TL;DR
Pancytopenia is the reduction of all three major blood cell lines: red blood cells (anemia), white blood cells (leukopenia), and platelets (thrombocytopenia). It is a clinical finding, not a disease itself, indicating an underlying issue.
Causes ▾ : The causes of pancytopenia are diverse and can be categorized into:
- Bone Marrow Disorders: Aplastic Anemia, Myelodysplastic Syndromes, Myelofibrosis, and Hematological Malignancies (Leukemia, Lymphoma).
- Nutritional Deficiencies: Vitamin B12 and folate deficiency.
- Infections: Viral (HIV, EBV), Bacterial (Tuberculosis), and Parasitic.
- Drugs and Toxins: Especially chemotherapy, leading to drug-induced myelosuppression.
- Autoimmune Conditions: Systemic Lupus Erythematosus (SLE).
Clinical Presentation ▾: Symptoms of pancytopenia depend on which cell line is most affected:
- Anemia: Fatigue, weakness, pallor, and shortness of breath.
- Leukopenia/Neutropenia: Recurrent infections and fever.
- Thrombocytopenia: Easy bruising, petechiae, and mucosal bleeding.
Laboratory Investigations ▾ : The diagnostic workup of pancytopenia is systematic:
- Initial Tests: A Complete Blood Count (CBC) confirms the diagnosis. A peripheral blood smear provides crucial morphological clues (e.g., blasts, giant platelets).
- Bone Marrow Examination: The definitive investigation, including an aspiration and biopsy, to assess cellularity and identify the underlying pathology (e.g., aplasia, infiltration).
- Supportive Care: Involves transfusions (red blood cells and platelets) and managing infections with antibiotics.
- Definitive Therapy: Is aimed at the underlying cause, such as Vitamin B12 replacement, immunosuppressive therapy or stem cell transplantation for aplastic anemia, or chemotherapy for leukemia. The prognosis is entirely dependent on the specific cause.
*Click ▾ for more information
Pancytopenia is a hematological abnormality defined by simultaneously low levels of hemoglobin (anemia), white blood cells (leukopenia, often specifically neutropenia), and platelets (thrombocytopenia). The absolute cut-off values can vary slightly between laboratories and clinical contexts, but generally include:
Supportive Care: Involves transfusions (red blood cells and platelets) and managing infections with antibiotics.
- Anemia: Hemoglobin <12 g/dL for females, <13 g/dL for males
