TL;DR
Thrombocytopenia is a condition characterized by an abnormally low platelets in the blood (generally below 150,000 platelets per microliter).
Causes ▾
- Decreased Platelet Production: Bone marrow disorders, vitamin deficiencies, medications, infections.
- Increased Platelet Destruction: Immune thrombocytopenic purpura (ITP), heparin-induced thrombocytopenia (HIT), hypersplenism.
- Other Mechanisms: Dilutional loss (massive transfusion), abnormal platelet distribution (splenomegaly).
Clinical Presentation ▾
- May have no symptoms with mild thrombocytopenia.
- Easy bruising, petechiae (tiny red spots on skin), prolonged bleeding from minor injuries are common symptoms with low platelets.
- Severe cases can lead to bleeding from mucous membranes (mouth, nose, gastrointestinal tract).
Diagnosis ▾
- Blood tests (complete blood count – CBC), peripheral blood smear examination.
- Additional tests depending on suspected cause (bone marrow biopsy, autoimmune workup).
Treatment ▾
- Address the underlying cause whenever possible.
- Platelet transfusions for severe bleeding or high bleeding risk.
- Medications to increase platelet production (thrombopoietin receptor agonists).
- Splenectomy (removal of spleen) in specific cases.
- Corticosteroids, immunoglobulin therapy, or other medications depending on the cause.
*Click ▾ for more information
Introduction
Thrombocytopenia is a condition characterized by an abnormally low platelets in the blood. In medical terms, a platelet count that falls below 150,000 platelets per microliter is generally considered thrombocytopenia.
The physiological role of platelets
Platelets are essential for hemostasis, the body’s natural process of stopping bleeding. Hemostasis occurs in a series of steps:
- Vascular Spasm: When a blood vessel is injured, it constricts to slow down blood flow.
- Platelet Plug Formation: Platelets are attracted to the damaged area and become sticky. They adhere to each other and the injured vessel wall, forming a temporary plug that seals the initial breach.
- Coagulation (Blood Clotting): Platelets also release chemicals that activate a cascade of proteins in the blood called clotting factors. These factors work together to create a stronger fibrin clot that reinforces the platelet plug.
- Clot Retraction and Fibrinolysis: Once bleeding is stopped, the clot contracts and eventually dissolves through a process called fibrinolysis, allowing for proper healing.
Causes of Thrombocytopenia (Low Platelets)
Thrombocytopenia (low platelets) can arise from various mechanisms that disrupt the normal balance of platelet production and destruction in the bloodstream.
Decreased Platelet Production
- Bone marrow disorders: Diseases like leukemia, aplastic anemia, and myelodysplastic syndromes can damage bone marrow stem cells, hindering their ability to produce platelets leading to low platelets.
- Nutritional deficiencies: Vitamin B12 and folate are vital for healthy blood cell production. Deficiencies in these vitamins can lead to low platelets production.
- Medications: Certain medications, including chemotherapy drugs, some antibiotics, and anticonvulsants, can have a suppressive effect on bone marrow, reducing platelet production.
- Viral infections: Infections like HIV, hepatitis C, and Epstein-Barr virus can temporarily suppress platelet production.
Increased Platelet Destruction
- Immune thrombocytopenia (ITP): In ITP, the immune system mistakenly attacks and destroys healthy platelets. This can be idiopathic (cause unknown) or secondary to another condition like lupus.
- Heparin-induced thrombocytopenia (HIT): This is a rare complication of heparin therapy, where antibodies develop against heparin-platelet complexes, leading to platelet destruction.
- Hypersplenism: An enlarged spleen can trap and destroy an excessive number of platelets. This often occurs due to underlying conditions like liver cirrhosis or Gaucher disease.
Dilutional Loss
- Massive blood transfusion: When large volumes of blood are rapidly transfused, the existing platelets become diluted, leading to a relative low platelets concentration.
Abnormal Platelet Distribution
- Splenomegaly (enlarged spleen): While contributing to increased destruction in some cases, an enlarged spleen can also simply sequester platelets, reducing their circulating number even though the overall production might be normal.
Drugs and Toxins
- Certain medications, like some antibiotics and anti-malarial drugs, can directly damage platelets or cause their destruction.
- Exposure to toxins, including heavy metals like arsenic and benzene, can also impair platelet production or function.
