What is hematology?
Hematology is the branch of medicine dedicated to the study of blood, blood-forming organs, and blood-related disorders. This encompasses a vast spectrum, from understanding the composition and function of blood cells to diagnosing and managing diseases of the blood and bone marrow.
Here’s a breakdown of its key aspects:
Scope
- Diagnosis and treatment: Hematologists diagnose and manage various blood disorders, including anemias, leukemias, lymphomas, myelomas, bleeding disorders, and more.
- Blood component therapy: This involves the transfusion of red blood cells, platelets, plasma, or other blood components to patients in need.
- Bone marrow transplantation: Hematologists play a crucial role in performing and managing bone marrow transplants for various conditions.
- Hematologic malignancies: They specialize in managing cancers of the blood and bone marrow, such as leukemias and lymphomas.
Focus
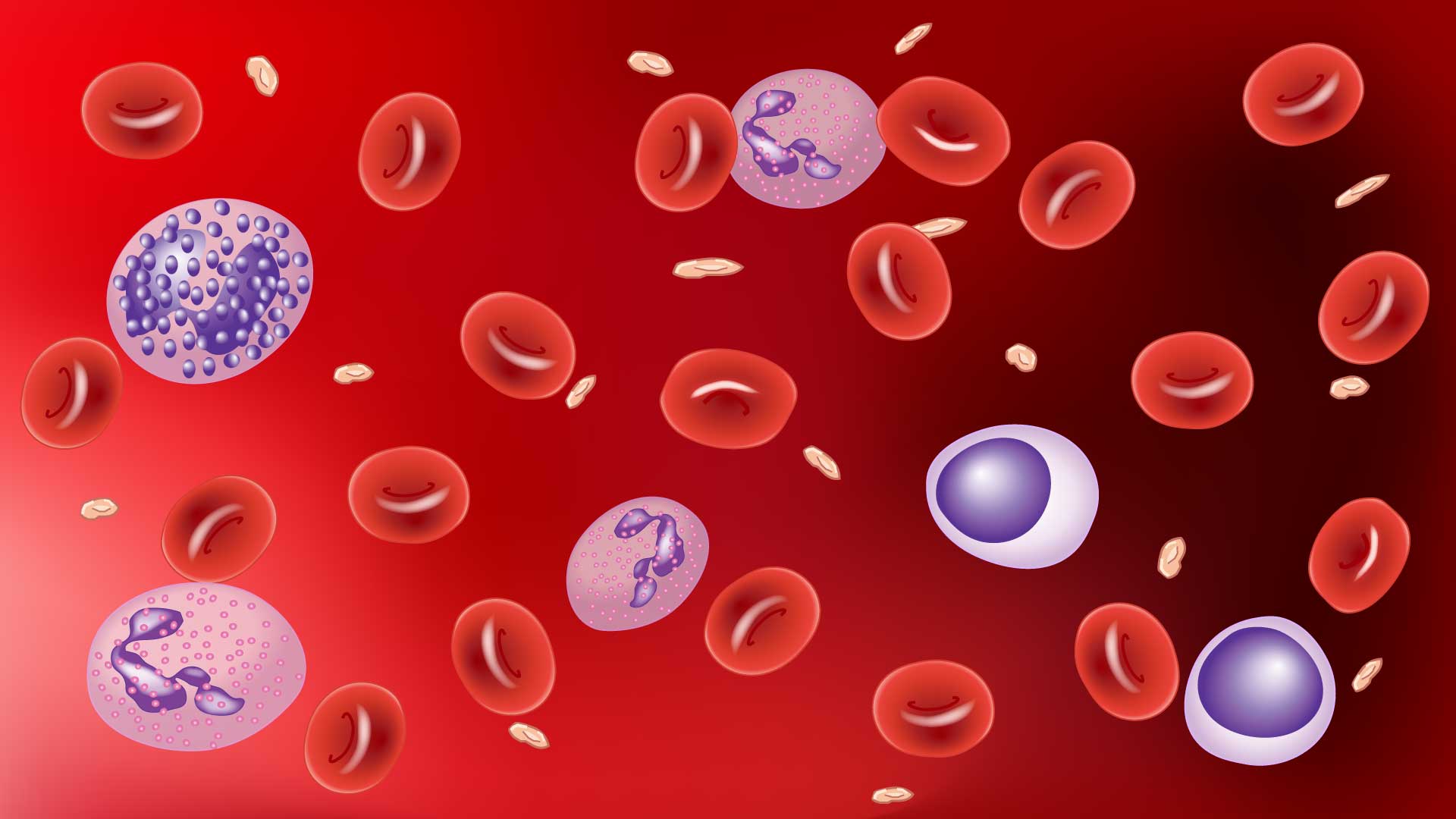
- Blood composition: Hematology delves into the different components of blood, including plasma, red blood cells, white blood cells, and platelets, and their respective functions.
- Blood cell function: It explores the diverse roles of various white blood cells in immunity, red blood cells in oxygen transport, and platelets in clotting.
- Hematopoiesis: This fascinating process within bone marrow, where stem cells differentiate into mature blood cells, is thoroughly studied in hematology.
- Bone marrow environment: The article can analyze the specialized microenvironment within the bone marrow that supports healthy blood cell production.
Why is hematology important?
