TL;DR
Petechiae are pinpoint (1-2mm), non-blanching red or purple spots on skin or mucous membranes as a results of small capillary bleeding.
Causes ▾:
- Increased pressure (coughing, straining).
- Low platelet count (thrombocytopenia).
- Platelet dysfunction.
- Infections (bacterial, viral, rickettsial).
- Vasculitis.
- Drug reactions.
- Nutritional deficiencies (Vitamin C, K).
- Hematologic malignancies.
Symptoms ▾:
- Characteristic small red/purple spots.
- Distribution varies (localized or widespread).
- Associated symptoms depend on the underlying cause (fever, bleeding, joint pain, etc.).
Investigations ▾:
- Complete Blood Count (CBC) with platelet count.
- Peripheral blood smear.
- Coagulation studies (PT/aPTT).
- Specific tests based on suspected cause (blood cultures, viral serology, autoimmune markers).
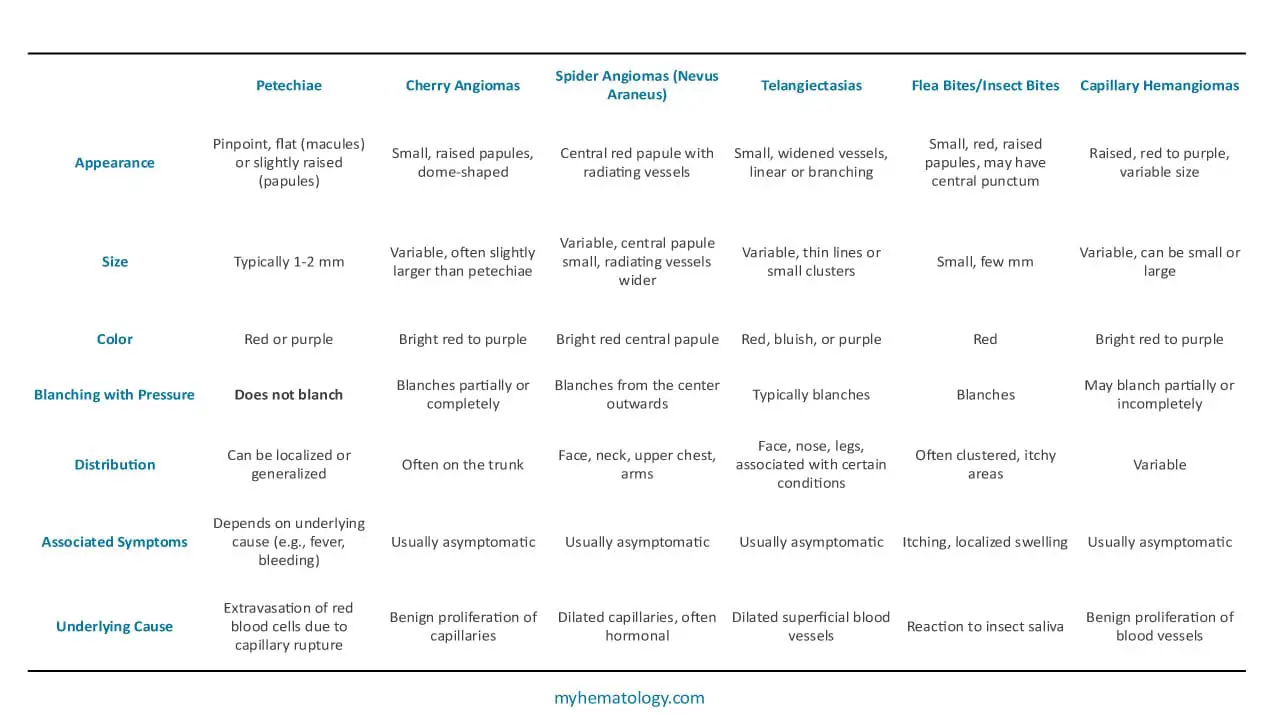
Differential Diagnosis ▾:
- Cherry angiomas (blanching, raised).
- Spider angiomas (blanching, central vessel).
- Telangiectasias (blanching, linear).
- Insect bites (blanching, itchy).
- Capillary hemangiomas (blanching, raised).
Treatment ▾:
- Focuses on treating the underlying cause.
- Supportive care (rest).
- May involve antibiotics, antivirals, immunosuppressants, or other specific therapies.