- Leukopenia: Total white blood cell count <4.0 x 10⁹/L (often with neutropenia <1.5 x 10⁹/L)
- Thrombocytopenia: Platelet count <150 x 10⁹/L
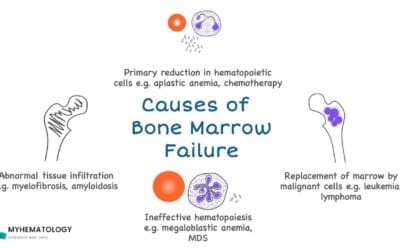
Causes of Pancytopenia
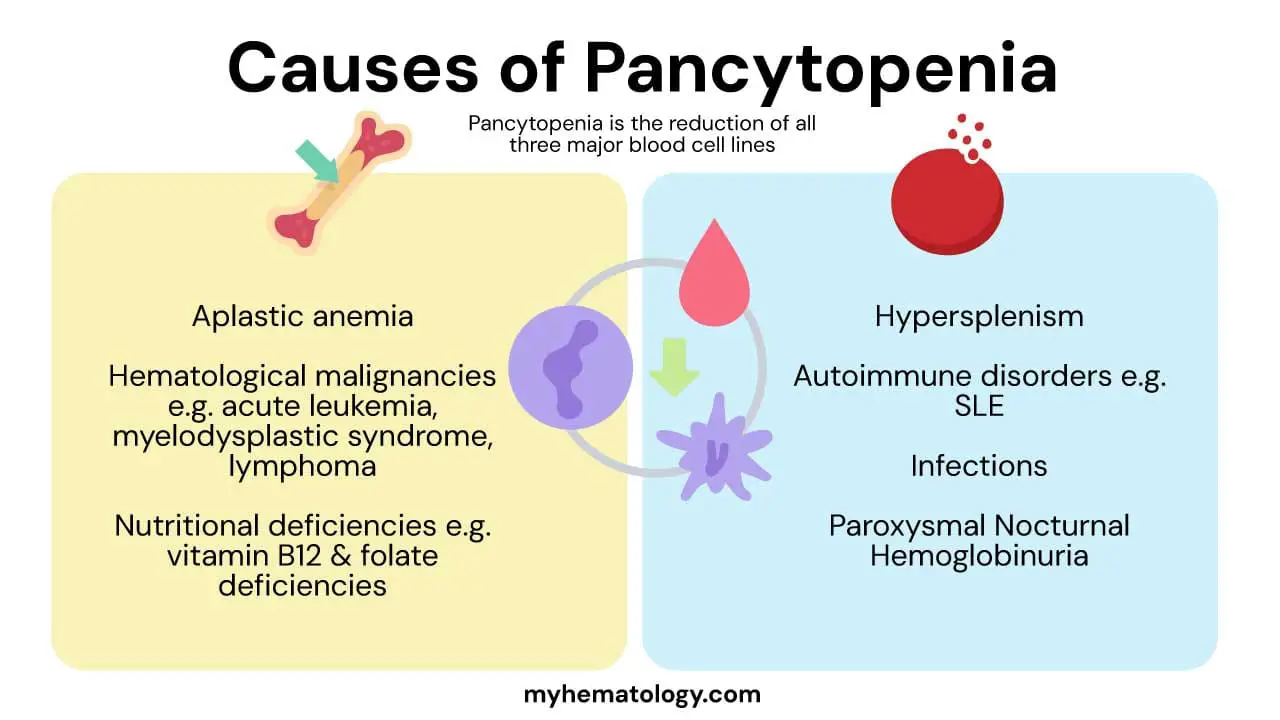
The causes of pancytopenia are diverse, but they can be broadly categorized into two main groups: decreased production in the bone marrow and increased destruction or sequestration in the peripheral blood. The following elaborates on these causes.
Decreased Production in the Bone Marrow (Bone Marrow Failure)
This is the most common mechanism leading to pancytopenia. The bone marrow’s ability to produce new blood cells is compromised.
- Aplastic Anemia: This is a condition where the bone marrow is unable to produce new blood cells because of the destruction of hematopoietic stem cells. It can be:
- Acquired: Most cases are due to an autoimmune attack where the body’s T-cells target and destroy the bone marrow’s stem cells. It can also be triggered by certain viral infections (e.g., Hepatitis, Parvovirus B19) or exposure to toxins and drugs.
- Inherited: These are rare genetic syndromes that cause bone marrow failure, such as Fanconi anemia.
- Hematological Malignancies: The bone marrow can be infiltrated and replaced by cancerous cells, leaving no room for normal blood cell production.
- Acute Leukemias: The bone marrow is filled with rapidly dividing, immature blast cells that crowd out normal hematopoietic cells.
- Myelodysplastic Syndromes (MDS): These are a group of clonal disorders of the hematopoietic stem cells that lead to ineffective hematopoiesis. The bone marrow is often overpopulated with cells, but they are defective and die before they can mature and enter the bloodstream.
- Lymphoma, Myeloma, and Metastatic Cancer: These cancers can spread to the bone marrow and physically crowd out the normal blood-forming tissue.
- Nutritional Deficiencies: The bone marrow needs specific nutrients to produce healthy blood cells. A deficiency can lead to defective cell production.
- Vitamin B12 and Folate Deficiency: This results in megaloblastic anemia, where red blood cell precursors are abnormally large and immature. This affects all cell lines, leading to pancytopenia.
Increased Destruction or Sequestration
In these cases, the bone marrow is often working correctly, but mature blood cells are being destroyed or trapped in the peripheral circulation.
