TL;DR
Atypical lymphocytes are reactive, morphologically altered lymphocytes (mainly activated T cells) that appear in the peripheral blood. They indicate an active immune response, not necessarily malignancy.
- Common Causes ▾: The most frequent triggers are viral infections (like EBV, CMV, COVID-19), but they can also be seen in certain bacterial/parasitic infections, drug reactions, and some autoimmune conditions.
- Key Challenge ▾: It is vital to differentiate these benign, reactive atypical lymphocytes from malignant lymphoid cells found in certain leukemias or lymphomas. This often requires detailed blood smear review and specialized tests like flow cytometry.
- Management ▾: Treatment focuses on addressing the underlying cause; supportive care is often sufficient for common viral etiologies.
*Click ▾ for more information
Introduction
What are Atypical Lymphocytes (Reactive Lymphocytes)?
Atypical lymphocytes, also known as reactive lymphocytes or activated lymphocytes, are lymphocytes that have undergone morphological changes in response to an immune stimulus.
These changes are a hallmark of immune activation and proliferation, distinguishing them from the quiescent morphology of normal, mature lymphocytes. The term “atypical” refers to their departure from the typical appearance of resting lymphocytes, rather than necessarily indicating malignancy.
Their presence often serves as a significant indicator of an active immune response, most commonly triggered by viral infections. It prompts clinicians to investigate the underlying cause, guiding appropriate diagnostic testing (e.g., serology for EBV or CMV).
Brief Review of Normal Lymphocyte Function and Morphology
Lymphocytes are essential components of the adaptive immune system, playing a critical role in specific immunity against pathogens, foreign substances, and even cancerous cells. They are broadly categorized into two main types:
- B lymphocytes (B cells): Primarily responsible for humoral immunity. Upon activation, they differentiate into plasma cells, which produce antibodies. These antibodies circulate in the bloodstream and lymph, targeting and neutralizing specific antigens.
- T lymphocytes (T cells): Mediate cell-mediated immunity. There are several subtypes:
- Helper T cells (CD4+ T cells): Coordinate immune responses by activating other immune cells, such as B cells, cytotoxic T cells, and macrophages.
- Cytotoxic T cells (CD8+ T cells): Directly kill infected or cancerous cells by inducing apoptosis.
- Regulatory T cells (Tregs): Suppress immune responses to prevent autoimmunity and maintain immune tolerance.
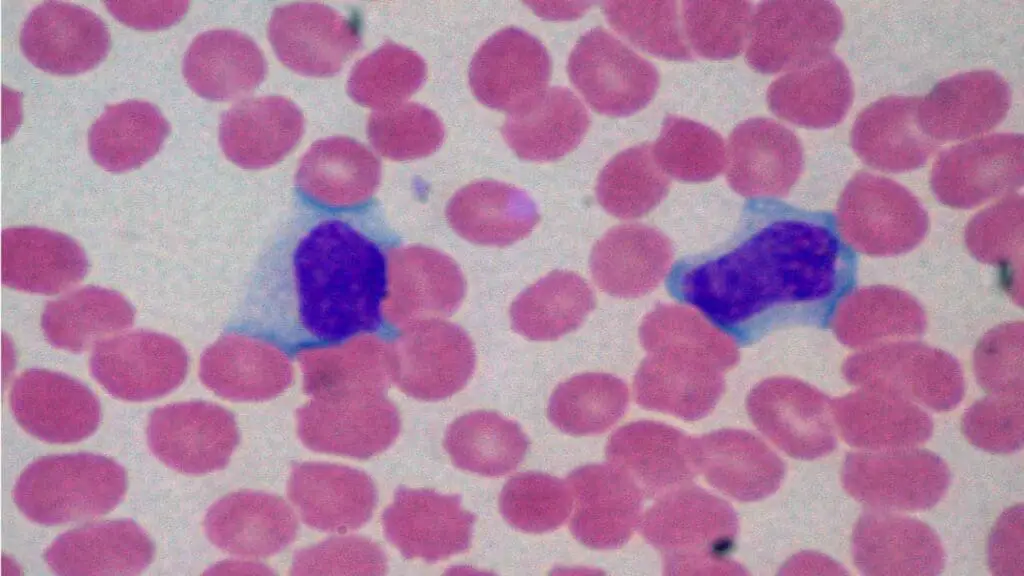
Morphology of Normal Lymphocytes: In a peripheral blood smear, normal, mature lymphocytes are typically characterized by:

- Size: Small to medium-sized, ranging from 7 to 10 μm in diameter, similar to a red blood cell or slightly larger.
