Introduction
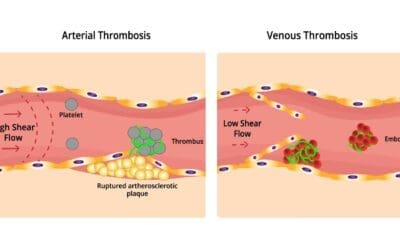
Thrombotic thrombocytopenic purpura (TTP) is a rare and life-threatening blood disorder. It is characterized by the formation of small blood clots (microthrombi) throughout the body. These microthrombi can block small blood vessels and damage organs, such as the brain, kidneys, and heart.
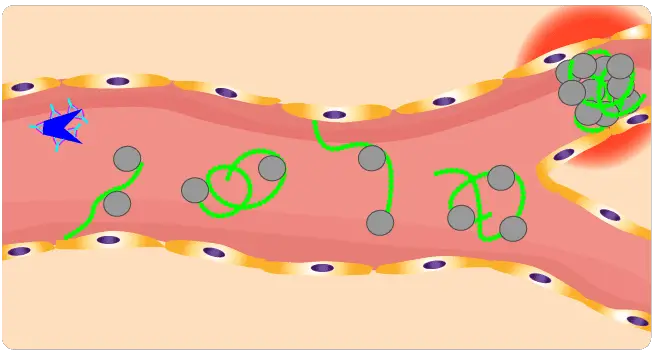
TTP is caused by a deficiency of a protein called ADAMTS13. ADAMTS13 is responsible for cleaving a large protein called von Willebrand factor (VWF). VWF acts as a bridge between platelets and the walls of blood vessels at the site of an injury by binding to collagen and capturing platelets. VWF also stabilizes factor VIII, another essential clotting protein. When ADAMTS13 is deficient, VWF forms large multimers that can clump together to form microthrombi.
There are two main types of TTP:
- Acquired: This is the most common type of TTP and is caused by an autoimmune disorder. In autoimmune disorders, the body’s immune system attacks its own tissues. In acquired TTP, the immune system attacks ADAMTS13.
- Congenital: This is caused by a genetic mutation that affects the ADAMTS13 gene and is rare.
Related Clinical Signs and Symptoms
TTP has traditionally been described as the pentad of thrombocytopenia, microangiopathic hemolytic anemia, neurologic abnormalities, renal failure and fever. The microvascular thrombosis causes variable degrees of tissue ischemia and infarction and is responsible for the microangiopathic hemolytic anemia and thrombocytopenia.
The clinical manifestations of this disorder depend on the severity of the disease and the organs that are affected. The most common clinical manifestations include:
- Thrombocytopenia
- Microangiopathic hemolytic anemia (MAHA)
- Neurologic signs and symptoms, such as headache, confusion, seizures, and focal neurologic deficits
- Renal failure
- Fever
- Fatigue
- Pallor
.
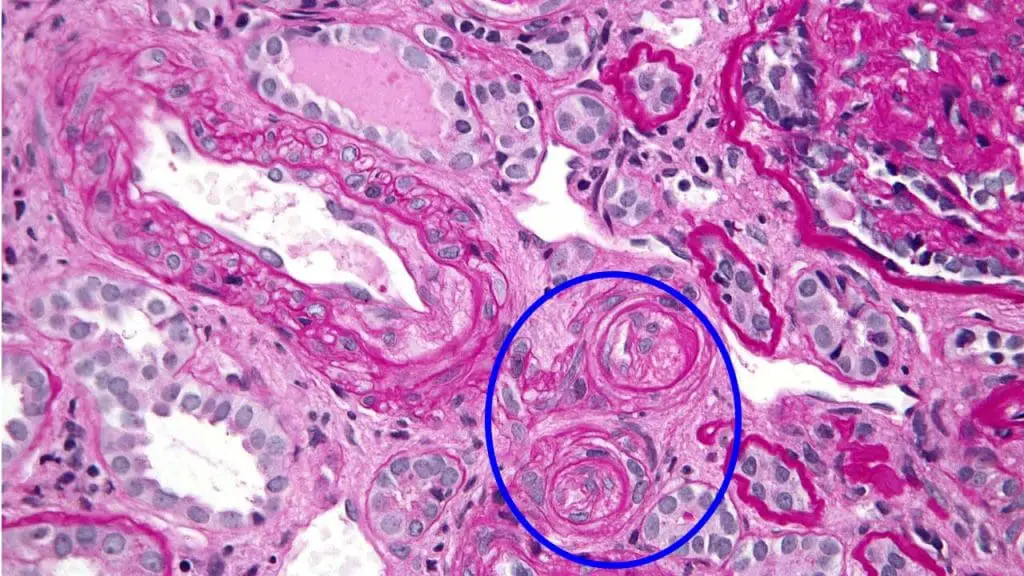
Blood Vessels with Onion Skinning in TTP Kidney Biopsy
Onion skinning refers to a specific histological finding in kidney biopsies. It describes the appearance of blood vessel walls with concentric layers of fibrinoid material. This layering resembles the skin of an onion, hence the name.
