What is hemato-oncology (blood cancer)?
Hemato-oncology specifically combines areas of hematology and oncology to diagnose and manage cancers that develop in the blood cells, bone marrow, lymph nodes, and other blood-related organs. Hemato-oncology is a fascinating and specialized field of medicine that bridges the gap between two important areas:
1. Hematology: This deals with the study, diagnosis, and treatment of blood disorders like anemias, bleeding disorders, and certain immune system issues.
2. Oncology: This focuses on the study, diagnosis, and treatment of cancers.
Origins
- Hemato-oncology emerged in the mid-20th century as advancements in diagnosis and treatment allowed for more targeted approaches to blood cancers.
- Pioneering physicians like Dr. David Karnofsky are credited with establishing this subspecialty, recognizing the unique needs of patients with these specific malignancies.
Focus on Blood Disorders and Cancers
Hemato-oncology covers a wide range of conditions, including:
- Leukemias: Cancers of the white blood cells, which can be acute (fast-growing) or chronic (slow-growing).
- Lymphomas: Cancers of the lymphatic system, including Hodgkin‘s and non-Hodgkin’s lymphoma.
- Myelomas: Cancers of plasma cells in the bone marrow, impacting bone health.
- Other blood cancers: Myeloproliferative disorders, myelodysplastic syndromes, and certain immune system tumors.
These conditions often share similar symptoms and require specialized knowledge and expertise for accurate diagnosis and effective treatment.
Global Prevalence and Impact of Blood Cancers
While advances in medicine have led to progress in various fields, blood cancers continue to cast a significant shadow across the globe.
Global Prevalence
- Staggering numbers: Globally, an estimated 4.4 million new cases of blood cancers were diagnosed in 2020, accounting for nearly 6% of all new cancers.
- Regional variations: The incidence varies geographically, with higher rates observed in developed countries due to factors like aging populations and environmental exposures.
- Specific trends: Leukemias are the most common blood cancers, followed by lymphomas and myelomas. The specific types and their frequency can also differ by region.
Impact on Individuals and Societies
- Mortality: Blood cancers in hemato-oncology are responsible for approximately 1.7 million deaths annually, making them the fourth leading cause of cancer death globally.
- Physical and emotional burden: Patients face challenging journeys marked by intense treatments, potential side effects, and emotional distress.
- Financial burden: Treatment costs for blood cancers can be substantial, creating financial hardship for patients and their families.
- Strain on healthcare systems: The increasing burden of blood cancers puts pressure on healthcare systems, requiring efficient allocation of resources and ongoing research for better prevention, diagnosis, and treatment options.
Looking Ahead
- Rising concerns: Population aging and potential environmental factors suggest the burden of blood cancers in hemato-oncology may continue to rise.
- Global efforts: Organizations like the World Health Organization are actively involved in raising awareness, improving access to diagnosis and treatment, and supporting research efforts.
- Importance of early detection and awareness: By staying informed about common signs and symptoms and seeking timely medical attention, individuals can contribute to early detection and better outcomes.
Why does hemato-oncology matters?
In the vast landscape of medicine, hemato-oncology stands out as a critical force in safeguarding human health and fostering advancements against complex blood cancers. Here’s why this subspecialty plays such a pivotal role:
Patient Care
- Early Detection and Accurate Diagnosis: Hemato-oncologists possess the expertise to identify even subtle indicators of blood cancers through specialized tests and analyses, ultimately leading to earlier intervention and potentially better outcomes.
- Individualized Treatment Plans: Each patient’s journey is unique, and hemato-oncologists leverage their deep understanding of various blood cancers and therapies to tailor treatment plans considering individual needs, age, and overall health.
- Management of Complexities: Blood cancers pose unique challenges beyond just tumor eradication. Hemato-oncologists manage side effects, monitor for complications, and provide supportive care throughout the treatment journey.
- Emotional and Psychological Support: Navigating a blood cancer diagnosis is emotionally draining. Hemato-oncologists partner with patients, families, and support systems to address anxieties and ensure holistic well-being throughout the entire experience.
Research Advancements
- Understanding Disease Mechanisms: Hemato-oncologists actively participate in research to uncover the causes, progression, and specific mutations driving different blood cancers. This knowledge fuels better diagnostic tools and treatment strategies.
- Developing New Therapies: They are at the forefront of developing novel treatment modalities like personalized medicine, targeted therapies, and immunotherapies, offering more precise and effective approaches with promising outcomes.
- Clinical Trials: Hemato-oncologists collaborate on and lead clinical trials, giving patients access to cutting-edge therapies and contributing to advancing the field for future generations.
- Advocacy and Awareness: They actively advocate for increased funding for research, wider access to diagnostics and treatments, and raising public awareness about blood cancers and their early signs.
