Introduction
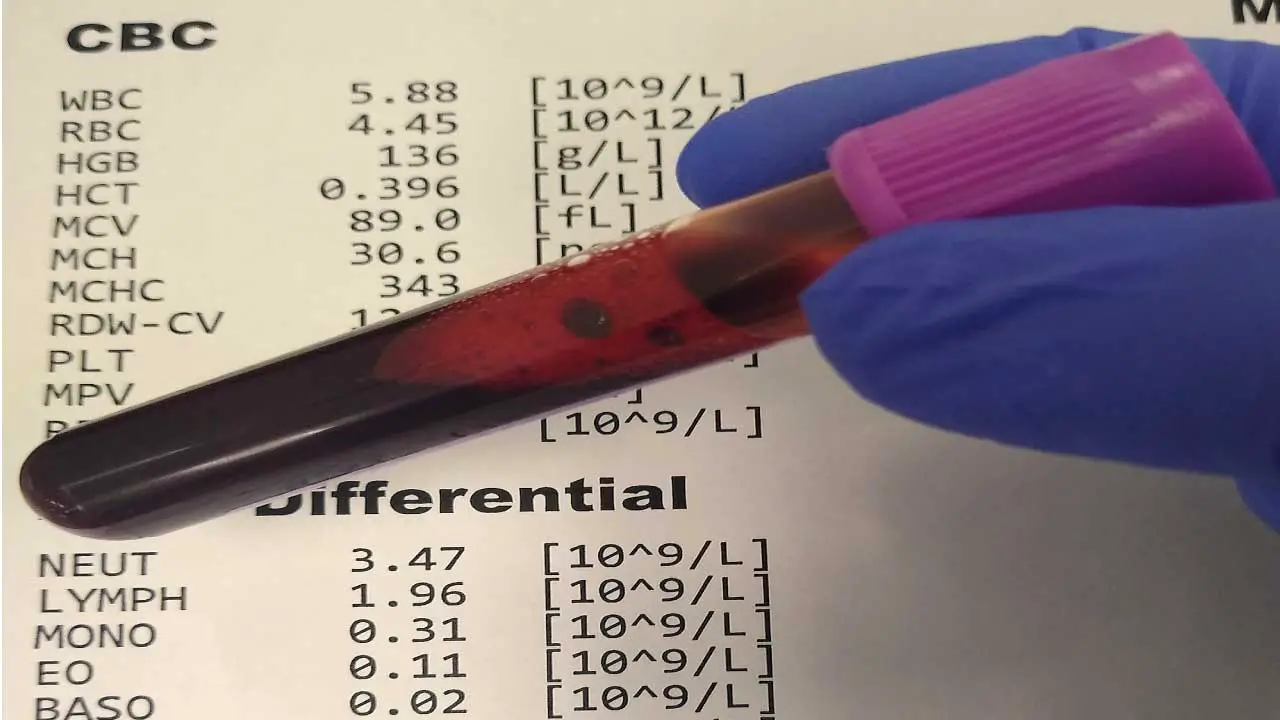
A Complete Blood Count (CBC) with Differential is a common and fundamental blood test that provides a detailed overview of the different types of cells circulating in the blood. It measures the number, size, and characteristics of
- Red Blood Cells (RBCs): Carries oxygen throughout the body.
- White Blood Cells (WBCs): Part of the immune system to fight infection. The “differential” part specifically breaks down the total WBC count into the five main types (neutrophils, lymphocytes, monocytes, eosinophils, and basophils), giving a more precise picture of an individual’s immune status.
- Platelets: Essential for blood clotting.
CBC with differential is used to screen for, diagnose, and monitor a wide range of conditions, including anemia, infections, inflammation, and blood disorders. Changes in blood cell counts can be early indicators of health problems, allowing for timely diagnosis and intervention.
Abnormal values in a CBC with differential can point towards various conditions. It can also be used to monitor the effectiveness of treatment for existing blood disorders.
Reference Ranges & What They Mean
Reference ranges are important because they provide a baseline for interpreting laboratory test results.
By comparing a patient’s test results to the reference range, for example in CBC with differential, healthcare providers can identify any values that fall outside of the normal range. This can help them to diagnose diseases, monitor the effectiveness of treatment, and identify potential complications.
Reference ranges are established by testing a large group of healthy people and determining the range of values that includes 95% of the results. This means that 2.5% of healthy people will have test results that fall outside of the reference range. This does not necessarily mean that they are sick, but it may indicate a need for further testing or evaluation.
Reference ranges can vary depending on a number of factors, including age, sex, race, ethnicity, and pregnancy status. This is why it is important to use a reference range that is appropriate for the patient’s population group.
Reference ranges are an important tool for healthcare providers in the diagnosis and management of hematologic diseases.
Complete Blood Count (CBC) with Differential for Adults
These are the most fundamental tests in hematology, providing a broad overview of the cellular components of blood.