- Nucleus: Round or oval, centrally located, and occupies the majority of the cell volume. The chromatin is densely clumped, appearing dark blue-purple, and nucleoli are usually indistinct or absent.
- Cytoplasm: Scant and clear, appearing as a thin, sky-blue rim around the nucleus. Granules are typically absent.
- Nuclear-to-Cytoplasmic (N:C) Ratio: High, typically around 4:1 or even higher, reflecting the large nucleus and minimal cytoplasm.
Morphological Characteristics of Atypical Lymphocytes (Reactive Lymphocytes)
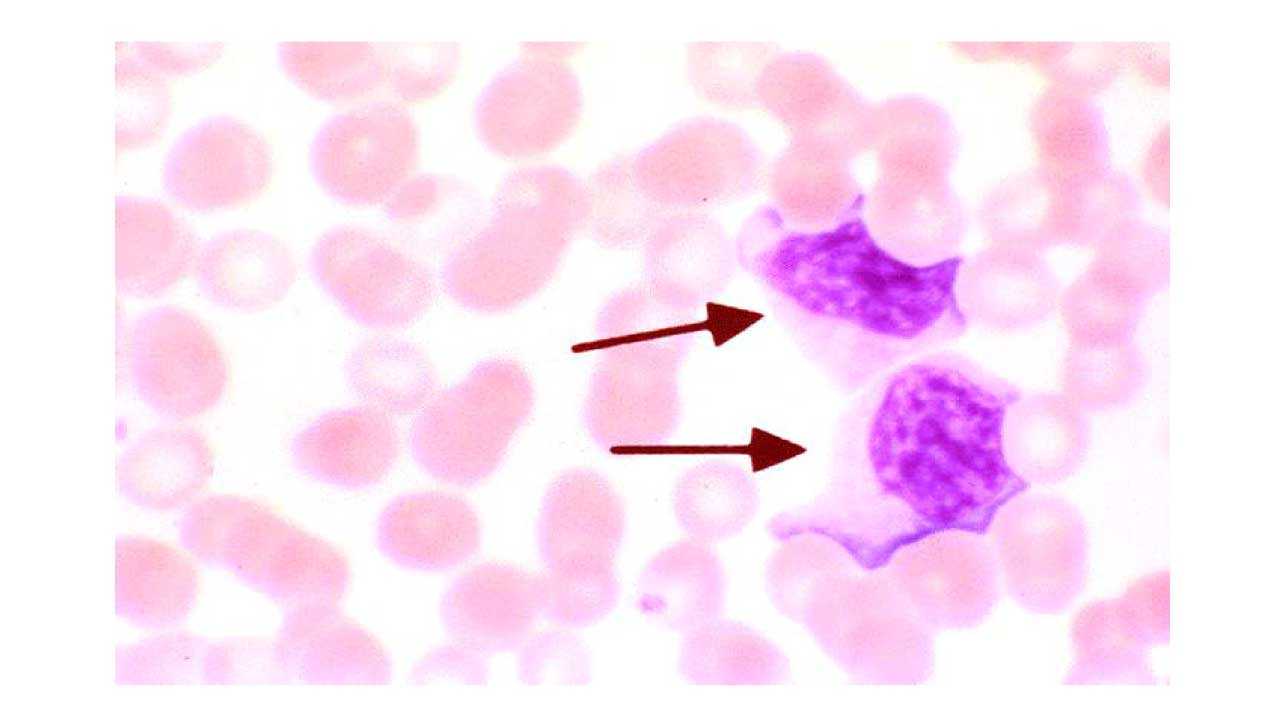
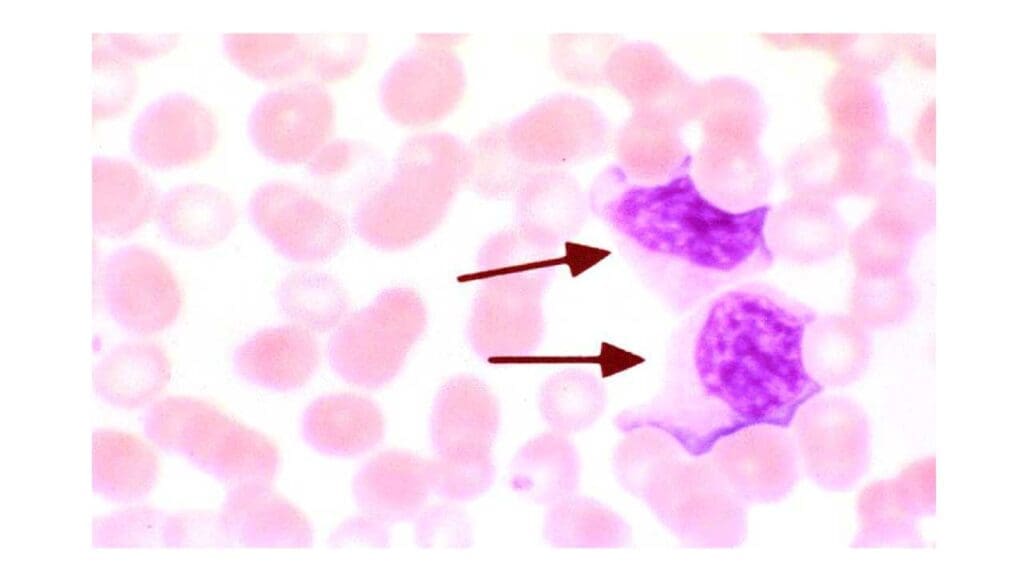
- Size: Often significantly larger than normal lymphocytes, ranging from 10 to 30 μm in diameter, and can even be larger than monocytes.
- Nuclear Shape: The nucleus can be round, oval, kidney-shaped, indented, or even lobulated, departing from the typical round or oval shape. Chromatin may be less condensed than in normal lymphocytes, appearing finer or more dispersed, and nucleoli may become visible or prominent.
- Cytoplasm: Abundant and often deeply basophilic (dark blue) due to increased RNA content, indicative of active protein synthesis. The cytoplasm may appear vacuolated. A characteristic feature, particularly in infectious mononucleosis, is a “scalloped” or irregular cytoplasmic border that often appears to indent or wrap around adjacent red blood cells.
- Nuclear-to-Cytoplasmic (N:C) Ratio: Reduced compared to normal lymphocytes due to the increased cytoplasmic volume, though still relatively high compared to many other cell types.