Hematology plays a critical role in various aspects of clinical practice, impacting the diagnosis, management, and treatment of a wide range of medical conditions. Here’s a closer look at its significance:
Diagnosis and Management of Blood Disorders
Hematologists are experts in diagnosing and managing a wide range of blood disorders, including:
- Anemias: Conditions characterized by low red blood cell count or abnormal function, leading to fatigue, weakness, and other symptoms.
- Leukemias: Cancers of the white blood cells, affecting their production and function, leading to infections, fatigue, and other complications.
- Lymphomas: Cancers of the lymphatic system, including Hodgkin’s lymphoma and non-Hodgkin’s lymphoma, causing fatigue, weight loss, and swollen lymph nodes.
- Myelomas: Cancers of plasma cells, a type of white blood cell, leading to bone pain, kidney damage, and other issues.
- Bleeding disorders: Conditions like hemophilia or von Willebrand disease, causing excessive bleeding due to problems with clotting factors.
By analyzing blood tests, bone marrow biopsies, and other diagnostic tools, hematologists can accurately identify the specific blood disorder and develop personalized treatment plans.
Guiding Treatment Decisions in Various Medical Conditions
Hematological findings are often crucial in guiding treatment decisions across various medical specialties. For example:
- Infectious diseases: Blood tests can reveal the presence and type of infection, aiding in selecting appropriate antibiotics or other therapies.
- Autoimmune diseases: Hematological abnormalities can be indicative of autoimmune disorders like lupus or rheumatoid arthritis, influencing treatment strategies.
- Cardiovascular diseases: Altered blood cell counts or clotting function can contribute to heart disease risk, informing preventive or therapeutic measures.
- Cancer management: Blood tests monitor treatment response and detect potential complications in various cancers beyond hematologic malignancies.
Therefore, hematology plays a supporting role in diverse medical fields, providing valuable insights for clinicians across various specialties.
Blood Transfusion and Component Therapy

Blood transfusion is an essential component in hematology. Hematologists are responsible for ensuring the safe and effective use of blood products in transfusions and component therapy. This involves:
- Blood typing and compatibility testing: Matching donor blood with recipient blood type to prevent transfusion reactions.
- Collection, processing, and storage of blood products: Ensuring the safety and quality of blood components like red blood cells, platelets, and plasma.
- Transfusion protocols and monitoring: Administering blood products safely and effectively while monitoring for potential complications.
Hematology expertise ensures that patients receive the appropriate blood products they need, significantly impacting their treatment outcomes and survival.
Bone Marrow Transplantation
Hematologists play a pivotal role in bone marrow transplantation, a potentially lifesaving treatment for various conditions like:
- Leukemias: Replacing diseased bone marrow with healthy donor or patient stem cells.
- Severe aplastic anemia: Rebooting the bone marrow with healthy stem cells to restore blood cell production.
- Immune system disorders: Using bone marrow transplantation to treat certain immune deficiencies.
Hematologists manage the entire process, from patient selection and conditioning to transplantation and post-transplant care, ensuring the best possible outcomes.
Development of New Therapies and Improving Patient Care
Hematologists are actively involved in research and development of new diagnostic tools, treatment strategies, and targeted therapies for various blood disorders. This includes:
- Personalized medicine: Tailoring treatments based on individual genetic and molecular profiles of patients.
- Gene therapy: Introducing healthy genes into patients’ cells to correct genetic defects causing blood disorders.
- Immunotherapy: Harnessing the power of the immune system to fight blood cancers.
By continuously advancing their field, hematologists contribute to improving patient care, survival rates, and overall quality of life for individuals with blood disorders.
Function of Blood
Blood is a complex and dynamic tissue with a multitude of crucial functions that keep us alive and healthy. Let’s delve into the fascinating world of hematology and explore its diverse roles in maintaining our well-being:
Transportation
- Oxygen Delivery: The red blood cells (RBCs), packed with hemoglobin, act as oxygen taxis. They pick up oxygen from the lungs and deliver it to every tissue.
- Nutrient Distribution: Blood transports essential nutrients like glucose, amino acids, and fatty acids absorbed from the digestive system to various tissues for growth, repair, and energy production.
- Waste Removal: Blood also carries waste products like carbon dioxide, a byproduct of cellular respiration, from tissues back to the lungs for exhalation. Additionally, metabolic waste products like urea and creatinine are transported to the kidneys for elimination.
Temperature Regulation
- Blood acts as a mobile heat exchanger, absorbing heat from active muscles and organs and releasing it through the skin’s surface, especially during sweating. This helps maintain our body temperature within a healthy range.
pH Regulation
- Blood acts as a buffer, maintaining a slightly alkaline pH (around 7.4) crucial for various enzymatic reactions and optimal organ function. Special proteins and buffer systems in the blood neutralize acidic waste products and prevent excessive changes in pH.
Immunity
- White blood cells (WBCs) are the body’s defense soldiers, patrolling the bloodstream and tissues for pathogens like bacteria, viruses, and parasites.
Body Fluid Electrolyte Regulation
- Blood maintains the proper balance of electrolytes like sodium, potassium, chloride, and calcium, which are essential for nerve and muscle function, fluid balance, and various other physiological processes.
Toxin Removal
- The liver, a vital organ for detoxification, filters toxins and waste products from the blood. These waste products are then eliminated through the kidneys, intestines, and lungs.
