TL;DR
Hemophilia is an inherited coagulation disorder caused by mutations on factor VIII gene leading to deficiency in plasma factor VIII for hemophilia A while mutations on factor IX gene for hemophilia B causes decreased factor IX. It is an X-linked recessive disorder.
Clinical features ▾
- Joint and soft tissue bleeds
- Excessive bruising
- Recurrent painful hemarthrosis and muscle hematomas may lead to progressive joint deformity and disability if poorly treated
Laboratory diagnosis ▾
- Abnormal: APTT, factor VIII clotting assay
- Normal: bleeding time, PT
- Positive mutation analysis
- Positive family history
Treatment and Management ▾
- Factor VIII replacement therapy depending on severity
- DDAVP in mild – moderate cases
- Self-treatment prophylactic factor VIII
- Recombinant factor VIIa or FEIBA if high inhibitory antibodies
*Click ▾ for more information
What is hemophilia?
Hemophilia is an inherited coagulation disorder caused by mutations on factor VIII or IX gene leading to deficiency in the respective plasma factors.
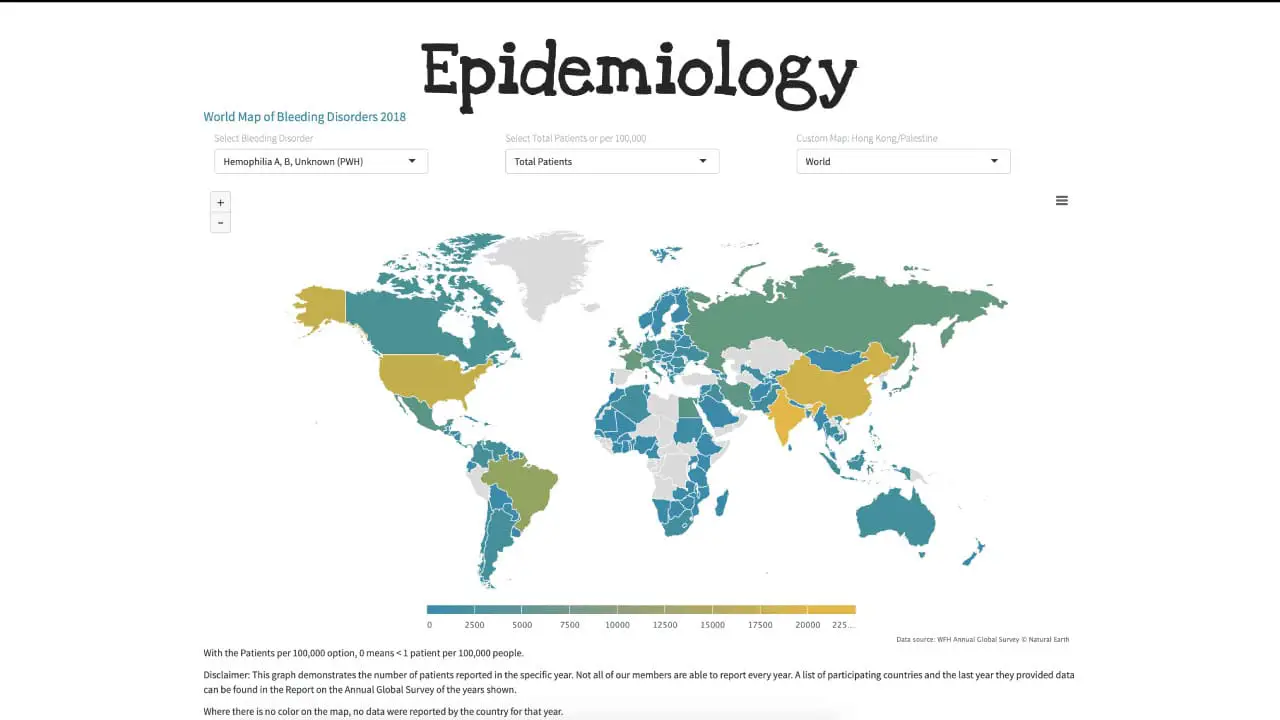
Hemophilia A is the most common of the hereditary clotting factor deficiencies. The prevalence is approximately 30 – 100 per million population and can be found almost all over in the world. The incidence of hemophilia B on the other hand is one-fifth of that of hemophilia A.
