Introduction
Apart from the ABO blood group system, the Rh blood group system is also important because anti-RhD can cause hemolytic transfusion reactions (highly immunogenic) and are normally IgG, thus able to cross the placenta and lead to hemolytic disease of the newborn (HDN). The Rh blood group system was discovered in 1939 by Karl Landsteiner and Alexander Wiener.
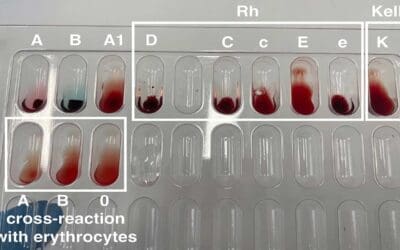
The Rh blood group system consists of two homologous transmembrane proteins, both encoded by genes on chromosome 1, that span the red blood cell plasma membrane 12 times. They appear to be used for the transport of carbon dioxide and/or ammonia across the plasma membrane. The Rh blood group locus is composed of 2 related structural genes, RhD and RhCE, which encode the membrane proteins that carry the D, Cc and Ee, antigens. The RhD gene may be either present or absent, giving the Rh D+ or Rh D- phenotype, respectively. Alternative RNA splicing from the RhCE gene generates 2 proteins, which encode the C, c, E or e antigens. Rh blood group antibodies rarely occur naturally; most are immune. Anti-D is responsible for most of the clinical problems associated with the system and a simple subdivision of subjects into Rh D+ and Rh D- using anti-D is sufficient for routine clinical purposes. Anti-C, anti-c, anti-E and anti-e are occasionally seen and may cause both transfusion reactions and hemolytic disease of the newborn. Anti-d does not exist.
While routine ABO Rh test often focuses on the RhD antigen, also known as the “D” positive or negative status, there’s a whole world of Rh typing waiting to be explored. Beyond D, several other Rh blood group antigens like C, c, E, and e play crucial roles in blood compatibility. Antibodies against these antigens can cause hemolytic reactions if incompatible blood is transfused. Luckily, commercially available reagents like anti-C, anti-c, anti-E, and anti-e can help identify these additional Rh phenotypes.
Rh typing can be performed using various techniques, including tube agglutination tests and gel card tests. While tube tests were the traditional method, gel cards have become increasingly popular due to their ease of use, speed, and improved sensitivity.