Pediatric and Pregnancy Considerations
Thrombocytopenia can occur in both children and pregnant women, but the underlying causes may differ from the general population.
Pediatrics
- Neonatal Thrombocytopenia:
- Fetomaternal alloimmune thrombocytopenia (FNAIT): This occurs when a mother develops antibodies against specific platelet antigens on her baby’s platelets. It can be a serious condition requiring specialized care.
- Transient Neonatal Thrombocytopenia: This is a common and usually benign condition where a baby has low platelets at birth but recovers on its own within a few days.
- Congenital Infections: Certain infections transmitted from mother to baby (e.g., cytomegalovirus, herpes) can cause thrombocytopenia (low platelets) in newborns.
- Childhood Infections: Viral infections such as measles, mumps, rubella, and parvovirus can cause temporary thrombocytopenia (low platelets) in children.
- Idiopathic Thrombocytopenic Purpura (ITP): This autoimmune condition can occur in children, often following a viral infection.
- Evans Syndrome: This is a rare autoimmune disorder affecting red blood cells, platelets, and sometimes white blood cells.
- Hematologic malignancies: Although less common, childhood leukemia can also cause thrombocytopenia (low platelets).
Pregnancy
- Gestational Thrombocytopenia: This is a mild decrease in platelet count that occurs in up to 8% of pregnancies. It is usually not a cause for concern and resolves on its own after delivery.
- Preeclampsia: This pregnancy complication can be associated with thrombocytopenia as part of a constellation of symptoms.
- HELLP syndrome: This severe form of preeclampsia involves hemolysis (red blood cell destruction), elevated liver enzymes, and low platelet count.
Disorders Related to Increased Platelet Consumption and Destruction
Several disorders can cause a rapid decline in platelet count due to their increased consumption or destruction.
Immune Thrombocytopenia (ITP)
- Cause: The immune system mistakenly attacks healthy platelets, leading to their destruction. Idiopathic ITP (cause unknown) is most common in children, while secondary ITP can be associated with autoimmune diseases like lupus or viral infections.
- Symptoms: Easy bruising, petechiae (tiny red spots on skin), prolonged bleeding from minor injuries. In severe cases, bleeding can occur in the brain or gastrointestinal tract.
- Diagnosis: Based on clinical symptoms, low platelet count on blood tests, and absence of other causes. Additional tests may be done to rule out secondary ITP.
- Treatment: Varies depending on severity and underlying cause. Options include corticosteroids, intravenous immune globulin (IVIG), platelet transfusions (for severe bleeding), and splenectomy (removal of spleen in specific cases).
Post-Transfusion Purpura (PTP)
- Cause: A rare but serious reaction to blood transfusions containing incompatible platelets. The body develops antibodies against foreign platelet antigens, leading to their destruction.
- Symptoms: Onset typically within 1-2 weeks after transfusion. Similar symptoms to ITP, including easy bruising and bleeding.
- Diagnosis: Based on history of transfusion, low platelet count, and presence of specific antibodies in the blood.
- Treatment: Supportive care to manage bleeding. Future blood transfusions should be carefully selected to avoid incompatible platelets.
