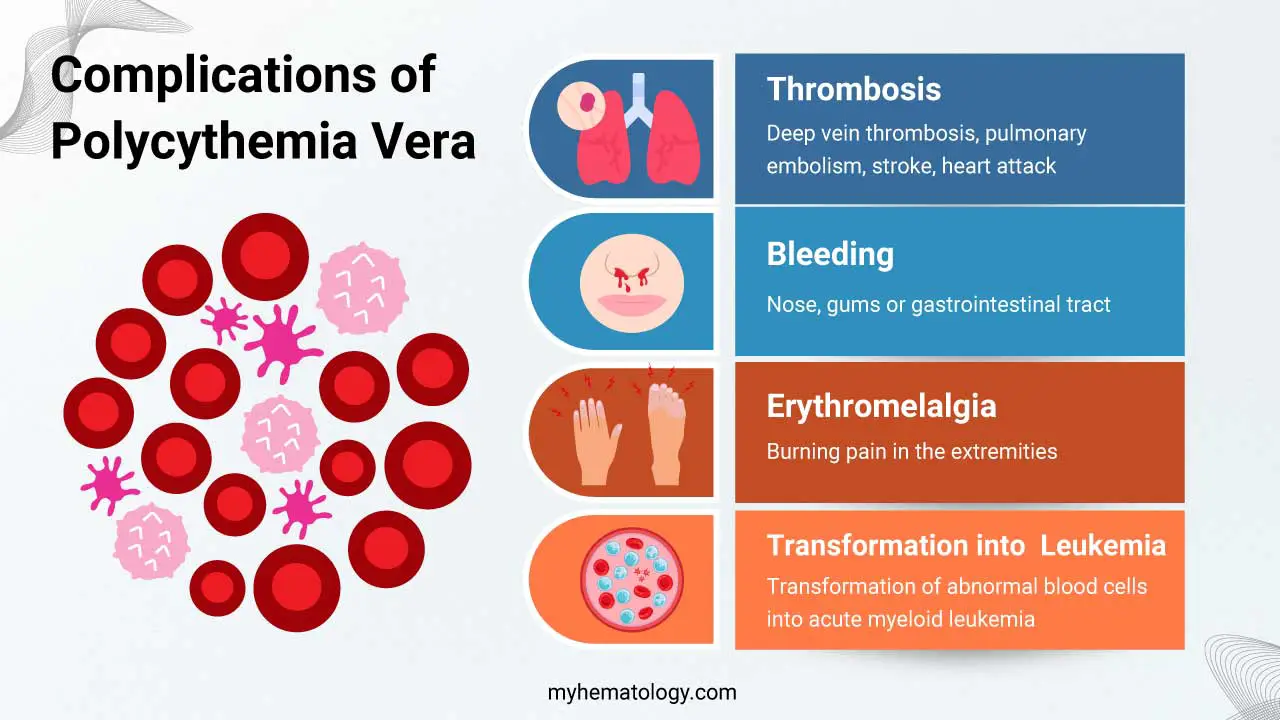
Polycythemia vera (PV) can lead to various complications if left untreated or not effectively managed.
Blood Clots (Thrombosis)
This is the most common and potentially serious complication of PV. Increased blood viscosity and abnormal platelet function contribute to a higher risk of blood clots forming in arteries and veins.
Depending on the location of the clot, symptoms can vary:
- Deep vein thrombosis (DVT): Pain, swelling, redness, and warmth in the legs.
- Pulmonary embolism (PE): Sudden shortness of breath, chest pain, coughing (may bring up blood), rapid heart rate, and lightheadedness.
- Stroke: If a clot blocks an artery in the brain, it can lead to weakness, numbness, speech difficulties, and other neurological symptoms depending on the affected area.
- Heart attack: If a clot blocks an artery supplying blood to the heart muscle, it can cause chest pain, shortness of breath, sweating, and nausea.
Bleeding
While less common than blood clots, PV can also increase the risk of bleeding, especially from areas like the nose, gums, or gastrointestinal tract. This is because abnormal platelet function and increased blood viscosity can impair the normal clotting process.
Erythromelalgia
This is a rare but potential complication of PV, characterized by burning pain, redness, and increased skin temperature, primarily affecting the extremities.