- Hypersplenism: An enlarged and overactive spleen can act as an aggressive filter, trapping and prematurely destroying red blood cells, white blood cells, and platelets. This is commonly seen in patients with liver cirrhosis and portal hypertension.
- Autoimmune Disorders: The immune system mistakenly attacks and destroys the body’s own blood cells. While this often affects one cell line, diseases like Systemic Lupus Erythematosus (SLE) can trigger a broader attack that leads to pancytopenia.
- Infections: Overwhelming infections, such as sepsis, can cause pancytopenia through multiple mechanisms, including bone marrow suppression and splenic sequestration.
- Paroxysmal Nocturnal Hemoglobinuria (PNH): This is a rare, acquired disorder where a genetic mutation in hematopoietic stem cells leads to a deficiency of protective proteins on the surface of blood cells. This leaves the cells vulnerable to destruction by the body’s own immune system, particularly the complement system. PNH is unique because it combines features of both marrow failure and increased destruction.
Drug-Induced Causes
- Drug-Induced Myelosuppression: This is a common and predictable cause of pancytopenia, especially with chemotherapy drugs that are designed to inhibit cell proliferation. The effect is typically dose-dependent and reversible after the medication is stopped.
- Idiosyncratic Drug Reactions: Some drugs (e.g., chloramphenicol, certain antibiotics, and anti-seizure medications) can cause a rare, unpredictable, and severe bone marrow failure that resembles aplastic anemia.
Clinical Presentation and Symptoms of Pancytopenia

The clinical presentation and symptoms of pancytopenia are a direct result of the deficiency of each of the three major blood cell lines: red blood cells, white blood cells, and platelets. The severity of symptoms often correlates with how low the cell counts are and how quickly they have dropped.
Symptoms Due to Anemia (Low Red Blood Cells)
Anemia is a deficiency in red blood cells or hemoglobin, which is responsible for carrying oxygen. Symptoms are related to the body’s tissues not receiving enough oxygen (hypoxia).
- Fatigue and Weakness: This is the most common symptom. Patients often report feeling constantly tired, even with adequate rest.
- Pallor: The skin, mucous membranes, and nail beds may appear pale due to a lack of hemoglobin. This is often more noticeable on the palms or inner eyelids.
- Shortness of Breath (Dyspnea): Patients may feel breathless, especially during physical exertion, as the body struggles to deliver enough oxygen to the muscles.
- Cardiovascular Signs: The heart may beat faster (tachycardia) or irregularly as it tries to compensate for the reduced oxygen-carrying capacity of the blood. Severe anemia can lead to chest pain or even heart failure.
Symptoms Due to Neutropenia (Low White Blood Cells)
A low white blood cell count, particularly neutrophils, compromises the body’s immune system, making patients highly susceptible to infections.
- Fever: Often the first and only sign of a severe infection. A fever in a patient with neutropenia is considered a medical emergency (febrile neutropenia).
- Recurrent or Severe Infections: Patients may experience infections more frequently and with greater severity. Common sites of infection include the mouth (gingivitis, mouth sores), skin (cellulitis), and lungs (pneumonia).
- Lack of Inflammatory Response: Because neutrophils are a key part of the inflammatory response, patients with neutropenia may not show the typical signs of an infection, like pus formation, even when a serious infection is present.
Symptoms Due to Thrombocytopenia (Low Platelets)
A low platelet count impairs the blood’s ability to clot, leading to bleeding.
- Easy Bruising (Ecchymosis): Minor bumps or injuries can result in large, discolored bruises.
- Petechiae: These are tiny, pinpoint-sized red or purple spots on the skin caused by bleeding from small capillaries. They often appear on the legs and are a classic sign of low platelet count.
- Mucosal Bleeding: This includes bleeding from the gums, nosebleeds (epistaxis), and heavy or prolonged menstrual bleeding (menorrhagia).
- Spontaneous Bleeding: In severe cases, patients are at risk for life-threatening spontaneous bleeding, particularly in the brain (intracranial hemorrhage) or the gastrointestinal tract, which can present as blood in the urine (hematuria) or stool.