Beyond individual patient care, hemato-oncologists contribute to the collective fight against blood cancers by:
- Sharing Knowledge and Collaborating: They actively share their expertise and collaborate with other specialists like surgeons, radiation oncologists, and clinical researchers to ensure comprehensive patient care and drive further advancements.
- Mentoring and Educating: By training future generations of medical professionals, they ensure the continuity of expertise and the future of effective blood cancer management.
- Maintaining Ethical Standards: They uphold the highest ethical standards in clinical practice and research, prioritizing patient safety and well-being while advancing knowledge responsibly.
What does a hemato-oncologist do?
A hemato-oncologist wears many hats and plays a crucial role in the lives of patients with blood cancers and blood disorders. Here’s a closer look at their diverse functions:
Diagnosis
- Discovering the cause: They utilize their expertise to interpret symptoms, analyze blood tests and biopsies, and conduct imaging studies to accurately diagnose blood cancers and disorders in hemato-oncology.
- Collaboration is key: They often collaborate with other specialists, like pathologists and radiologists, to gather a comprehensive picture and ensure an accurate diagnosis for hemato-oncology disorders.
Treatment
- Tailoring the approach: They don’t offer a one-size-fits-all solution. Instead, they develop personalized treatment plans in hemato-oncology disorders by considering the specific diagnosis, disease stage, individual health, and preferences.
- A toolbox of options: Their arsenal includes chemotherapy, radiation therapy, targeted therapies, immunotherapies, and stem cell transplantation, and they choose the combination most likely to benefit the patient.
- Managing side effects: Battling cancer comes with challenges. Hemato-oncologists manage side effects, prescribe supportive medications, and provide symptom relief throughout the treatment journey.
Management
- Beyond treatment: The fight doesn’t end with the last dose. Hemato-oncologists monitor patients for recurrence, adjust treatment plans if needed, and offer long-term supportive care and follow-up.
- Emotional support: They understand the emotional toll of a diagnosis and provide counseling, connect patients with support groups, and advocate for their well-being.
Research and Innovation
- Advancing the future: Hemato-oncologists actively participate in clinical trials, research new therapies, and contribute to knowledge-sharing, pushing the boundaries of treatment and improving outcomes for future generations.
- Patient advocacy: They advocate for increased funding for research, wider access to diagnostics and treatments, and raising public awareness about blood cancers.
Collaboration and Communication
- Teamwork makes the dream work: They collaborate with other specialists, nurses, researchers, and social workers to provide holistic care and ensure every aspect of the patient’s needs is addressed.
- Clear communication: They prioritize clear and transparent communication with patients and families, explaining diagnoses, treatment options, and potential outcomes in a language they understand.
Diseases treated by hemato-oncologists
Hemato-oncologists are specialized doctors who diagnose and treat a wide range of diseases affecting the blood, bone marrow, and lymphatic system. These diseases can be broadly categorized into two main groups in hemato-oncology: blood cancers and non-cancerous blood disorders.
While blood cancers are a major focus of their expertise, hemato-oncologists play a crucial role in diagnosing, managing, and providing treatment for a wide spectrum of non-cancerous blood disorders as well. They possess the extensive knowledge and specialized skills necessary to guide patients with various blood-related conditions throughout their journey towards improved health and well-being.
Blood Cancers
- Leukemias: These are cancers of the white blood cells, which are responsible for fighting infection. There are several different types of leukemia, each with its own unique characteristics and treatment approach. Here are some of the most common types:
- Acute lymphoblastic leukemia (ALL): This is the most common type of leukemia in children. It is characterized by the rapid growth of immature lymphocytes (a type of white blood cell).
- Acute myeloid leukemia (AML): This is a fast-growing cancer of the myeloid cells, which are precursors to red blood cells, white blood cells, and platelets.
- Chronic lymphocytic leukemia (CLL): This is a slow-growing cancer of the lymphocytes. It is most common in older adults.
- Chronic myeloid leukemia (CML): This is a slow-growing cancer of the myeloid cells. It is caused by a specific genetic abnormality.
- Lymphomas: These are cancers of the lymphatic system, which is part of the immune system. Lymphomas can develop in lymph nodes, the spleen, the thymus, or other organs. There are two main types of lymphoma:
- Hodgkin’s lymphoma: This type of lymphoma is characterized by the presence of Reed-Sternberg cells, a specific type of cancer cell.
- Non-Hodgkin’s lymphoma: This is a more diverse group of lymphomas, with many different subtypes.
