TL;DR
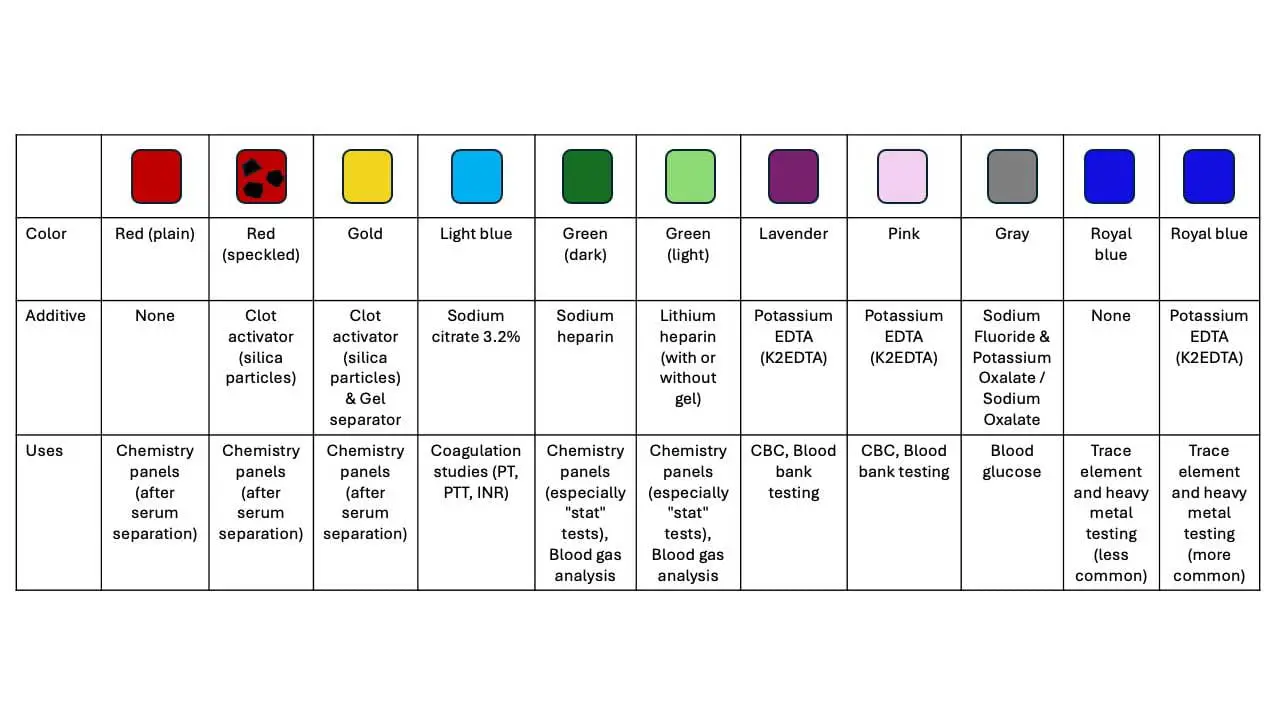
| Blood Tube Top Color | Additive | Mode of Action | Commonly Associated Tests |
| Red (Plain) | None | N/A (allows natural clotting) | Chemistry panels (after serum separation) |
| Red (Speckled) | Clot activator (silica particles) | Promotes clotting | Chemistry panels (after serum separation) |
| Gold | Clot activator (silica particles) & Gel separator | Promotes clotting & Separates serum from RBCs after centrifugation | Chemistry panels (after serum separation) |
| Light Blue | Sodium citrate 3.2% | Binds calcium ions, preventing clotting | Coagulation studies (PT/INR, aPTT) |
| Green (Darker) | Sodium heparin | Inhibits thrombin formation, preventing clotting | Chemistry panels (especially “stat” tests), Blood gas analysis |
| Green (Lighter) | Lithium heparin (with or without gel) | Similar to sodium heparin | Chemistry panels (especially “stat” tests), Blood gas analysis |
| Lavender | Potassium EDTA (K2EDTA) | Binds calcium ions, preventing clotting | Hematology (CBC), Blood bank testing |
| Pink | Potassium EDTA (K2EDTA) | Similar to lavender top | Hematology (CBC), Blood bank testing |
| Gray | Sodium Fluoride & Potassium Oxalate / Sodium Oxalate | Sodium Fluoride: inhibits glycolysis; Potassium Oxalate/Sodium Oxalate: binds calcium to prevent clotting | Blood glucose, Blood alcohol (sometimes) |
| Royal Blue (No Additive) | None | N/A (relies on natural clotting) | Trace element and heavy metal testing (less common) |
| Royal Blue (EDTA) | Potassium EDTA (K2EDTA) | Similar to lavender/pink top | Trace element and heavy metal testing (more common) |
Introduction to Blood Tube (Vacutainer)
Blood tests are a cornerstone of modern medicine, providing vital information for diagnosis, monitoring treatment, and overall health assessment. However, the accuracy of these tests hinges heavily on proper blood collection technique and the use of the right blood tube or vacutainer with their specific additives.