Red Blood Cell (RBC) Parameters
Red blood cells (RBCs) are the workhorses of the oxygen transport system in the body. They carry hemoglobin, a protein that binds oxygen in the lungs and delivers it to tissues throughout the body. The complete blood picture or the CBC with differential evaluates various aspects of RBCs to identify potential issues like anemia or abnormal RBC production.
- RBC Count: This measures the total number of RBCs per microliter of blood in a CBC with differential. A low count can indicate anemia, while a high count may suggest dehydration or certain blood cancers.
- Hemoglobin: This measures the total amount of hemoglobin in the blood, typically expressed in grams per deciliter (g/dL) in a CBC with differential. Low hemoglobin is a hallmark of anemia, potentially caused by iron deficiency, blood loss, or vitamin deficiencies. High hemoglobin can be linked to dehydration or certain blood disorders.
- Hematocrit: This represents the percentage of the blood volume occupied by RBCs. A low hematocrit reflects anemia, while a high hematocrit can suggest dehydration or specific blood conditions.
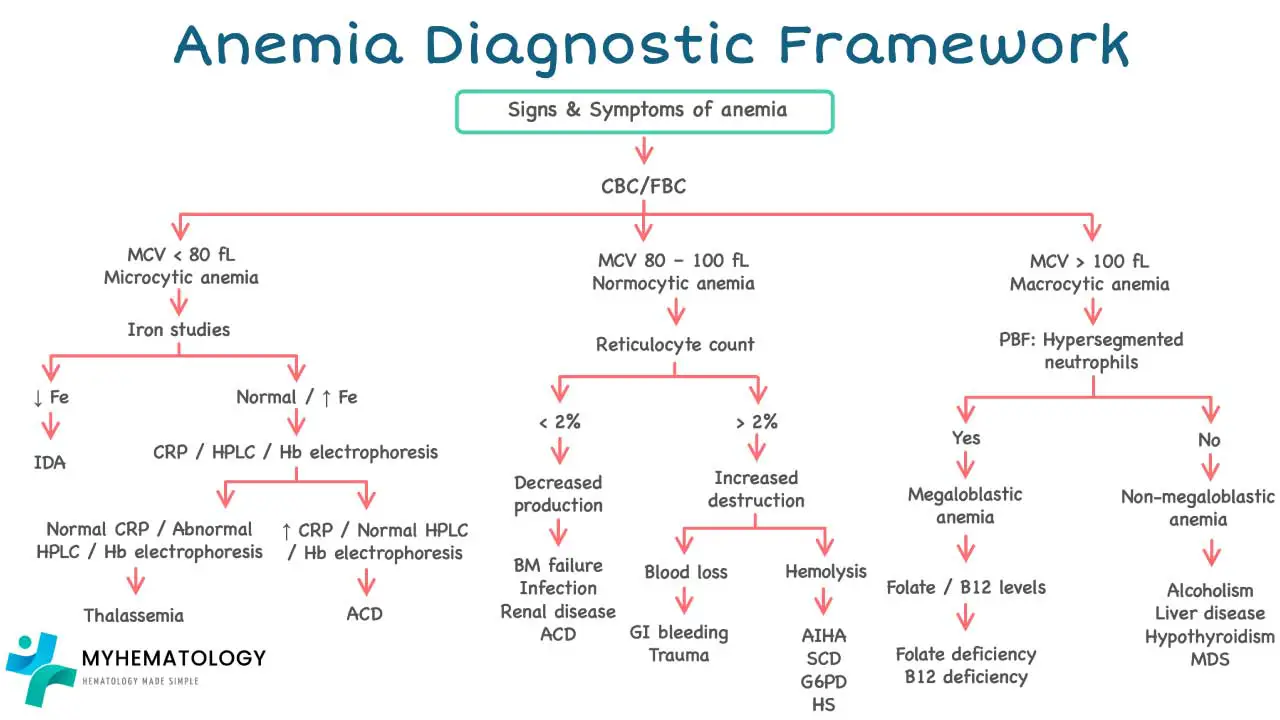
- Mean Corpuscular Volume (MCV): This reflects the average size of RBCs in a CBC with differential.
- Microcytosis (MCV < 80 fL): Suggests small RBCs, potentially indicating iron deficiency anemia.
- Macrocytosis (MCV > 96 fL): Indicates larger RBCs, seen in vitamin B12 deficiency or folate deficiency anemia.
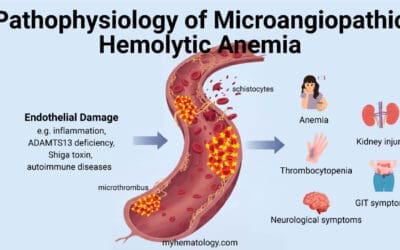
- Normocytic (MCV within normal range): RBC size is normal. Disorders that can be seen with normocytic RBCs but low RBC count include hemolytic anemias.
- Mean Corpuscular Hemoglobin (MCH): This measures the average amount of hemoglobin present in each RBC in a CBC with differential.
- Hypochromia (MCH < 27 pg): Indicates low hemoglobin content per RBC, often seen in iron deficiency anemia.
- Normochromia (MCH within normal range): Hemoglobin content per RBC is normal.