Systemic Symptoms and Clues from Physical Examination
Beyond the specific signs of each cytopenia, a thorough history and physical exam can provide clues to the underlying cause.
- Constitutional Symptoms: Fever, unexplained weight loss, and night sweats can suggest an underlying malignancy or chronic infection.
- Splenomegaly: An enlarged spleen on physical examination may suggest hypersplenism, where the spleen is trapping and destroying blood cells, or a hematological malignancy like leukemia.
- Lymphadenopathy: Enlarged lymph nodes can point to an infection, lymphoma, or other cancers.
Diagnostic Approach to Pancytopenia
A systematic and thorough diagnostic evaluation is important to uncover the underlying cause of pancytopenia.
History
Elicit information on symptoms related to anemia, infection, and bleeding. Inquire about drug exposure (prescription, over-the-counter, illicit), chemical/toxin exposure, travel history (endemic infections), family history of hematologic disorders, autoimmune conditions, and pre-existing medical conditions.
Physical Examination
Assess for pallor, jaundice, petechiae, purpura, ecchymoses, lymphadenopathy, hepatomegaly, splenomegaly, and signs of infection.
Initial Blood Tests and Analysis
- Complete Blood Count (CBC) with Differential: This test confirms the low counts of red blood cells, white blood cells, and platelets. The differential provides a breakdown of the different types of white blood cells. A very low absolute neutrophil count (ANC) is a key concern.
- Peripheral Blood Smear: A manual review of a blood sample under a microscope is essential. This can reveal vital information not provided by an automated CBC, such as:
- Abnormal cell morphology: The presence of large, immature red blood cells (macrocytosis) suggests a nutritional deficiency. Teardrop-shaped red blood cells might indicate myelofibrosis.
- Immature cells: The presence of blast cells (immature white blood cells) is a strong indicator of acute leukemia.
- Infiltrating cells: The presence of abnormal lymphocytes or other cells can point to a lymphoma or metastatic cancer.
- Reticulocyte Count: This test measures the number of immature red blood cells in the blood. A low reticulocyte count in a patient with anemia suggests a problem with the bone marrow’s production capability (e.g., aplastic anemia or leukemia). A high count, in contrast, would point toward a peripheral cause like hypersplenism or immune destruction.
Targeted Blood Tests
Based on the initial findings from the CBC and smear, additional blood tests are ordered to rule out specific causes.
- Nutritional Studies: If the peripheral smear shows macrocytic anemia (large red blood cells), testing for Vitamin B12 and folate levels is critical, as deficiencies can cause pancytopenia and are easily treatable.
- Liver and Renal Function Tests: Abnormalities here can indicate liver disease leading to hypersplenism or kidney failure.
- Infection Serology: Tests for viruses such as HIV, Epstein-Barr Virus (EBV), and Hepatitis are important, as these infections can directly suppress bone marrow function.
- Autoimmune Markers: If an autoimmune condition is suspected, tests for markers like antinuclear antibodies (ANA) for Systemic Lupus Erythematosus (SLE) may be performed.