Function & Additives
Blood tubes, often referred to by the brand name “Vacutainers,” are sterile, evacuated (vacuum-sealed) tubes made of glass or plastic. Blood tube (Vacutainer) is designed to draw a precise, predetermined volume of blood directly from a patient’s vein for various laboratory tests.
Key features include:
- Vacuum: The internal vacuum facilitates the automatic drawing of blood into the blood tube (vacutainer).
- Color-coded stoppers: The rubber or plastic stoppers are color-coded to indicate the type of additive (or lack thereof) inside the blood tube (vacutainer).
- Additives: These substances preserve the blood sample in the blood tube (vacutainer) and prepare it for specific analyses.
- Clot activators: Promote clotting for serum separation using serum separator tube (vacutainer).
- Anticoagulants: Prevent clotting for whole blood or plasma analysis (e.g., sodium citrate, heparin, EDTA). These work by different mechanisms, like binding calcium (essential for clotting) or inhibiting clotting factors.
- Other additives: Some blood tubes (vacutainers) may contain additional components like gel separators (to isolate serum after centrifugation) or specific inhibitors (e.g., sodium fluoride in gray-top blood tube (vacutainer) to preserve glucose levels during transport).
- System components: They are typically used as part of a blood collection system that includes a double-ended needle (one end for the patient’s vein, the other for the tube stopper) and a holder to secure the blood tube (vacutainer) during collection.

Blood tubes (vacutainers) are not simply containers; they play a critical role in maintaining sample quality. By using the correct blood tube (vacutainer) and handling it appropriately, we ensure optimal blood sample quality, leading to:
- Accurate test results: Reliable test results are crucial for informed clinical decisions and patient care.
- Improved patient outcomes: Accurate diagnoses and timely treatment interventions can significantly impact patient well-being.
- Cost-effectiveness: Avoiding unnecessary repeat tests due to pre-analytical errors saves healthcare resources.
Why does proper collection matter?
Minimizing pre-analytical errors: Blood collection is the first step in the testing process. Errors at this stage can significantly impact the results, leading to misdiagnosis, unnecessary interventions, or delays in treatment.
Ensuring sample integrity: Blood is a complex mixture of cells and components. Proper collection methods and tubes help maintain the sample’s integrity, preventing contamination, hemolysis (red blood cell destruction), or activation of unwanted cellular processes that can alter test results.
Common Blood Collection Tubes (Vacutainers)
Serum Separator Tube (SST)
Serum Separator Tube (SST) is often recognized by gold, red-and-gold, or marbled red-and-grey stopper (though specific colors can vary by manufacturer). A Serum Separator Tubes (SST) is a specialized blood tube (vacutainer) designed to efficiently separate blood serum from cellular components for a wide range of laboratory tests requiring serum.
Color Tops of Serum Separator Tube
- Red (plain): No additives in the blood tube (vacutainer), allows for natural clotting.
- Red with clot activator (speckled): Contains silica particles that promote clotting.
- Gold (with gel): Similar to the red speckled top blood tube with clot activator, but also includes a gel separator that aids in separating serum from red blood cells after centrifugation.
Additives of Serum Separator Tube
- Plain red top: None.
- Red speckled top and Gold top: The inner wall of a serum separator tube is coated with very fine, micronized silica particles (clot activator). These particles are crucial because they provide a surface that activates the coagulation cascade in the blood. This accelerates the clotting process, ensuring that the blood clots quickly and completely after collection.
Mode of Action of Serum Separator Tube
- Plain red top: Blood clots naturally without any additives.
- Red speckled top: Silica particles activate the clotting cascade.
- Gold top: It has silica particles to activate the clotting cascade. The gel separator in the gold top blood tube (vacutainer) acts as a physical barrier after centrifugation, isolating the clear serum layer above the clot and red blood cells.
Clotting Time for Serum Separator Tube
Allow blood to clot in the blood tube (vacutainer) completely before centrifugation. This typically takes 15-30 minutes at room temperature. Insufficient clotting can lead to hemolysis (red blood cell rupture) and contaminate the serum.
In the gel separator tubes, once centrifugation is complete and the centrifuge stops, the gel solidifies again. This creates a stable, clear barrier. It will effectively separates the serum from the clot, preventing re-mixing and allowing for easy aspiration of the pure serum without contamination from cellular elements.