- Platelet transfusions in severe thrombocytopenia.
*Click ▾ for more information
Introduction
The sudden appearance of tiny, red or purple spots on the skin or mucous membranes can often be a cause for concern. These small but potentially significant lesions are known as petechiae. Derived from the Italian word “peticchio,” meaning a small spot or blemish, petechiae are characterized as pinpoint, non-blanching macules or papules, typically ranging from 1 to 2 millimeters in diameter. Unlike larger bruises (ecchymoses) or slightly larger purplish spots (purpura), it represent the extravasation of small amounts of blood from capillaries into the surrounding tissues.
While seemingly minor, the presence of petechiae should not be dismissed lightly. Their appearance can be a subtle yet crucial indicator of a wide spectrum of underlying medical conditions, ranging from benign and self-limiting issues to serious and potentially life-threatening disorders.
Causes of Petechiae
The appearance of petechiae signifies a disruption in the integrity of small blood vessels, specifically capillaries, leading to the leakage of red blood cells into the surrounding dermis or subcutaneous tissue. Understanding the various mechanisms that can cause this vascular fragility or increased pressure is crucial in determining the underlying cause.
Non-Pathological Causes
In some instances, petechiae can arise due to mechanical factors that temporarily increase intravascular pressure without indicating a systemic illness.
Trauma and Increased Pressure
- Forceful Coughing, Vomiting, and Straining: Activities that significantly raise intrathoracic or intra-abdominal pressure can cause capillaries in the head, neck, and upper chest to rupture, resulting in petechiae in these areas.
- Prolonged Crying: Similar to coughing, sustained crying in infants can lead to petechiae on the face and neck.
- Tight Clothing or External Pressure: Constrictive clothing or prolonged external pressure on the skin can occasionally cause localized petechiae.
- Childbirth: The intense physical exertion during labor can lead to petechiae on the face, neck, and upper chest of the mother.
Prolonged Standing
In rare cases, prolonged standing can increase hydrostatic pressure in the lower extremities, potentially leading to the appearance of petechiae in the legs and ankles.
Hematologic and Coagulation Disorders
These conditions directly impact the components of blood responsible for maintaining vascular integrity and hemostasis.
Thrombocytopenia (Low Platelet Count)
Platelets play a vital role in forming primary hemostatic plugs to seal damaged blood vessels. A reduced number of platelets significantly impairs this process, making even minor capillary damage result in bleeding and petechiae. Thrombocytopenia can arise from:
- Decreased Production: Bone marrow disorders such as aplastic anemia, leukemia, myelodysplastic syndromes, and infections can impair platelet production.
- Increased Destruction: Immune thrombocytopenia (ITP), thrombotic thrombocytopenic purpura (TTP), hemolytic-uremic syndrome (HUS), and drug-induced thrombocytopenia lead to premature destruction of platelets.
- Sequestration: Splenomegaly can lead to increased trapping and destruction of platelets in the spleen.
Platelet Dysfunction
Even with a normal platelet count, impaired platelet function can lead to an increased bleeding tendency and petechiae. This can be due to:
- Inherited Disorders: Glanzmann thrombasthenia and Bernard-Soulier syndrome are examples of inherited platelet function defects.
- Acquired Disorders: Medications (e.g., aspirin, clopidogrel), uremia, and myeloproliferative disorders can impair platelet function.
Coagulation Factor Deficiencies
While typically associated with larger bruises and bleeding into joints or muscles, severe deficiencies in coagulation factors can occasionally contribute to petechiae, especially in conjunction with minor trauma or other predisposing factors.
Infections
A wide range of infectious agents can cause petechiae through various mechanisms, including direct vascular damage, inflammation, and disseminated intravascular coagulation (DIC).
Bacterial Infections
- Meningococcemia: A severe bloodstream infection with Neisseria meningitidis that can cause a characteristic petechial or purpuric rash, often with rapid progression to a life-threatening condition.
- Rocky Mountain Spotted Fever: Caused by Rickettsia rickettsii, this tick-borne illness often presents with a petechial rash that starts on the extremities and spreads centrally.
- Scarlet Fever: Caused by Streptococcus pyogenes, the rash in scarlet fever is typically erythematous and sandpaper-like, but petechiae may be present in skin folds (Pastia’s lines).
