TL;DR
Basophilia (High basophils) are abnormally high absolute basophil count (typically > 0.1 x 109/L).
- Role of Basophils ▾: Primarily involved in allergic reactions (releasing histamine, heparin, leukotrienes), defense against parasites, and modulating immune responses (especially Th2). They also contribute to chronic inflammation.
- Causes ▾: The most significant are Myeloproliferative Neoplasms (MPNs) like CML, PV, ET, and PMF. Other causes include allergic reactions, chronic inflammatory conditions (e.g., IBD, RA), and hypothyroidism.
- Symptoms ▾: Generally, basophilia itself causes no specific symptoms. Symptoms are related to the underlying cause (e.g., fatigue, splenomegaly, itching in MPNs; allergic symptoms; signs of chronic inflammation).
- Investigations ▾: Starts with CBC and peripheral blood smear review. If MPN is suspected, bone marrow examination and molecular genetic testing (e.g., BCR-ABL1, JAK2) are crucial. Allergy testing or thyroid function tests are done if those causes are suspected.
- Treatment ▾: Focuses entirely on treating the underlying condition (e.g., TKIs for CML, antihistamines for allergies, thyroid hormone for hypothyroidism).
*Click ▾ for more information
Introduction
Basophilia is a medical condition characterized by an abnormally high number of basophils in the circulating blood. While basophils are the least common granulocyte, an elevated count usually indicates an underlying health issue, such as allergic reactions, chronic inflammatory conditions, or, most notably, myeloproliferative neoplasms like chronic myeloid leukemia.
What is the function of basophils?
Basophils, though the least abundant type of white blood cell, play crucial roles in the immune system, particularly in mediating allergic reactions and contributing to defense against certain pathogens.
Allergic and Hypersensitivity Reactions
This is perhaps their most well-known function. Basophils express high-affinity receptors (FcεRI) for immunoglobulin E (IgE) antibodies on their surface. When an allergen (a foreign substance) binds to these IgE antibodies, it triggers a process called degranulation. During degranulation, basophils rapidly release pre-formed mediators stored in their cytoplasmic granules. These mediators include:
- Histamine: A potent vasodilator that increases blood flow to the affected area, leading to redness and swelling. It also increases vascular permeability, allowing other immune cells and fluid to reach the site of inflammation. This contributes to classic allergic symptoms like itching, runny nose, and watery eyes.
- Heparin: An anticoagulant that helps prevent blood clots from forming too quickly, ensuring that blood flow is maintained to the inflamed area, which is important for healing and immune cell recruitment.
- Leukotrienes and Cytokines (e.g., IL-4, IL-13): These are newly synthesized mediators that further amplify the inflammatory response, attract other immune cells (like eosinophils), and influence the differentiation of T helper cells (specifically promoting Th2 responses, which are central to allergic reactions and anti-parasitic immunity).
Host Defense Against Parasites
While eosinophils are the primary cells for fighting parasitic infections, basophils also contribute. Their release of mediators and cytokines helps to recruit and activate other immune cells necessary for clearing parasitic worms and other large pathogens.
Modulation of Immune Responses
Beyond immediate reactions, basophils can influence the broader immune response. Their production of cytokines, particularly IL-4, is important for:
- B cell activation: Promoting B cells to produce antibodies, including IgE.
- T cell differentiation: Guiding CD4+ T cells towards a Th2 phenotype, which is crucial for allergic responses and immunity against extracellular pathogens.
- Cross-talk with other immune cells: Interacting with and activating other cells of both the innate and adaptive immune system.
Contribution to Chronic Inflammatory Processes
Basophils, through their sustained release of inflammatory mediators and their capacity to promote Type 2 immune responses and interact with other immune cells, act as important contributors to the perpetuation and exacerbation of chronic inflammatory processes, particularly those with an allergic or Th2-driven component. Their presence and activity in chronically inflamed tissues exacerbate conditions such as asthma, atopic dermatitis, and inflammatory bowel disease.
Basophils fuel chronic inflammation by:
- Sustained release of inflammatory chemicals: Continuously releasing substances like histamine and leukotrienes that maintain inflammation.