Commonly Associated Tests for Serum Separator Tube
- Routine Chemistry Panels: Such as liver function tests, kidney function tests, electrolyte panels, glucose, cholesterol, and lipid profiles uses serum separator tube.
- Hormone Level Tests: Including thyroid hormones, reproductive hormones, and other endocrine markers.
- Serology and Immunology Tests: For detecting antibodies (e.g., for infectious diseases, autoimmune disorders), and certain proteins.
- Therapeutic Drug Monitoring (TDM): Although caution is sometimes advised as some drugs or hormones can diffuse into the gel, newer serum separator tube formulations aim to minimize this.
- Tumor Markers: Used in oncology for diagnosis and monitoring.
Additional Notes
While plain red top serum separator tube (vacutainer) can be used, the red-speckled top serum separator tube is more common as they ensure complete clotting even with slight variations in collection technique.
Gel serum separator tube (gold top) is generally preferred for routine chemistry testing as they simplify the separation process and minimize handling time.
Coagulation Blood Tube (Vacutainer) (Light Blue Top)
Coagulation blood tube (vacutainer), also known as citrate blood tube, is specifically designed for tests that assess blood clotting function.
Color Top: Light Blue
Additive: Sodium citrate 3.2%
Mode of Action: Sodium citrate works by chelating (binding to) calcium ions (Ca2+) in the blood. Calcium is an essential cofactor for many steps in the coagulation cascade. By removing the free calcium, sodium citrate effectively halts the clotting process. The anticoagulation provided by sodium citrate is reversible. In the laboratory, when coagulation tests are performed, calcium is intentionally added back to the plasma, allowing the clotting process to be initiated and measured.
After blood collection, the blood tube needs to be gently inverted several times to prevent hemolysis and to ensure proper mixing of the blood with the sodium citrate.
Coagulation tubes are essential for monitoring patients with bleeding disorders, those on anticoagulant medications, or undergoing procedures that require blood clotting control.
Commonly Associated Tests
- Prothrombin Time (PT) / International Normalized Ratio (INR):
- PT: Measures the time it takes for plasma to clot after the addition of tissue factor and calcium. It primarily assesses the extrinsic and common pathways of coagulation.
- INR: A standardized way to report PT results, especially important for monitoring patients on oral anticoagulant therapy like warfarin.
- Activated Partial Thromboplastin Time (APTT or PTT): Measures the time it takes for plasma to clot after the addition of an activator (like phospholipid) and calcium. It primarily assesses the intrinsic and common pathways of coagulation and is used to monitor unfractionated heparin therapy.
- D-dimer: A test that measures the presence of D-dimer, a protein fragment produced when a blood clot is broken down. Elevated levels can indicate recent or ongoing clotting activity, often used in the diagnosis of deep vein thrombosis (DVT) or pulmonary embolism (PE).
- Fibrinogen: Measures the concentration of fibrinogen, a key protein involved in clot formation.
- Specific Coagulation Factor Assays: Tests to measure the levels and activity of individual clotting factors (e.g., Factor VIII, Factor IX).
Heparin Blood Tube (Green Top)
Heparin tubes are another type of blood tube (vacutainer) used for tests requiring whole blood or plasma analysis.
Color Top: Green (darker shade for sodium heparin, lighter shade for lithium heparin)
Additive: Sodium heparin or lithium heparin (may be present with or without a gel separator)
Mode of Action: Heparin functions as an anticoagulant by enhancing the activity of a naturally occurring enzyme inhibitor called antithrombin III (ATIII).
When heparin binds to ATIII, it causes a conformational change that dramatically increases ATIII’s ability to inactivate key clotting factors, particularly thrombin (Factor IIa) and Factor Xa. By inhibiting these factors, heparin effectively blocks the coagulation cascade, preventing the formation of a fibrin clot.
Commonly Associated Tests
- Clinical Chemistry Tests (Plasma):
- Electrolyte panels (sodium, potassium, chloride, bicarbonate)
- Renal function tests (urea, creatinine)
- Liver function tests (ALT, AST, ALP, bilirubin)
- Enzyme assays (e.g., amylase, lipase, creatine kinase)
- Glucose (especially for rapid glucose measurements, though grey top tubes are preferred for delayed glucose testing)
- Lipid profiles (cholesterol, triglycerides)
- Proteins (total protein, albumin)
- Some hormone assays
- Blood Gas Analysis (Whole Blood): Crucial for measuring pH, partial pressure of oxygen (pO2), partial pressure of carbon dioxide (pCO2), and bicarbonate levels, as heparin ensures the blood remains liquid without altering gas levels.
- Cytogenetics/Karyotyping: Heparin is often the anticoagulant of choice for preserving cells for chromosome analysis.