Blood Components
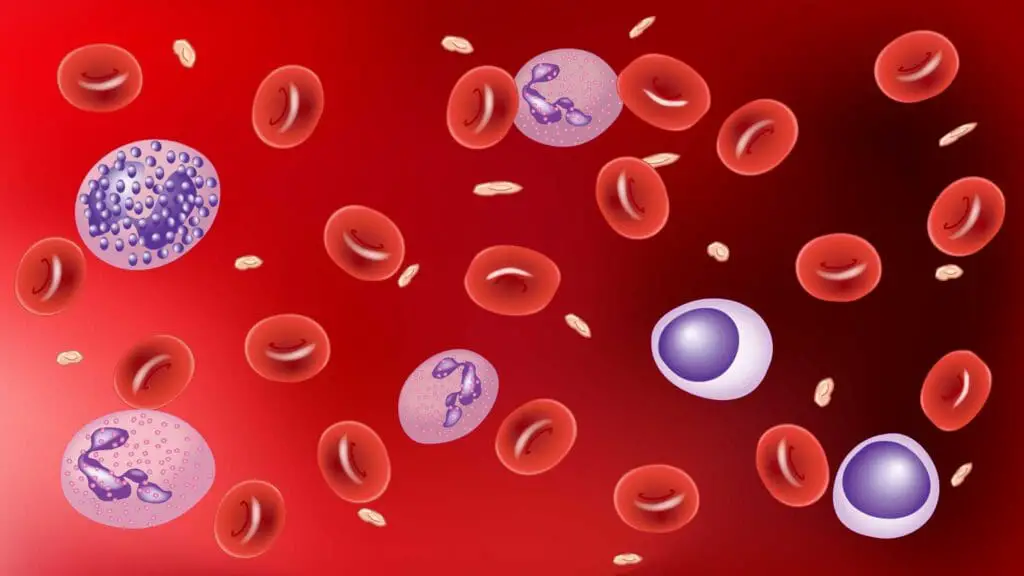
Blood is a complex mixture of cells and fluid, each component playing a crucial role in maintaining our health. Let’s delve into the diverse types of blood cells and their functions, along with the critical role of plasma in this intricate system.
Red Blood Cells (RBCs)
- Function: RBCs are the workhorses of oxygen transport. They contain a protein called hemoglobin, which binds to oxygen in the lungs and delivers it to all tissues in the body. They also carry carbon dioxide, a waste product of cellular respiration, back to the lungs for exhalation.
- Shape and Structure: RBCs are unique in having a biconcave, disc-shaped structure without a nucleus, allowing for maximum surface area for efficient oxygen diffusion. Their small size and flexibility also enable them to easily squeeze through tiny blood vessels.
- Production: RBCs are continuously produced in the bone marrow, primarily regulated by the hormone erythropoietin.
White Blood Cells (WBCs)
- Function: WBCs are the soldiers of our immune system, defending the body against infections, diseases, and foreign invaders. Different types of WBCs have specialized roles in immune defense:
- Neutrophils: These are the most abundant WBCs, acting as the first line of defense against bacteria by engulfing and digesting them (phagocytosis).
- Lymphocytes: These B and T lymphocytes are crucial for adaptive immunity. B cells produce antibodies that target specific pathogens, while T cells directly attack infected cells or regulate the immune response.
- Monocytes: These develop into macrophages that engulf and destroy pathogens, debris, and cancer cells.
- Eosinophils: They fight against parasitic infections and allergies by releasing chemicals that damage parasites and trigger inflammatory responses.
- Basophils: These are involved in allergic reactions by releasing histamine, a chemical that causes vasodilation and inflammation.
- Production: WBCs are produced in the bone marrow and lymphoid organs like the spleen and lymph nodes.
Platelets
- Function: Platelets are tiny, disc-shaped fragments of cells that play a crucial role in blood clotting. They clump together at the site of injury, forming a plug to prevent excessive bleeding.
- Shape and Structure: Platelets lack nuclei but contain granules filled with clotting factors and other chemicals essential for hemostasis.
- Production: Platelets are not actually produced as individual cells, but rather are fragments of much larger cells called megakaryocytes. These megakaryocytes reside and mature in the bone marrow, specifically in the spongy tissue within the core of most bones.
Plasma
- Function: Plasma is the liquid component of blood that makes up about 55% of its total volume. It acts as a transportation medium for various solutes, including:
- Nutrients: Glucose, amino acids, and fatty acids absorbed from the digestive system are transported in plasma to reach tissues for growth and energy production.
- Waste products: Carbon dioxide, urea, and other waste products are carried in plasma to the lungs, kidneys, and other organs for elimination.
- Hormones: Chemical messengers produced by endocrine glands are transported in plasma to target tissues and regulate various bodily functions.
- Electrolytes: Minerals like sodium, potassium, chloride, and calcium are essential for nerve and muscle function, and their balance is maintained within plasma.
- Proteins: Plasma proteins like albumin help maintain blood volume and pressure, transport various substances, and contribute to blood clotting.
- Immune factors: Antibodies, complement proteins, and other immune system components are present in plasma to fight infections.
Common Hematological Disorders
Anemias
- Description: A decrease in the number of red blood cells or the amount of hemoglobin in them, leading to reduced oxygen delivery to tissues.
- Presentations: Fatigue, weakness, pale skin, shortness of breath, dizziness, headache, cold hands and feet.