- Other features: Occasional cytoplasmic granules may be present, though less prominent than in granulocytes.
The morphological changes seen in atypical lymphocytes are a direct reflection of their functional activation.
When the immune system encounters a pathogen or foreign antigen, specific lymphocytes are activated, proliferate rapidly, and differentiate into effector cells. This process requires increased metabolic activity, leading to the cellular enlargement and altered cytoplasmic and nuclear features observed.
For instance, in viral infections like infectious mononucleosis, cytotoxic T cells become activated and proliferate extensively to combat the virus-infected cells, leading to their atypical morphology. These cells are actively involved in immune surveillance and direct killing or regulation of other immune cells.
Common Misconceptions About Atypical Lymphocytes
- Atypical = Cancer: This is the most prevalent misconception. While some malignant cells can have atypical features, the vast majority of cases of atypical lymphocytes (reactive lymphocytes) seen in routine clinical practice are reactive and benign, primarily caused by viral infections. It is a sign of an active, healthy immune response, not necessarily a disease state itself.
- The Cause is Always Infectious Mononucleosis: While infectious mononucleosis (due to EBV) is the classic and most common cause of significant atypical lymphocytosis, many other conditions, including other viral infections (CMV, HIV, viral hepatitis), bacterial infections, drug reactions, and even some autoimmune conditions, can also lead to their presence.