Principle of Rh Typing
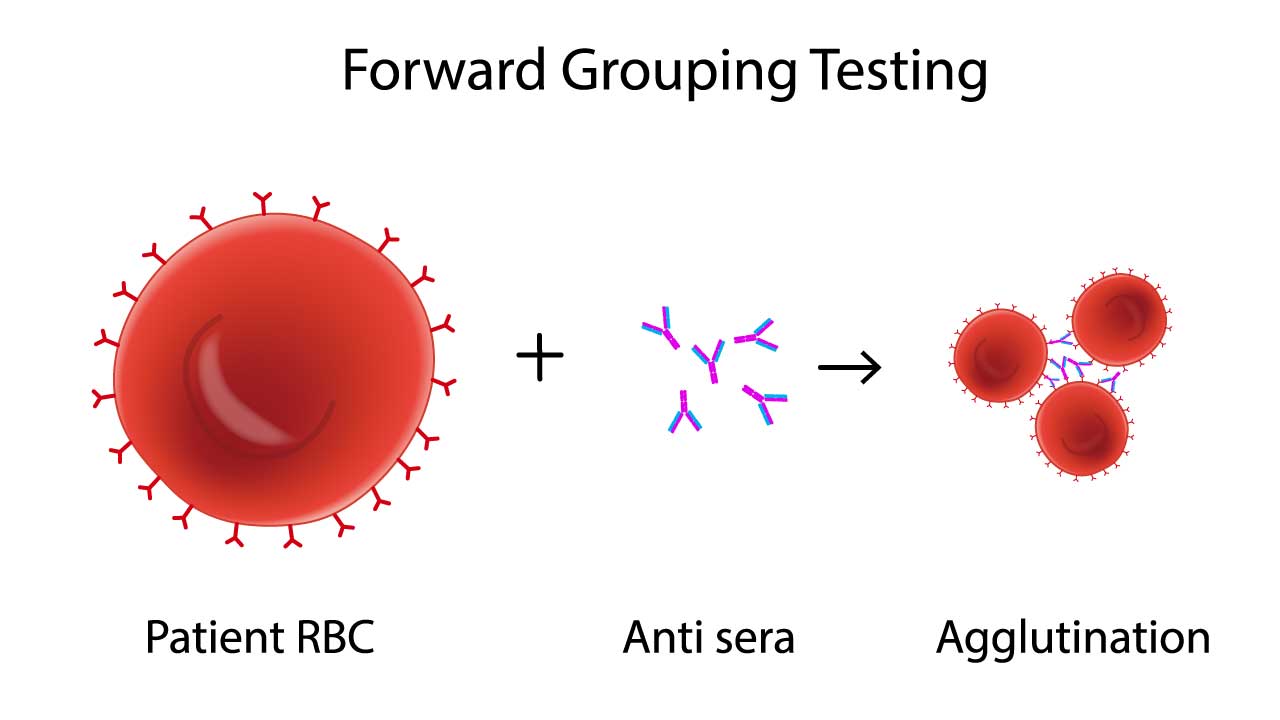
At the heart of the protocol lies the concept of antigen-antibody interaction, similar to ABO RhD blood group typing. Rh proteins, like D, C, E, and e, adorn the surface of red blood cells, acting as antigens. If your body lacks a specific antigen, say D, it may develop antibodies against it (anti-D). Transfusing incompatible blood bearing that antigen triggers a violent immune response, potentially leading to life-threatening hemolytic reactions.
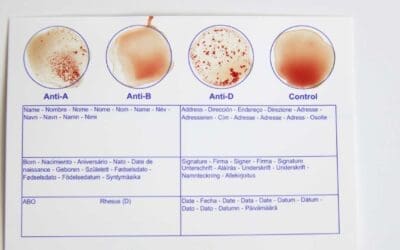
Red blood cells are first suspended in a solution containing antisera, each targeting a specific Rh antigen (e.g., anti-D, anti-C, anti-E). If a cell possesses the specific antigen, it binds to the corresponding antibody, forming visible clumps called agglutination. The absence of agglutination indicates a lack of the antigen
If a potential incompatibility is detected, red blood cells are subjected to individual tests with each antisera. This detailed analysis confirms the presence or absence of specific Rh antigens, allowing for a precise determination of the individual’s Rh phenotype.
Materials
- Polypropylene/glass tubes 10 mm x 75 mm
- Serofuge
- Centrifuge
- Pasteur pipettes
- Commercially prepared anti-D, -C, -E, -c and -c sera
- Patient’s EDTA whole blood
- Normal saline
Protocol
- Label each test tube with the corresponding antibody (Anti-D, Anti-C, etc.). Include a control tube with no antibody.
- Using a Pasteur pipette, add one drop of blood into each test tube.
- Add two drops of the appropriate antisera to each respective tube.
- Gently flick or rotate the tubes to mix the blood and reagents thoroughly.
- Place the tubes in a 37°C incubator for 30 minutes to allow for optimal antigen-antibody reactions.
- After incubation, centrifuge the tubes for 1 minute at 1000 RPM.
- Gently resuspend the cell button by tapping the tubes.
- Examine each tube under a light source to look for visible clumping or agglutination of red blood cells.