Transformation into Acute Leukemia
This is a rare but serious complication, occurring in less than 1% of polycythemia vera (PV) patients over time. It involves the transformation of abnormal blood cells in the bone marrow into acute myeloid leukemia (AML).
Investigations in Polycythemia Vera
Diagnosing polycythemia vera involves a combination of clinical evaluation, laboratory tests, and sometimes bone marrow examination.
Complete Blood Count (CBC) with Differential
In polycythemia vera (PV), the CBC typically shows:
- Elevated red blood cell count (erythrocytosis)
- May show normal or slightly elevated white blood cell and platelet counts
- Hematocrit: This measures the percentage of red blood cells in whole blood. In PV, the hematocrit is typically elevated, often above 50% in men and 48% in women.
Erythrocyte Sedimentation Rate (ESR)
While not specific for PV, this test measures the rate at which red blood cells settle in a blood sample. An elevated ESR is not uncommon in polycythemia vera (PV) but can also occur in other conditions and is not diagnostic on its own.
Bone Marrow Examination
This may be necessary to confirm the diagnosis and rule out other conditions that can mimic PV. In PV, the bone marrow often shows increased cellularity (more blood cells) and may reveal specific abnormalities suggestive of the disease.
Molecular Mutation Testing
This analyzes the genetic mutations associated with PV, particularly:
- JAK2 V617F mutation: This is the most common mutation, found in around 95% of polycythemia vera (PV) patients.
- CALR and MPL mutations: These occur in a smaller percentage of patients.
Identifying these mutations strongly supports the diagnosis of PV and helps guide treatment decisions.
Other Relevant Investigations
- Imaging studies: X-rays, ultrasounds, or CT scans may be used to check for enlarged spleen (splenomegaly) or other potential complications.
- Serum erythropoietin (EPO) level: This hormone stimulates red blood cell production. In most PV cases, the EPO level is low due to the bone marrow already overproducing red blood cells. However, normal or elevated EPO levels might indicate secondary polycythemia instead of polycythemia vera (PV).
Diagnostic Criteria
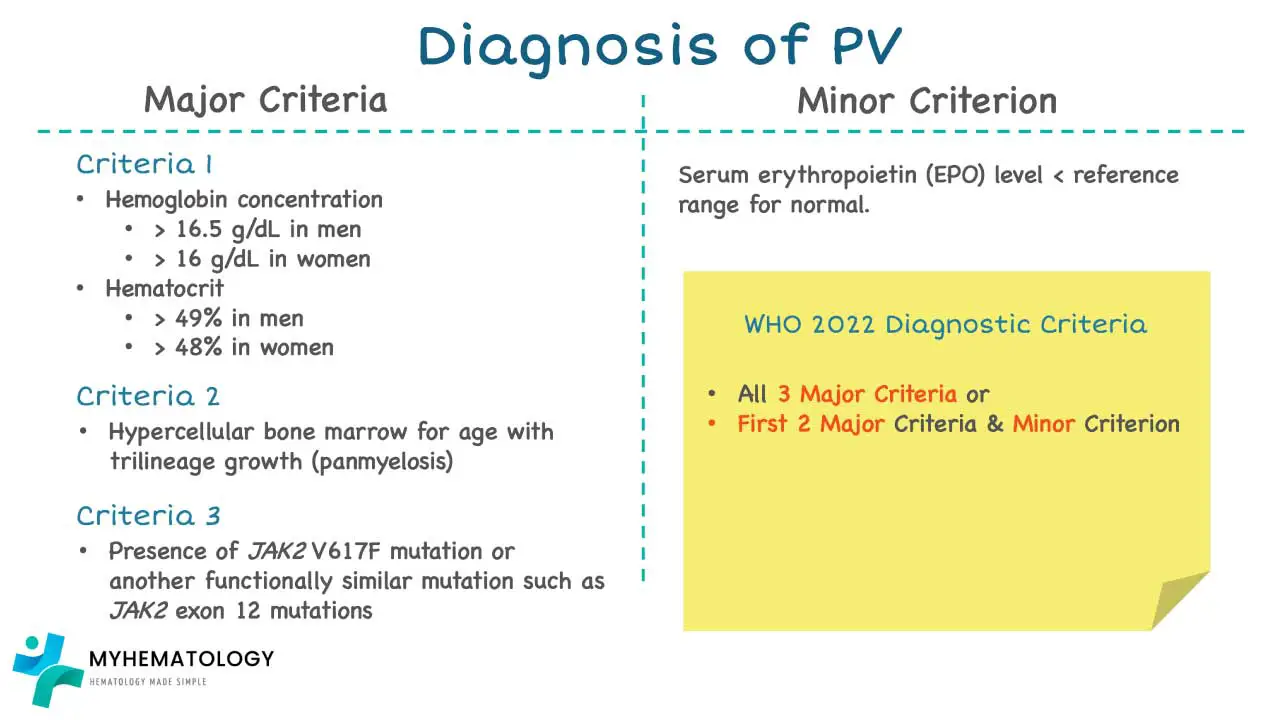
A diagnosis of polycythemia vera (PV) requires either all 3 major criteria or first 2 major plus the minor criterion of according. to the 2022 WHO Diagnostic Criteria for MPN.