Disseminated Intravascular Coagulation (DIC)
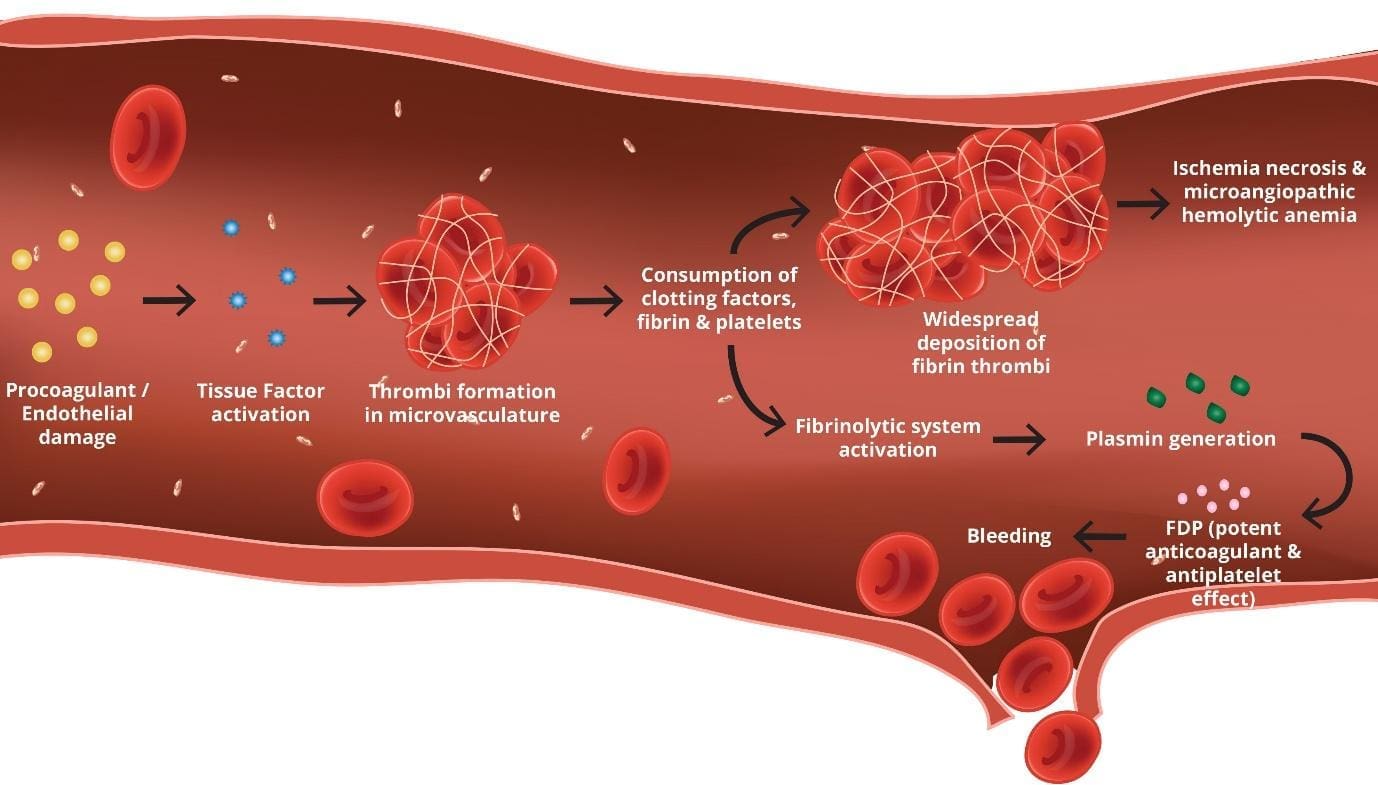
- Cause: A complex disorder characterized by widespread activation of blood clotting throughout the body. This leads to formation of small clots that consume platelets and clotting factors, ultimately causing bleeding.
- Symptoms: Can vary depending on the underlying cause. May include easy bruising, bleeding from various sites, and signs of organ dysfunction (e.g., kidney failure) due to microvascular thrombosis.
- Diagnosis: Based on clinical presentation, laboratory tests showing abnormal clotting parameters and evidence of decreased platelets and clotting factors.
- Treatment: Address the underlying cause of DIC (e.g., sepsis, severe trauma). Supportive measures include blood transfusions (platelets, plasma, red blood cells) and medications to manage bleeding and prevent further clot formation.
Infections
- Cause: Certain infections, like bacterial sepsis or viral infections (dengue fever), can trigger immune responses that lead to increased platelet destruction.
- Symptoms: Variable depending on the specific infection. May include fever, malaise, and bleeding along with signs of the underlying infection.
- Diagnosis: Based on clinical presentation, blood tests showing low platelet count and identification of the causative infection.
- Treatment: Treatment of the underlying infection is crucial. Platelet transfusions may be needed in severe cases.
Drug-Induced Immune Thrombocytopenia (DIT)
- Cause: Certain medications can trigger an immune reaction that destroys platelets. Examples include heparin, quinine, and some antibiotics.
- Symptoms: Similar to ITP, with easy bruising and bleeding. Onset typically occurs within days or weeks of starting the medication.
- Diagnosis: Based on history of medication use, low platelet count, and improvement of platelet count after stopping the suspected drug.
- Treatment: Discontinuation of the offending medication and use of alternative therapies. Platelet transfusions may be needed in severe cases.