- Mean Corpuscular Hemoglobin Concentration (MCHC): This reflects the concentration of hemoglobin within an RBC in CBC with differential.
- Hypochromia (MCHC < 32 g/dL): Indicates low hemoglobin concentration, often seen in iron deficiency anemia.
- Normochromia (MCHC within normal range): Hemoglobin concentration is normal.
- Red Cell Distribution Width (RDW): This measures the variation in the size of the RBCs in CBC with differential. Increased RDW indicates greater variation in RBC size, potentially suggesting a nutritional deficiency or other blood disorders.
- Reticulocyte Count: This measures the percentage of immature RBCs (reticulocytes) in the blood. The reticulocyte count is important in the CBC with differential as it tells the clinicians how the bone marrow is responding to anemia.
- Increased reticulocyte count: May indicate the body is attempting to increase RBC production in response to anemia.
- Decreased reticulocyte count: May suggest bone marrow suppression, hindering RBC production.
White Blood Cell (WBC) Parameters
- Total WBC Count: This measures the total number of WBCs per microliter (mcL) of blood in CBC with differential.
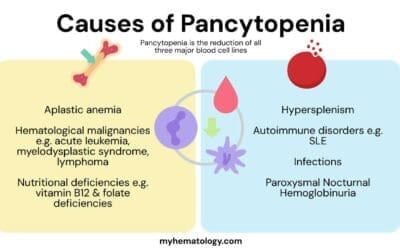
- Elevated WBC count (Leukocytosis): Can indicate infection, inflammation, or certain blood cancers.
- Decreased WBC count (Leukopenia): May suggest bone marrow problems, autoimmune disorders, or viral infections.
- Neutrophils (Reference Range: 40-70%): These are the most abundant WBCs, acting as the body’s first responders against bacterial infections. They engulf and destroy invading bacteria through phagocytosis.
- Lymphocytes (Reference Range: 20-40%): These come in two main types:
- T lymphocytes (T cells): Orchestrate the immune response by coordinating the attack on infected cells and directing other immune cells.
- B lymphocytes (B cells): Produce antibodies, specialized proteins that target and neutralize specific pathogens.
- Increased lymphocytes can suggest a viral infection or immune system activation.
- Monocytes (Reference Range: 2-10%): These are large phagocytic cells that engulf debris from dead cells, bacteria, and other foreign materials. They also play a role in chronic infections and inflammation.
- Eosinophils (Reference Range: 1-4%): These are involved in allergic reactions and parasitic infections. They release chemicals to combat these conditions. Increased eosinophils can indicate allergies or parasitic infections.
- Basophils (Reference Range: 0-1%): These are the least common WBC type and are involved in allergic reactions and inflammatory disorders. They release histamine, a chemical that triggers allergic reactions. Increased basophils can be linked to certain allergic conditions or mast cell disorders.
Platelet Parameters
- Platelet Count (Reference Range): This measures the number of platelets per microliter (mcL) of blood in the CBC with differential.
- Thrombocytosis (Platelet count > 450,000/mcL): An elevated platelet count can increase the risk of blood clots, potentially leading to strokes, heart attacks, or deep vein thrombosis. It may be caused by inflammatory conditions, certain cancers, or iron deficiency.
- Thrombocytopenia (Platelet count < 150,000/mcL): A low platelet count can increase your risk of excessive bleeding, even from minor injuries. It can be caused by various factors, including decreased platelet production, increased platelet destruction, or enlarged spleen trapping platelets.
| Parameters | Male | Female | Unit |
| White blood cell (WBC) Count | 4.1 – 10.34 | 4.3 – 11.68 | x 109/L |
| Red blood cell (RBC) count | 4.44 – 5.97 | 3.89 – 5.25 | x 1012/L |
| Hemoglobin (Hb) level | 13.02 – 17.16 | 11.25 – 15.19 | g/dL |
| Hematocrit | 39.8 – 51.02 | 34.7 – 45.35 | % |
| Mean cell volume (MCV) | 80.72 – 96.93 | 78.63 – 97.22 | fL |
| Mean cell hemoglobin (MCH) | 27.43 – 32.46 | pg | |
| Mean cell hemoglobin concentration (MCHC) | 31.77 – 35.21 | g/dL | |
| Platelet count (PLT) | 155.45 – 389.87 | x 109/L | |
| Red cell distribution width (RDW) | 11.7 – 14.43 | % | |
| Neutrophil count (NEUT#) | 1.87 – 6.92 | 1.94 – 7.44 | x 109/L |
| Lymphocyte count (LYMPH#) | 1.15 – 3.77 | x 109/L | |
| Monocyte count (MONO#) | 0.22 – 0.84 | x 109/L | |
| Eosinophil count (EO#) | 0.04 – 0.65 | x 109/L | |
| Basophil count (BASO#) | 0.01 – 0.1 | x 109/L | |
| NEUT%* | 40.86 – 72.08 | % | |
| LYMPH% | 19.94 – 47.59 | % | |
| MONO% | 4.03 – 11.8 | % | |
| EO% | 0.55 – 8.59 | % | |
| BASO% | 0.13 – 1.73 | % | |
| Reticulocyte count (RET#) | 35.75 – 107.5 | x 109/L | |
| RET% | 0.48 – 2.07 | % |
Other Common Hematology Tests
Erythrocyte sedimentation rate (ESR)
The Erythrocyte Sedimentation Rate (ESR) is a simple and inexpensive blood test that measures the rate at which red blood cells (RBCs) settle at the bottom of a test tube over a period of time. While not a specific diagnostic tool, an elevated ESR can be a valuable indicator of inflammation or other underlying conditions in the body.