Major criteria
- Increased Hb concentration hematocrit or RBC mass
- Hypercellular BM biopsy (after age-adjusted) displaying proliferation of all lineages with prominent erythroid and granulocytic lineages and increase in pleomorphic, mature megakaryocytes without atypia
- JAK2V617F or JAK2 exon 12 mutation
Minor criterion
- Low serum EPO level
Treatment and Management
The treatment and management of Polycythemia Vera (PV) aim to reduce the risk of thrombotic events (the most significant cause of morbidity and mortality), alleviate symptoms, and prevent disease progression to myelofibrosis or acute leukemia. The approach is individualized based on the patient’s risk stratification, age, comorbidities, and symptom burden.
Risk Stratification
- High-Risk: Patients with any of the following:
- Age ≥ 60 years
- History of prior thrombotic event (arterial or venous)
- Low-Risk: Patients who do not meet any high-risk criteria (age < 60 years and no history of thrombosis).
Risk stratification guides the intensity of treatment.
Phlebotomy (Venesection)
Regular removal of a unit of blood (usually 450-500 mL) is performed. The frequency of phlebotomy varies depending on the individual patient’s Hct levels and the response to treatment.
Initially, it may be needed weekly or even more frequently, gradually decreasing as the Hct stabilizes. The goal of phlebotomy is to reduce the red blood cell mass and maintain the hematocrit (Hct) below a target level, typically <45% for both men and women.
Maintaining this target has been shown to reduce the risk of cardiovascular events and thrombosis. Repeated phlebotomies can lead to iron deficiency. While this can help control erythrocytosis, symptomatic iron deficiency should be managed cautiously, and the primary goal remains Hct control.
Iron supplementation is generally avoided unless severe symptomatic deficiency occurs and Hct control remains adequate.
Low-Dose Aspirin
This is recommended for most polycythemia vera patients, regardless of risk stratification, unless there are contraindications (e.g., history of major bleeding, aspirin allergy). It acts as an antiplatelet agent, reducing the risk of thrombotic events by inhibiting platelet aggregation. The dosage is typically 75-100 mg once daily.
Cytoreductive Therapy
- Indications: Primarily for high-risk patients and sometimes for low-risk patients with:
- Symptomatic thrombocytosis (high platelet count causing symptoms).
- Progressive splenomegaly causing discomfort or cytopenias.
- Constitutional symptoms (e.g., severe pruritus, night sweats) refractory to other treatments.
- Poor tolerance of phlebotomy or requiring frequent phlebotomies to maintain Hct.
- History of microvascular disturbances (e.g., erythromelalgia, transient neurological events).
- Common Cytoreductive Agents
- Hydroxyurea: A commonly used first-line agent. It is a ribonucleotide reductase inhibitor that reduces the production of all blood cell lines.
- Dosage: Started at a low dose and adjusted based on blood counts and tolerability.
- Monitoring: Regular monitoring of CBC is essential due to the risk of myelosuppression (anemia, leukopenia, thrombocytopenia).
- Side Effects: Can include skin rashes, mucositis, gastrointestinal disturbances, and, rarely, secondary malignancies with long-term use.
- Interferon-alpha (IFN-α) (including pegylated forms): Can be an effective option, particularly for younger patients and pregnant women (category C). It has immunomodulatory and antiproliferative effects.
- Dosage: Administered subcutaneously, frequency varies depending on the formulation.
- Monitoring: Regular monitoring for side effects, including flu-like symptoms, fatigue, depression, and autoimmune complications.