- The Number of Atypical Lymphocytes Correlates with Disease Severity: While a higher percentage of atypical lymphocytes (reactive lymphocytes) might suggest a more robust immune response, it doesn’t directly correlate with the severity of the patient’s symptoms or the prognosis of the underlying condition. A patient with severe symptoms might have only a modest number of atypical cells, and vice versa.
- Atypical Lymphocytes are Pathognomonic for a Specific Condition: Atypical lymphocytes (reactive lymphocytes) are a non-specific finding. Their presence indicates immune activation but does not, on its own, pinpoint a single diagnosis. Clinical context, history, physical examination, and further laboratory tests are always required to determine the specific etiology.
- Atypical Lymphocytes Mean You Need Antibiotics: Since the most common causes are viral, antibiotics are generally ineffective and inappropriate. This misconception can lead to unnecessary antibiotic use and contribute to antimicrobial resistance.
Causes of Atypical Lymphocytosis
The presence of atypical lymphocytes (reactive lymphocytes) in the peripheral blood is a strong indicator of an active immune response.
Infectious Causes
The most common triggers for atypical lymphocytosis are infections, particularly viral ones, as the immune system mounts a robust defense.
Viral Infections (Most Common)
These are by far the leading cause of atypical lymphocytes (reactive lymphocytes). The atypical morphology often represents activated cytotoxic T cells (CD8+ T cells) that are proliferating to eliminate virus-infected cells.
- Epstein-Barr Virus (EBV) – Infectious Mononucleosis:
- Pathophysiology: EBV primarily infects B lymphocytes. The body’s immune response to these infected B cells is dominated by a strong proliferation of CD8+ cytotoxic T cells, which become morphologically atypical. These “activated” T cells are the classical “Downey cells” seen in infectious mononucleosis.
- Clinical Presentation: Characterized by the classic triad of fever, pharyngitis (often severe with exudates), and lymphadenopathy (especially cervical). Splenomegaly is common, and fatigue can be profound and protracted.
- Characteristic Lab Findings: Besides atypical lymphocytosis (often >10-20% of total WBCs, sometimes up to 70-80%), a positive heterophile antibody test (Monospot) and specific EBV serology (VCA IgM positive for acute infection) are diagnostic.
- Cytomegalovirus (CMV): CMV infection can cause a mononucleosis-like syndrome with fever, malaise, lymphadenopathy, and significant atypical lymphocytosis. CMV mononucleosis typically lacks the severe pharyngitis seen in EBV. Diagnosis is made through CMV serology (IgM for acute infection) or PCR for CMV DNA.
- HIV Infection (Acute Seroconversion Syndrome): During the acute phase of HIV infection (seroconversion), a mononucleosis-like illness can occur, often accompanied by a transient rash, fever, and generalized lymphadenopathy. Atypical lymphocytosis is a common hematological finding as the immune system reacts to the initial viral surge.
- Viral Hepatitis (Hepatitis A, B, C): Acute viral hepatitis can trigger a reactive atypical lymphocytosis, reflecting the immune response to the liver infection. Elevated liver enzymes will also be a key finding.
- Adenovirus: Commonly causes respiratory tract infections, pharyngitis, and conjunctivitis. Can lead to a mild to moderate atypical lymphocytosis, particularly in children.
- Varicella-Zoster Virus (VZV): The virus causing chickenpox and shingles can induce a reactive atypical lymphocytosis during acute infection.
- Human Herpesvirus 6 (HHV-6): Primarily known for causing Roseola Infantum (Exanthem Subitum) in young children, which presents with high fever followed by a rash. Atypical lymphocytes (reactive lymphocytes) can be seen during the febrile phase.
- Dengue Virus: A common cause of acute febrile illness in tropical regions. Dengue infection can cause significant atypical lymphocytosis, which, along with thrombocytopenia, can mimic other acute febrile illnesses.
Bacterial Infections
While less common than viral causes, some bacterial infections can elicit an atypical lymphocytic response.
- Mycobacterium tuberculosis (Tuberculosis): While often associated with monocytosis, chronic tuberculosis, especially extrapulmonary forms or disseminated disease, can sometimes lead to a reactive lymphocytosis, and atypical forms may be present as part of the immune response, particularly in lymph node involvement.