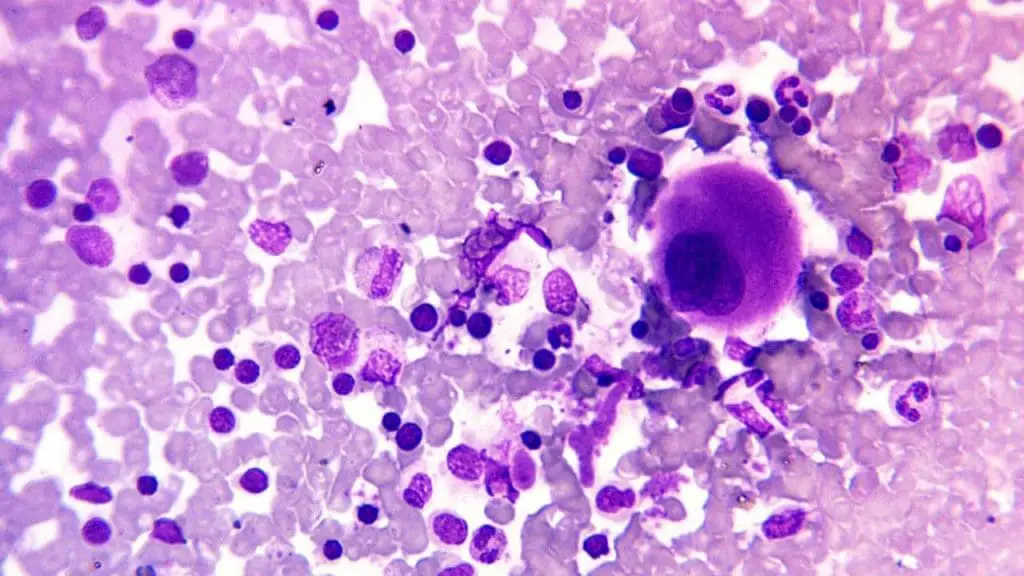
- Myelomas: These are cancers of the plasma cells, which are white blood cells that make antibodies. Myelomas typically develop in the bone marrow and can cause bone pain, anemia, and kidney problems.
Non-Cancerous Blood Disorders
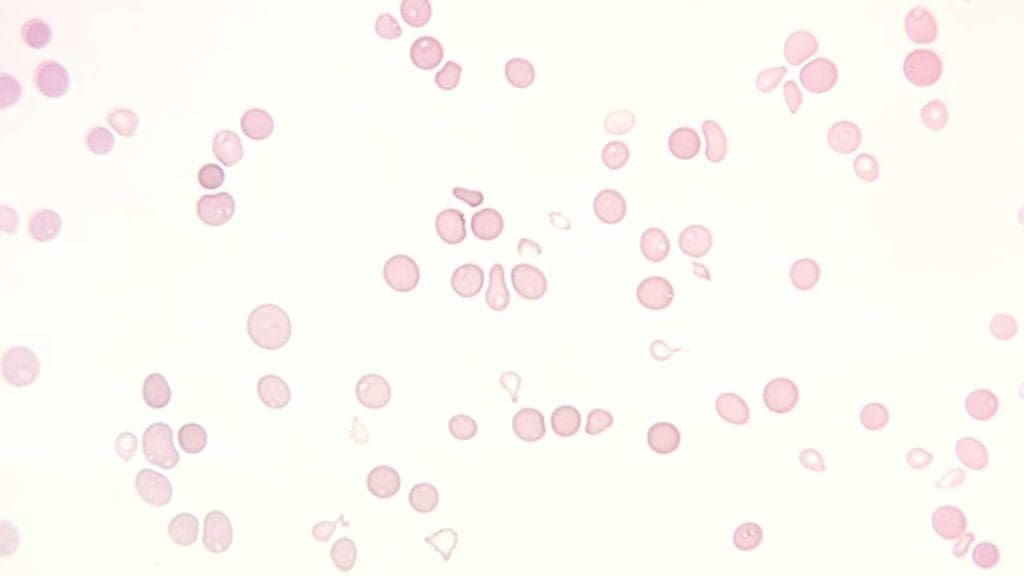
- Anemia: This is a condition in which there are not enough red blood cells or the red blood cells are not functioning properly. This can lead to fatigue, shortness of breath, and other symptoms.
- Bleeding disorders: These are conditions that affect the blood’s ability to clot properly. This can lead to excessive bleeding after injury or surgery.
- Immune thrombocytopenic purpura (ITP): This is an autoimmune disorder that causes low levels of platelets (a type of blood cell that helps with clotting). This can lead to easy bruising and bleeding.