- Advantages: May have disease-modifying potential and lower risk of secondary malignancies compared to hydroxyurea.
- Ruxolitinib: A JAK1/JAK2 inhibitor. Particularly useful for patients with symptomatic splenomegaly or refractory pruritus, or those intolerant or resistant to hydroxyurea.
- Dosage: Administered orally twice daily, based on platelet count.
- Monitoring: Regular monitoring of CBC is essential as it can cause myelosuppression.
- Side Effects: Can include thrombocytopenia, anemia, neutropenia, increased risk of infections, and non-melanoma skin cancers.
- Anagrelide: Primarily a platelet-lowering agent. May be used in ET-like PV with predominantly thrombocytosis, but less effective for erythrocytosis control.
- Hydroxyurea: A commonly used first-line agent. It is a ribonucleotide reductase inhibitor that reduces the production of all blood cell lines.
Management of Polycythemia Vera Symptoms
- Pruritus
- Antihistamines (e.g., diphenhydramine, loratadine).
- Selective serotonin reuptake inhibitors (SSRIs) like paroxetine.
- Cholestyramine (bile acid sequestrant).
- Ultraviolet B (UVB) phototherapy.
- Ruxolitinib can be very effective for refractory pruritus.
- Gout: Managed with urate-lowering agents (e.g., allopurinol) during acute flares and for prophylaxis.
- Erythromelalgia (burning pain and redness in extremities): Low-dose aspirin, avoidance of triggers (heat, standing for long periods), sometimes cytoreductive therapy.
Management of Complications
- Thrombosis: Prompt treatment with anticoagulants (e.g., heparin, warfarin, direct oral anticoagulants). Address underlying risk factors.
- Bleeding: Manage appropriately based on the site and severity. Avoid unnecessary antiplatelet or anticoagulant use in patients with bleeding tendencies.
- Transformation to Myelofibrosis: Management is complex and may involve supportive care, JAK inhibitors (e.g., ruxolitinib for symptomatic splenomegaly or constitutional symptoms), and potentially allogeneic stem cell transplantation in selected younger patients.
- Transformation to Acute Leukemia: Treatment follows standard protocols for acute myeloid leukemia (AML).
Lifestyle Modifications and Supportive Care
- Hydration: Maintaining adequate hydration is important to reduce blood viscosity.
- Avoidance of Dehydration: Be cautious in hot weather or during strenuous exercise.
- Smoking Cessation: Crucial for overall cardiovascular health.
- Management of Cardiovascular Risk Factors: Control hypertension, diabetes, and hyperlipidemia.
- Regular Exercise: As tolerated.
- Patient Education and Support: Providing information about the disease, treatment options, and potential complications is essential. Support groups can be beneficial.
Monitoring and Follow-Up
- Regular monitoring of CBC (frequency depends on treatment and stability).
- Assessment of spleen size.
- Evaluation for new symptoms or complications.
- Monitoring for treatment side effects.
- Bone marrow biopsies may be repeated in certain situations (e.g., suspected disease progression).
Prognosis
Polycythemia Vera (PV) is a chronic condition that currently can’t be cured. However, with proper treatment and management, most patients can maintain a good quality of life and have a near-normal life expectancy.
In recent years, polycythemia vera (PV) prognosis has significantly improved due to advancements in treatment strategies and greater understanding of the disease. The median survival for patients with polycythemia vera (PV) is around 14-20 years, and many patients live significantly longer.
Frequently Asked Questions (FAQs)
Can polycythemia vera be cured?
Currently, polycythemia vera (PV) cannot be cured. However, the good news is that with proper treatment and management, most patients with polycythemia vera (PV) can achieve a good quality of life and have a near-normal life expectancy.
What organ does polycythemia affect?
Polycythemia vera (PV) primarily affects the bone marrow, which is the soft, spongy tissue inside some of our bones responsible for producing blood cells.
In polycythemia vera (PV), the bone marrow becomes overactive due to genetic mutations, leading to:
- Increased production of red blood cells: The most characteristic feature of polycythemia vera (PV) is an abnormally elevated red blood cell count in the bloodstream.
- Potential increase in white blood cells and platelets: While not always the case, in some individuals with polycythemia vera (PV), the overactive bone marrow may also lead to an increase in the production of white blood cells and platelets.