EDTA Blood Tube (Lavender or Pink Top)
EDTA (Ethylenediaminetetraacetic acid) tubes are among the most commonly used blood tubes in clinical laboratories, primarily for hematology. They are typically identified by their lavender or purple stoppers, although pink and royal blue tops can also contain EDTA for specific trace element or blood banking applications.
One of the most significant advantages of EDTA is its ability to preserve the cellular components of blood (red blood cells, white blood cells, and platelets) with minimal morphological changes for an extended period after collection (typically up to 24 hours at room temperature, longer if refrigerated). This makes them ideal for tests that require detailed examination of blood cells.
Color Top: Lavender or Pink
Additive: Potassium EDTA (K2EDTA)
Mode of Action: EDTA functions as an anticoagulant by chelating calcium ions. Similar to sodium citrate in coagulation tubes (vacutainers), calcium plays a critical role in blood clotting. Calcium is an absolute requirement for almost all steps in the blood coagulation cascade.
By effectively removing free calcium from the blood sample, EDTA prevents the blood from clotting. This binding is irreversible, meaning the blood will not clot again even if calcium is later added.
Prolonged tourniquet application during blood collection can lead to artificial cell activation and potentially alter some test results.
Commonly Associated Tests
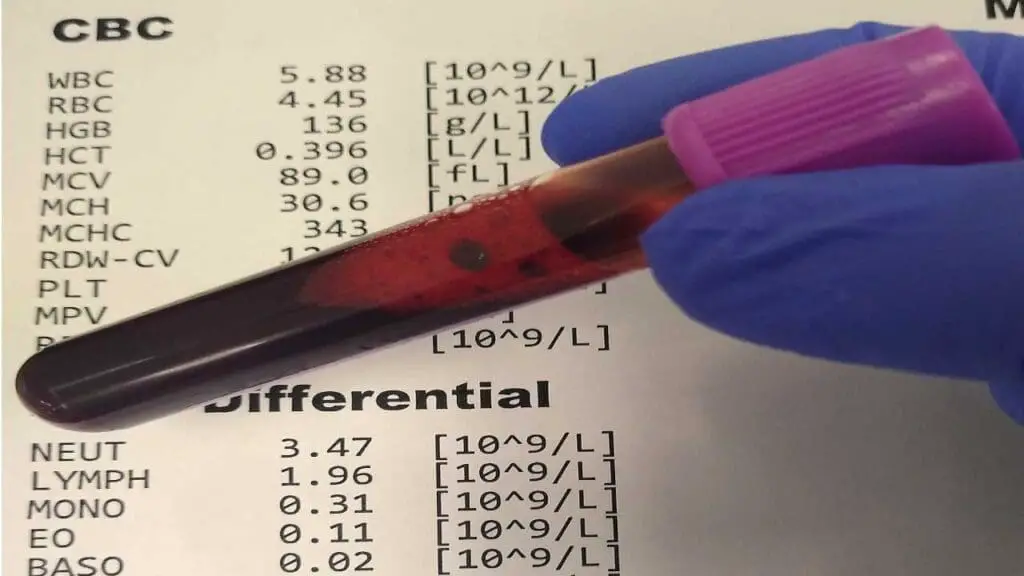
- Complete Blood Count (CBC): This is the most common test performed using an EDTA tube.
- Erythrocyte Sedimentation Rate (ESR): Measures the rate at which red blood cells settle in a vertical tube, used as a non-specific indicator of inflammation.
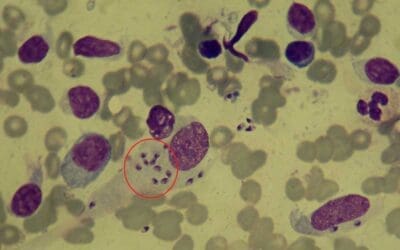
- Blood Film/Smear Examination: For microscopic examination of blood cell morphology (shape, size, abnormalities), crucial for diagnosing various blood disorders, infections, or parasitic diseases (e.g., malaria).
- Hemoglobin A1c (HbA1c): Measures average blood glucose levels over the past 2-3 months, primarily for diabetes monitoring.
- Blood Typing and Cross-matching: Essential for determining blood group (ABO and Rh type) and for ensuring compatibility between donor and recipient blood for transfusions.
- Molecular Diagnostics: EDTA-treated blood samples are excellent for DNA and RNA extraction, making them vital for genetic testing, PCR, and viral load detection.
- Direct Coombs Test (Direct Antiglobulin Test): Detects antibodies attached to the surface of red blood cells, used in diagnosing autoimmune hemolytic anemia and transfusion reactions.
