Procedure At a Glance
The purpose of the Direct Antiglobulin (Coombs) Test (DAT) procedure is to detect in vivo sensitization of red blood cells with antibodies or complement components.
Collect Patient Sample: Obtain an anticoagulated blood sample (e.g., in an EDTA tube) from the patient.
Wash Red Blood Cells: Thoroughly wash the patient’s RBCs with saline multiple times. This step is crucial to remove any unbound antibodies or plasma proteins that could cause interference.
Add Antihuman Globulin (AHG): Add the AHG (Coombs reagent), which contains antibodies against human IgG and/or complement components (e.g., C3d), to the washed RBCs.
Centrifuge & Observe: Centrifuge the mixture briefly to bring the cells into close proximity. Gently resuspend the cell button and visually inspect for agglutination (clumping of RBCs).
- Agglutination: Indicates a positive DAT, meaning antibodies and/or complement are coating the patient’s RBCs.
- No Agglutination: Indicates a negative DAT.
Quality Control (for negative results): If the initial test is negative, add Coombs Control Cells (also known as “check cells” or “IgG-sensitized cells”) to confirm that the AHG reagent was active and the washing steps were performed correctly. Agglutination must occur with the control cells for a valid negative result.
*Click ▾ for more information
Introduction
The Direct Antiglobulin Test (DAT), also known as the Direct Coombs Test, functions to directly detect antibodies (usually IgG) or complement proteins (like C3d) that are already attached or bound to the surface of a patient’s own red blood cells in vivo (inside the body).
It works by adding a reagent called Coombs serum (antihuman globulin) to the patient’s washed red blood cells. If antibodies or complement are coating the red blood cells, the Coombs serum will bind to them, causing the red blood cells to clump together (agglutinate), indicating a positive result.
Its primary function is to diagnose immune-mediated hemolysis, where the body’s own immune system is attacking and destroying its red blood cells, such as in autoimmune hemolytic anemia, drug-induced hemolytic anemia, or hemolytic disease of the newborn.
Coombs Test During Pregnancy
The Coombs test is crucial to be performed during pregnancy, primarily to assess the risk of hemolytic disease of the newborn (HDN), also known as erythroblastosis fetalis. This condition occurs when there’s an incompatibility between the mother’s and baby’s blood types, leading to the mother’s immune system attacking and destroying the baby’s red blood cells.
There are two main types of Coombs tests relevant to pregnancy.
- Indirect Antiglobulin (Coombs) Test (IAT): This test is performed on the mother’s blood during prenatal care, typically in the first trimester and sometimes repeated. It looks for antibodies in her serum that could cross the placenta and harm the baby. The most common concern is Rh incompatibility (e.g., an Rh-negative mother carrying an Rh-positive baby). A positive IAT indicates the mother has been sensitized and has produced such antibodies, necessitating close monitoring of the pregnancy and potentially interventions like Rh immunoglobulin (RhoGAM) if she’s not yet sensitized.
- Direct Antiglobulin (Coombs) Test (DAT): While not routinely done on the mother’s blood during pregnancy, the DAT is performed on the newborn baby’s umbilical cord blood at birth if the mother had a positive IAT or if the baby shows signs of jaundice or anemia. This test directly detects maternal antibodies that are already attached to the baby’s red blood cells, confirming that immune-mediated red blood cell destruction is occurring in the baby, which is indicative of HDN.
Coombs Test For Newborn Babies
The Coombs test for newborn babies, primarily the Direct Antiglobulin (Coombs) Test (DAT), is performed on the baby’s blood to detect if maternal antibodies have attached to and are attacking the baby’s red blood cells. It’s often performed on umbilical cord blood at birth, especially if the mother is Rh-negative, has known “atypical” antibodies, or if there’s an ABO blood type incompatibility (e.g., mother is O type, baby is A or B).
These antibodies, typically IgG from the mother, cross the placenta and can cause the baby’s red blood cells to break down (hemolysis). It’s also done if a newborn develops early or severe jaundice or signs of anemia.
A positive DAT indicates that the baby’s red blood cells are coated with maternal antibodies, confirming immune-mediated hemolysis (hemolytic disease of the newborn). This prompts close monitoring for jaundice and anemia, and may guide treatment decisions like phototherapy or, in severe cases, blood transfusions, to prevent complications like kernicterus (brain damage from high bilirubin).