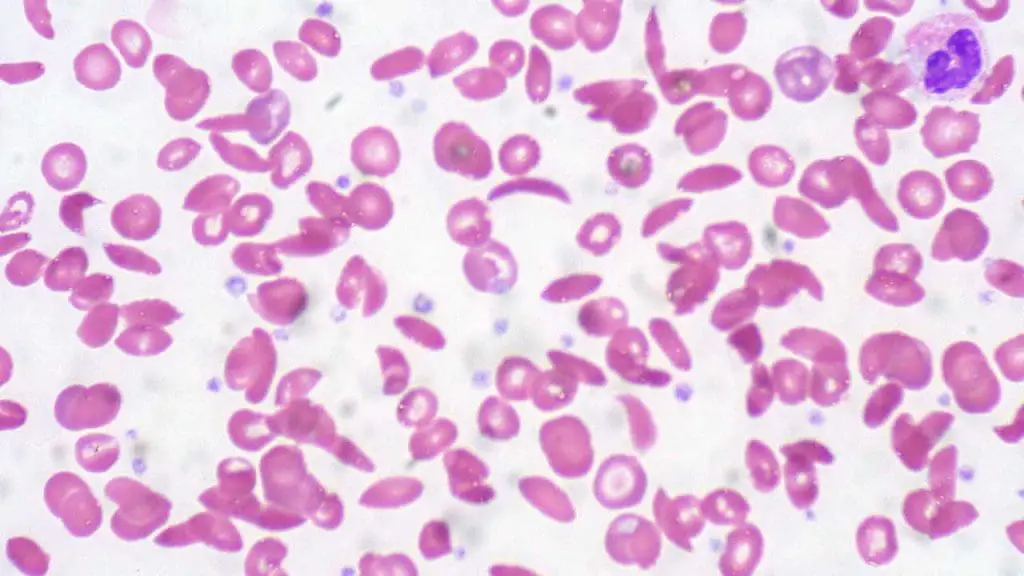
- Sickle cell disease: This is a genetic disorder that affects the shape of red blood cells. Sickle-shaped cells can block blood vessels, causing pain, organ damage, and other complications.
This is just a brief overview of some of the diseases treated by hemato-oncologists. It is important to note that this is not an exhaustive list and there are many other blood disorders that can be treated by these specialists.
General signs and symptoms of blood cancers
While specific symptoms can vary depending on the type of blood cancer in hemato-oncology, some general warning signs should prompt seeking medical attention.
Common Indicators
- Fatigue: Persistent tiredness and lack of energy that doesn’t improve with rest.
- Fever: Frequent or unexplained fevers, often accompanied by night sweats.
- Easy Bruising/Bleeding: Unexplained bruising or bleeding, even from minor injuries.
- Weight Loss: Unintentional and unexpected weight loss without obvious explanation.