Hemophilia A is due to the deficiency in factor VIII while hemophilia B is due to the deficiency in factor IX.
What are the roles of factor VIII and factor IX in the coagulation pathway?
Factor VIII and factor IX are two essential clotting factors that play a key role in the coagulation cascade, the complex process by which blood clots form.
The coagulation cascade is a series of enzymatic reactions that lead to the formation of fibrin, a protein that forms a mesh-like structure that traps blood cells and other proteins, forming a clot.
Factor VIII and factor IX are both serine proteases, which are enzymes that can cleave other proteins. In the coagulation cascade, factor VIII and factor IX work together to activate factor X, another important clotting factor.
Factor VIII is first activated by thrombin, a protease that is generated earlier in the coagulation cascade. Once activated, factor VIII activates factor IX. Activated factor IX then activates factor X.
Activated factor X then activates factor V, and together these two factors activate prothrombin, converting it to thrombin. Thrombin is the most important clotting factor, as it is responsible for both cleaving fibrinogen to form fibrin and activating factor VIII.
In addition to their role in the coagulation cascade, factor VIII and factor IX also play a role in other cellular processes. For example, factor VIII is involved in the adhesion of platelets to blood vessels and the migration of leukocytes to sites of inflammation. Factor IX is involved in the maturation of osteoclasts, cells that are responsible for bone resorption.
Deficiencies in factor VIII or factor IX can lead to bleeding disorders, such as hemophilia A and hemophilia B, respectively. People with hemophilia A or hemophilia B have a decreased ability to form blood clots, which can lead to excessive bleeding.
Causes of hemophilia
Genes encoding factors VIII and IX are both quite closely related on the long arm of the X chromosome, thus both have an X-linked inheritance pattern. About 30% of patients have no family history of abnormal bleeding. In de novo mutation, the gene mutation occurs for the first time in the child. Although hemophilia A can occur in homozygous females, the rare females who bleed abnormally are usually heterozygous carriers of the hemophilia gene. There are variable levels of factor VIII activity in carriers because of random inactivation of X chromosome also known as lyonization.
A wide variety of gene mutations have been identified in hemophilia patients, including missense mutations, nonsense mutations leading to premature termination of translation, frame shifts, deletions, and rearrangements. The most commonly encountered mutation in factor VIII gene is an inversion that reverses the orientation of the 3’ end of the gene relative to the 5’ promoter and transcriptional start site. Alleles bearing this rearrangement, observed in about 50% of severe hemophilia A patients, produce no factor VIII. The great majority of mutations in patients with severe hemophilia A have either inversions, large deletions, nonsense mutations, or frame shifts, all of which do not produce full-length factor VIII. In contrast, those with moderate and mild hemophilia A usually have missense mutations in which full-length protein is produced but has impaired stability or function.
Clinical signs and symptoms of hemophilia
The clinical manifestations of hemophilia vary depending on the severity of the clotting factor deficiency. People with mild hemophilia may have normal blood clotting times and only experience bleeding after surgery or dental work. People with severe hemophilia may have frequent and spontaneous bleeding episodes.
Common clinical manifestations of hemophilia include:
- Easy bruising and bleeding: People with hemophilia bruise easily and may bleed excessively from even minor cuts and injuries. Prolonged bleeding occurs after dental extractions. Operative and post-traumatic hemorrhage are life-threatening.
- Nosebleeds: Nosebleeds are a common problem for people with hemophilia, especially children.
- Heavy menstrual periods: Women with hemophilia may have heavy menstrual periods.
- Bleeding into the joints: Bleeding into the joints, known as hemarthrosis, is a common complication of hemophilia. Patients with repeated joint hemorrhage develop chronic disability due to swelling, deformity, severe pain, limited motion and contractures that can be corrected only by joint replacement.
- Bleeding into the muscles: Bleeding into the muscles, known as hematoma, can also occur in people with hemophilia. Hematomas can be painful and can limit movement.
- Internal bleeding: Internal bleeding can occur anywhere in the body, but it is most common in the digestive tract and urinary tract. Internal bleeding can be serious and life-threatening if not treated promptly.