In the context of thrombotic thrombocytopenic purpura (TTP), onion skinning is a significant finding and indicates vascular occlusive disease. TTP is a rare but serious disorder characterized by microangiopathic hemolytic anemia, thrombocytopenia, and neurological symptoms.
The mechanism behind onion skinning in TTP involves the deposition of platelet-fibrin thrombi within small blood vessels, particularly the arterioles. These thrombi consist of platelets, fibrin, and other blood components. As the thrombi accumulate, they cause the vessel walls to become thickened and layered, leading to the characteristic onion-skinning appearance.
Significance:
- Diagnosis: The presence of onion skinning in a kidney biopsy is a strong indicator of TTP and can aid in diagnosis.
- Prognosis: The degree of onion skinning seen in the biopsy can also provide information about the severity of the disease and potentially help predict the patient’s prognosis.
- Treatment: Identifying onion skinning helps confirm the diagnosis of TTP, allowing for swift initiation of appropriate treatment, such as plasma exchange therapy.
It’s important to note that while onion skinning is a significant finding in TTP, it can also be seen in other conditions. Therefore, a comprehensive clinical evaluation is essential for accurate diagnosis.
Pathophysiology of TTP
This disorder occurs in familial or acquired forms.
There is a deficiency of ADAMTS13 metalloprotease which breaks down ultra large von Willebrand factor multimers. In the inherited forms, there are more than 50 ADAMTS13 mutations and the acquired forms follow the development of an inhibitory IgG autoantibody which may be stimulated by infection, autoimmune or connective tissue disease, certain drugs, stem cell transplantation or cardiac surgery.
Ultra large vWF multimeric strings secreted from Weibel-Palade bodies are anchored to the endothelial cells and passing platelets adhere via their GP1bɑ receptors. Increasing platelet aggregation onto the ULVWF multimeric strings has the potential to form large, occlusive, platelet thrombi. These strings are capable of embolising to microvessels downstream contributing to organ ischemia.
Under physiological circumstances a metalloprotease ADAMTS13 cleaves high molecular weight multimers at a Tyr-842-Met-843 bond, resulting in vWF with a molecular weight of 500 – 20000 kDA. In acquired TTP, an antibody develops against the metalloprotease and impedes the cleavage of vWF multimers while in congenital TTP, the protease is absent.
Laboratory Investigations of TTP
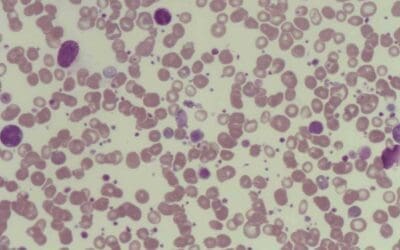
- Complete blood count (CBC): A CBC measures the levels of red blood cells, white blood cells, and platelets in the blood. In TTP, the CBC will typically show thrombocytopenia (low platelet count) and microangiopathic hemolytic anemia (MAHA), a type of anemia characterized by the presence of fragmented red blood cells (schistocytes).
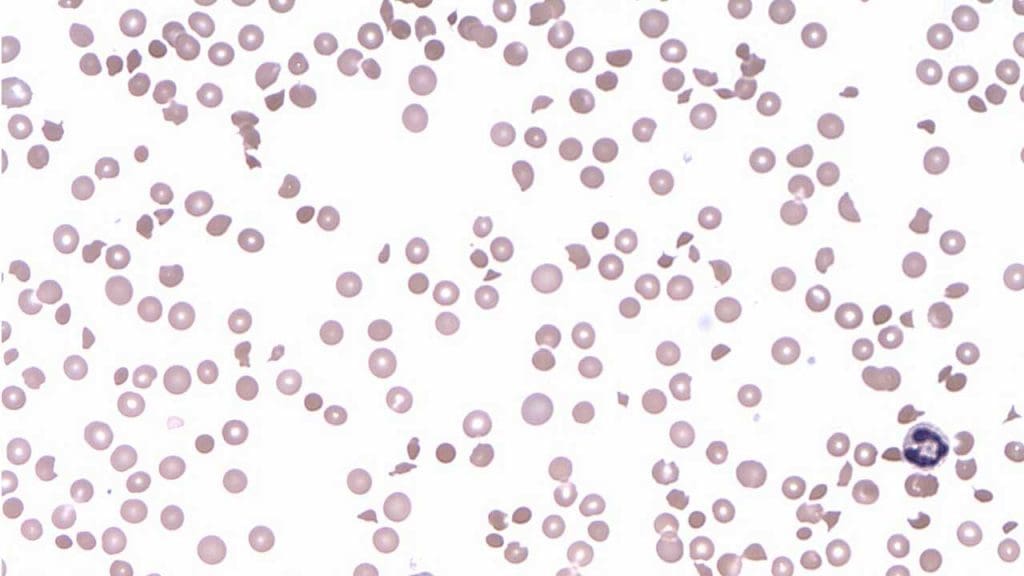
- Peripheral blood smear: A peripheral blood smear is a microscopic examination of the blood cells. In TTP, the peripheral blood smear will typically show schistocytes.