- Swollen Lymph Nodes: Painless enlargements in the neck, armpits, or groin.
Disease-Specific Symptoms
- Night sweats: Excessive sweating during sleep, particularly in lymphoma.
- Bone pain: Deep, aching bone pain, more commonly associated with myeloma.
General diagnosis and screening of blood cancers
Blood cancers in hemato-oncology can present with various symptoms, but pinpointing the exact diagnosis requires a multi-pronged approach involving both diagnostic tools and screening methods.
Blood Tests
- Complete Blood Count (CBC): This basic test measures red blood cells, white blood cells, platelets, and hemoglobin levels, providing initial clues about potential abnormalities.
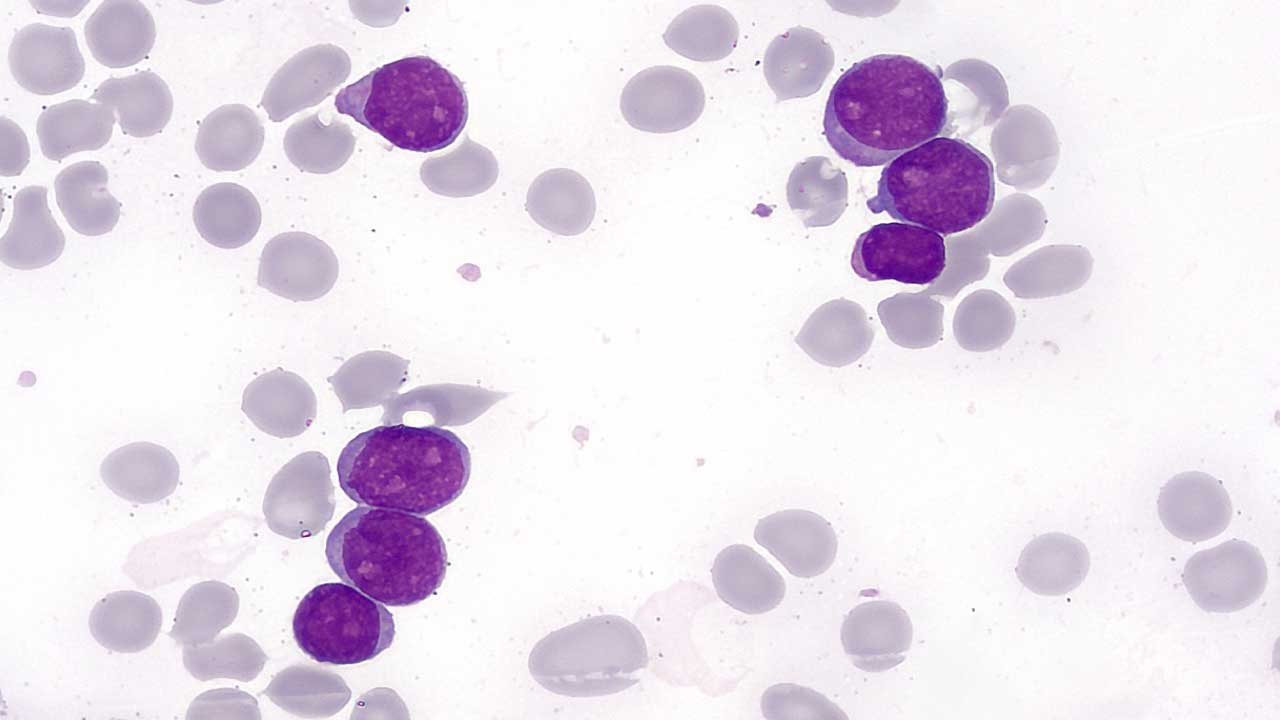
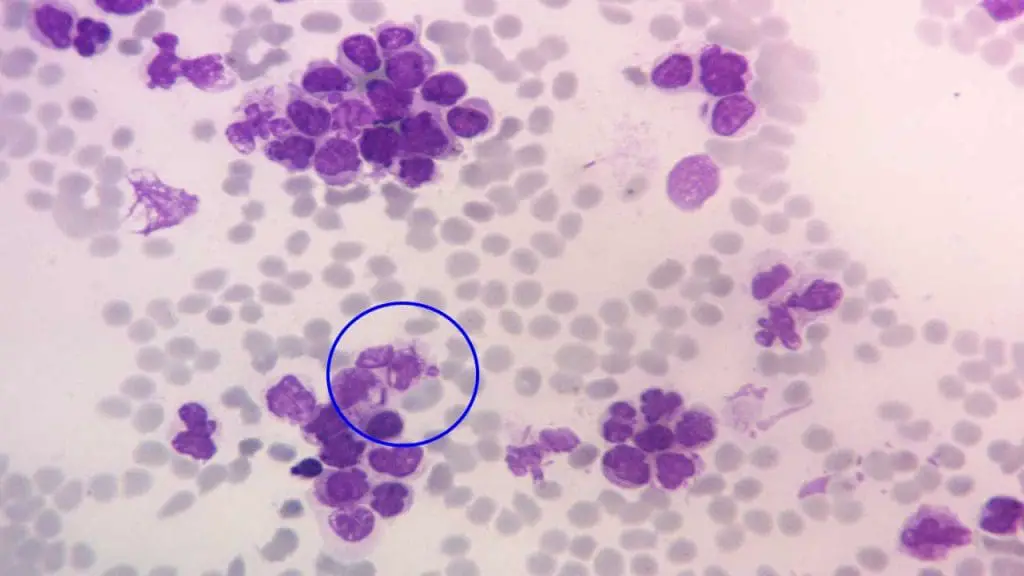
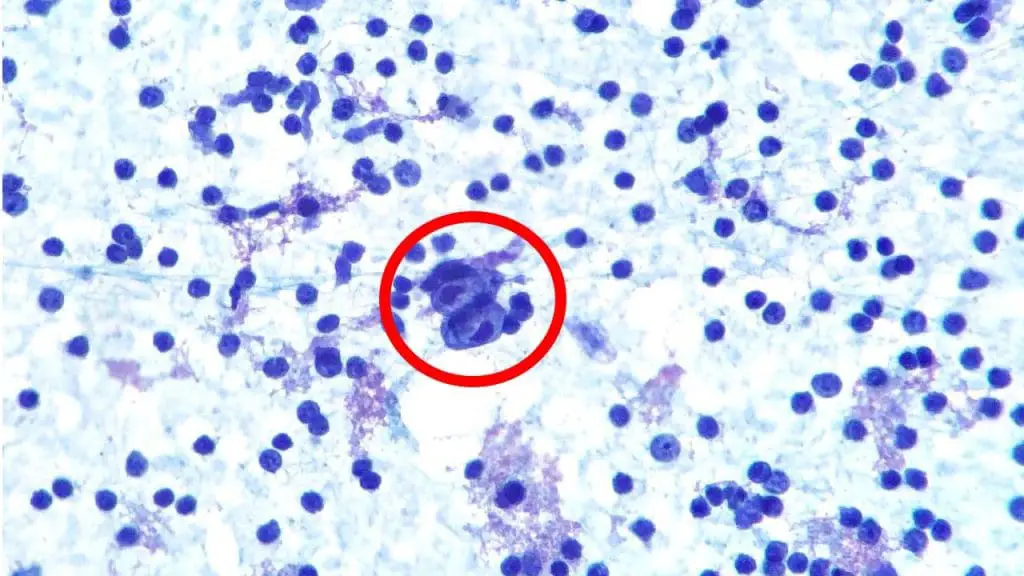
- Peripheral Blood Smear: Microscopic examination of blood cells reveals their size, shape, and presence of abnormal cells, offering further insight.