- Types:
- Iron deficiency anemia: Most common type, caused by iron deficiency in the diet or blood loss.
- Vitamin B12 deficiency anemia: Caused by lack of vitamin B12, essential for red blood cell production.
- Hemolytic anemias: Red blood cells are destroyed prematurely due to genetic factors, autoimmune reactions, or infections.
- Aplastic anemia: Bone marrow fails to produce enough blood cells due to various causes.
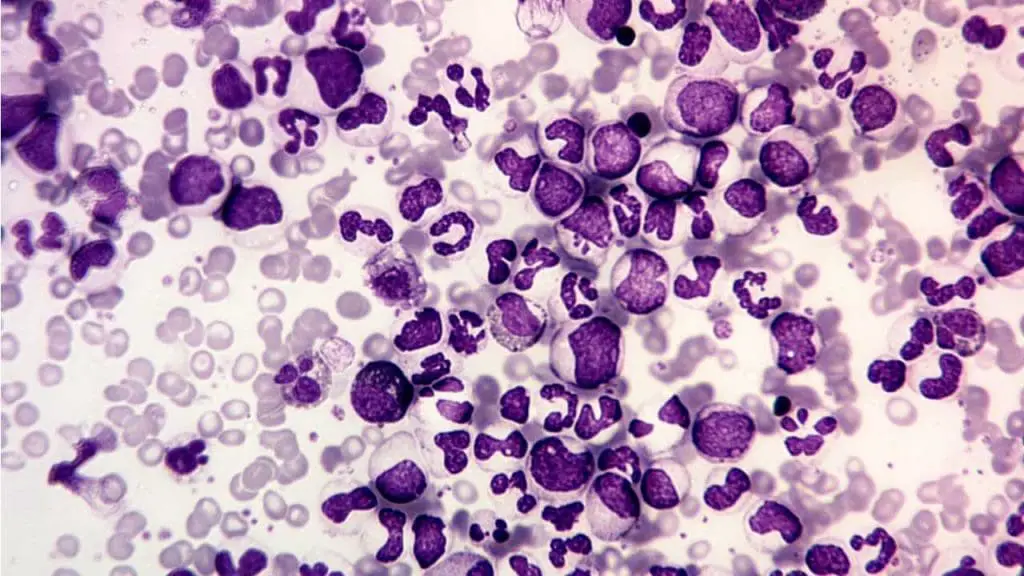
Leukemias
- Description: Cancers of the white blood cells, causing uncontrolled proliferation of abnormal white blood cells.
- Presentations: Fatigue, fever, infections, easy bruising or bleeding, swollen lymph nodes, weight loss, bone pain.
- Types:
- Acute leukemias: Rapidly progressive, requiring immediate treatment.
- Acute lymphoblastic leukemia (ALL): Affects lymphocytes.
- Acute myeloid leukemia (AML): Affects myeloid cells, precursors to various types of white blood cells and red blood cells.
- Chronic leukemias: Slower progression, often with milder symptoms initially.
- Chronic lymphocytic leukemia (CLL): Affects lymphocytes.
- Chronic myeloid leukemia (CML): Affects myeloid progenitor cells.
- Acute leukemias: Rapidly progressive, requiring immediate treatment.
Lymphomas
- Description: Cancers of the lymphatic system, including lymph nodes, spleen, and thymus.
- Presentations: Swollen lymph nodes, fever, night sweats, fatigue, weight loss, itching, chest pain or cough (if lymphoma involves lungs).
- Types:
- Hodgkin’s lymphoma: Characterized by the presence of Reed-Sternberg cells.
- Non-Hodgkin’s lymphoma: Diverse group with various subtypes and presentations.

Myelomas
- Description: Cancers of plasma cells, a type of white blood cell that produce antibodies.
- Presentations: Bone pain, fatigue, fractures, anemia, kidney problems, infections.
Bleeding Disorders
- Description: Conditions causing excessive or prolonged bleeding due to problems with blood clotting factors or platelets.
- Presentations: Easy bruising, frequent nosebleeds, excessive bleeding after injuries or surgery, heavy menstrual bleeding.
- Types:
- Hemophilia: Inherited disorder affecting clotting factors VIII and IX.
- Von Willebrand disease: Most common inherited bleeding disorder, affecting the von Willebrand factor involved in platelet adhesion.
- Thrombocytopenia: Low platelet count, leading to easy bruising and bleeding.
Common Hematological Tests and Its Uses
- Complete Blood Count (CBC): This is the most common hematology test and is used to assess overall health and diagnose a wide range of conditions, including anemia, infection, and leukemia. It measures:
- Red blood cell (RBC) count, hematocrit, and hemoglobin: These tests measure the number and size of red blood cells and the amount of hemoglobin, the protein that carries oxygen in the blood.
- White blood cell (WBC) count and differential: This test measures the total number of white blood cells and the percentage of each type of white blood cell.
- Platelet count: This test measures the number of platelets, which are involved in blood clotting.