- ADAMTS13 activity assay: The ADAMTS13 activity assay measures the level of ADAMTS13 in the blood. ADAMTS13 is a protein that cleaves von Willebrand factor (VWF), a large protein that plays a role in blood clotting. In TTP, the ADAMTS13 activity level is typically low.
- ADAMTS13 inhibitor assay: The ADAMTS13 inhibitor assay detects the presence of autoantibodies that inhibit ADAMTS13 activity. Autoantibodies are antibodies that are produced by the body’s own immune system against its own tissues or cells. In acquired TTP, the most common type of TTP, autoantibodies against ADAMTS13 are present in the blood.
In current clinical practice, thrombocytopenia, schistocytosis and an impressively elevated serum LDH are sufficient to suggest the diagnosis. The bone marrow is hypercellular with erythroid hyperplasia. Coagulation tests are normal. ADAMTS13 is absent or severely reduced in plasma.
Treatment and management
The treatment and management of thrombotic thrombocytopenic purpura (TTP) is aimed at increasing the levels of ADAMTS13 in the blood and preventing the formation of microthrombi. The mainstay of treatment is plasma exchange, a procedure in which the plasma (liquid portion of the blood) is removed and replaced with fresh plasma from a donor. Plasma exchange provides a source of ADAMTS13 and also removes autoantibodies that may be inhibiting ADAMTS13 activity.
Other treatments that may be used include:
- Corticosteroids: Corticosteroids can suppress the immune system and reduce inflammation. Corticosteroids are often used in conjunction with plasma exchange in patients with acquired TTP.
- Rituximab: Rituximab is a monoclonal antibody that targets and destroys B cells, which are the type of white blood cell that produces autoantibodies. Rituximab may be used in patients with acquired TTP who have a high risk of relapse, or in patients who do not respond to plasma exchange and corticosteroids.
- Caplacizumab: Caplacizumab is a monoclonal antibody that targets and blocks von Willebrand factor (VWF), preventing platelet aggregation and microthrombus formation. Caplacizumab is a newer treatment that has been shown to be effective in reducing the mortality rate of TTP.
Key Points of TTP
Definition
Thrombocytopenia due to deficiency of ADAMTS13 metalloprotease which leads to formation of platelet thrombi in microvessels.
Signs and symptoms (pentad)
- Thrombocytopenia
- Microangiopathic hemolysis
- Neurologic dysfunction
- Renal impairment
- Fever
Causes
- Inherited mutations
- Acquired: inhibitory IgG autoantibodies stimulated by infection, autoimmune/connective tissue disease, drugs, stem cell transplantation or cardiac surgery
Pathophysiology
ADAMTS-13, an enzyme responsible for cleaving large von Willebrand factor (VWF) multimers, plays a pivotal role in maintaining the delicate balance of blood vessel integrity. In TTP, the absence of ADAMTS-13 leads to an accumulation of these large VWF multimers, creating a sticky environment that promotes platelet aggregation.
Laboratory investigations
Full blood count and peripheral blood characteristics
Full blood count: Thrombocytopenia
Peripheral blood smear: Schistocytosis
Bone marrow characteristics
Markedly hypercellular with erythroid hyperplasia
Other important investigations and expected results
- ↑↑ serum LDH
- Coagulation tests normal
- Specific assay: ADAMTS-13 ↓↓ or absent
Treatment and management of TTP
- Plasma exchange using FFP or cryosupernatant
- Rituximab
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Kovala M, Seppälä M, Kaartinen K, Meri S, Honkanen E, Räisänen-Sokolowski A. Vascular Occlusion in Kidney Biopsy Is Characteristic of Clinically Manifesting Thrombotic Microangiopathy. Journal of Clinical Medicine. 2022; 11(11):3124. https://doi.org/10.3390/jcm11113124.
- UpToDate – Diagnosis of Immune TTP.
- Nuñez Zuno JA, Khaddour K. Thrombotic Thrombocytopenic Purpura Evaluation and Management. [Updated 2023 Sep 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
- Inés Gómez-Seguí, Cristina Pascual Izquierdo, María Eva Mingot Castellano & Javier de la Rubia Comos (2023) An update on the pathogenesis and diagnosis of thrombotic thrombocytopenic purpura, Expert Review of Hematology, 16:1, 17-32, DOI: 10.1080/17474086.2023.2159803
- Rizzo C, Rizzo S, Scirè E, Di Bona D, Ingrassia C, Franco G, Bono R, Quintini G, Caruso C. Thrombotic thrombocytopenic purpura: a review of the literature in the light of our experience with plasma exchange. Blood Transfus. 2012 Oct;10(4):521-32. doi: 10.2450/2012.0122-11. Epub 2012 Jun 27. PMID: 22790258; PMCID: PMC3496241.
- Goldberg S, Hoffman J. Clinical Hematology Made Ridiculously Simple, 1st Edition: An Incredibly Easy Way to Learn for Medical, Nursing, PA Students, and General Practitioners (MedMaster Medical Books). 2021.