- Sepsis: Systemic bacterial infections can lead to DIC and widespread petechiae.
Viral Infections
Many viral infections can cause petechiae, often due to thrombocytopenia or viral-induced vasculitis.
- Dengue Fever and Chikungunya: These mosquito-borne viral illnesses can cause thrombocytopenia and petechiae, often accompanied by fever, severe joint pain, and rash.
- Measles and Rubella: While the characteristic rashes are maculopapular, petechiae can sometimes be present.
- Cytomegalovirus (CMV) and Epstein-Barr Virus (EBV): These common viruses can cause thrombocytopenia and petechiae, particularly in immunocompromised individuals.
- Enteroviruses (e.g., Coxsackievirus): Certain enterovirus infections can be associated with petechial rashes.
Rickettsial Infections
Besides Rocky Mountain Spotted Fever, other rickettsial infections can also cause petechiae.
Vasculitis and Inflammatory Conditions
Inflammation of blood vessels can lead to their damage and subsequent leakage of red blood cells.
- Henoch-Schönlein Purpura (IgA Vasculitis): This systemic small-vessel vasculitis, often triggered by an infection, is characterized by a palpable purpuric rash (which can include petechiae), abdominal pain, joint pain, and kidney involvement.
- Systemic Lupus Erythematosus (SLE): This autoimmune disease can cause vasculitis affecting small blood vessels, leading to petechiae.
- Other Vasculitic Syndromes: Various other forms of vasculitis, such as hypersensitivity vasculitis, can manifest with petechiae.
Drug-Induced
Certain medications can cause petechiae as a side effect, often due to drug-induced thrombocytopenia or vasculitis.
- Chemotherapeutic Agents: Many chemotherapy drugs can suppress bone marrow function, leading to thrombocytopenia.
- Antibiotics: Some antibiotics, such as certain penicillins and sulfonamides, have been associated with thrombocytopenia or vasculitis.
- Non-Steroidal Anti-inflammatory Drugs (NSAIDs): Rarely, NSAIDs can cause thrombocytopenia or platelet dysfunction.
- Other Medications: A wide range of other drugs, including certain diuretics and anticonvulsants, can occasionally be implicated.
Nutritional Deficiencies
Certain vitamin deficiencies can affect vascular integrity.
- Vitamin C (Scurvy): Vitamin C is essential for collagen synthesis, which is crucial for the structural integrity of blood vessels. Deficiency can lead to fragile capillaries and petechiae, along with other characteristic signs like bleeding gums and follicular hyperkeratosis.
- Vitamin K: While primarily involved in coagulation factor synthesis, severe vitamin K deficiency can theoretically contribute to increased bleeding, though it less commonly presents as isolated petechiae.
Malignancies
Hematologic malignancies can directly affect platelet production or function, or infiltrate tissues leading to vascular compromise.
- Leukemia: Bone marrow infiltration by leukemic cells can suppress normal hematopoiesis, leading to thrombocytopenia.
- Lymphoma: Similar to leukemia, lymphoma can involve the bone marrow or cause immune-mediated thrombocytopenia.
- Myelodysplastic Syndromes: These bone marrow disorders are characterized by ineffective hematopoiesis, often resulting in thrombocytopenia.
Other Miscellaneous Causes
- Amyloidosis: Deposition of amyloid protein in blood vessel walls can weaken them, leading to increased fragility and petechiae.
- Ehlers-Danlos Syndrome: This group of inherited connective tissue disorders can be associated with fragile blood vessels and easy bruising.
Clinical Presentation and Symptoms
The hallmark of petechiae is their distinctive appearance on the skin or mucous membranes. However, the distribution of these lesions and the presence of accompanying symptoms can provide valuable clues to the underlying etiology.
Characteristic Appearance and Distribution

Common Sites
Petechiae can appear on virtually any part of the body, but some areas are more commonly affected depending on the cause.
- Extremities (especially lower legs): Often seen in vasculitis, infections like Rocky Mountain Spotted Fever, and conditions associated with increased hydrostatic pressure.
- Trunk: Common in viral exanthems, meningococcemia, and some drug reactions.
- Mucous Membranes (e.g., inside the mouth, conjunctivae): Strongly suggestive of thrombocytopenia or platelet dysfunction.
- Areas of Increased Pressure (face, neck, upper chest): May occur after forceful coughing, vomiting, or prolonged crying.