- Bartonella henselae (Cat Scratch Disease): Causes regional lymphadenopathy, often after a cat scratch or bite. While typically causing neutrophilia, reactive atypical lymphocytes can sometimes be observed in the peripheral blood.
- Syphilis (Secondary Stage): The generalized lymphadenopathy and systemic symptoms (fever, rash, malaise) of secondary syphilis can be associated with a reactive lymphocytosis, including atypical forms.
- Other Bacterial Infections: Less commonly, conditions like Bordetella pertussis (whooping cough) can cause marked lymphocytosis, though not always predominantly atypical lymphocytes (reactive lymphocytes).
Parasitic Infections
- Toxoplasma gondii (Toxoplasmosis): A parasitic infection that can mimic infectious mononucleosis, causing fever, lymphadenopathy (often cervical and non-tender), and sometimes hepatosplenomegaly. Atypical lymphocytosis, mild anemia, and elevated liver enzymes are common. Diagnosis is confirmed by Toxoplasma serology.
- Malaria (Acute Phase): Acute malaria can sometimes present with atypical lymphocytes (reactive lymphocytes), along with thrombocytopenia, mimicking other tropical febrile illnesses like dengue. Microscopic examination of blood for parasites is essential for diagnosis in endemic areas.
Non-Infectious Causes
Beyond infections, several other conditions can lead to the appearance of atypical lymphocytes (reactive lymphocytes).
Drug Reactions
Certain medications can trigger a hypersensitivity reaction that includes immune activation and the presence of atypical lymphocytes (reactive lymphocytes). This is often part of a broader syndrome.
- Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS Syndrome): A severe, sometimes life-threatening, idiosyncratic drug reaction. It’s characterized by fever, widespread skin rash, lymphadenopathy, eosinophilia, and involvement of internal organs (e.g., liver, kidney, lung). Atypical lymphocytes (reactive lymphocytes) are a common hematological finding.
- Common Culprit Drugs:
- Anticonvulsants: Phenytoin, Carbamazepine, Phenobarbital.
- Sulfonamides: A group of antibiotics and other drugs.
- Dapsone: Used in the treatment of leprosy and certain dermatological conditions.
- Allopurinol (used for gout).
Autoimmune Diseases
In conditions where the immune system is dysregulated and attacks the body’s own tissues, a reactive lymphocytosis with atypical forms can sometimes occur.
- Systemic Lupus Erythematosus (SLE): While lymphopenia is often a feature, reactive lymphocytosis, sometimes with atypical forms, can be seen during flares or in response to therapies. The overall picture will guide the diagnosis.
- Rheumatoid Arthritis (RA): Less common, but chronic inflammation in autoimmune conditions can sometimes lead to reactive changes in lymphocytes.
Stress/Post-surgical states
Physiological stress, trauma, or the post-surgical period can sometimes induce a transient, mild reactive lymphocytosis with a few atypical forms, reflecting the body’s general inflammatory and immune response.
Splenectomy
The spleen acts as a filter and reservoir for various blood cells, including lymphocytes. After a splenectomy, there can be a persistent, usually mild, increase in lymphocyte count, and a small percentage of these might exhibit atypical features as the immune system compensates for the absence of the splenic filter.
Malignancies (to differentiate from truly atypical)
This category is crucial because while these are not causes of reactive atypical lymphocytosis, the atypical lymphocytes (reactive lymphocytes) themselves can be confused with malignant cells. A thorough evaluation is very important.
- Acute Lymphoblastic Leukemia (ALL): Malignant lymphoblasts are immature cells that can sometimes be mistaken for highly atypical reactive lymphocytes. However, blasts typically exhibit a more uniform, immature morphology, often with prominent nucleoli, fine chromatin, and a lack of mature cytoplasmic features. Flow cytometry is essential for differentiation.
- Chronic Lymphocytic Leukemia (CLL): While classic CLL lymphocytes are small and mature, a variant called prolymphocytic transformation (or CLL/PLL) can occur where a significant number of cells with prominent nucleoli and abundant cytoplasm (prolymphocytes) are seen. These can appear atypical. In rare cases, CLL itself can present with some reactive-appearing lymphocytes, but the underlying clonal population is the key.