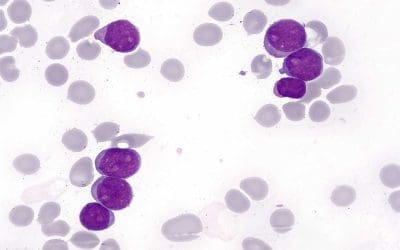
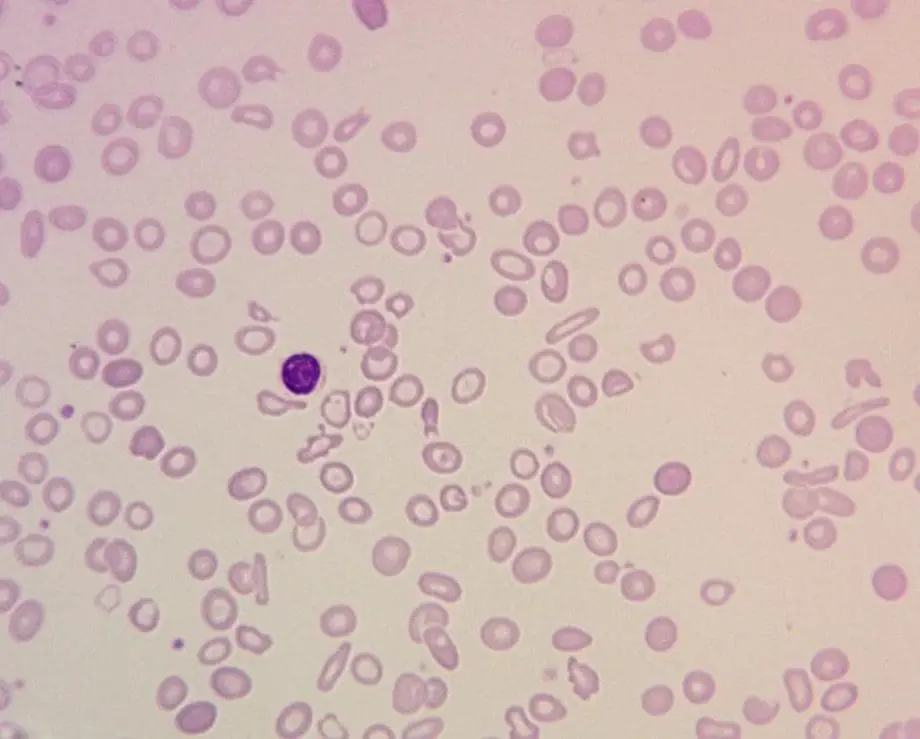
- Peripheral Blood Smear: This test involves examining a thin layer of blood under a microscope to look for abnormalities in the size, shape, and color of red blood cells and white blood cells. It can be used to diagnose anemia, leukemia, and other blood disorders.
- Bone Marrow Biopsy and Aspiration: This test involves removing a small sample of bone marrow from the hip bone and examining it under a microscope. It can be used to diagnose a variety of blood disorders, including leukemia, lymphoma, and aplastic anemia.
- Coagulation Tests: These tests measure the blood’s ability to clot. They are used to diagnose bleeding disorders and to monitor the effectiveness of blood thinners.
- Blood Typing and Rh Factor: This test determines a person’s blood type (A, B, AB, or O) and Rh factor (positive or negative). This information is important for blood transfusions and for determining if a pregnant woman is Rh compatible with her baby.
- Iron Studies: These tests measure the amount of iron in the blood and the body’s ability to store and use iron. They are used to diagnose iron deficiency anemia.
- Vitamin B12 and Folate Levels: These tests measure the levels of vitamin B12 and folate in the blood. Deficiencies in these vitamins can cause anemia.
- Erythrocyte Sedimentation Rate (ESR): This test measures the rate at which red blood cells settle to the bottom of a test tube. It is used to diagnose inflammation, infection, and autoimmune diseases.
These are just a few of the many common hematology tests. The specific tests that are ordered will depend on the patient’s symptoms and medical history.
Hematology-Oncology: The Intersection of Blood and Cancer
Hematology-oncology, often abbreviated as “hem-onc,” is a specialized field that bridges the gap between hematology (study of blood and blood disorders) and oncology (study and treatment of cancer). This crucial area focuses on diagnosing and managing hematological malignancies, which are cancers that arise from the blood, bone marrow, and lymphatic system.
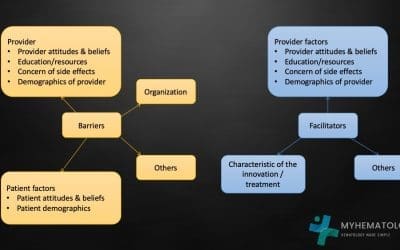
Diagnosis and Treatment
Diagnosing hematological malignancies involves a multi-pronged approach:
- Detailed history and physical examination: Identifying potential risk factors and symptoms like fatigue, weight loss, swollen lymph nodes, bleeding, or bruising.
- Blood tests: Complete blood count, peripheral blood smear, bone marrow biopsy and aspiration, flow cytometry, and molecular analysis to identify specific genetic mutations.
- Imaging tests: X-rays, CT scans, PET scans, and MRIs to assess the extent of the cancer and involvement of other organs.
Treatment options depend on the specific type of malignancy, its stage, and individual patient factors. Key modalities include:
- Chemotherapy: Uses powerful drugs to kill cancer cells. Can be administered intravenously, orally, or topically.
- Radiation therapy: Uses high-energy beams to target and destroy cancer cells. Can be delivered externally or internally through brachytherapy.
- Stem cell transplantation: Replaces diseased bone marrow with healthy stem cells from a donor or the patient (autologous transplant).