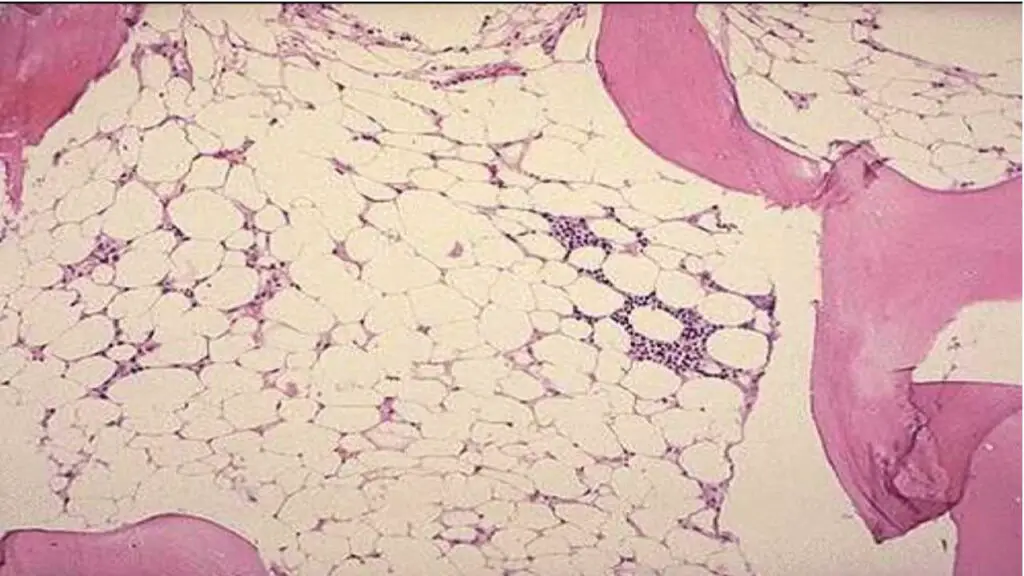
The Definitive Investigation: Bone Marrow Examination
When the initial workup fails to provide a clear diagnosis, a bone marrow examination is the gold standard and is considered a mandatory step. It allows for a direct look at the “factory” of blood cell production.
- Bone Marrow Aspiration: A liquid sample of bone marrow is withdrawn from the iliac crest (hip bone). This sample is used to assess:
- Cellularity: The ratio of hematopoietic cells to fat cells. This can show if the marrow is hypocellular (e.g., aplastic anemia) or hypercellular (e.g., leukemia, myelodysplastic syndrome).
- Cell Morphology: The maturation and appearance of the different cell lineages are examined to look for signs of dysplasia (abnormal development) or the presence of malignant cells.
- Bone Marrow Biopsy: A small, solid core of bone marrow is taken. This provides an important architectural view of the marrow that aspiration cannot. It is essential for:
- Assessing Cellularity and Fibrosis: It provides a better estimate of overall cellularity and can detect conditions like myelofibrosis, where scar tissue replaces normal marrow.
- Detecting Infiltration: It is the best way to identify subtle infiltration by cancer cells (e.g., metastatic carcinoma or lymphoma) or granulomas from infections like tuberculosis.
Advanced Diagnostic Tools
Once the bone marrow samples are collected, further specialized tests are performed to refine the diagnosis and guide treatment.
- Cytogenetics and Molecular Studies: Chromosomal analysis of bone marrow cells can detect specific abnormalities that are characteristic of certain diseases, such as the specific genetic mutations seen in Myelodysplastic Syndromes (MDS) and Acute Myeloid Leukemia (AML).
- Flow Cytometry: This technique analyzes the surface proteins on blood cells. It is invaluable for identifying and classifying different types of leukemia and lymphoma. For example, it can detect the absence of the CD55 and CD59 proteins, which is diagnostic for Paroxysmal Nocturnal Hemoglobinuria (PNH).
Clinical Guidelines and Management Principles
The treatment and management of pancytopenia depend entirely on the underlying cause. Because pancytopenia is a symptom, not a disease, a correct and timely diagnosis is the first and most crucial step. Management involves a combination of supportive care and definitive, cause-specific therapy.
Supportive Care
Supportive care aims to manage the immediate symptoms and risks associated with low blood counts, regardless of the underlying cause.
- Red Blood Cell Transfusions: Used to treat severe anemia. This can alleviate symptoms like fatigue and shortness of breath and prevent cardiovascular complications. Transfusions are given when hemoglobin levels drop below a certain threshold or if the patient is symptomatic.
- Platelet Transfusions: Administered to prevent or stop bleeding in patients with severe thrombocytopenia. They are typically given to patients with very low platelet counts or those who are actively bleeding before a procedure.
- Granulocyte-Colony Stimulating Factor (G-CSF): For patients with severe neutropenia (low neutrophil count), G-CSF can be used to stimulate the bone marrow to produce more white blood cells. This helps reduce the risk of severe bacterial and fungal infections.