- Lymphoma: Certain lymphomas, particularly those with a leukemic phase (e.g., some T-cell lymphomas like Sézary syndrome, or mantle cell lymphoma), can shed malignant cells into the peripheral blood that might have an atypical or “transformed” appearance.
- Myelodysplastic Syndromes (MDS): While primarily affecting myeloid cell lines, some MDS subtypes can be associated with reactive lymphocytosis as part of the dysregulated hematopoiesis.
General Signs and Symptoms Associated with Atypical Lymphocytosis
When atypical lymphocytes (reactive lymphocytes) are present in the blood, the patient’s symptoms are usually those of the illness that triggered the immune activation. Since infections, particularly viral ones, are the most common cause, the symptoms often resemble those of a common cold, flu, or a mononucleosis-like syndrome.
Therefore, a thorough patient history and physical examination, followed by targeted laboratory investigations, are essential to identify the specific cause of the atypical lymphocyte (reactive lymphocyte) presence. The presence and combination of these symptoms, along with epidemiological factors (e.g., recent travel for dengue, contact history for EBV), will help narrow down the differential diagnosis.
- Fever: This is one of the most common and earliest symptoms, indicating an active immune response to an infection or inflammatory process. The fever can range from low-grade to high, depending on the severity and type of underlying cause.
- Fatigue/Malaise: A general feeling of tiredness, lack of energy, and discomfort is very common. In some conditions, like infectious mononucleosis, fatigue can be profound and long-lasting.
- Sore Throat (Pharyngitis): Especially prominent in viral infections affecting the upper respiratory tract, such as Epstein-Barr Virus (EBV) or Adenovirus. The throat can appear red and inflamed, sometimes with exudates (pus).
- Lymphadenopathy: Swollen and tender lymph nodes are a classic sign of immune system activation. This can occur in various regions.
- Splenomegaly: Enlargement of the spleen is particularly common in viral infections like infectious mononucleosis and cytomegalovirus (CMV) due to the proliferation of lymphocytes within the splenic parenchyma. A palpable spleen may or may not be associated with left upper quadrant abdominal discomfort. This is a critical sign as it carries a risk of splenic rupture, especially with trauma.
- Rash: Various types of rashes can occur, depending on the underlying cause. For example:
- A generalized maculopapular rash can be seen in acute HIV seroconversion or certain drug reactions.
- A specific rash (e.g., Roseola in HHV-6, petechial rash in severe dengue) might provide clues to the diagnosis.
- Patients with infectious mononucleosis treated with ampicillin or amoxicillin often develop a characteristic maculopapular rash.
- Myalgia/Arthralgia: Muscle aches (myalgia) and joint pain (arthralgia) are common systemic symptoms accompanying viral infections and inflammatory conditions.
Laboratory Investigations in Atypical Lymphocytosis
The discovery of atypical lymphocytes (reactive lymphocytes) on a routine complete blood count (CBC) with differential immediately prompts further investigation. The goal of laboratory investigations is to differentiate between benign reactive causes (which are most common) and potentially more serious conditions, including malignancies, and to pinpoint the specific etiology.
Complete Blood Count (CBC) with Differential
This is usually the initial test that flags the presence of atypical lymphocytes (reactive lymphocytes).
The CBC will show an elevated total white blood cell (WBC) count, often due to an absolute lymphocytosis (an increase in the total number of lymphocytes). The percentage of lymphocytes may also be significantly elevated.
Most automated hematology analyzers can flag “atypical lymphocytes” (reactive lymphocytes) or “variant lymphocytes.” However, visual microscopic review is essential for accurate enumeration and morphological assessment. A percentage of atypical lymphocytes (reactive lymphocytes) often exceeding 10-20% is considered significant and commonly seen in conditions like infectious mononucleosis.
Anemia or thrombocytopenia (low platelets) can sometimes be present, especially in more severe or systemic infections, or could raise suspicion for a bone marrow disorder if significant.
Peripheral Blood Smear Review (Crucial Step)
This is perhaps the most critical initial investigation following the CBC, as it allows for direct visualization and detailed assessment of the atypical cells.
- Detailed Morphological Description of Atypical Lymphocytes:
- Large size: Compared to normal lymphocytes.