ESR is used as complementary to CBC with differential to provide a more comprehensive picture, helping clinicians differentiate between various conditions and monitor disease progression or treatment effectiveness.
| Parameter | Male | Female | Unit |
| 17 – 50 yr | 1 – 7 | 3 – 9 | mm/hr |
| 51- 60 yr | 2 – 10 | 5 – 15 | mm/hr |
Coagulation profile
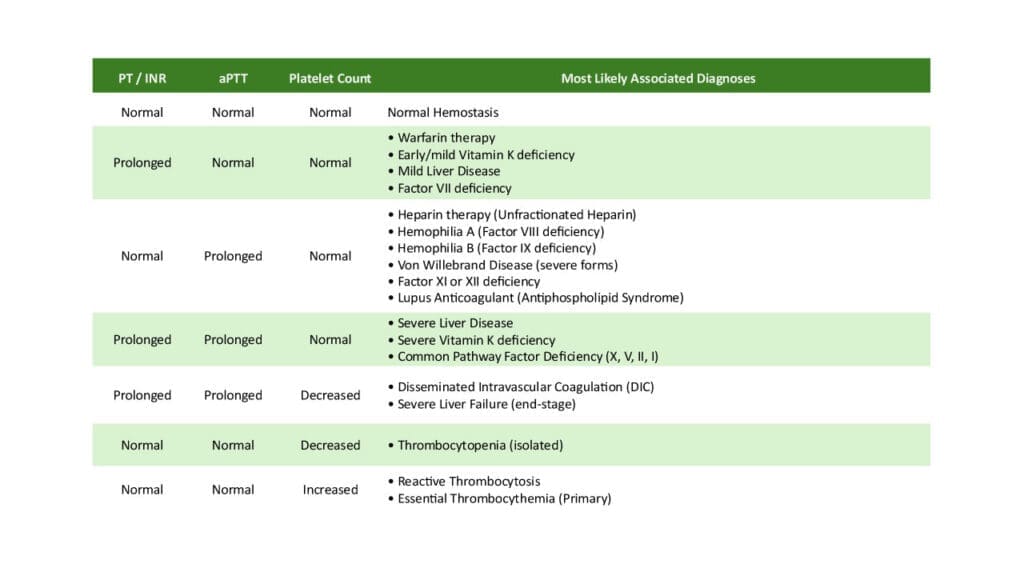
CBC with differential identifies quantitative and qualitative issues with blood cells, including the number of platelets, while the coagulation profile evaluates the function of the complex system that forms blood clots. They are often used in tandem to pinpoint the exact nature of a bleeding or clotting problem and to monitor underlying diseases or responses to treatment.
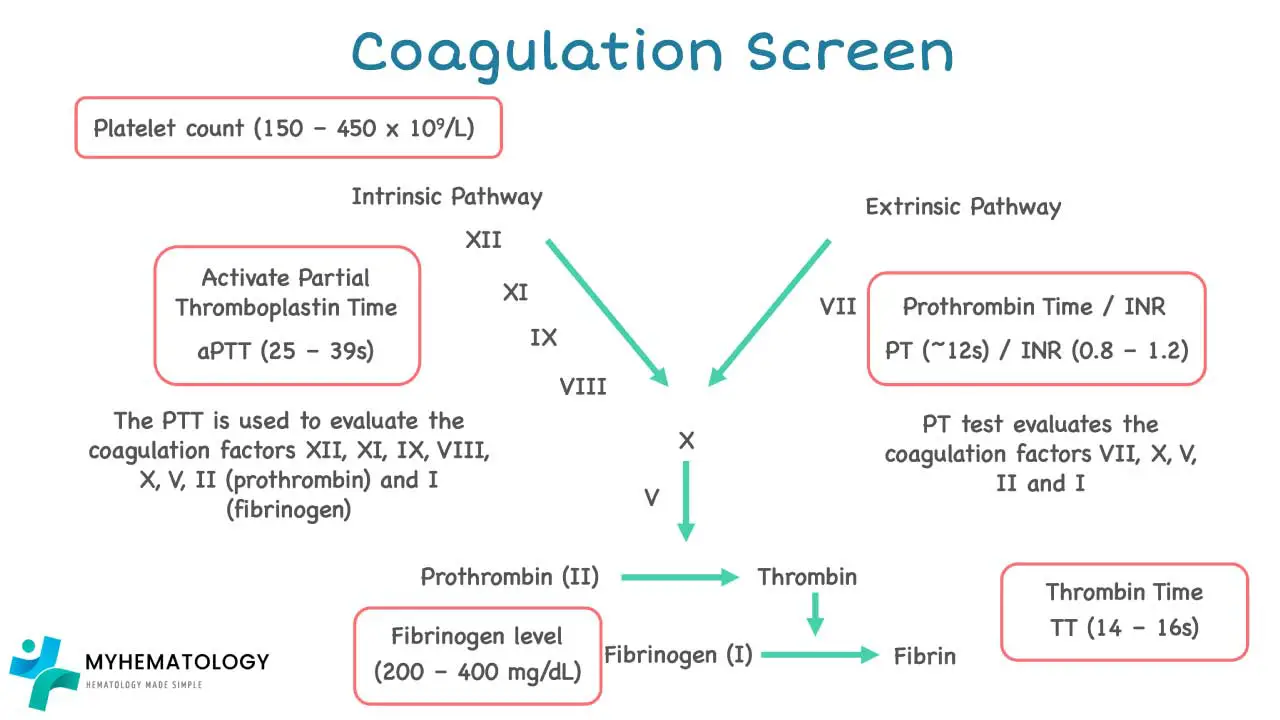
The coagulation profile, also known as a clotting profile, is a series of blood tests that assess the blood’s ability to form clots and prevent excessive bleeding. It plays a crucial role in diagnosing and managing bleeding and clotting disorders.