- Infection Management: Prophylactic antibiotics or antifungal agents may be used in patients with severe, prolonged neutropenia. Any fever in a neutropenic patient is a medical emergency requiring immediate hospitalization and broad-spectrum antibiotics until the cause is identified.
Cause-Specific Treatment
Once the diagnosis is established, definitive treatment is initiated to address the root cause of the pancytopenia.
- Nutritional Deficiencies: Pancytopenia caused by Vitamin B12 or folate deficiency is easily and effectively treated with replacement therapy. Once the deficiency is corrected, the bone marrow typically recovers, and blood counts return to normal.
- Aplastic Anemia: For younger, otherwise healthy patients with a matched sibling donor, allogeneic hematopoietic stem cell transplantation (HSCT) is the definitive cure. For patients without a suitable donor, or those who are older, immunosuppressive therapy (IST) using drugs like antithymocyte globulin (ATG) and cyclosporine is the standard treatment.
- Leukemia and other Malignancies: The treatment for leukemia is a complex regimen of chemotherapy, targeted therapy, immunotherapy, and in some cases, HSCT. The goal is to kill the malignant cells in the bone marrow and allow normal blood production to resume.
- Myelodysplastic Syndromes (MDS): Treatment depends on the risk level of the disease. Lower-risk patients may be managed with supportive care, while higher-risk patients may receive hypomethylating agents or, if eligible, HSCT.
- Infections: If pancytopenia is due to a viral, bacterial, or parasitic infection, treating the underlying infection with antiviral, antibiotic, or antiparasitic drugs is key. The pancytopenia will often resolve as the infection clears.
- Drug-Induced Myelosuppression: The most straightforward management is to discontinue the offending medication. For cancer patients on chemotherapy, this may involve adjusting the dose or delaying the next cycle to allow the bone marrow to recover.
- Autoimmune Conditions: If pancytopenia is caused by an autoimmune disease like SLE, treatment involves managing the underlying disease with immunosuppressive drugs such as corticosteroids, cyclophosphamide, or rituximab.
Monitoring and Prognosis
Patients with pancytopenia require close and continuous monitoring of their blood counts. The prognosis is highly variable and depends entirely on the underlying cause. For reversible conditions like nutritional deficiencies, the prognosis is excellent. For others, like aplastic anemia or acute leukemia, the prognosis is much more guarded and depends on the response to specific therapies.
Conclusion
Pancytopenia represents a critical finding demanding a thorough diagnostic workup. Its diverse etiologies range from benign and treatable conditions like vitamin deficiencies to severe bone marrow failure syndromes and malignancies. A systematic approach, integrating clinical history, physical examination, comprehensive laboratory tests, and crucially, bone marrow examination with advanced molecular diagnostics, is essential. Timely and accurate diagnosis paves the way for specific, often life-saving, interventions and optimal supportive care, improving patient outcomes and prognosis.
Frequently Asked Questions (FAQs)
What are the most common initial symptoms of pancytopenia?
Patients typically present with symptoms related to the specific cell line deficiencies: fatigue, pallor, and shortness of breath (anemia); recurrent infections or fever (leukopenia/neutropenia); and easy bruising, petechiae, or bleeding (thrombocytopenia).
Is pancytopenia always indicative of a serious underlying condition?
While pancytopenia can be caused by serious conditions like aplastic anemia or leukemia, it can also result from treatable causes such as severe vitamin deficiencies (B12, folate). A thorough diagnostic workup is essential to determine the severity and underlying etiology.
How long does it take to diagnose the cause of pancytopenia?
The diagnostic timeline varies widely. Simple cases like vitamin deficiencies can be diagnosed quickly with blood tests. More complex conditions like bone marrow failure syndromes or leukemias require bone marrow examination and specialized genetic testing, which can take several days to a few weeks for comprehensive results.
Can diet impact pancytopenia?