Principle of Direct Antiglobulin (Coombs) Test (DAT)
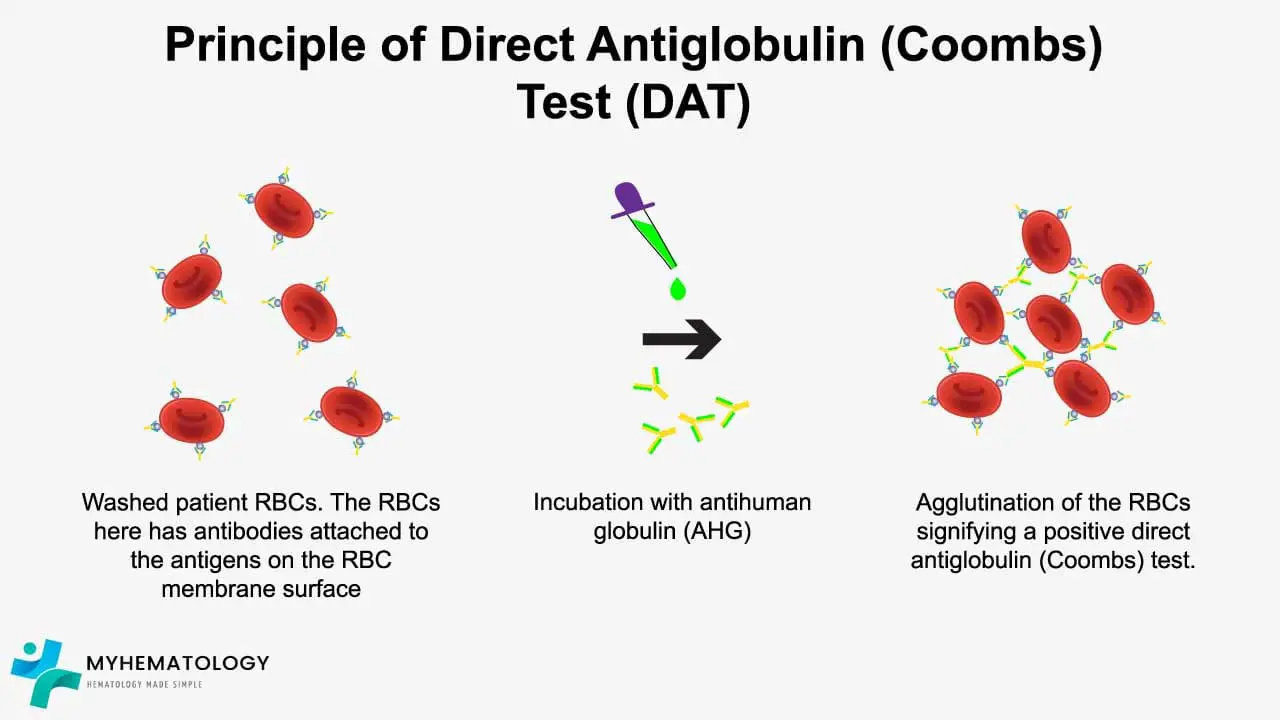
At the heart of the direct antiglobulin (Coombs) test (DAT) lies the unique property of RBCs – their negative surface charge. This charge acts like a built-in shield, repelling each other and preventing them from clumping together. However, when an antibody or complement protein binds to an RBC, it acts as a bridge, overcoming this repulsive force. This allows multiple RBCs coated with the same antibody or complement to clump together, a phenomenon called agglutination.
Antihuman globulin (AHG) is a specially designed antibody that recognizes and binds to the Fc portion of human antibodies and complement proteins. Essentially, AHG acts like a “double agent,” recognizing the immune cloak worn by the sensitized RBCs.
The direct antiglobulin (Coombs) test (DAT) protocol revolves around this interaction. The direct antiglobulin (Coombs) test (DAT) plays a crucial role in diagnosing conditions where in vivo coating of RBCs by antibodies or C3d occurs, leading to their premature destruction.
Washing the cells eliminates freely circulating antibodies, allowing for the specific detection of those directly attached to the RBCs. Then, AHG is introduced.