While the bone marrow is the primary organ directly affected by polycythemia vera (PV), the increased number of blood cells can have consequences for various organs throughout the body, including:
- Blood vessels: Thickened blood due to elevated red blood cell count can lead to increased blood viscosity, making it harder for blood to flow smoothly through the vessels. This can potentially increase the risk of blood clots and impair blood flow to vital organs.
- Spleen: The spleen helps filter old and damaged blood cells. In polycythemia vera (PV), the spleen can become enlarged due to the increased workload of removing excess red blood cells.
- Liver: Similar to the spleen, the liver can also be affected in some cases of polycythemia vera (PV), potentially leading to liver function abnormalities.
- Skin: The increased blood viscosity can contribute to itching, particularly after exposure to hot water (aquagenic pruritus).
What is end stage polycythemia vera?
While the term “end stage” isn’t commonly used in the context of Polycythemia Vera (PV), some sources describe an advanced stage with specific characteristics.
Polycythemia vera (PV) is a chronic condition, and it’s not considered curable. However, with proper management, most patients can live long and fulfilling lives. Nonetheless, as the disease progresses, complications can arise, and some individuals might experience a more advanced stage with specific features.
- Transformation: In rare cases (less than 1%), PV can transform into other blood cancers, primarily acute myeloid leukemia (AML) over time. This is considered a serious and life-threatening complication.
- Myelofibrosis: This can occur when the bone marrow becomes progressively scarred and replaced by fibrous tissue, hindering its ability to produce healthy blood cells. This can lead to complications like anemia (low red blood cell count), fatigue, and splenomegaly and hepatomegaly.
What level of hemoglobin is dangerously high?
A dangerously high hemoglobin level is typically considered to be above:
- 18 g/dL in adult males.
- 16.5 g/dL in adult females.
These levels can significantly increase blood viscosity (thickness), making blood flow more difficult and increasing the risk of complications like:
- Blood clots (thrombosis): Thick blood is more likely to form clots in arteries and veins, which can lead to serious conditions like deep vein thrombosis (DVT), pulmonary embolism (PE), heart attack, or stroke.
- Organ damage: Reduced blood flow due to thickened blood can impair oxygen delivery to vital organs like the heart, kidneys, and brain, potentially causing damage.
Does drinking a lot of water help polycythemia?
While staying adequately hydrated is generally important for overall health, including for individuals with polycythemia vera (PV), drinking a lot of water specifically to lower red blood cell count is not an effective or recommended approach. Overhydration can lead to electrolyte imbalances, which can be harmful and require medical attention.
Is PV fatal?
While PV itself is not directly fatal, it can be a serious condition and requires ongoing management to prevent complications.
Can PV cause high blood pressure?
Yes, polycythemia vera (PV) can contribute to high blood pressure (hypertension) due to the following reasons:
- Increased blood viscosity: PV leads to an abnormally elevated red blood cell count, making the blood thicker and more viscous. This thicker blood encounters greater resistance as it flows through blood vessels, similar to trying to push syrup through a straw compared to water. This increased resistance can elevate blood pressure.
- Interference with blood vessel function: PV can also impair the ability of blood vessels to relax and dilate, which naturally helps to regulate blood pressure. This can further contribute to hypertension.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- https://mpn-hub.com/medical-information/international-consensus-classification-2022-for-myeloproliferative-neoplasms
- Gianelli U, Thiele J, Orazi A, Gangat N, Vannucchi AM, Tefferi A, Kvasnicka HM. International Consensus Classification of myeloid and lymphoid neoplasms: myeloproliferative neoplasms. Virchows Arch. 2023 Jan;482(1):53-68. doi: 10.1007/s00428-022-03480-8. Epub 2022 Dec 29. PMID: 36580136; PMCID: PMC9852206.
- Madden C. THE PROACTIVE APPROACH TO POLYCYTHEMIA VERA: Essential Strategies For Patients, Caregivers, And Healthcare Professionals – Navigating Diagnosis, Treatment, And Practical Coping Strategies
- Goldberg S, Hoffman J. Clinical Hematology Made Ridiculously Simple, 1st Edition: An Incredibly Easy Way to Learn for Medical, Nursing, PA Students, and General Practitioners (MedMaster Medical Books). 2021.
- Keohane EM, Otto CN, Walenga JM. Rodak’s Hematology 6th Edition (Saunders). 2019.