Thrombotic Thrombocytopenic Purpura (TTP)
ADAMTS-13, an enzyme responsible for cleaving large von Willebrand factor (VWF) multimers, plays a pivotal role in maintaining the delicate balance of blood vessel integrity. In TTP, the absence of ADAMTS-13 leads to an accumulation of these large VWF multimers, creating a sticky environment that promotes platelet aggregation and thrombocytopenia.
- Cause: A rare, life-threatening condition characterized by severe deficiency of an enzyme called ADAMTS13. This enzyme normally breaks down large von Willebrand factor (vWF) multimers in the blood. Without proper breakdown, these large vWF multimers cause platelet aggregation and microthrombi formation throughout the body, leading to platelet consumption and tissue damage.
- Symptoms: Can include fever, neurologic symptoms (confusion, headache), kidney failure, and bleeding (less common).
- Diagnosis: Based on clinical presentation, laboratory tests showing low platelet count, abnormal blood smear with schistocytes (fragmented red blood cells), and ADAMTS13 activity testing.
- Treatment: Plasma exchange is the mainstay of treatment. This removes abnormal vWF multimers and ADAMTS13 antibodies from the circulation. Medications like corticosteroids may also be used.
Hemolytic-Uremic Syndrome (HUS)
- Cause: There are two main types: typical HUS, which occurs in children after a diarrheal illness caused by Shiga toxin-producing E. coli (STEC) bacteria, and atypical HUS, which can be associated with genetic abnormalities or autoimmune disorders. Both types damage blood vessels and lead to platelet consumption.
- Symptoms: Can include triad of symptoms: thrombocytopenia, microangiopathic hemolytic anemia, and acute kidney injury.
- Diagnosis: Blood tests, stool cultures (for typical HUS), may require genetic testing (for atypical HUS).
- Treatment: Supportive care, may involve plasma exchange or medications to suppress the immune system (for atypical HUS).
Thrombocytopenia (Low Platelets) Symptoms
Symptoms of low platelets can manifest in various ways, with some individuals experiencing no noticeable symptoms at all, particularly in cases of mild reduction in platelet count. However, as the platelet count falls, individuals may experience a range of signs and symptoms that indicate a potential bleeding problem.
Signs and Symptoms of Low Platelets
- Easy Bruising (Ecchymosis): This is a common early sign. Bruises form more easily than usual, even with minimal trauma. They may appear larger and deeper than expected.
- Petechiae: These are tiny, flat, reddish-purple spots under the skin caused by bleeding from small blood vessels. They typically appear on the lower legs but can occur anywhere.
- Prolonged Bleeding from Minor Injuries: Cuts or injuries take longer than usual to stop bleeding. Even minor procedures like shaving or nosebleeds can be problematic.
- Bleeding in Mucous Membranes: This can manifest as bleeding gums, blood in the stool (appearing black or tarry), or blood in the urine (red or pink urine).
- Heavy Menstrual Periods: Women with thrombocytopenia may experience unusually heavy or prolonged menstrual bleeding.
Importance of Platelet Count in Bleeding Risk Assessment
The severity of bleeding risk in thrombocytopenia is directly related to the platelet count. While a mild decrease might not cause significant symptoms, a very low platelet count can be life-threatening. Here’s a general guide:
- Platelet Count > 100,000/µL: Low risk of bleeding.
- Platelet Count 50,000-100,000/µL: Increased risk of bleeding with minor trauma or surgery.
- Platelet Count < 50,000/µL: Significant risk of spontaneous bleeding, including internal bleeding.
- Platelet Count < 10,000/µL: Very high risk of life-threatening bleeding.
It’s important to remember that these are just general guidelines. The bleeding risk can also be influenced by other factors like the size and location of the injury, as well as any underlying medical conditions.
Laboratory Investigations of Thrombocytopenia
Complete Blood Count (CBC)
This is the initial and most crucial test. It measures various blood cell counts, including platelets. A low platelet count on a CBC is the primary indicator of thrombocytopenia.