Sodium Fluoride/Potassium Oxalate Blood Tube (Gray Top)
Sodium Fluoride/Potassium Oxalate (NaF/K Oxalate) tubes, typically identified by their grey stoppers, are specialized blood tubes primarily designed for the accurate measurement of glucose and lactate levels. Their unique combination of additives serves two critical purposes: anticoagulation and, more importantly, the inhibition of glycolysis.
The primary advantage of this blood tube is the stabilization of glucose levels in the blood sample for an extended period (up to 24 hours at room temperature, longer if refrigerated). This is critical for accurate diagnosis and monitoring of diabetes, especially when samples cannot be processed immediately.
Sodium fluoride also helps stabilize lactate levels, as lactate is a product of glycolysis. This is important for tests measuring lactate, which can be an indicator of tissue hypoxia or metabolic acidosis.
Color Top: Gray
Additives: This tube can contain two possible combinations:
- Sodium Fluoride & Potassium Oxalate
- Sodium Oxalate (alone)
Mode of Action: The combination of additives works in two ways:
- Sodium Fluoride: This is the distinguishing feature of these blood tubes. Sodium fluoride acts as an antiglycolytic agent, meaning it inhibits the process of glycolysis. Glycolysis is the metabolic pathway by which glucose (sugar) is broken down by blood cells (especially red blood cells and white blood cells) to produce energy. If glycolysis is not inhibited, the glucose in a collected blood sample will be consumed by the cells, leading to a falsely decreased glucose reading over time, particularly if there’s a delay in processing the sample.
- Potassium Oxalate (or Sodium Oxalate): Acts as an anticoagulant by chelating calcium ions, similar to EDTA and sodium citrate in other tubes (vacutainers). This prevents clotting and preserves the cellular components of the blood.
Commonly Associated Tests
- Blood Glucose Measurement: The most common use, including:
- Fasting Blood Glucose (FBG)
- Random Blood Glucose (RBG)
- Oral Glucose Tolerance Test (OGTT)
- Post-prandial Glucose
- Lactate Levels: For assessing metabolic status, shock, or tissue oxygenation.
- Alcohol Levels: While not their primary design, they are sometimes used for blood alcohol concentration (BAC) testing because sodium fluoride helps prevent bacterial growth that could produce or consume alcohol in the sample.
Royal Blue Top Blood Tube
Royal blue top tubes are a specialized category of blood tubes (vacutainers) designed with a very specific purpose: to provide a sample that is exceptionally free from trace element contamination. This makes them essential for tests that measure minute quantities of metals and other elements in the blood, where even tiny amounts of contaminants from the tube itself could skew results.
Royal blue top tubes are manufactured under clean room conditions to minimize contamination from dust or other environmental factors, which is crucial for accurate trace element and heavy metal analysis.
There are actually two variations of the royal blue top blood tube, with slightly different characteristics. These tubes are not suitable for routine blood tests like chemistry panels or CBCs.
1. Royal Blue Top with No Additive
Additives: None
Mode of Action: Relies on the natural clotting process. The clot formation separates the cellular components from the serum, which is then used for analysis. However, this type of blood tube is less common due to potential contamination issues.
2. Royal Blue Top with EDTA
Additive: Potassium EDTA (K2EDTA)
Mode of Action: Similar to the lavender or pink top EDTA tubes, K2EDTA chelates calcium ions, preventing blood clotting and preserving whole blood for analysis. This is the more common variant of the royal blue top blood tube (vacutainer).
Clotting Time: The clotting time depends on the specific type of royal blue top blood tube.
- No additive: Allow blood to clot completely (typically 15-30 minutes).
- EDTA: No clotting required, but gentle inversion 8-10 times after collection is essential for proper mixing.
Commonly Associated Tests:
- Heavy Metals:
- Lead (Pb)
- Mercury (Hg)
- Arsenic (As)
- Cadmium (Cd)
- Aluminum (Al)
- Chromium (Cr)
- Cobalt (Co)
- Manganese (Mn)
- Trace Elements and Micronutrients:
- Zinc (Zn)
- Copper (Cu)
- Selenium (Se)
- Iodine (I)
- Toxicology Screens: For certain drug or poison analyses where elemental contamination is a concern.
Specimen Quality Concerns of Vacutainer
Specimen quality is paramount when it comes to blood tests. Improper blood collection or handling can significantly impact the results, leading to misdiagnosis or unnecessary procedures.
- Incomplete clotting: If blood doesn’t clot completely before centrifugation of serum separator tube, red blood cells (RBCs) can lyse (rupture), releasing hemoglobin into the serum. This hemolysis can alter the results of various tests, especially those measuring enzymes or bilirubin.
- Excessive mixing: Vigorous or prolonged mixing can also cause hemolysis, especially with clot activator tubes (red-speckled top). Gentle inversion 8-10 times is sufficient for proper mixing.