- Irregular nuclear contours: The nucleus may be kidney-shaped, indented, or lobulated.
- Prominent nucleoli: Although not always present, visible nucleoli can be a feature of activated lymphocytes.
- Abundant basophilic cytoplasm: The cytoplasm appears dark blue and plentiful, often with vacuoles.
- Indented cytoplasm by red blood cells: The classic “scalloped” appearance of the cytoplasm wrapping around or indenting adjacent red blood cells is highly suggestive of reactive atypical lymphocytes, particularly in infectious mononucleosis.
- Differentiation from Blasts (Immature Lymphoid or Myeloid Cells) and Other Reactive Forms: Blasts, indicative of acute leukemia, typically have a more uniform immature appearance, finer chromatin, and more prominent nucleoli, often lacking the “scalloped” cytoplasm. Distinguishing these requires expertise and often further specialized tests.
Flow Cytometry
This specialized test is typically reserved for cases where there is a suspicion of a lymphoproliferative disorder (leukemia or lymphoma) or if the atypical lymphocytes (reactive lymphocytes) persist, increase, or have ambiguous morphology on the blood smear.
- Reactive cells: Show a polyclonal pattern (mixture of T and B cells, often predominantly T cells), with normal expression of various T-cell or B-cell markers.
- Malignant cells: Typically show a monoclonal pattern (all cells derived from a single clone), with aberrant expression or absence of specific markers, helping to diagnose leukemia or lymphoma.
Other Relevant Investigations Based on Clinical Suspicion
- Serological Testing for Infectious Agents: Serology is used to pinpoint common infectious causes.
- Liver Function Tests (LFTs): Often elevated in viral hepatitis, infectious mononucleosis, and CMV infections.
- C-Reactive Protein (CRP) / Erythrocyte Sedimentation Rate (ESR): Non-specific markers of inflammation that can be elevated in various infections or inflammatory conditions.
- Autoimmune Markers: If an autoimmune disease is suspected (e.g., ANA for SLE).
- Drug Screens/History: To identify potential drug-induced causes.
Treatment and Management of Atypical Lymphocytosis
The approach to treating and managing atypical lymphocytosis hinges entirely on identifying and addressing the specific underlying cause. In most cases, especially those caused by common viral infections, the condition is self-limiting and requires only supportive care.
Frequently Asked Questions (FAQs)
Does COVID cause atypical lymphocytes?
Yes, COVID-19 (caused by SARS-CoV-2) can definitely cause atypical lymphocytes (reactive lymphocytes).
While lymphopenia (a decrease in the total lymphocyte count) was a more frequently reported hallmark of severe COVID-19, studies have consistently shown the presence of atypical or reactive lymphocytes in the peripheral blood of COVID-19 patients.
What cancers cause atypical lymphocytes?
While most atypical lymphocytes are reactive to infections, certain cancers, specifically lymphoproliferative disorders, can present with malignant lymphocytes that appear “atypical” or frankly abnormal in the peripheral blood.
- Reactive Atypical Lymphocytes: These are normal lymphocytes that have become activated and changed their appearance in response to a stimulus (like a viral infection). They are part of a healthy immune response.
- Malignant Lymphocytes (from cancer): These are abnormal, cancerous lymphocytes that are proliferating uncontrollably. Their “atypical” appearance is due to their malignant nature, not a normal immune activation.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- https://ashpublications.org/thehematologist/article/doi/10.1182/hem.V22.2.2025210/535833/A-Hematopathologist-s-Approach-to-Atypical
- Cunha, B.A., Connolly, J.J. & Irshad, N. Are atypical lymphocytes present with viral influenza-like illnesses (ILIs) in hospitalized adults?. Eur J Clin Microbiol Infect Dis 35, 1399–1401 (2016). https://doi.org/10.1007/s10096-016-2675-z
- Cano RLE, Lopera HDE. Introduction to T and B lymphocytes. In: Anaya JM, Shoenfeld Y, Rojas-Villarraga A, et al., editors. Autoimmunity: From Bench to Bedside [Internet]. Bogota (Colombia): El Rosario University Press; 2013 Jul 18. Chapter 5. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459471/
- Hamad H, Mangla A. Lymphocytosis. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK549819/