Interpretation
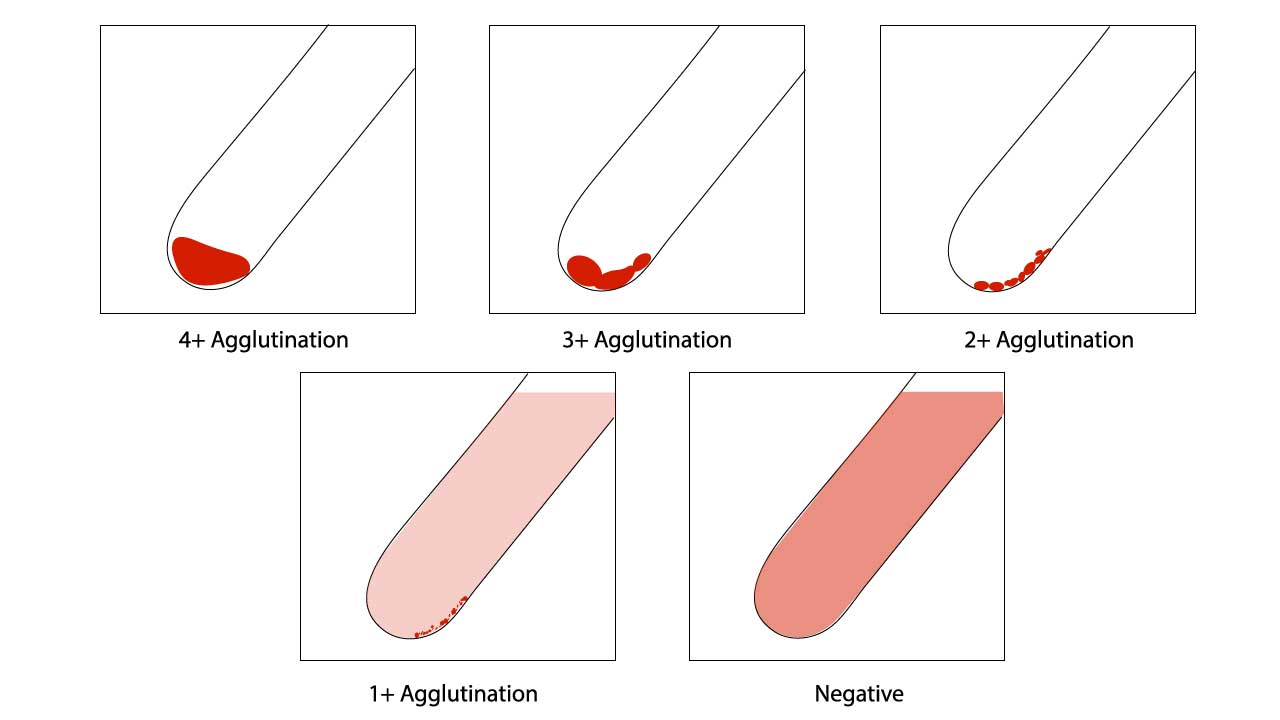
Positive results Rh typing are indicated by agglutination of tested blood. A negative result is observed when there is a clear supernatant after resuspension in the red cell agglutination test.
- Agglutination in a tube: Indicates the presence of the corresponding antigen on the red blood cells.
- No agglutination: Indicates the absence of the corresponding antigen.
- Control tube: Should show no agglutination, confirming the validity of the test.
Assessment of red cell agglutination test grading
| Symbol | Agglutination score | Description |
| 4+ / Complete (C) | 12 | Macroscopically visible cell button with a clear supernatant. |
| 3+ | 10 | Macroscopically visible large clumps of cell button with a clear supernatant. |
| 2+ | 8 | Macroscopically visible small clumps of cell button with a clear supernatant. |
| 1+ | 5 | Just macroscopically visible fine granular clumps of the cell button and the supernatant is turbid and reddish. |
| or weak (w) | 3 | Only microscopically visible fine granules of the cell button and the supernatant is turbid. |
| 0 | 0 | No agglutination seen. The supernatant is clear and reddish in color. |
| MF (mixed field) | MF | A mixture of agglutinated and unagglutinated red cells seen. |
| H | Complete hemolysis of the patient sample. The supernatant is grossly red with no evidence of red cells. |
Disclaimer: This protocol is intended for informational purposes only and may need to be modified depending on the specific laboratory procedures and patient circumstances. Always consult with a qualified healthcare professional for guidance. See additional information.
References
- American Association of Blood Banks (AABB). Technical Manual, 21st Edition, 2023.
- Dean L. Blood Groups and Red Cell Antigens [Internet]. Bethesda (MD): National Center for Biotechnology Information (US); 2005.
- Harmening DM. Modern Blood Banking & Transfusion Practices (FA Davis Company). 2018.
- Li HY, Guo K. Blood Group Testing. Front Med (Lausanne). 2022 Feb 11;9:827619. doi: 10.3389/fmed.2022.827619. PMID: 35223922; PMCID: PMC8873177.