Coagulation Blood Tube (Light Blue Top)
- Underfilling or overfilling: The blood-to-sodium citrate ratio is crucial for accurate coagulation testing. Underfilling concentrates the anticoagulant, while overfilling dilutes it, both leading to unreliable results.
- Improper mixing: Failure to mix the blood with sodium citrate upon collection can lead to localized clotting and inaccurate results in coagulation tests.
Heparin Blood Tube (Green Top)
- Underfilling: Similar to coagulation tubes (vacutainers), underfilling heparinized tubes can alter the blood-to-anticoagulant ratio, affecting test results.
- Presence of air bubbles: Air bubbles in the tube (vacutainer) can interfere with some tests, like blood gas analysis, as they alter the gas composition of the sample.
- Prolonged mixing delay: Heparin can slightly alter certain analytes over time. Prompt processing or analysis of the blood sample is recommended to minimize this effect.
EDTA Blood Tube (Lavender or Pink Top)
- Prolonged tourniquet application: Keeping the tourniquet on for an extended period can lead to artificial cell activation and potentially alter some blood cell parameters in a CBC.
- Overfilling: Similar to other tubes, overfilling an EDTA tube (vacutainer) can dilute the blood sample and affect test results.
- Presence of clots: Even small clots in an EDTA tube (vacutainer) can interfere with complete blood cell analysis, especially for white blood cell counts and differentials.
Sodium Fluoride/Potassium Oxalate Blood Tube (Gray Top)
- Underfilling: Underfilling significantly alters the blood-to-additive ratio, compromising the effectiveness of the preservatives and potentially leading to inaccurate glucose or lactate measurements.
- Improper mixing: Localized clotting due to inadequate mixing can affect test results, especially for glucose levels.
- NaF/K Oxalate blood tubes (vacutainers) are not suitable for most routine blood tests as the additives can interfere with certain analytes.
- The glycolysis-inhibiting effect of sodium fluoride is not immediate. There can be a delay of up to 1-4 hours before complete inhibition of glycolysis occurs. During this initial period, some glucose can still be metabolized, leading to a slight drop in glucose concentration. This is a crucial pre-analytical consideration.
General Concerns
- Improper labeling: Incorrect labeling of blood tubes (vacutainers) can lead to sample mix-up and compromise patient safety and test accuracy.
- Improper handling and storage: Blood samples need to be stored and transported under specific temperature conditions depending on the test. Failing to do so can alter the stability of certain analytes.
Order of Proper Draw
The importance of collecting blood tubes (vacutainers) in a specific order, often referred to as the “order of draw,” focuses on preventing contamination of the blood sample by additives present in different collection blood tubes.
Contamination Risks
Each blood tube (vacutainer) contains a specific additive (anticoagulant, clot activator, etc.) designed to preserve the sample for a particular type of test. If the order of draw is not followed, residual amounts of additives from a previously filled blood tube can be introduced into the next blood tube during the blood collection process.
This contamination can significantly alter test results:
- For example, if some heparin from a green-top blood tube (vacutainer) mixes with blood in a subsequent red-top serum separator tube (SST) (vacutainer), it can interfere with clot formation, leading to hemolysis (red blood cell rupture) and affecting various test results.
- Similarly, residual sodium citrate from a light blue coagulation blood tube (vacutainer) could contaminate a subsequent EDTA tube (lavender or pink top) (vacutainer), potentially affecting cell counts in a complete blood count (CBC).
Maintaining Sample Integrity
The order of draw ensures that the blood sample maintains its original composition as much as possible, minimizing the influence of additives from previous blood tube (vacutainer). This allows for accurate analysis of various blood components and reliable test results across different tests ordered.