- Flow cytometry: This technique analyzes individual cells based on their surface markers, aiding in identifying specific types of leukemia and lymphoma.
- Tumor markers: Elevated levels of specific proteins in the blood can indicate certain blood cancers.
Bone Marrow Biopsy and Aspiration: Removing a small sample of bone marrow allows for examination of cells under a microscope, providing definitive diagnosis of leukemias, lymphomas, and myelomas.
Lymph Node Biopsy: Examining a lymph node under a microscope helps diagnose lymphomas and other conditions involving the lymphatic system.
Imaging Studies
- X-rays: Can reveal bone abnormalities associated with myeloma or enlarged lymph nodes.
- CT scans: Offer detailed 3D images of internal organs, identifying enlarged lymph nodes, spleen, or liver, potentially affected by blood cancers.
- PET scans: Use radioactive tracers to identify areas with increased metabolic activity, potentially indicating cancer cells.
Importance of Accurate Diagnosis
- Choosing the most effective treatment: Different blood cancers require specific treatment approaches, and accurate diagnosis ensures the right therapy is targeted.
- Determining prognosis and survival: Understanding the specific type and stage of the cancer allows for a more accurate prediction of potential outcomes.
- Guiding future care: Accurate diagnosis informs decisions about follow-up care, monitoring, and potential risks of recurrence.
Treatment options of blood cancers
Blood cancersin hemato-oncology, despite their complexities, offer a range of treatment options, each with its own strengths and limitations. Here’s a glimpse into the diverse arsenal available:
Standard Treatments
- Chemotherapy: The workhorse of cancer treatment, chemo utilizes powerful drugs to kill rapidly dividing cancer cells. However, it can also affect healthy cells, leading to various side effects like nausea, fatigue, hair loss, and increased risk of infection.
- Radiation Therapy: This targeted approach uses high-energy beams to destroy cancer cells or shrink tumors. Depending on the area treated, side effects can include skin irritation, fatigue, and nausea.
- Stem Cell Transplantation: This involves replacing damaged bone marrow with healthy stem cells from a donor or the patient themselves. It offers a potential cure but carries risks of infection and graft-versus-host disease (GVHD).
Emerging Therapies
- Immunotherapy: This harnesses the body’s own immune system to fight cancer. Checkpoint inhibitors, CAR-T cell therapy, and other approaches offer promising results with more specific targeting and potentially fewer side effects compared to traditional therapies.
- Personalized Medicine: This tailors treatment based on the unique genetic makeup of the patient’s cancer, allowing for more targeted and effective therapies with reduced side effects. CAR-T cell therapy, for example, falls under this category.
Individualized Treatment Plans
The key lies in individualized treatment plans crafted by a team of specialists. They consider:
- Specific type and stage of the blood cancer: Different cancers respond differently to treatments.
- Patient’s age, overall health, and medical history: Individual factors influence treatment options and potential risks.
- Personal preferences and goals: Patient input is crucial in shaping the treatment approach.
Additional Points
- Treatment combinations: Often, multiple treatments like chemotherapy and radiation are combined for optimal results.
- Supportive care: Managing side effects and improving quality of life are crucial aspects of care throughout the treatment journey.
- Clinical trials: These offer access to cutting-edge therapies and contribute to research advancements.
Ethical considerations in hemato-oncology
Hemato-oncology, like many areas of medicine, is not immune to ethical dilemmas. Due to the complexity of diagnoses, potential treatments, and the emotional toll on patients and families, several ethical considerations arise in this field:
Resource Allocation
- Limited access to treatment: High costs of advanced therapies and limited resources can create challenges in ensuring equitable access to optimal care for all patients.
- Balancing research and clinical care: Funding and resources must be carefully allocated between research for future advancements and providing the best possible care for current patients.
- Clinical trials: Striking a balance between offering patients access to potentially life-saving new treatments through trials and protecting them from unnecessary risks associated with experimental therapies.