Emerging Therapies and Future Directions
The field of hematology-oncology is constantly evolving, with exciting new therapies on the horizon:
- Targeted therapy: Drugs that specifically target cancer cells’ vulnerabilities, reducing side effects compared to traditional chemotherapy.
- Immunotherapy: Harnessing the body’s own immune system to fight cancer, with promising developments in CAR T-cell therapy.
- Gene therapy: Addressing underlying genetic mutations that cause cancer, offering potential cures for specific malignancies.
- Precision medicine: Tailoring treatments based on individual genetic and molecular profiles of each patient’s cancer.
Frequently Asked Questions (FAQs)
What does hematology check for?
Hematology checks for a broad range of things related to the blood, blood cells, and bone marrow. Here’s a breakdown of the key areas it investigates:
1. Blood cell counts and function
- Red blood cells (RBCs): Hematology checks for the number, size, and shape of RBCs, as well as their hemoglobin content. This helps diagnose anemia, infections, and other conditions affecting oxygen delivery.
- White blood cells (WBCs): Hematology analyzes the total WBC count and the individual types of WBCs (neutrophils, lymphocytes, monocytes, eosinophils, basophils). This helps diagnose infections, immune disorders, and leukemias.
- Platelets: Hematology checks the platelet count and function, which is crucial for blood clotting and preventing excessive bleeding.
2. Blood disorders and abnormalities
- Anemia: Hematology identifies various types of anemia (iron deficiency, vitamin B12 deficiency, hemolytic) by analyzing red blood cell characteristics and other factors.
- Leukemias: Blood tests and bone marrow examination help diagnose different types of leukemias (acute or chronic, lymphocytic or myeloid) based on abnormal white blood cell characteristics.
- Lymphomas: Hematology helps identify Hodgkin’s and non-Hodgkin’s lymphomas through enlarged lymph nodes, blood tests, and sometimes bone marrow biopsies.
- Myelomas: Abnormal plasma cells in the bone marrow, detected through blood tests and bone marrow examination, indicate myeloma.
- Bleeding disorders: Hematology investigates conditions like hemophilia or von Willebrand disease by analyzing clotting factors and platelet function.
3. Bone marrow health and function
- Bone marrow biopsy and aspiration: These procedures allow direct examination of bone marrow cells, helping diagnose various blood disorders, infections, and even some cancers.
- Stem cell evaluation: Hematology assesses the number and function of stem cells in the bone marrow, which are crucial for blood cell production.
4. Other blood-related issues
- Infections: Hematology tests like WBC count and differential can help identify and categorize infections based on the type of white blood cells involved.
- Immune system disorders: Abnormal white blood cell counts or function can indicate autoimmune diseases or other immune system issues.
- Nutritional deficiencies: Hematology tests can reveal deficiencies in iron, vitamin B12, or other nutrients that can affect blood cell production.
Why would a doctor refer you to hematology?
There are several reasons why a doctor might refer you to a hematologist, a specialist in blood disorders. Here are some of the most common:
1. Abnormal blood test results
- Complete Blood Count (CBC) issues: Low red blood cell count (anemia), low white blood cell count (leukopenia), high white blood cell count (leukocytosis), low platelet count (thrombocytopenia), abnormal size or shape of blood cells.
- Other blood tests: Abnormal clotting tests, high or low iron levels, abnormal vitamin B12 or folate levels, positive blood tests for specific diseases like lupus.
2. Symptoms suggestive of blood disorders
- Fatigue, paleness, shortness of breath (anemia)
- Frequent infections, fever, night sweats (immunodeficiency)
- Easy bruising or bleeding (bleeding disorder)
- Enlarged lymph nodes, bone pain, weight loss (lymphoma)
- Unexplained pain, fatigue, feeling unwell (various blood disorders)
3. Suspected blood disorder based on other medical conditions
- Certain autoimmune diseases that can affect blood cells (lupus, rheumatoid arthritis)
- Some cancers that can spread to the bone marrow
- Kidney disease affecting red blood cell production
4. Need for specialized treatment or consultation
- If you have a complex or rare blood disorder requiring expert management.
- If you need specialized treatments like chemotherapy, radiation therapy, or stem cell transplantation.
- If you are considering clinical trials for new blood disorder treatments.
5. Pregnancy-related concerns
- If you have a blood disorder that could affect your pregnancy or your baby’s health.
- If you have abnormal blood test results during pregnancy.
Is hematology related to cancer?
Hematology is partially related to cancer, but it’s important to understand the specific connection:
Hematology: This medical specialty focuses on the study, diagnosis, and treatment of blood, blood cells, and bone marrow. This includes various disorders and diseases affecting these components.
Cancer: This is a broad term encompassing uncontrolled cell growth that can affect any organ or tissue in the body. While not all cancers involve the blood, a significant portion of them do:
- Hematological malignancies: These are cancers of the blood, bone marrow, and lymphatic system. They are directly within the domain of hematology. Examples include leukemias, lymphomas, myelomas, and some types of sarcomas.
- Solid tumors: These cancers affect solid organs like lungs, breasts, or colon. While not directly studied by hematologists, they might involve blood tests for evaluation or side effects impacting the blood. Additionally, some treatments like chemotherapy or stem cell transplantation, often managed by hematologists, might be used for these cancers.