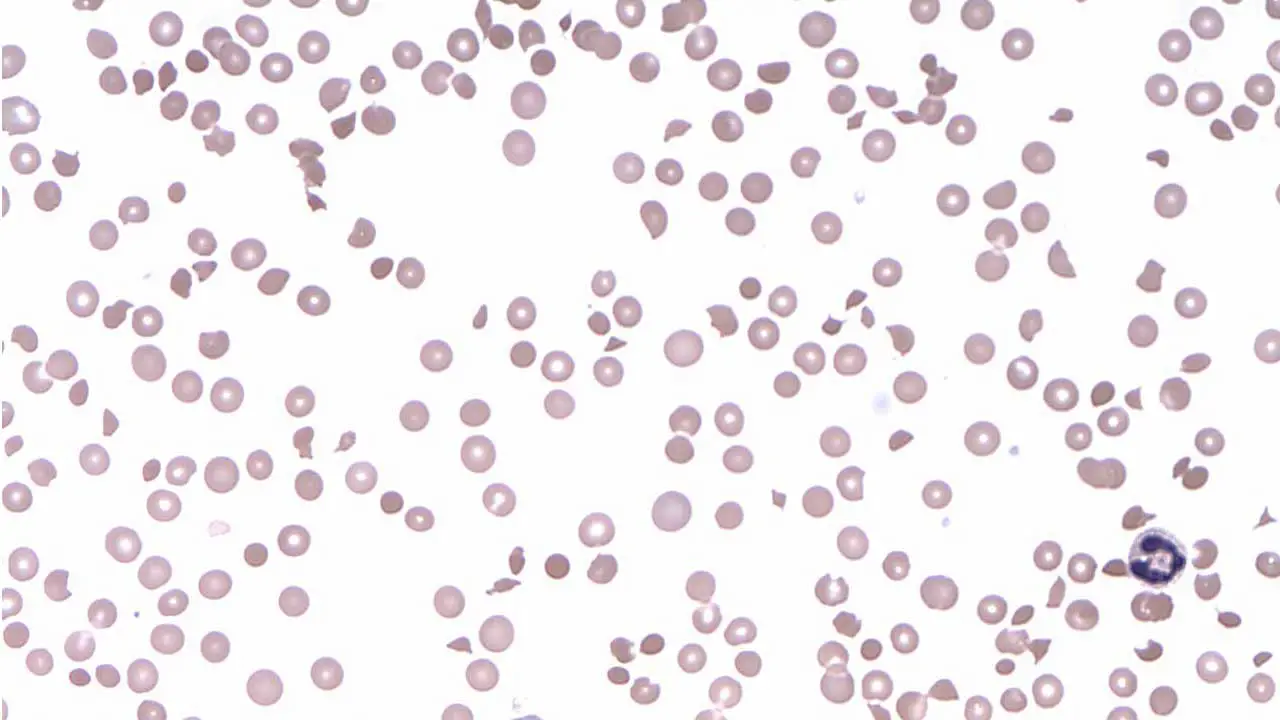
Peripheral Blood Smear Examination
A blood smear allows visualization of platelet size, shape, and number under a microscope. It can reveal abnormal platelet morphology (appearance) that might suggest specific causes, such as large platelets in MYH9-related disease or fragmented platelets in thrombotic thrombocytopenic purpura (TTP).
Additional Tests Depending on Suspected Cause
- Coagulation Studies: These tests (PT, aPTT, TT, fibrinogen assay and D-dimer) assess the clotting cascade and might be helpful in conditions like disseminated intravascular coagulation (DIC) where abnormal clotting is a contributing factor.
- Bone Marrow Aspiration and Biopsy: In some cases, examining bone marrow can be necessary to evaluate platelet production and identify disorders like aplastic anemia or bone marrow infiltration by cancer cells.
- Autoimmune Workup: If an autoimmune cause (like ITP) is suspected, tests to look for specific antibodies or assess immune system function might be ordered.
- Direct Antiglobulin Test (DAT): This test helps identify antibodies coating red blood cells, which can be relevant in some cases of drug-induced immune thrombocytopenia.
Treatment of Thrombocytopenia
The treatment for thrombocytopenia (low platelets) depends entirely on the underlying cause and the severity of the condition.
Addressing the Underlying Cause
- This is the ideal approach whenever possible. For example, treating a viral infection that’s causing thrombocytopenia or stopping a medication that might be responsible.
- In cases of autoimmune thrombocytopenic purpura (ITP), addressing the underlying immune dysfunction can help improve platelet count.