Autonomy and Informed Consent
- Complex treatment decisions: Patients may face overwhelming choices with varying risks and benefits, requiring clear communication and support in making informed decisions aligned with their values.
- End-of-life care: Balancing aggressive treatment options with respecting patient autonomy and preferences for comfort and quality of life in advanced stages.
- Genetic testing and counseling: Sharing sensitive genetic information and its implications for patients and their families requires thoughtful approaches and respecting individual autonomy.
Ethical Conduct in Research in Hemato-oncology
- Recruitment and selection of participants: Ensuring fair and ethical recruitment practices within clinical trials, avoiding exploitation of vulnerable populations.
- Data privacy and confidentiality: Protecting patient data collected during research while allowing for valuable advancements in the field.
- Conflict of interest: Addressing potential conflicts that may arise when researchers have financial ties to pharmaceutical companies developing therapies.
Additionally
- Psychosocial support: Recognizing the emotional and psychological impact of blood cancers and providing appropriate support mechanisms.
- Culturally sensitive care: Ensuring culturally competent care that respects patients’ diverse backgrounds and values.
- Communication and collaboration: Fostering open communication and collaboration between patients, families, healthcare professionals, and researchers for optimal care and ethical decision-making.
Remember, this is not an exhaustive list, and the specific ethical considerations may vary depending on the specific situation and individual case. However, being aware of these potential challenges allows for open discussions, promotes transparency, and ultimately guides ethical practices within the field of hemato-oncology.
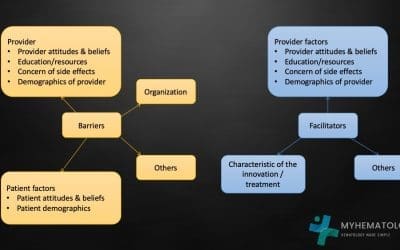
Role of clinical trials in advancing treatment options in hemato-oncology
Clinical trials play a crucial and irreplaceable role in advancing treatment options for a variety of diseases, including blood cancers. They serve as the bridge between promising therapies discovered in the lab and making them available to patients in need.
Testing Novel Approaches
- Investigate new drugs, therapies, and interventions: Clinical trials evaluate the safety, efficacy, and potential benefits of new approaches that haven’t been used in patients before.
- Compare existing treatments to new ones: This allows researchers to determine if the new option is as effective or even better than the standard treatment.
- Explore different combinations of therapies: Trials assess if combining existing treatments offers improved outcomes compared to single therapies.
Generating Evidence-Based Medicine
- Gather robust data on safety and efficacy: Clinical trials follow rigorous methodologies to collect reliable data on how well a new treatment performs and its potential side effects.
- Inform treatment guidelines and standards: This data forms the basis for developing evidence-based clinical guidelines that healthcare professionals rely on to make informed treatment decisions for their patients.
- Contribute to continuous improvement: The findings from trials inform future research and development, leading to further refinement and evolution of treatment options.
Benefits for Patients
- Access to potentially life-saving therapies: Patients participating in trials may gain access to cutting-edge therapies unavailable elsewhere, offering hope for improved outcomes.
- Contribute to medical progress: By participating, patients actively contribute to advancing medical knowledge and potentially benefit future generations facing similar conditions.
- Receive close monitoring and care: Trial participants are meticulously monitored by healthcare professionals throughout the process, ensuring their safety and well-being.
Challenges and Considerations
- Time and resource commitment: Participating in a clinical trial often requires significant time and commitment from patients, which might not be feasible for everyone.
- Uncertainty of outcomes: New treatments may not always be effective, and there’s a chance of experiencing side effects.
- Ethical considerations: Ensuring informed consent, fair participant selection, and data privacy are crucial aspects of ethical conduct in clinical trials.
Overall
While clinical trials are not without their challenges, they hold immense potential for advancing treatment options and improving patient outcomes. By understanding their role, benefits, and considerations, individuals can make informed decisions about participating and contribute to the progress of medical knowledge for future generations.
Frequently Asked Questions (FAQs)
What to expect when seeing a hemato-oncologist?
Visiting a hemato-oncologist can be daunting, especially when navigating a blood cancer diagnosis or managing a blood disorder. Here’s a glimpse into what to expect during your first consultation:
Preparation
- Gather your medical records: Bring previous diagnoses, test results, treatment history, and medications you’re currently taking.
- List your symptoms: Write down any symptoms you’re experiencing, their duration, and severity.
- Prepare questions: Don’t hesitate to write down your concerns and questions beforehand.
The Consultation
- Introductions and history: The doctor will introduce themselves and their team, then review your medical history and family history.
- Physical examination: This may involve checking your lymph nodes, spleen, and other areas for abnormalities.
- Discussion of symptoms: Be prepared to detail your symptoms, including their onset, progression, and any related concerns.