Therefore, hematology plays a crucial role in diagnosing, treating, and managing hematological malignancies, but it’s not solely focused on cancer. It encompasses a wider range of blood-related disorders, including non-cancerous conditions like anemia, bleeding disorders, and immune system issues.
What is the difference between a hematologist and a hematopathologist?
While both hematologists and hematopathologists specialize in blood-related conditions, they have distinct roles within the field:
Hematologist
- Clinical focus: Primarily patient-facing doctors who diagnose and treat blood disorders, including
- Hematological malignancies: Leukemias, lymphomas, myelomas, etc.
- Non-malignant conditions: Anemias, bleeding disorders, immune system problems, etc.
- Training: Completes internal medicine or pediatrics residency followed by a fellowship in hematology.
- Responsibilities:
- Conducts patient consultations and physical examinations.
- Orders and interprets blood tests, bone marrow biopsies, and other diagnostic tests.
- Develops and manages treatment plans, including chemotherapy, radiation therapy, and stem cell transplantation.
- Provides ongoing care and monitors patients’ progress.
Hematologist-Pathologist (Hematopathologist)
- Laboratory focus: Primarily analyze blood, bone marrow, and tissues under a microscope to diagnose disorders.
- Specialize in diagnosing blood cancers and other hematological malignancies through microscopic examination.
- May also provide expert opinion on non-malignant blood disorders.
- Training: Completes a pathology residency after medical school and then pursues additional subspecialty training in hematopathology.
- Responsibilities:
- Examines slides of blood, bone marrow, and tissue samples using microscopes and other specialized techniques.
- Analyzes cell morphology, immunophenotyping, and other characteristics to identify abnormalities.
- Provides written reports to clinicians that are crucial for diagnosis and treatment decisions.
- May participate in research and clinical trials related to hematological diseases.
Key Differences
- Patient interaction: Hematologists interact directly with patients, while hematopathologists primarily work in the laboratory.
- Primary role: Hematologists diagnose and manage, while hematopathologists diagnose through microscopic analysis.
- Training: Hematologists have clinical training, while hematopathologists have combined clinical and laboratory training.
Collaboration
Both specialists closely collaborate in managing blood disorders. Hematologists rely on hematopathologists’ expertise for accurate diagnosis, particularly in complex cases, and to inform treatment decisions. Conversely, hematopathologists depend on clinical information from hematologists to understand the patient’s context and provide the most relevant diagnosis.
Is a hematologist the same as an oncologist?
No, a hematologist is not the same as an oncologist, although their fields do overlap in some ways. Here’s a breakdown of their key differences:
Specialization
- Hematologist: Focuses specifically on blood, bone marrow, and the lymphatic system, dealing with both cancerous (hematological malignancies like leukemias and lymphomas) and non-cancerous conditions (anemias, bleeding disorders, etc.).
- Oncologist: Deals with cancers affecting various organs and tissues throughout the body, including solid tumors like lung cancer and breast cancer, and other types like brain tumors and sarcomas.
Training
- Hematologist: Completes residency followed by a fellowship in hematology.
- Oncologist: Completes followed by a fellowship in a specific oncology subspecialty, such as medical oncology, surgical oncology, or radiation oncology.
Scope of Practice
- Hematologist: Diagnoses and treats a wide range of blood disorders, including both cancerous and non-cancerous conditions.
- Oncologist: Primarily manages various cancers, focusing on specific treatment modalities like surgery, chemotherapy, radiation therapy, and targeted therapies.
Overlap
- Hematological malignancies: Both hematologists and oncologists may be involved in managing blood cancers, but hematologists often take the lead due to their deeper expertise in these specific diseases.
- Treatment modalities: Both may utilize chemotherapy, radiation therapy, and stem cell transplantation, depending on the cancer type and overall management plan.
Collaboration
Hematologists and oncologists often work together for optimal patient care, especially in cases of blood cancers:
- Hematologists: Provide expertise in diagnosing and managing blood cancers.
- Oncologists: Offer expertise in specific treatment modalities like chemotherapy or radiation therapy.
In summary
- Think of a hematologist as a specialist for blood and its disorders, both cancerous and non-cancerous.
- Think of an oncologist as a specialist for cancers affecting various organs and tissues throughout the body.
Both play crucial roles in diagnosing and treating different types of cancers, sometimes collaborating for patient care, particularly in cases of blood cancers.
What is the difference between benign blood disorders and common blood cancers?
Benign blood disorders and common blood cancers, despite both affecting the blood, are distinct entities with significant differences.
Nature
- Benign blood disorders: These are non-cancerous conditions, meaning the cells involved do not grow uncontrollably or spread to other parts of the body. They can arise from various factors like genetic mutations, nutritional deficiencies, infections, or autoimmune reactions.
- Common blood cancers: These are malignancies involving the uncontrolled growth of abnormal blood cells or cells in the bone marrow and lymphatic system. These abnormal cells can crowd out healthy cells and potentially spread to other organs, causing significant health problems.
Examples
- Benign blood disorders
- Anemia (various types like iron deficiency, vitamin B12 deficiency, hemolytic)
- Thrombocytopenia (low platelet count)
- Sickle cell disease
- Hemophilia
- Common blood cancers
- Leukemias (acute lymphocytic leukemia, acute myeloid leukemia, chronic lymphocytic leukemia, chronic myeloid leukemia)
- Lymphomas (Hodgkin’s lymphoma, non-Hodgkin’s lymphoma)
- Myelomas (multiple myeloma)
Symptoms
- Benign blood disorders: Symptoms can vary depending on the specific condition but may include fatigue, weakness, dizziness, easy bruising or bleeding, pale skin, or shortness of breath.