If the RBCs are coated with antibodies or complement, AHG binds to them, forming visible clumps. This agglutination signifies a positive direct antiglobulin (Coombs) test (DAT). This bound antibody-AHG complex formation reveals sensitized RBCs, providing valuable clues for the diagnosis of autoimmune hemolytic anemia, hemolytic disease of the newborn, drug-induced hemolysis, and other immune-mediated disorders.
A negative direct antiglobulin (Coombs) test (DAT), on the other hand, suggests the absence of bound antibodies or complement. However, this doesn’t guarantee the absence of an immune reaction. Some antibodies, particularly weak ones, may not cause visible agglutination even though they are present. This is why the direct antiglobulin (Coombs) test (DAT) has different sensitivity levels, utilizing polyspecific AHG for broad detection and monospecific AHG for identifying specific antibody types.
Materials
- Patient’s EDTA-anticoagulated blood sample
- Normal saline (0.9% NaCl)
- Antihuman globulin (AHG) reagents: polyspecific, anti-IgG, and anti-C3d
- Glass tubes
- Centrifuge
- Coombs control red cells – IgG coated red cell (CCC)
Protocol
- Prepare a red cell suspension by washing 5 mL patient RBCs with normal saline 3 – 4 times, discard the supernatant and resuspend RBCs to a 3-5% suspension in saline.
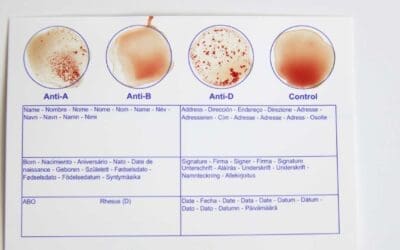
- Label four test tubes: Polyspecific, IgG, C3d, and Negative Control.
- Add one drop of RBC suspension to each tube.
- Add 2 drops of the respective AHG reagent to each tube (Polyspecific, IgG, C3d).
- Add 2 drops of saline to the Negative Control tube.
- Mix the suspension by flicking the tubes gently to thoroughly resuspend the cells.
- Centrifuge the tubes for 15-20 seconds at 1000-1500 RPM.
- Incubate Polyspecific and C3d tubes at 37°C for 5 minutes (optional).
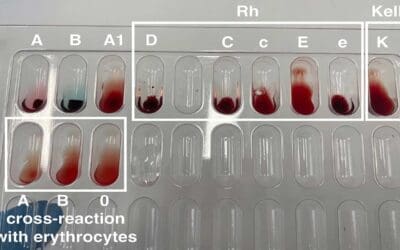
- Gently resuspend cell buttons and observe for agglutination macroscopically and microscopically.
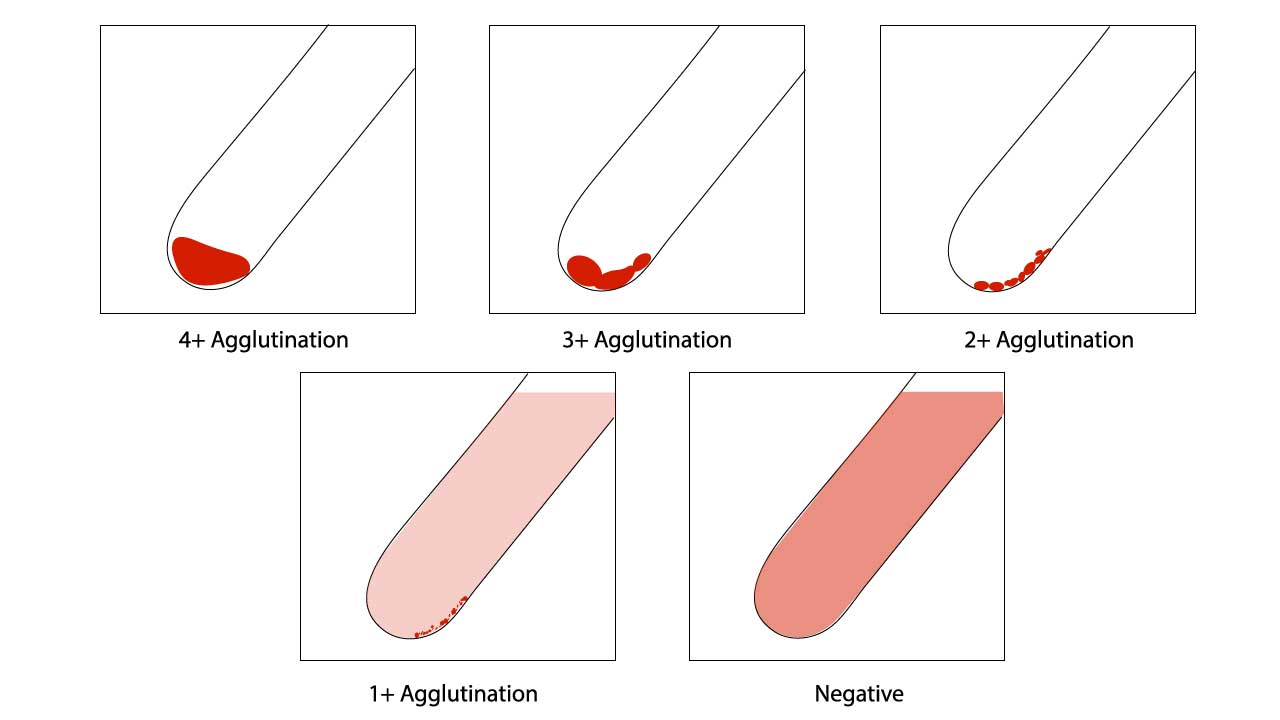
- Grade agglutination strength (0 to 4+) if present.