Patterns of Distribution
The way petechiae are distributed can be informative.
- Localized: Suggests a local cause, such as trauma or increased pressure in a specific area.
- Generalized: Often points towards a systemic issue like an infection, hematologic disorder, or vasculitis.
- Palpable Purpura: When petechiae are raised and can be felt, it is highly suggestive of vasculitis, particularly Henoch-Schönlein Purpura.
Associated Symptoms Based on Underlying Cause
The presence or absence of other symptoms is critical in narrowing down the differential diagnosis.
- Fever, chills, malaise: These systemic symptoms are common in infectious etiologies, such as bacterial (e.g., meningococcemia, sepsis), viral (e.g., dengue, measles), and rickettsial infections (e.g., Rocky Mountain Spotted Fever).
- Joint pain (arthralgia), abdominal pain, hematuria (blood in urine): This triad of symptoms is highly characteristic of Henoch-Schönlein Purpura (IgA vasculitis).
- Bleeding from other sites (e.g., nosebleeds, gum bleeding, heavy menstrual periods, gastrointestinal bleeding): These suggest a more generalized bleeding disorder, often due to thrombocytopenia or platelet dysfunction.
- Fatigue, weakness, pallor, weight loss, lymphadenopathy (swollen lymph nodes): These constitutional symptoms may be associated with hematologic malignancies (leukemia, lymphoma) or other systemic illnesses.
- Rash characteristics beyond petechiae: The type of rash accompanying petechiae can be very helpful.
- Maculopapular rash: Often seen in viral infections like measles or rubella.
- Sandpaper-like rash with Pastia’s lines (petechiae in skin folds): Suggestive of scarlet fever.
- Vesicular rash: May be seen in certain viral infections, although petechiae are less common.
- Neurological symptoms (e.g., headache, stiff neck, altered mental status): In the context of petechiae, these are red flags for serious infections like meningococcemia.
- Jaundice (yellowing of the skin and eyes): May suggest liver disease or hemolytic anemia as a potential underlying cause of thrombocytopenia.
- Bone pain: Can be a symptom of bone marrow involvement in leukemia or other malignancies.
Importance of Detailed History Taking
A thorough patient history is paramount in evaluating petechiae.
- Onset and duration of petechiae: When did the petechiae first appear? Have they spread or changed in appearance?
- Recent illnesses: Any recent viral or bacterial infections? Travel history? Exposure to ticks or other vectors?
- Medications: A detailed medication history, including over-the-counter drugs and supplements, is crucial to identify potential drug-induced causes.
- Allergies: While less common, allergic reactions can sometimes manifest with skin findings.
- Bleeding history (personal and family): Any prior episodes of easy bruising, prolonged bleeding after minor cuts, nosebleeds, or a family history of bleeding disorders?
- Systemic symptoms: Inquiry about fever, chills, fatigue, weight loss, joint pain, abdominal pain, headaches, or any other associated symptoms.
Associated Laboratory Investigations
The choice of laboratory investigations in a patient with petechiae is guided by the clinical presentation, the patient’s history, and the suspected underlying etiologies. The initial focus is often on assessing platelet count and coagulation, followed by more specific tests to identify infections, autoimmune disorders, or other potential causes.
Initial Screening Tests
These are typically the first-line investigations to assess the basic hematologic parameters.
- Complete Blood Count (CBC) with Differential: This is a fundamental test that provides information about all the cellular components of blood.
- Platelet Count: This is arguably the most critical initial test in evaluating petechiae. A low platelet count (thrombocytopenia) is a common cause of petechiae. The severity of thrombocytopenia often correlates with the risk of bleeding.
- Hemoglobin and Hematocrit: To assess for anemia, which might be associated with certain underlying conditions like hematologic malignancies or chronic bleeding.
- White Blood Cell (WBC) Count and Differential: An elevated WBC count with a specific differential (e.g., increased neutrophils, lymphocytes, or atypical cells) can suggest infection, inflammation, or hematologic malignancy.
- Peripheral Blood Smear: Examining a blood smear under a microscope can provide valuable qualitative information about blood cells.
- Platelet Morphology: Helps to identify large platelets (megathrombocytes) suggesting increased platelet destruction, or abnormal platelet clumping.