- Prothrombin Time (PT): Measures the time it takes for blood to clot after adding tissue factor and calcium. An abnormal PT can indicate deficiencies in factors involved in the extrinsic clotting pathway, such as Factor VII, Factor X, or prothrombin itself. This could increase bleeding risk.
- Activated Partial Thromboplastin Time (APTT): Measures the time it takes for blood to clot after adding a phospholipid and an activator that bypasses the initial steps of clotting. An abnormal APTT suggests deficiencies in factors involved in the common clotting pathway, including Factors VIII, IX, XI, XII, or abnormalities in platelets or clotting proteins. This could also indicate an increased risk of bleeding.
- Thrombin Time (TT): Measures the time it takes for fibrin to form after adding thrombin, the enzyme responsible for converting fibrinogen to fibrin (the clot). An abnormal TT suggests issues with fibrinogen or thrombin activity, potentially leading to impaired clot formation.
Markers for Blood Clot Formation and Breakdown
- D-Dimer: A fragment produced during fibrin breakdown. Elevated D-Dimer levels can suggest increased clotting activity or ongoing clot breakdown, potentially helpful in diagnosing deep vein thrombosis (DVT) or pulmonary embolism (PE). However, other conditions can also elevate D-Dimer.
- Fibrin Degradation Products (FDP): Similar to D-Dimer, these are fragments of fibrin degradation. Elevated FDP levels indicate ongoing clot breakdown, but they are not as specific as D-Dimer.
Tests for Specific Clotting Factors
- Proteins C & S, Antithrombin: These are natural anticoagulants that regulate clot formation. Deficiencies in these proteins can increase the risk of blood clots.
- Factors II (Prothrombin) through XII: These are individual proteins involved in the various clotting pathways. Testing for specific factors helps pinpoint the exact cause of abnormal PT or APTT results, allowing for targeted treatment of clotting factor deficiencies.
Platelet Function Tests
- Platelet Aggregation Test: Measures the ability of platelets to clump together and form a plug at the site of injury, triggered by various agents like collagen, arachidonic acid, ADP, and epinephrine. Abnormal platelet aggregation suggests impaired platelet function, potentially leading to increased bleeding risk. This can be caused by various factors such as medications, inherited disorders, or certain diseases.
- Platelet ATP Release: Measures the release of adenosine triphosphate (ATP) from platelets upon activation, which plays a role in platelet aggregation and signaling. Reduced ATP release can indicate abnormal platelet function.
| Parameter | Reference range | Unit |
| Prothrombin time | 12 – 14 | Seconds (s) |
| Activated partial thromboplastin time (APTT) | 24 – 35 | s |
| Thrombin time (TT) | 12 – 17 | s |
| D-Dimer for DVT/PE | <400 | ng/mL |
| Protein S | 65 – 140 | % |
| Protein C | 70 – 140 | % |
| Antithrombin | 80 – 120 | % |
| Factor II | 50 -150 | % |
| Factor V | 50 -150 | % |
| Factor VII | 50 -150 | % |
| Factor VIII | 50 – 200 | % |
| Factor IX | 50 – 150 | % |
| Factor X | 50 – 150 | % |
| Factor XI | 50 – 150 | % |
| Factor XII | 50 -150 | % |
| Willebrand factor activity | 60 – 200% | % |
| Willebrand factor antigen | 50 – 160 | % |
| Factor VIII-inhibitor | 0 – 0.5 | Bethesda unit |
| Alpha2-antiplasmin | 80-120 | % |
| Plasminogen | 80-120 | % |
| Fibrin degradation products (latex particles) | <20 | ug/mL |
| Platelet Aggregation (in platelet-rich plasma) | ||
| with collagen (2ug/mL) | 70-95 | % |
| with arachidonic acid (0.5mM) | 70-100 | % |
| with ADP 5uM | 70-90 | % |
| with ADP 10uM | 70 – 90 | % |
| with epinephrine (5uM) | 75-90 | % |
| with ristocetin (1.0 mg/mL) | 60 -80 | % |
| Platelet ATP release (in blood) | ||
| with thrombin (1 unit) | >0.5 | nmoles of ATP |
| with collagen (2 mg/mL) | 0.5 – 1.7 | nmoles of ATP |
| (5mg/mL) | 0.9 – 1.7 | nmoles of ATP |
| with arachidonic acid (0.5mM) | 0.56 – 1.4 | nmoles of ATP |
| ADP (5mM) | 0 – 0.7 | nmoles of ATP |
| ADP (19mM) | 0.38 – 1.71 | nmoles of ATP |
Iron Studies
Iron studies and a CBC with differential are closely linked, especially when evaluating and diagnosing anemia, particularly Iron Deficiency Anemia (IDA).