- In the absence of agglutination after initial centrifugation, incubate the mixture at room temperature for 5 minutes (if recommended by the manufacturer).
- Recentrifuge, resuspend, and re-assess for agglutination.
- If still negative, add Coombs control cells (CCC) and centrifuge as per manufacturer instructions. Observe and record any agglutination with CCC, confirming test validity.
Direct Antiglobulin (Coombs) Test (DAT) Interpretation
Positive Direct Antiglobulin (Coombs) Test (DAT)
Agglutination of red blood cells (RBCs) in the test indicates the presence of antibodies or complement proteins bound to the RBC surface in vivo.
Strength of agglutination (graded 0 to 4+) can provide clues about the amount of bound antibody or complement.
Specific AHG reagent used (polyspecific, anti-IgG, anti-C3d) can help narrow down the type of immune involvement.
Negative Direct Antiglobulin (Coombs) Test (DAT)
No agglutination suggests the absence of significant RBC-bound antibodies or complement. However, it does not completely rule out immune hemolysis, as weakly bound antibodies or complement may not be detected.
Clinical correlation with patient symptoms and other laboratory findings is essential.
Assessment of red cell agglutination test grading
| Symbol | Agglutination score | Description |
| 4+ / Complete (C) | 12 | Macroscopically visible cell button with a clear supernatant. |
| 3+ | 10 | Macroscopically visible large clumps of cell button with a clear supernatant. |
| 2+ | 8 | Macroscopically visible small clumps of cell button with a clear supernatant. |
| 1+ | 5 | Just macroscopically visible fine granular clumps of the cell button and the supernatant is turbid and reddish. |
| or weak (w) | 3 | Only microscopically visible fine granules of the cell button and the supernatant is turbid. |
| 0 | 0 | No agglutination seen. The supernatant is clear and reddish in color. |
| MF (mixed field) | MF | A mixture of agglutinated and unagglutinated red cells seen. |
| H | Complete hemolysis of the patient sample. The supernatant is grossly red with no evidence of red cells. |
Function of Coombs Control Cells (CCC)
- Quality control measure to ensure the validity of the direct antiglobulin (Coombs) test (DAT) reagents and technique.
- Consists of RBCs pre-coated with antibodies in the laboratory.
- Should agglutinate when mixed with AHG reagent, demonstrating its ability to detect antibody-coated RBCs.
- Negative CCC reaction with AHG suggests a technical error or reagent issue for example AHG was not added or inadequate, the reagent has expired or the AHG has been neutralized by free antibodies due to insufficient washing of the red cells.