Yes, in cases where pancytopenia is due to nutritional deficiencies (e.g., severe vitamin B12 or folate deficiency), dietary changes and supplementation are crucial parts of the treatment. However, most causes of pancytopenia are not primarily diet-related.
What is the role of a bone marrow biopsy in diagnosing pancytopenia?
A bone marrow biopsy is often critical. It allows clinicians to assess the cellularity of the marrow, identify abnormal cells (like blasts or metastatic cancer cells), detect fibrosis, and perform cytogenetic and molecular studies, all of which are vital for an accurate diagnosis and prognosis.
Glossary of Medical Terms
- Anemia: A condition in which the blood lacks healthy red blood cells, leading to reduced oxygen delivery to the body’s tissues.
- Aplastic Anemia: A rare and serious condition in which the bone marrow fails to produce enough blood cells.
- Cytopenia: A reduction in the number of blood cells (e.g., leukopenia, neutropenia, thrombocytopenia, anemia).
- Dysplasia: Abnormal development or growth of cells, often seen in myelodysplastic syndromes.
- Erythrocytes: Red blood cells, responsible for oxygen transport.
- Hematopoiesis: The process of blood cell formation in the bone marrow.
- Hematopoietic Stem Cells (HSCs): Immature cells that can develop into all types of blood cells.
- Hypersplenism: A condition characterized by an enlarged spleen that leads to the premature destruction of blood cells.
- Leukocytes: White blood cells, essential for the immune system.
- Leukopenia: A reduction in the total number of white blood cells.
- Megaloblastic Anemia: Anemia characterized by very large red blood cells, often due to vitamin B12 or folate deficiency.
- Myelodysplastic Syndromes (MDS): A group of cancers in which immature blood cells in the bone marrow do not mature or become healthy blood cells.
- Neutropenia: A type of leukopenia specifically referring to a low count of neutrophils (a type of white blood cell).
- Pancytopenia: A condition in which there is a reduction in all three major blood cell lines: red blood cells, white blood cells, and platelets.
- Pathophysiology: The functional changes associated with a disease or injury.
- Platelets (Thrombocytes): Small, colorless cell fragments in our blood that form clots and stop or prevent bleeding.
- Splenomegaly: Enlargement of the spleen.
- Thrombocytopenia: A condition in which you have a low blood platelet count.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Chiravuri S, De Jesus O. Pancytopenia. [Updated 2023 Aug 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563146/
- Chew, S., & Kamangar, M. (2024). Approach to pancytopenia: From blood tests to the bedside. Clinical medicine (London, England), 24(5), 100235. https://doi.org/10.1016/j.clinme.2024.100235
- Sharma, R., & Nalepa, G. (2016). Evaluation and Management of Chronic Pancytopenia. Pediatrics in review, 37(3), 101–113. https://doi.org/10.1542/pir.2014-0087
- Barry, M., Chandra, S., & Hymes, K. B. (2018). Cytopenias in Transplant Patients. Principles and Practice of Transplant Infectious Diseases, 199–207. https://doi.org/10.1007/978-1-4939-9034-4_10
- Massimino, M., Iaquinta, F. S., Naty, S., Andreozzi, F., & Grembiale, R. D. (2023). Persistent Pancytopenia as a Long-COVID Manifestation in a Patient with Adult-Onset Still’s Disease: A Case Report. Medicina (Kaunas, Lithuania), 59(7), 1349. https://doi.org/10.3390/medicina59071349
- Ueki, Y., Suzuki, M., Horikawa, Y., Watanabe, H., Yamaguchi, Y., Morita, C., Tsukada, A., Takumida, H., Kusaba, Y., Katsuno, T., Tsujimoto, Y., Sakamoto, K., Hashimoto, M., Terada, J., Ishii, S., Takasaki, J., Naka, G., Iikura, M., Izumi, S., Takeda, Y., … Sugiyama, H. (2020). Pembrolizumab-induced pancytopenia in a patient with squamous cell lung cancer. Thoracic cancer, 11(9), 2731–2735. https://doi.org/10.1111/1759-7714.13582