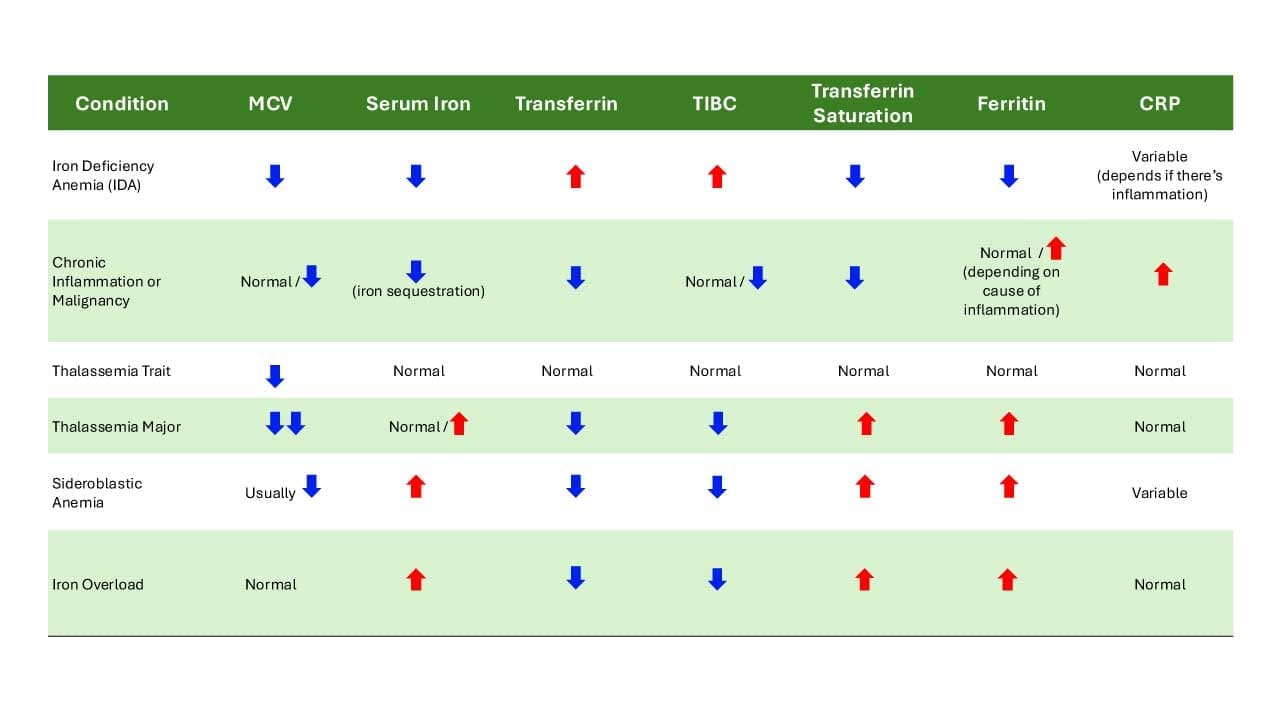
- Serum Iron: Measures the amount of iron circulating in the blood attached to a protein carrier called transferrin. Low serum iron can suggest iron deficiency, while high levels might indicate iron overload.
- Total Iron Binding Capacity (TIBC): Reflects the total amount of iron that transferrin can bind. High TIBC with low serum iron suggests iron deficiency, while a low TIBC with high serum iron might indicate inflammation or liver disease.
- Transferrin Saturation: Indicates the percentage of transferrin sites occupied by iron (serum iron divided by TIBC). A low transferrin saturation suggests iron deficiency, while a high saturation could indicate iron overload or inflammation.
- Ferritin: Stores iron in the body, primarily in the liver. Low ferritin is a more reliable indicator of iron deficiency compared to serum iron alone. High ferritin can suggest iron overload or inflammation.
Vitamin Deficiencies
The CBC with differential acts as a screening tool, providing morphological clues (especially the MCV) that alert clinicians to the possibility of certain vitamin deficiencies. These CBC findings then prompt specific vitamin level tests (e.g., serum B12, serum folate, red cell folate) to confirm the diagnosis and guide appropriate supplementation or treatment.