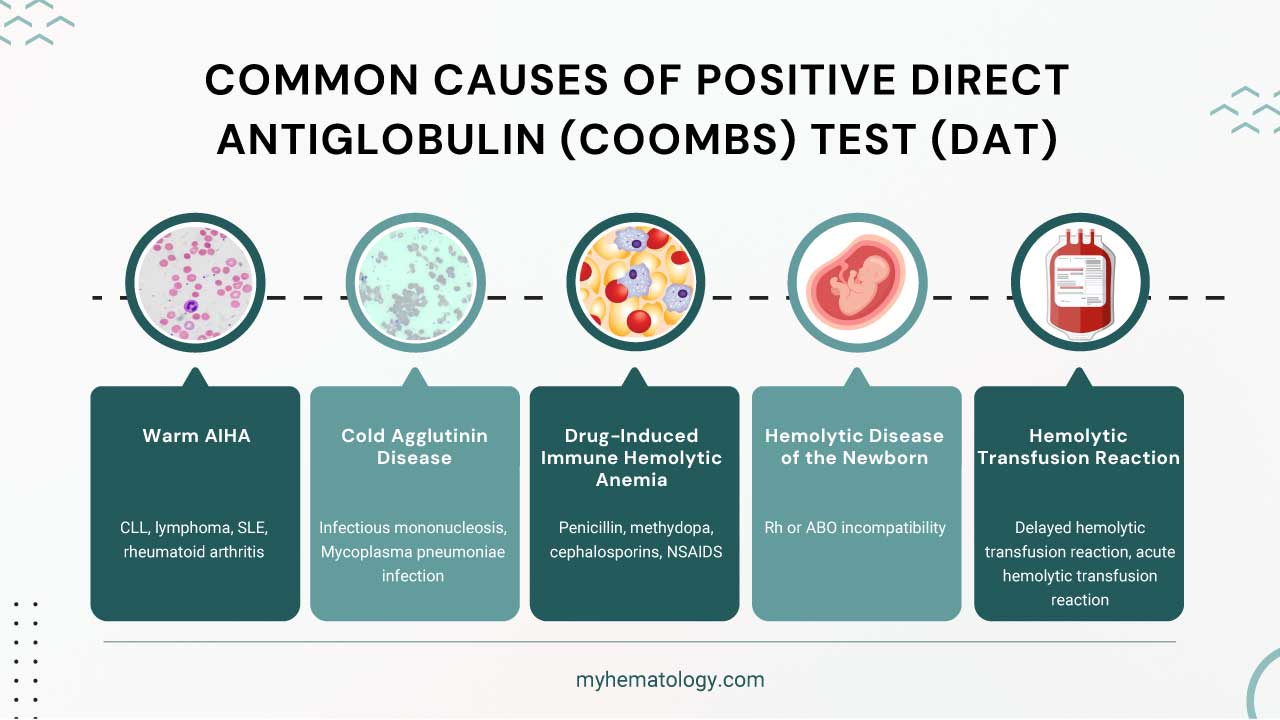
Possible Causes of Positive Direct Antiglobulin (Coombs) Test (DAT)
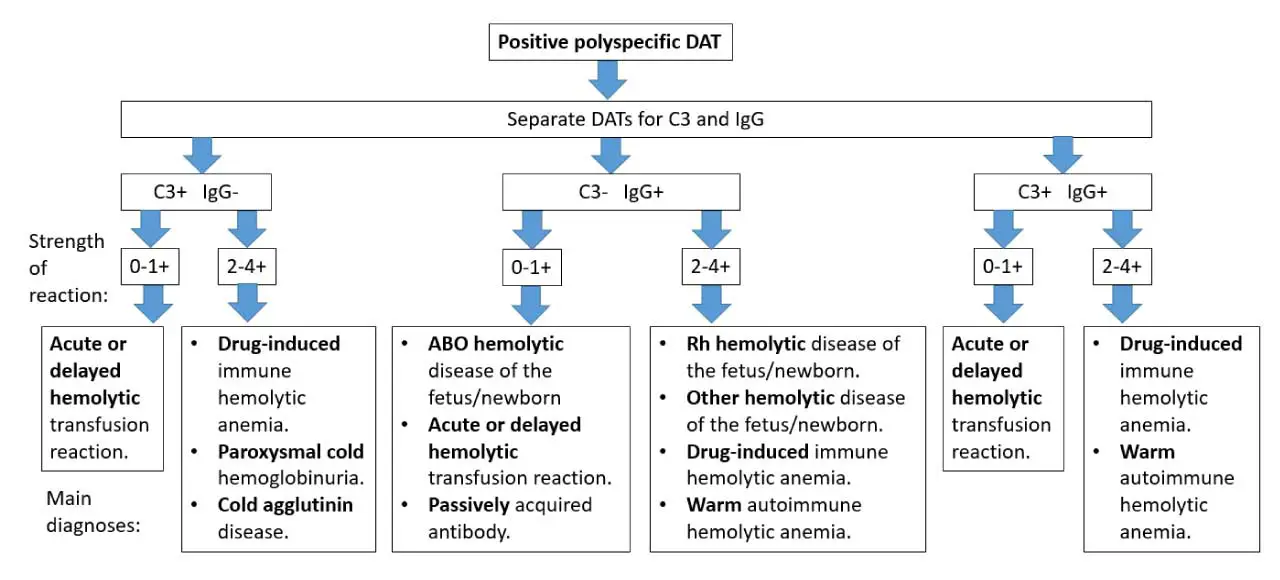
- Autoimmune hemolytic anemia (AIHA): Immune system attacks and destroys its own RBCs.