- Review of diagnostic tests: Your doctor will go through any existing test results and explain their implications.
- Additional tests: Based on your case, further tests like blood tests, bone marrow biopsies, or imaging studies might be recommended.
- Diagnosis and treatment discussion: If a diagnosis is available, the doctor will explain it in detail and discuss potential treatment options. This includes the rationale behind each option, its expected benefits and risks, and its impact on your daily life.
- Time for questions: Openly ask any questions you have about the diagnosis, treatment options, side effects, prognosis, and anything else that concerns you.
Additional Points
- Bring a support person: Having someone there for emotional support and note-taking can be helpful.
- Dress comfortably: Wear loose clothing that allows for easy examination.
- Be prepared for lengthy appointments: Initial consultations can last an hour or longer.
- Express your feelings: Don’t be afraid to share your emotional concerns and fears. Your doctor wants to provide holistic care.
- Second opinions: You have the right to seek second opinions from other specialists if you feel comfortable doing so.
Remember: Each patient and diagnosis are unique, so the specific details of your consultation may vary. The key takeaway is to be informed, prepared, and actively involved in your healthcare journey. Don’t hesitate to ask questions, express your concerns, and work collaboratively with your hemato-oncologist for the best possible outcome.
Why would I be referred to hematology oncology?
There are several broad reasons why someone might be referred to a hematologist-oncologist:
Blood-related abnormalities
- Abnormal blood test results: This could include low blood counts (anemia), high blood counts (leukocytosis), changes in white blood cell types, or abnormal platelet levels.
- Suspected blood cancer: Symptoms like fatigue, fever, easy bruising or bleeding, night sweats, and bone pain can raise concerns about various blood cancers.
- Non-cancerous blood disorders: Conditions like anemia, hemophilia, sickle cell disease, and immune thrombocytopenic purpura (ITP) also fall under the purview of hematologists-oncologists.
- Complications from other conditions: Some infections, autoimmune diseases, and other medical conditions can affect the blood, requiring specialist evaluation and management.
Family history or genetic risk factors
- If you have a family history of blood cancers or genetic predispositions, you might be referred for monitoring or early detection purposes.
Monitoring after previous blood cancer diagnosis
- Even after treatment, regular follow-up with a hematologist-oncologist is crucial to monitor for recurrence or late effects.
Seeking an expert opinion
- If your primary care doctor feels they require additional expertise or a second opinion to diagnose or manage a complex blood-related concern, they may refer you to a hematologist-oncologist.
Remember: This is not an exhaustive list, and the specific reason for your referral will depend on your individual situation. The best way to understand why you were referred is to ask your doctor directly. They can explain the reasoning behind their decision and address any questions or concerns you have.
What is pediatric hematology-oncology?
Pediatric hematology-oncology is a specialized medical field focusing on diagnosing and treating blood disorders and cancers in children and adolescents. These specialists possess expertise in both hematology (blood disorders) and oncology (cancers), offering comprehensive care for young patients with various blood-related conditions.
Scope of Practice
- Blood disorders: This includes diagnosing and managing conditions like anemia, hemophilia, sickle cell disease, immune thrombocytopenia (ITP), and other non-cancerous blood abnormalities.
- Childhood cancers: They diagnose and treat various childhood cancers, including leukemias, lymphomas, brain tumors, bone tumors, and other malignancies affecting the blood, bone marrow, and lymphatic system.
- Specific childhood considerations: Their understanding of child development, growth, and unique sensitivities allows them to tailor treatment plans and provide compassionate care that addresses the specific needs of young patients.
Treatment Approaches
- Utilizing evidence-based practices: They adhere to the latest research and guidelines while considering the individual needs and developmental stage of each child.
- Minimizing side effects: Their focus is on using therapies that offer optimal outcomes while minimizing the potential for long-term side effects and preserving quality of life.
- Collaborative care: They work closely with other specialists, including pediatric oncologists, surgeons, radiation therapists, nurses, and psychologists, to provide holistic and coordinated care.
- Supporting families: They recognize the emotional toll on families and provide support systems and resources to navigate the challenges of diagnosis and treatment.
Why is it important?
- Specialized expertise: These specialists have a deep understanding of childhood blood disorders and cancers, crucial for accurate diagnosis and effective treatment.
- Tailored care: They offer individualized treatment plans considering the unique needs and vulnerabilities of children.
- Improved outcomes: Advancements in research and specialized care have led to significantly improved survival rates for many childhood cancers and blood disorders.
- Supporting families: They provide holistic care and support, recognizing the emotional and practical challenges families face alongside their children.
Remember: This is a simplified overview, and specific details of practice and treatment approaches may vary depending on the individual child’s condition and healthcare system.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.