- Serum Vitamin B12: Essential for DNA synthesis and red blood cell production. Deficiency can cause megaloblastic anemia with large, immature red blood cells.
- Serum Folate: Another crucial vitamin for red blood cell production. Deficiency can also lead to megaloblastic anemia.
- Red Cell Folate: Measures folate levels directly within red blood cells, potentially providing a more accurate picture of folate status. Low red cell folate can confirm folate deficiency even if serum folate levels appear normal.
Red Blood Cell Production
- Serum Soluble Truncated Transferrin Receptor (sTfR): Released by bone marrow when iron is deficient to increase iron uptake for red blood cell production. High sTfR levels suggest iron deficiency, while normal or low levels may indicate adequate iron stores or other causes of anemia.
- Serum Haptoglobin: Binds to free hemoglobin released from damaged red blood cells. Low haptoglobin can suggest ongoing hemolysis (destruction of red blood cells).
- Serum Erythropoietin: A hormone produced by the kidneys that stimulates red blood cell production in response to low oxygen levels. High erythropoietin levels can be a sign of anemia due to various causes, including iron deficiency, vitamin deficiencies, or bone marrow problems.
| Parameter | Reference range | Unit |
| Serum iron | 11.5 – 30.5 | umol/L |
| TIBC | 45.5 – 75 | umol/L |
| Transferrin saturation | 15 – 47.5 | % |
| Ferritin | 20 – 325 | ug/L |
| Serum vitamin B12 | 180 – 1000 | pg/mL |
| Serum folate | 7 – 45 | nmol/L |
| Red cell folate | 300 – 1000 | nmol/L |
| Serum soluble truncated transferrin receptor (sTfR) | 9 – 28 | nmol/L |
| Serum haptoglobin | 30 – 200 | mg/dL |
| Serum erythropoietin | 4 – 19 | mU/mL |
Lymphocyte subsets
Lymphocyte subsets are a specific group of white blood cells (WBCs) within the lymphocyte category that play a critical role in the adaptive immune system. A CBC with differential count doesn’t typically provide a detailed breakdown of lymphocyte subsets. However, some advanced hematology tests can measure these subsets using markers like CD3, CD4, CD8, and calculate the CD4/CD8 ratio.
- CD3 Positive (CD3+): This marker identifies mature T lymphocytes, a major component of the adaptive immune system. A low CD3+ count may suggest immunodeficiency or malnutrition.
- CD4 Positive (CD4+): These are T helper cells, vital for directing and regulating the immune response. They activate other immune cells and help B cells produce antibodies. A low CD4+ count is a hallmark of HIV infection and can also be seen in some autoimmune diseases.
- CD8 Positive (CD8+): These are cytotoxic T lymphocytes (CTLs) that directly target and kill virus-infected cells or abnormal cells like cancer cells. An increased CD8+ count can be seen in viral infections or chronic inflammatory conditions.
- CD4/CD8 Ratio: This compares the number of CD4+ helper T cells to CD8+ cytotoxic T cells.
- A low ratio (less than 1.0): May suggest HIV infection, immunosuppression, or certain autoimmune diseases.
- A high ratio (more than 3.0): Less common, but can be seen in some viral infections or immune system disorders.
| Parameter | Reference Range | Unit |
| CD3# | 694 – 2362 | cell/uL |
| CD4# | 391 – 1548 | cell/uL |
| CD8# | 185 – 1049 | cell/uL |
| CD3% | 51.19 – 81.65 | % |
| CD4% | 26.38 – 54 | % |
| CD8% | 12.89 – 40.69 | % |
| CD4/8 ratio | 0.77 – 3.93 |
Hemoglobin Subtypes
Hemoglobin subtypes themselves are not routinely measured in a CBC with differential. However, understanding their importance lies in their role in diagnosing specific blood disorders like sickle cell disease and thalassemia. Identifying the type of abnormal hemoglobin (e.g., HbA, HbA2, HbF, HbS) helps guide treatment decisions and manage these conditions effectively.
| Parameter | Reference range | Unit |
| HbA1 | 96.1 – 99.0 | % |
| HbA2 | 1.6 – 3.5 | % |
| Hb F | 0.0 – 1.4 | % |
Frequently Asked Questions (FAQs)
What are 5 things the CBC can show signs of?
The Complete Blood Count (CBC) with differential is a very common and foundational blood test that can reveal signs of a wide range of health issues by evaluating the types and numbers of cells in the blood.
- Anemia: This is one of the most common findings. A CBC with differential will show low levels of red blood cells (RBC count), hemoglobin (the protein that carries oxygen), and/or hematocrit (the percentage of red blood cells in the blood). The red blood cell indices (like MCV, MCH) can further classify the type of anemia (e.g., iron deficiency, vitamin B12 deficiency).
- Infections: Changes in the white blood cell (WBC) count and differential can strongly indicate an infection in the CBC with differential.