- Driving Type 2 immunity: Producing cytokines (like IL-4 and IL-13) that promote allergic-type responses and recruit other inflammatory cells, particularly eosinophils.
- Interacting with other immune cells: Influencing cells like dendritic cells and T cells to perpetuate the chronic inflammatory cycle.
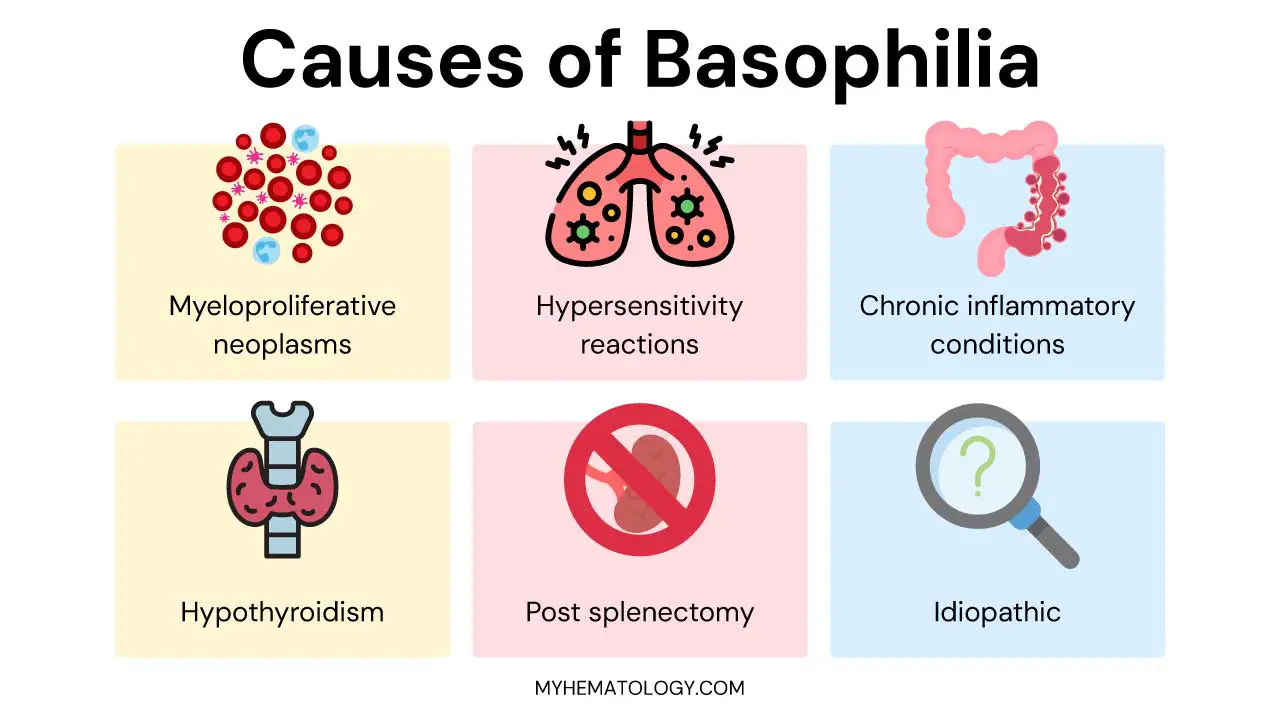
Causes of Basophilia (High Basophils)
Basophilia, an elevated basophil count, is not a disease in itself but rather a sign of an underlying medical condition. The causes can broadly be categorized into several groups, ranging from reactive (part of an immune response) to neoplastic (related to blood cancers).
Myeloproliferative Neoplasms (MPNs)
These are the most significant and often serious causes of persistent basophilia (high basophils). MPNs are a group of chronic conditions where the bone marrow produces too many of one or more types of blood cells. Basophilia (high basophils) is a common feature because basophils originate from the myeloid stem cell line, which is dysregulated in these disorders.
- Chronic Myeloid Leukemia (CML): This is the classic example and often the first condition suspected with significant basophilia (high basophils). CML is characterized by the presence of the Philadelphia chromosome (t(9;22)), which creates the BCR−ABL1 fusion gene. Basophilia (high basophils) can be one of the earliest and most prominent findings in CML, and very high basophil counts can indicate disease progression.