- Hemolytic disease of the newborn (HDN): Maternal antibodies attack fetal RBCs, causing hemolysis.
- Drug-induced immune hemolytic anemia (DIIHA): Certain drugs can trigger antibody formation against RBCs.
- Transfusion reactions: Incompatible blood transfusions can lead to antibody-mediated hemolysis.
- Paroxysmal cold hemoglobinuria (PCH): Cold-induced destruction of RBCs by antibodies.
- Myelofibrosis: Bone marrow disorder sometimes associated with positive direct antiglobulin (Coombs) test (DAT).
- Evans syndrome: Combination of AIHA and immune thrombocytopenia (low platelets).
- Infections: Some infections (e.g., cytomegalovirus, Epstein-Barr virus) can cause transient positive direct antiglobulin (Coombs) test (DAT).
- Solid tumors and lymphomas: Rarely associated with positive direct antiglobulin (Coombs) test (DAT).
- Allogeneic bone marrow transplantation: Immune reactions against donor RBCs can cause a positive direct antiglobulin (Coombs) test (DAT).
Frequently Asked Questions (FAQs)
What is the difference between DAT and antibody test?
The key difference between a direct antiglobulin (Coombs) test (DAT) and an antibody test lies in what they are looking for and how they approach detection.
- Direct antiglobulin (Coombs) test (DAT): This test specifically focuses on red blood cells (RBCs). It checks for antibodies that are already attached to the surface of RBCs. A positive direct antiglobulin (Coombs) test (DAT) indicates that these antibodies are binding to and potentially destroying the RBCs.
- Antibody Test (Broader Term): This is a broader term encompassing various tests that can detect different types of antibodies in the blood, not just those targeting RBCs. It can include tests like:
- Indirect Antiglobulin Test (IAT): This test, also known as the indirect Coombs test, looks for free antibodies in the blood plasma that have the potential to bind to RBCs. Unlike the direct antiglobulin (Coombs) test (DAT), these antibodies aren’t attached yet. A positive IAT indicates a risk of problems during a blood transfusion or in a newborn with hemolytic disease.
- Infectious Disease Antibody Tests: These tests detect antibodies produced by the immune system in response to a specific infection, such as HIV or hepatitis.
- Autoimmune Antibody Tests: These tests identify antibodies directed against the body’s own tissues, which can be helpful in diagnosing autoimmune diseases like lupus or rheumatoid arthritis.
What does Coombs positive mean for a baby?
A Coombs positive test result for a baby, also known as a positive direct antiglobulin test (DAT), indicates that antibodies are attached to the baby’s red blood cells (RBCs). This doesn’t necessarily mean there’s a serious problem, but it does require further investigation to determine the cause and potential risks.
Possible Reasons for Positive Coombs Test
- Rh Incompatibility: This is a major concern when a Rh-negative mother carries an Rh-positive baby. The mother’s immune system might develop antibodies against the baby’s Rh-positive RBCs, which can lead to hemolytic disease of the fetus and newborn (HDFN). HDFN can cause anemia and other complications in the baby.
- ABO Incompatibility: This is a less concerning scenario where the mother’s blood type (A, B, or AB) is incompatible with the baby’s blood type (usually O). However, unlike Rh incompatibility, ABO incompatibility rarely causes severe problems for the baby.
- Maternal Antibodies: In some cases, the mother might have pre-existing antibodies from a previous pregnancy or blood transfusion that can target the baby’s RBCs.