- An elevated total WBC count, often with a significant increase in neutrophils, suggests a bacterial infection.
- An elevated lymphocyte count might point to a viral infection.
- Increased eosinophils can suggest parasitic infections or allergic reactions.
- Inflammation (General): While not specific to the cause, alterations in WBC counts (e.g., leukocytosis) or specific WBC types can signal that there’s an inflammatory process happening in the body due to various causes, including infections, autoimmune diseases, or tissue damage.
- Bleeding or Clotting Problems:
- A low platelet count (thrombocytopenia) can indicate an increased risk of bleeding.
- A high platelet count (thrombocytosis) can indicate an increased risk of clotting or be a sign of an underlying inflammatory condition or bone marrow issue.
- Significant blood loss, whether acute or chronic, will manifest as anemia on the CBC with differential.
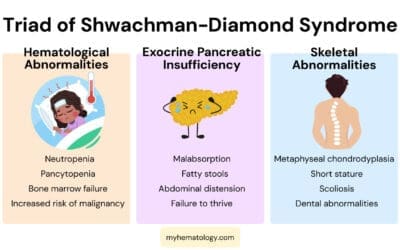
- Bone Marrow Disorders and Cancers: Abnormalities in any of the cell lines (red, white, or platelets), especially very high or very low counts, the presence of immature cells, or unusual cell morphology (as might be seen on a peripheral blood smear if abnormal cells are flagged by the analyzer), can be a sign of underlying bone marrow problems or blood cancers like leukemia, lymphoma, or myelodysplastic syndromes.
Can a CBC test detect kidney problems?
While a CBC (Complete Blood Count) with differential doesn’t directly diagnose kidney problems, it can certainly show signs and complications that are highly suggestive of kidney dysfunction or disease.
- Anemia (Most Common Sign): Healthy kidneys produce a hormone called erythropoietin (EPO), which signals the bone marrow to produce red blood cells. In chronic kidney disease (CKD), damaged kidneys produce less EPO, leading to a decreased production of red blood cells. This manifests as anemia on the CBC with differential, specifically a low hemoglobin, hematocrit, and RBC count. It’s often a normocytic, normochromic anemia (normal MCV, MCH, MCHC) in early to moderate kidney disease. Anemia is a very common complication of CKD and is often one of the first indicators seen on routine blood tests.
- Abnormal Platelet Count/Function: Kidney disease can sometimes affect platelet production or, more commonly, their function. While the CBC with differential will show the platelet count, severe kidney failure can lead to uremia (buildup of waste products), which can impair platelet function, increasing the risk of bleeding even if the platelet count is normal
- White Blood Cell Changes (Indirectly): While not a direct sign of kidney damage, kidney disease can sometimes be associated with increased susceptibility to infections, which might be reflected in changes in the WBC count or differential on the CBC if an infection is present.
A CBC with differential alone cannot definitively diagnose kidney problems. To directly assess kidney function, other specific blood tests are crucial, such as:
- Creatinine and Blood Urea Nitrogen (BUN): Waste products that accumulate in the blood when kidneys are not filtering effectively.
- Estimated Glomerular Filtration Rate (eGFR): Calculated from creatinine (and sometimes other factors), this is the best measure of kidney function.
- Urinalysis: To check for protein or blood in the urine, which are key signs of kidney damage.
How many hours fasting for CBC with differential?
Generally, an individual do not need to fast for a CBC (Complete Blood Count) with differential test. Food and drink typically do not affect the components measured in a CBC with differential, such as red blood cells, white blood cells, hemoglobin, hematocrit, and platelets.
If the CBC with differential is ordered as part of a larger blood panel that includes other tests that do require fasting (like a glucose test for blood sugar, or a lipid panel for cholesterol and triglycerides), then the individual will likely be instructed to fast. The typical fasting period for these combined tests is 8 to 12 hours.
Disclaimer: This article is intended for informational purposes only and is specifically targeted toward medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. This article does not provide exhaustive information on all aspects of the discussed hematological disorders, and new research and understanding may emerge over time. See additional information.
References
- Jastinton A. LAB VALUES INTERPRETATION: The Indispensable Guide to Quickly Learn and Interpret The Laboratory Results.Find and Understand Everything That Impacts a Diagnosis of Disease. 2021.
- El Brihi J, Pathak S. Normal and Abnormal Complete Blood Count With Differential. [Updated 2024 Jun 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK604207/
- George-Gay, B., & Parker, K. (2003). Understanding the complete blood count with differential. Journal of perianesthesia nursing : official journal of the American Society of PeriAnesthesia Nurses, 18(2), 96–117. https://doi.org/10.1053/jpan.2003.50013
- Agrawal, Deepak et al. Complete Blood Count or Complete Blood Count with Differential: What’s the Difference? The American Journal of Medicine, Volume 130, Issue 8, 915 – 916
- Tefferi, A., Hanson, C. A., & Inwards, D. J. (2005). How to interpret and pursue an abnormal complete blood cell count in adults. Mayo Clinic proceedings, 80(7), 923–936. https://doi.org/10.4065/80.7.923