- Common blood cancers: Similar symptoms are often present, but additional signs like fever, night sweats, swollen lymph nodes, weight loss, bone pain, and persistent infections can occur.
Treatment
- Benign blood disorders: Treatment depends on the specific cause and may involve addressing underlying conditions, lifestyle changes, medication, or blood transfusions.
- Common blood cancers: Treatment usually involves chemotherapy, radiation therapy, targeted therapies, immunotherapy, or stem cell transplantation, depending on the type and stage of the cancer.
Prognosis
- Benign blood disorders: Prognosis is generally good with proper management and often involves long-term control of the condition.
- Common blood cancers: Prognosis varies depending on the type and stage of the cancer, along with treatment response and individual factors. Some cancers are highly curable, while others may require long-term management or supportive care.
In summary
- Benign blood disorders: Non-cancerous, diverse conditions manageable with appropriate interventions.
- Common blood cancers: Malignant growths with potential for spread and requiring specific cancer treatments.
Both conditions require proper medical attention and diagnosis to determine the optimal approach for management and improving patient outcomes.
What should I expect from my appointment with my hematologist?
What you can expect from your appointment with a hematologist depends on several factors, including the reason for the referral and your medical history. However, here’s a general overview of what you might encounter:
The reason for your appointment
- First appointment: If it’s your first time seeing a hematologist, expect a detailed medical history review, including symptoms, past diagnoses, and medications. The doctor may also ask about family history of blood disorders.
- Follow-up appointment: If you’re already being treated for a blood disorder, the focus will be on monitoring progress, discussing any new symptoms or side effects, and adjusting treatment plans as needed.
The type of blood disorder you have
- Non-cancerous conditions: If you have a benign blood disorder like anemia or bleeding disorder, the appointment might involve a physical exam, blood tests, and potentially other diagnostic tests.
- Blood cancers: If you’re suspected of having or already diagnosed with a blood cancer, the appointment might involve more extensive diagnostic tests like bone marrow biopsies, imaging scans, and more detailed blood analyses.
Here’s a general overview of what you can expect:
Before the appointment
- Gather your medical records: Bring copies of any relevant medical records, including blood test results, imaging scans, and doctor’s notes.
- Make a list of questions: Write down any questions or concerns you have about your blood disorder, treatment options, or overall health.
- Prepare a brief timeline: Create a timeline of your symptoms and any events that might be relevant to your blood disorder.
During the appointment
- Discussion and history review: The hematologist will likely ask detailed questions about your symptoms, medical history, family history, lifestyle habits, and any medications you are taking.
- Physical examination: This may involve a general examination and potentially checking for specific signs like swollen lymph nodes, enlarged spleen, or paleness.
- Diagnostic tests: Depending on your situation, the hematologist may order various blood tests like Complete Blood Count (CBC), bone marrow biopsies, imaging scans, or other relevant tests to understand your blood health better.
- Diagnosis and treatment discussion: Based on the collected information, the hematologist will discuss their diagnosis, if available, and explain the next steps, which could include further tests, specific treatment plans, or referrals to other specialists.
- Q&A session: Take this opportunity to ask any questions you might have about your condition, treatment options, potential side effects, and prognosis.
After the appointment
- Review any information: Ask the doctor for any written instructions or information about your blood disorder and treatment plan.
- Schedule follow-up appointments: Make sure you schedule any necessary follow-up appointments as instructed by the doctor.
- Ask questions: If you have any questions after the appointment, don’t hesitate to call the doctor’s office.
It’s important to remember that each appointment is unique and the specific details will vary depending on your individual situation. However, by understanding the general flow of a hematologist appointment and preparing beforehand, you can feel more informed and comfortable during your visit.
What questions should I ask my hematologist?
Here are some questions you might want to ask your hematologist, categorized by different aspects of your condition and concerns:
Diagnosis
- What are the possible causes of my symptoms?
- What tests are needed to confirm the diagnosis?
- How long will it take to get the results?
- What does the diagnosis mean for my overall health?
Treatment
- What are the different treatment options available for my condition?
- What are the potential benefits and risks of each treatment?
- What are the side effects I can expect?
- How long will the treatment last?
- What will happen if I don’t receive treatment?
Prognosis
- What is the long-term outlook for my condition?
- What are the chances of remission or cure?
- What can I expect in terms of managing the condition?
- What resources or support groups are available for me?
Living with the condition
- What lifestyle changes can I make to manage my condition?
- What dietary restrictions or recommendations do you have?
- How can I monitor my symptoms at home?
- When should I contact you or seek medical attention?
- What are the potential complications I should be aware of?
Additional questions
- How often will I need to see you for follow-up appointments?
- What should I do if I have any new symptoms or concerns?
- Are there any clinical trials or research studies relevant to my condition that I could participate in?
- Are there any specific brochures or information leaflets you recommend I read?
Remember, these are just suggestions, and the best questions to ask will depend on your specific situation. Don’t hesitate to write down your questions beforehand and bring them to your appointment. It’s also important to be open and honest with your hematologist and express any concerns or anxieties you may have.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.