In addition to these common clinical manifestations, people with hemophilia may also experience:
- Anemia: Anemia is a condition in which the blood does not have enough healthy red blood cells to carry oxygen to the body’s tissues. Anemia can be caused by excessive bleeding in people with hemophilia.
- Arthritis: Arthritis is inflammation of the joints. Arthritis can be caused by repeated bleeding into the joints in people with hemophilia.
- Pseudotumor cerebri: Pseudotumor cerebri is a condition in which the pressure inside the skull increases, but there is no tumor present. Pseudotumor cerebri can be caused by bleeding into the brain in people with hemophilia.
How is hemophilia diagnosed?
Hemophilia is diagnosed based on a medical history, physical examination, and laboratory tests.
Medical history
The doctor will ask questions about the patient’s family history of bleeding disorders, as well as any personal history of bleeding problems.
Physical examination
The doctor will perform a physical examination to look for signs of bleeding, such as bruising, nosebleeds, and bleeding into the joints and muscles.
Laboratory tests
The most important laboratory test for diagnosing hemophilia is the factor VIII or factor IX assay, which measures the level of factor VIII or factor IX in the blood.
Other laboratory tests that may be helpful in diagnosing hemophilia include:
- Prothrombin time (PT): This test measures how long it takes for blood to clot. A prolonged PT is a sign of a bleeding disorder, such as hemophilia.
- Normal bleeding and thrombin time.
- Genetic testing: Genetic testing can be used to identify the specific mutation in the gene that codes for the clotting factor that is deficient. This information can be helpful in confirming the diagnosis of hemophilia and in guiding genetic counseling and prenatal testing.
Diagnosis of hemophilia in infants
If a newborn male has a family history of hemophilia A or B, the doctor may recommend a factor VIII or factor IX assay shortly after birth. This is to determine if the infant has inherited the bleeding disorder.
If a newborn male has no family history of hemophilia, but has signs or symptoms of bleeding, such as bruising or bleeding into the joints, the doctor may also recommend a factor VIII or factor IX assay.
Diagnosis of hemophilia in women
Women can be carriers of hemophilia, but they rarely have symptoms of the disorder themselves. However, if a woman has a family history of hemophilia, she may be concerned about passing the disorder on to her children.
If a woman is a known carrier of hemophilia, she may choose to have genetic testing of her fetus during pregnancy. This can be done to determine if the fetus has inherited the bleeding disorder.
Patients are assigned to one of three levels of severity according to plasma levels of the coagulation factors. These levels generally predict the phenotype of the patient. Those with 1% or less of the factor are severe hemophiliacs with an average of 20 – 30 episodes per year of either spontaneous bleeding or excessive bleeding after minor trauma. Patients with 1 – 5% factor levels have moderate hemophilia, whereas individuals with greater than 5% of factor levels generally have bleeding episodes only after trauma or surgery.
Treatment and management of hemophilia
Most patients attend specialized hemophilia centers where there is a multidisciplinary team dedicated to their care.
Bleeding episodes are treated with specific coagulation factor replacement therapy and spontaneous bleeding is usually controlled if the patient’s factor level is raised to 30 – 50% of normal.
Guidelines exist for the plasma level to be achieved for different types of hemorrhage. For major surgery, serious post-traumatic bleeding or when hemorrhage is occurring at a dangerous site, the factor level should be elevated to 100% and then maintained above 50% when acute bleeding has stopped, until healing has occurred.
In hemophilia A, DDAVP or desmopressin provides an alternative means of increasing the plasma factor VIII level in milder hemophiliacs. In hemophilia B, recombinant factor IX and ultrapure plasma derived factor IX are used for treatment.
Complications that are related to hemophilia apart from repetitive hemarthroses include infections of hepatitis B and C and HIV in the plasma-derived factors. The development of AIDS in hemophilia patients enormously complicates their management and for the last 2 decades, has been the leading cause of death among adult patients with severe disease.
A second major complication is the development of antibodies that neutralizes the factors. For example, infusions of factor VIII in patients with high anti-factor VIII antibodies can result in an anamnestic antibody response and they are at very high risk of catastrophic bleeding. In hemophilia B patients who develop high-titer inhibitors to factor IX, they are treated with recombinant activated factor VII.
Frequently Asked Questions (FAQs)
Can a person with hemophilia live a normal life?