What Happens Next
- Further Testing: Doctors will likely perform additional tests to determine the cause of the positive direct antiglobulin (Coombs) test (DAT) and assess potential risks. This might include:
- Antibody Identification: This test pinpoints the specific antigens targeted by the antibodies in the mother’s blood.
- Evaluation of Mom’s Blood Type and Rh Status: This confirms the mother’s blood type and Rh factor.
- Fetal Blood Typing (if possible): This test, depending on the pregnancy stage and medical technology available, can determine the baby’s Rh factor and blood type, if possible.
- Amniocentesis (in some cases): This prenatal diagnostic test involves collecting a small amount of amniotic fluid to analyze fetal cells and potentially determine the baby’s Rh status. However, this is usually a later-stage option due to its invasive nature.
- Bilirubin Levels: Monitoring the baby’s bilirubin levels can help assess the severity of any potential breakdown of red blood cells.
Potential Outcomes
- Close Monitoring: If the cause is ABO incompatibility or the baby shows no signs of anemia, close monitoring of the baby’s bilirubin levels and health might be sufficient.
- Rh Incompatibility Management: If Rh incompatibility is confirmed and the baby is at risk for HDFN, doctors can take steps to prevent complications. This might involve administering Rh immunoglobulin (RhoGam) to the mother at specific intervals during pregnancy. RhoGam helps suppress her immune response and protect the baby’s red blood cells.
- Treatment for Anemia: If the baby develops anemia due to RBC destruction, they might require phototherapy treatment to help break down bilirubin or even blood transfusions in severe cases.
What does a positive Coombs test before a blood transfusion mean?
A positive Coombs test before a blood transfusion (specifically an indirect antiglobulin (Coombs) test or antibody screen) means the patient has antibodies in their blood that could react with donor red blood cells. This indicates a risk of a transfusion reaction if incompatible blood is given.
Therefore, the blood bank will need to identify these antibodies and select antigen-negative blood for the transfusion to ensure patient safety. A positive Coombs test before a blood transfusion, specifically an Indirect Antiglobulin (Coombs) Test (IAT), means that the recipient’s blood contains antibodies that could react with and destroy red blood cells from potential donors.
This signals to healthcare providers that they need to exercise caution in selecting donor blood to prevent a potentially severe transfusion reaction. It means standard blood types might not be enough, and a more specific “cross-match” with donor units is critical to find compatible blood.
What is a positive direct Coombs test without hemolysis?
A positive Direct Antiglobulin (Coombs) Test (DAT) without hemolysis means that antibodies are attached to the patient’s red blood cells, but these antibodies are not currently causing significant destruction (hemolysis) of the red blood cells.
While a positive DCT often suggests an immune-mediated problem, it doesn’t automatically mean the patient has hemolytic anemia. It can occur due to:
- Clinically insignificant antibodies: Antibodies present on the red blood cells that don’t cause significant red cell destruction.
- Drug-induced positivity: Certain medications can cause antibodies to bind to red blood cells without leading to hemolysis.
- Recent transfusion: Alloantibodies from a recent transfusion might still be present on red blood cells.
- Low antibody levels: The amount of antibody coating the red blood cells might be too low to cause noticeable hemolysis.
- Underlying conditions: Some conditions like systemic lupus erythematosus (SLE) can cause a positive DAT without active hemolysis.
- “False” positives: Less commonly, high serum protein levels or certain infections can lead to a positive result without an immune attack on red blood cells.
Therefore, a positive DAT must always be interpreted in the context of the patient’s full clinical picture, including their symptoms, other lab results (like hemoglobin, bilirubin, haptoglobin, reticulocyte count), and medical history.
Disclaimer: This protocol is intended for informational purposes only and may need to be modified depending on the specific laboratory procedures and patient circumstances. Always consult with a qualified healthcare professional for guidance. See additional information.
References
- American Association of Blood Banks (AABB). Technical Manual, 21st Edition, 2023.
- Dean L. Blood Groups and Red Cell Antigens [Internet]. Bethesda (MD): National Center for Biotechnology Information (US); 2005.
- Bain BJ, Bates I, Laffan MA. Dacie and Lewis Practical Haematology: Expert Consult: Online and Print 12th Edition (Elsevier). 2016.
- Theis SR, Hashmi MF. Coombs Test. [Updated 2022 Sep 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK547707/