- Red Blood Cell Morphology: Can reveal signs of microangiopathic hemolytic anemia (schistocytes), which may be seen in conditions like TTP or HUS.
- White Blood Cell Morphology: Can identify blasts (immature cells) suggestive of leukemia or atypical lymphocytes seen in viral infections like EBV.
Coagulation Studies
These tests assess the integrity of the coagulation cascade.
- Prothrombin Time (PT) and Activated Partial Thromboplastin Time (aPTT): These tests measure the time it takes for blood to clot via different pathways. Prolonged PT or aPTT might suggest a coagulation factor deficiency or the presence of inhibitors. While less commonly a primary cause of isolated petechiae, they are important in the broader context of bleeding disorders and disseminated intravascular coagulation (DIC).
- Bleeding Time or Platelet Function Assays: If the platelet count is normal but there is a suspicion of platelet dysfunction (e.g., prolonged bleeding history despite adequate platelet numbers), these tests might be ordered. However, bleeding time is less commonly used now due to its poor reproducibility. Platelet function assays assess the ability of platelets to aggregate and adhere.
Tests for Specific Etiologies
Depending on the clinical suspicion, further investigations may be necessary to pinpoint the underlying cause.
- Blood Cultures: If a bacterial infection is suspected (especially with fever, chills, or signs of sepsis), blood cultures are essential to identify the causative organism (e.g., Neisseria meningitidis).
- Viral Serology and PCR: For suspected viral infections (e.g., Dengue, Chikungunya, Measles, EBV, CMV), serological tests can detect specific antibodies, and polymerase chain reaction (PCR) can detect viral genetic material. The choice of test depends on the suspected virus and the stage of infection.
- Autoimmune Markers: If an autoimmune etiology is considered (e.g., SLE, vasculitis), tests like Antinuclear Antibody (ANA), anti-double-stranded DNA (anti-dsDNA), and Antineutrophil Cytoplasmic Antibodies (ANCA) may be ordered.
- IgA Levels: In cases of suspected Henoch-Schönlein Purpura, serum IgA levels may be elevated, although this is not always the case.
- Bone Marrow Biopsy: This invasive procedure is indicated if there is suspicion of a bone marrow disorder as the cause of thrombocytopenia (e.g., leukemia, aplastic anemia, myelodysplastic syndromes) or if other hematologic abnormalities are present. It involves aspirating and/or taking a core biopsy of the bone marrow for microscopic examination.
- Drug Screen: If drug-induced petechiae is a possibility, a thorough medication history is crucial. In some cases, specific drug assays might be available.
- Vitamin Levels: If nutritional deficiency (e.g., Vitamin C deficiency in scurvy) is suspected based on the history and physical exam, measuring serum vitamin levels can be helpful.
Imaging Studies
While not directly used to diagnose petechiae themselves, imaging studies may be indicated based on associated symptoms or to investigate potential underlying conditions.
- Chest X-ray: May be ordered if a respiratory infection is suspected.
- Abdominal Ultrasound: Could be used to assess for splenomegaly (a cause of platelet sequestration) or other organ involvement in conditions like Henoch-Schönlein Purpura.
- CT Scans or MRIs: May be necessary to investigate neurological symptoms or other organ-specific concerns.
Differential Diagnosis
When encountering small red or purple spots on the skin, it’s essential to distinguish petechiae from other lesions that may mimic their appearance. The key difference lies in the underlying pathophysiology: petechiae result from the extravasation of red blood cells due to capillary rupture, and therefore, they do not blanch (fade) when pressure is applied. This is a critical differentiating factor.
Treatment and Management
The primary goal is not to treat the petechiae themselves, as they are merely a sign of an underlying condition. Effective management focuses on identifying and addressing the root cause.The approach to treating and managing petechiae is highly dependent on the underlying etiology. Therefore, a thorough diagnosis is paramount.
Frequently Asked Questions (FAQs)
Is petechiae worrying?
Yes, petechiae can be worrying as they often indicate an underlying medical condition that may range from mild and self-limiting to serious and potentially life-threatening. While some cases can be due to benign causes like increased pressure from coughing or straining, petechiae can also be a sign of thrombocytopenia (low platelet count), infections (such as meningococcemia or Rocky Mountain Spotted Fever), vasculitis, autoimmune disorders, or even hematologic malignancies. Therefore, the appearance of new or unexplained petechiae warrants medical evaluation to determine the underlying cause and ensure timely and appropriate management.