Yes, a person with hemophilia can live a normal life. With proper treatment and management, individuals with hemophilia can enjoy many of the same activities and experiences as anyone else.
Advances in medical technology, particularly in the area of blood clotting factor replacement therapy, have significantly improved the quality of life for people with hemophilia. This treatment involves replacing the missing clotting factor in the blood, allowing for better blood clotting and reducing the risk of bleeding episodes.
While there may be certain precautions to take, such as avoiding contact sports or activities that could lead to injuries, individuals with hemophilia can still engage in a wide range of activities, including education, employment, and hobbies.
It’s important to note that the severity of hemophilia can vary, and individual experiences may differ. However, with appropriate care and support, people with hemophilia can lead fulfilling and active lives.
Is hemophilia life threatening?
Hemophilia can be life-threatening if not managed properly. While advancements in treatment have significantly improved the quality of life for individuals with hemophilia, uncontrolled bleeding can lead to serious complications, including:
- Internal bleeding: This can occur in organs like the brain, joints, or muscles, leading to pain, swelling, and even organ damage.
- Hemarthrosis: This is bleeding into the joints, which can cause pain, swelling, and decreased mobility.
- Spontaneous bleeding: This can occur without any apparent injury or trauma.
- Life-threatening bleeding: In severe cases, uncontrolled bleeding can lead to shock or death.
However, with proper treatment, including regular monitoring, medication, and preventative measures, individuals with hemophilia can significantly reduce the risk of serious complications and live long, healthy lives.
Can hemophilia get worse with age?
Yes, hemophilia can get worse with age. While the severity of hemophilia varies from person to person, it is generally considered a lifelong condition. As people age, their bodies may undergo changes that can affect the effectiveness of clotting factor replacement therapy, leading to an increased risk of bleeding episodes.
Additionally, some individuals with hemophilia may develop inhibitors, which are antibodies that interfere with the effectiveness of clotting factor replacement therapy. These inhibitors can make it more difficult to manage hemophilia and may require specialized treatments.
Can hemophiliacs donate blood?
No, individuals with hemophilia cannot donate blood. People with hemophilia often rely on blood products, such as clotting factor concentrates, to manage their condition. Donating blood would reduce the available supply of these essential products.
Is hemophilia a painful condition?
Yes, hemophilia can be a painful condition. Bleeding episodes, particularly into the joints, can cause significant pain, swelling, and stiffness. These symptoms can interfere with daily activities and reduce quality of life.
While advancements in treatment have significantly improved the management of hemophilia, individuals with the condition may still experience pain, especially during periods of active bleeding or joint damage. It’s important to seek prompt medical attention for any pain or discomfort associated with hemophilia.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Saba HI, Roberts HR. Hemostasis and Thrombosis: Practical Guidelines in Clinical Management (Wiley Blackwell). 2014.
- DeLoughery TG. Hemostasis and Thrombosis 4th Edition (Springer). 2019.
- Keohane EM, Otto CN, Walenga JM. Rodak’s Hematology 6th Edition (Saunders). 2019.
- Tiede A, Collins P, Knoebl P, Teitel J, Kessler C, Shima M, Di Minno G, d’Oiron R, Salaj P, Jiménez-Yuste V, Huth-Kühne A, Giangrande P (2020). International recommendations on the diagnosis and treatment of acquired hemophilia A. Haematologica; 105(7). https://doi.org/10.3324/haematol.2019.230771.
- Leebeek FWG, Miesbach W. Gene therapy for hemophilia: a review on clinical benefit, limitations, and remaining issues. Blood (2021) 138 (11): 923–931.
- Berntorp, E., Fischer, K., Hart, D.P. et al. Haemophilia. Nat Rev Dis Primers 7, 45 (2021). https://doi.org/10.1038/s41572-021-00278-x
- Sarmiento Doncel S, Díaz Mosquera GA, Cortes JM, Agudelo Rico C, Meza Cadavid FJ, Peláez RG. Haemophilia A: A Review of Clinical Manifestations, Treatment, Mutations, and the Development of Inhibitors. Hematol Rep. 2023 Feb 16;15(1):130-150. doi: 10.3390/hematolrep15010014. PMID: 36810557; PMCID: PMC9944491.