Platelet Transfusions
- In situations with severe bleeding or a very low platelet count that poses a high bleeding risk (usually below 10,000-20,000/mcL), platelet transfusions are given to increase the circulating platelet count and prevent bleeding complications.
- Platelet transfusions are a temporary solution and may need to be repeated depending on the underlying cause and the body’s response.
Medications to Increase Platelet Production (Thrombopoietin Receptor Agonists)
- These drugs stimulate the bone marrow to produce more platelets. They are often used in chronic ITP or other conditions where the bone marrow is not producing enough platelets.
Splenectomy (Spleen Removal)
- In specific cases, particularly chronic ITP that doesn’t respond well to other treatments, the spleen may be surgically removed. The spleen plays a role in platelet destruction, and removing it can help increase the circulating platelet count.
Corticosteroids
- These medications can suppress the immune system and are sometimes used in ITP to reduce platelet destruction. However, they are typically used as a short-term solution due to potential side effects.
Immunoglobulin Therapy (IVIG)
- Intravenous immune globulin (IVIG) can be used in some cases of ITP to temporarily improve platelet count by blocking the destruction of platelets by the immune system.
Other Medications
- Depending on the specific cause of thrombocytopenia, other medications like antifibrinolytics (to prevent clot breakdown) or immunosuppressants (for severe autoimmune cases) might be used.
Frequently Asked Questions (FAQs)
What happens if thrombocytopenia is untreated?
The consequences of untreated thrombocytopenia (low platelets) depend on the severity of the condition, which is primarily determined by the platelet count.
Mild Thrombocytopenia (Platelet Count > 50,000/µL):
- In some cases, individuals with mild thrombocytopenia may not experience any noticeable symptoms of low platelets and might not require immediate treatment.
- However, even with a seemingly minor decrease in platelet count, there’s an increased risk of easy bruising and bleeding from minor injuries compared to those with normal platelet levels.
Moderate Thrombocytopenia (Platelet Count 20,000-50,000/µL):
- The risk of bleeding becomes more significant with a moderate decrease in platelet count.
- Individuals might experience more frequent and extensive bruising, bleeding from gums or nosebleeds.
- Internal bleeding in the gastrointestinal tract (manifesting as blood in vomit or stool) can also occur in some cases.
Severe Thrombocytopenia (Platelet Count < 20,000/µL):
- This is a serious condition with a high risk of life-threatening bleeding complications.
- Internal bleeding in the brain (intracranial hemorrhage) can be a devastating consequence of severe thrombocytopenia.
- Bleeding into other organs, such as the lungs or gastrointestinal tract, can also occur.
Here are some additional points to consider:
- The location of bleeding can significantly impact its severity. Bleeding in critical areas like the brain can be life-threatening, even with a moderate decrease in platelet count.
- The underlying cause of thrombocytopenia can also influence the risk of complications. For example, some conditions like disseminated intravascular coagulation (DIC) can lead to both low platelet count and abnormal clotting, further increasing bleeding risk.
- Individuals with underlying medical conditions or taking medications that affect blood clotting are at a higher risk of complications from thrombocytopenia.
Do low platelets make you tired?
Low platelet count itself (thrombocytopenia) typically doesn’t directly cause fatigue.
Can thrombocytopenia be cured?
In most cases, thrombocytopenia itself cannot be definitively cured. However, the treatment approach focuses on managing the underlying cause and preventing bleeding complications. The possibility of achieving a normal platelet count and preventing future episodes depends on the specific cause
Can thrombocytopenia cause blood clots, stroke or deep vein thrombosis (DVT)?
Thrombocytopenia, the condition of having a low platelet count, typically does not directly cause blood clots, stroke, or deep vein thrombosis (DVT).
How do NSAIDs cause thrombocytopenia?
NSAIDs (nonsteroidal anti-inflammatory drugs) like ibuprofen or aspirin are known for their blood-thinning effects, but they typically don’t cause true thrombocytopenia (drastically low platelet count) However, in rare cases, NSAIDs can trigger an immune reaction that leads to platelet destruction. This can cause a mild decrease in platelet count and a temporary increase in bleeding risk. This is more likely in individuals with a predisposition or those taking high doses for extended periods.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.