Universal Order of Draw
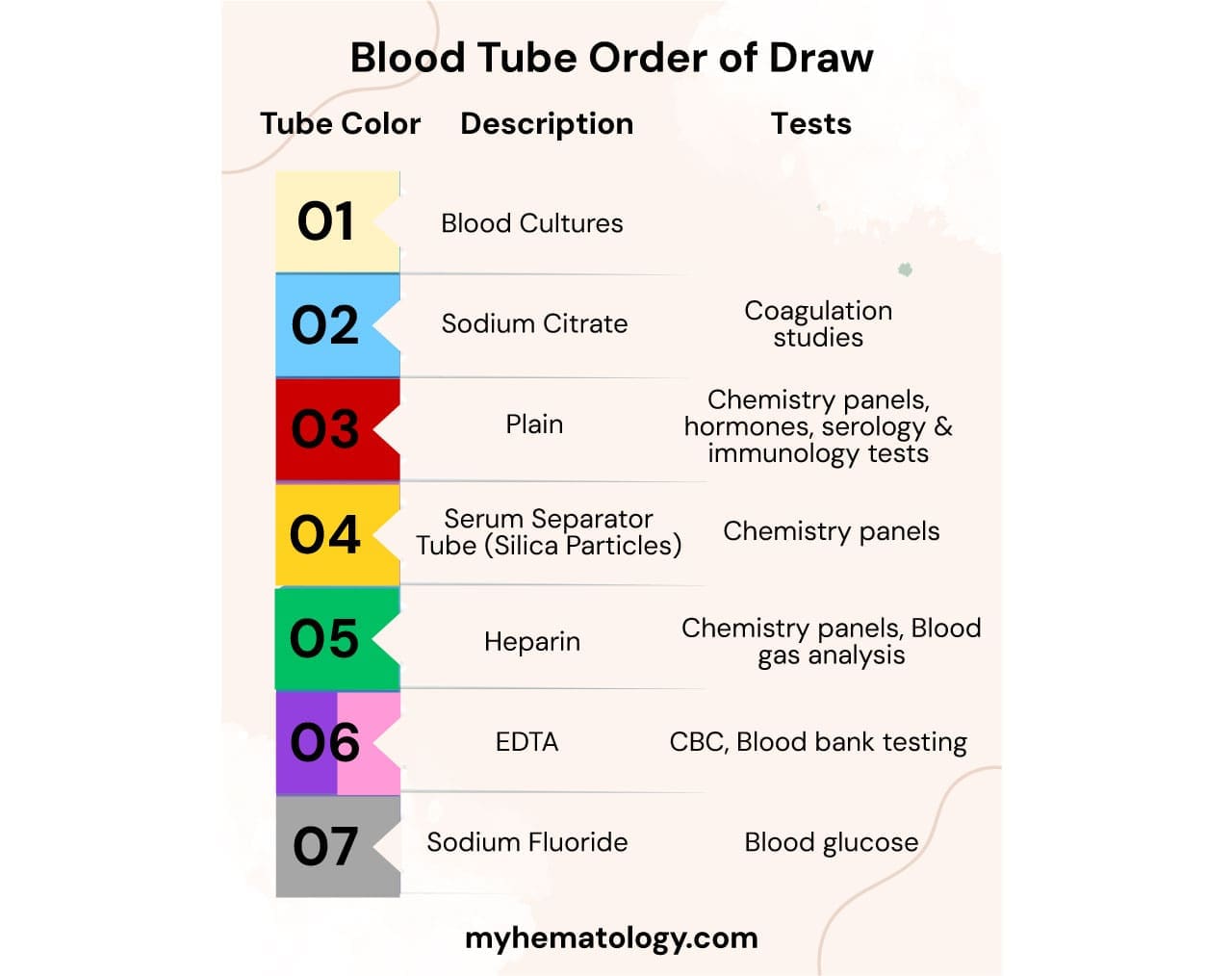
While specific protocols may vary slightly between institutions, a generally accepted order of draw exists:
- Coagulation Blood Tube (Light Blue Top) (Vacutainer)
- Serum Separator Tube (SST) – Red Top (plain), Red Speckled Top (clot activator), Gold Top (with gel) (Vacutainer): Order within serum separator tubes (SSTs) might vary depending on the presence of clot activator or gel separator.
- Heparin Blood Tube (Green Top) (Vacutainer)
- EDTA Blood Tube (Lavender or Pink Top) (Vacutainer)
- Sodium Fluoride/Potassium Oxalate Blood Tube (Gray Top) (Vacutainer)
Benefits of Following Order of Draw
- Ensures accurate and reliable test results for various blood tests.
- Minimizes the risk of misdiagnosis or the need for repeat blood draws.
- Promotes patient safety by providing a clear and standardized collection procedure.
Frequently Asked Questions (FAQs)
What is a yellow blood tube used for?
A yellow top blood tube (vacutainer) can be used for a few different purposes, depending on the specific additive it contains. Some yellow-capped tubes are blood culture bottles. However, when referring to yellow-capped blood collection tubes for laboratory analysis, the two most common types are:
- Yellow Top Tube with Acid-Citrate-Dextrose (ACD):
- Additives: ACD is an anticoagulant that works by binding calcium, preventing blood from clotting. Dextrose helps to nourish and preserve red blood cells.
- Uses: These tubes are primarily used for specialized tests that require whole blood or plasma where cell viability is important. This includes:
- Blood Bank Studies: Such as ABO grouping, Rh typing, and compatibility testing for blood transfusions.
- HLA Typing: Used for tissue typing in organ transplantation and certain immunogenetic studies.
- Molecular Diagnostic Testing: For DNA extraction and various genetic studies, including PCR assays.