Will petechiae go away?
Yes, petechiae can go away, but this depends entirely on the underlying cause. If the petechiae are due to a minor and self-limiting issue like increased pressure from forceful coughing or vomiting, they will typically fade and disappear on their own within a few days. However, if the petechiae are a symptom of a more serious underlying medical condition, such as an infection, a bleeding disorder, or vasculitis, they will likely persist or even spread until the underlying condition is effectively treated. Therefore, while the spots themselves may eventually resolve, addressing the root cause is the crucial factor in their disappearance and preventing further occurrence.
Which vitamin deficiency has petechiae?
Deficiencies in both vitamin C and vitamin K can lead to petechiae. Vitamin C is crucial for collagen synthesis, which maintains the integrity of blood vessel walls, and its deficiency (scurvy) can result in fragile capillaries that rupture easily. Vitamin K is essential for the production of clotting factors, and a deficiency can impair the body’s ability to form blood clots effectively, leading to increased bleeding and the appearance of petechiae.
Is it normal to get petechiae from scratching?
Yes, it is possible to get petechiae from vigorous or forceful scratching. When you scratch your skin intensely, you can damage the small blood vessels (capillaries) just beneath the surface, causing them to rupture and leak small amounts of blood into the surrounding tissue. This results in the pinpoint red or purple spots characteristic of petechiae along the scratched area. While occasional petechiae from minor trauma like light scratching are usually not a cause for concern, petechiae appearing spontaneously or from minimal pressure might indicate an underlying issue requiring medical attention.
Should I go to a dermatologist for petechiae?
While a dermatologist specializes in skin conditions, petechiae often indicate an underlying systemic issue rather than a primary dermatological problem. Therefore, your first point of contact should ideally be your general practitioner (GP) or primary care physician. They can assess your overall health, consider your medical history and any other symptoms, and perform initial investigations like a blood count to check your platelets. Based on their findings, they can then determine if a referral to a dermatologist or another specialist, such as a hematologist (for blood disorders) or an infectious disease specialist, is necessary. A dermatologist might become involved if the petechiae are part of a broader skin condition or if the diagnosis remains unclear after initial investigations.
How long does petechiae last?
The duration that petechiae last can vary significantly depending on the underlying cause. In cases where petechiae are caused by minor mechanical factors like forceful coughing or straining, they may disappear on their own within a few days to a week. However, if petechiae are a symptom of an underlying medical condition such as an infection, a bleeding disorder, vasculitis, or medication side effect, they will likely persist until the underlying issue is effectively treated. In some instances, petechiae might evolve in appearance over time, changing from red to purple or brownish as the blood is reabsorbed by the body.
Can petechiae get bigger?
Yes, petechiae themselves, as individual spots, typically do not get significantly bigger. They represent a small, localized leakage of blood. However, what can happen is that more petechiae can appear over time, or existing petechiae might coalesce or cluster together, giving the impression that the affected area is growing or the spots are enlarging.
Additionally, if the underlying condition causing the petechiae worsens or if there is ongoing bleeding, the number of petechiae can increase and they might spread to new areas of the body. In some cases, smaller petechiae can also be accompanied by larger areas of bruising (ecchymoses) or purpura, which are also caused by blood leaking under the skin but involve a larger volume of blood.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Goldberg S, Hoffman J. Clinical Hematology Made Ridiculously Simple, 1st Edition: An Incredibly Easy Way to Learn for Medical, Nursing, PA Students, and General Practitioners (MedMaster Medical Books). 2021.
- Scott J, Clarke C, Marchell R. Petechiae, Purpura, and Hemorrhagic Vesicles. JAMA Dermatol. 2017 Jul 1;153(7):707-708. doi: 10.1001/jamadermatol.2016.5965. PMID: 28146222.
- McGrath A, Barrett MJ. Petechiae. [Updated 2023 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482331/
- Sweet JM, Mulkey BH. Lower Extremity Petechiae and Purpura. Am Fam Physician. 2020 May 1;101(9):567-568. PMID: 32352732.
- Vaishya R, Vaish A, Iyengar KP. Exercise-induced petechiae (EIP) of the forearm after intense, railing-assisted squat exercise. BMJ Case Reports CP 2023;16:e255969.