- Paternity Testing: Since they preserve DNA well.
- Virology Studies: For the detection of viral infections in plasma samples.
- Yellow Top Blood Tube (often called a “Gold Top” or “Tiger Top” for serum separator tube): The specifics of serum separator tube have been described above.
Which color tube can be used for blood bank collection?
For blood bank collection, where accurate blood typing, crossmatching, and antibody screening are crucial for safe transfusions, the most commonly used tubes are:
- Pink Top Tube: This is the primary tube for blood bank testing. It contains EDTA (ethylenediaminetetraacetic acid), which is an anticoagulant that preserves the red blood cells and prevents clotting without significantly altering their morphology. The pink color is often specifically designated for immunohematology (blood bank) use to help prevent mix-ups and ensure the correct additive for these sensitive tests.
- Lavender/Purple Top Tube: While the pink top is specifically for blood bank, the lavender/purple top tube also contains EDTA. Because it also has EDTA and preserves cell integrity well, it can sometimes be used for blood bank tests, especially for blood typing and certain antibody screens, if a pink tube is not available or if the lab protocol allows for it. However, the pink top is typically preferred due to its specific designation and often larger volume to accommodate the needs of blood bank testing.
- Yellow Top Tube (with ACD): Some specialized blood bank studies, particularly those involving HLA typing (Human Leukocyte Antigen) or DNA studies, may use a yellow top tube containing Acid-Citrate-Dextrose (ACD). ACD is an anticoagulant that also helps preserve the viability of red blood cells and other cellular components, making it suitable for genetic and cell-based tests.
- Red Top Tube (Plain or with Clot Activator): In some specific blood bank protocols, especially for serum-based tests like antibody screening that require serum rather than whole blood, a plain red top tube (no additive) or a red top with a clot activator might be used. However, these are less common for routine blood bank collection compared to the EDTA tubes.
What is an orange tube?
An orange top tube is typically a specialized blood collection tube designed for rapid serum collection, especially in emergency or “STAT” situations. The key additive in an orange top tube is thrombin. Thrombin is a potent natural clotting factor that significantly accelerates the clotting of blood. This speed is critical when immediate test results are needed, such as in emergency rooms for rapid chemistry panels.
What is the black tube used for?
A black top tube is specifically designed for one main test: the Erythrocyte Sedimentation Rate (ESR), also commonly known as a “sed rate.” The black top tube contains sodium citrate as an anticoagulant. The ratio of blood to anticoagulant is critical for the ESR test, typically 4 parts blood to 1 part sodium citrate solution. This tube is generally not suitable for other types of blood tests due to the specific concentration and type of anticoagulant.
What color tube for CRP?
For a C-Reactive Protein (CRP) test, the most common blood collection tubes used are those that yield serum or plasma. For example, Gold Top Tube (or Tiger Top Serum Separator Tube), Red Top Tube, Green Top Tube and Lavender/Purple Top Tube (EDTA).
What color tube for ferritin?
For a ferritin test, the most common and preferred blood collection tubes are those that yield serum or heparinized plasma. For example, Gold Top Tube (or Tiger Top Serum Separator Tube), Red Top Tube and Green Top Tube.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Bain BJ. A Practical Guide. 6th Edition (Wiley). 2022.
- Bain BJ, Bates I, Laffan MA. Dacie and Lewis Practical Haematology: Expert Consult: Online and Print 12th Edition (Elsevier). 2016.
- Bayot ML, Tadi P. Laboratory Tube Collection. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK555991/
- Bowen, R. A., & Remaley, A. T. (2014). Interferences from blood collection tube components on clinical chemistry assays. Biochemia medica, 24(1), 31–44. https://doi.org/10.11613/BM.2014.006
- Kitchen, S., Adcock, D. M., Dauer, R., Kristoffersen, A. H., Lippi, G., Mackie, I., Marlar, R. A., & Nair, S. (2021). International Council for Standardisation in Haematology (ICSH) recommendations for collection of blood samples for coagulation testing. International journal of laboratory hematology, 43(4), 571–580. https://doi.org/10.1111/ijlh.13584
- Dimeski, G., Yow, K. S., & Brown, N. N. (2015). What is the most suitable blood collection tube for glucose estimation?. Annals of clinical biochemistry, 52(Pt 2), 270–275. https://doi.org/10.1177/0004563214544708
- Nell, E. M., Bailly, J., Oelofse, D., Linström, M., Opie, J., Chapanduka, Z. C., Vreede, H., & Korf, M. (2023). Multicentre verification of haematology laboratory blood collection tubes during a global blood collection tube shortage. International journal of laboratory hematology, 45(5), 707–716. https://doi.org/10.1111/ijlh.14129