- Polycythemia Vera (PV): Characterized by an overproduction of red blood cells, but often also involves increased white blood cells (including basophils) and platelets. Many patients have a JAK2 V617F mutation.
- Essential Thrombocythemia (ET): Primarily involves an overproduction of platelets, but can also be associated with mild to moderate basophilia (high basophils). Often linked to JAK2, CALR, or MPL mutations.
- Primary Myelofibrosis (PMF): Marked by bone marrow fibrosis, leading to ineffective blood cell production and often causing extramedullary hematopoiesis (blood cell production outside the bone marrow), splenomegaly, and can present with basophilia (high basophils).
- Other less common MPNs: Such as atypical CML or chronic myelomonocytic leukemia (CMML), can also involve basophilia (high basophils).
Allergic and Hypersensitivity Reactions
Basophils are key players in allergic responses, so their numbers can increase, especially in chronic or severe allergic conditions. This is a “reactive” cause, meaning the body is responding to an allergen.
- Acute allergic reactions: Although less common for prominent basophilia compared to eosinophilia, severe reactions like anaphylaxis, acute urticaria, or angioedema can cause a transient increase.
- Chronic allergic conditions: Persistent exposure to allergens in conditions like allergic asthma, chronic allergic rhinitis, or atopic dermatitis can lead to sustained, albeit usually mild to moderate, basophilia.
- Drug or food allergies: Specific reactions to medications or foods can sometimes trigger basophilia.
Chronic Inflammatory and Infectious Conditions
Basophils contribute to and are influenced by chronic inflammation, so their numbers can rise in various inflammatory and certain infectious states.
- Inflammatory Bowel Disease (IBD): Both Crohn’s disease and ulcerative colitis are often associated with basophilia (high basophils), reflecting the chronic immune activation in the gut.
- Rheumatoid Arthritis (RA): Another autoimmune inflammatory condition where basophilia (high basophils) can sometimes be observed.
- Chronic infections: While eosinophilia is more common in parasitic infections, basophilia (high basophils) can occasionally be seen. Certain chronic bacterial infections (like tuberculosis) or some viral infections (e.g., influenza) have also been linked to basophilia.
- Other autoimmune diseases: Like lupus, though less frequently causes basophilia (high basophils).
Endocrine Disorders
- Hypothyroidism (Myxedema): A well-known association, where an underactive thyroid gland can lead to a general slowing of metabolic processes, which can include increased basophil counts. The mechanism is not fully understood but may involve altered cytokine regulation.
Post-Splenectomy
After surgical removal of the spleen, there can be a transient increase in various blood cell counts, including basophils, as the spleen normally filters these cells from circulation.
Idiopathic Basophilia (High Basophils)
In some rare cases, after a thorough investigation, no underlying cause can be identified. This is then termed idiopathic basophilia, a diagnosis of exclusion.
Signs and Symptoms Associated with Basophilia
Basophilia (high basophils) itself typically does not cause specific signs or symptoms. Instead, the signs and symptoms observed in a patient with basophilia are almost entirely those of the underlying condition that is causing the elevated basophil count.
Therefore, when evaluating a patient with basophilia (high basophils), the clinician’s focus shifts to identifying the primary disease process.
Symptoms Related to Myeloproliferative Neoplasms (MPNs)
Since MPNs are a frequent cause of sustained basophilia (high basophils), their symptoms are often the ones encountered. These symptoms are generally non-specific and can overlap with many other conditions, highlighting the need for a thorough workup.
- Constitutional Symptoms (“B Symptoms”): These are systemic symptoms that often indicate a chronic inflammatory state or a malignancy.
- Fatigue: Persistent and profound tiredness, often not relieved by rest.
- Unexplained weight loss: Significant weight loss without intentional dieting or exercise.
- Night sweats: Drenching sweats that require changing clothes or bedding.
- Low-grade fever: Persistent fever without an obvious infection.
- Splenomegaly: An enlarged spleen, which can lead to:
- Abdominal fullness or discomfort: Especially in the left upper quadrant.
- Early satiety: Feeling full quickly after eating small amounts due to the spleen pressing on the stomach.
- Left upper quadrant pain: From the enlarged spleen itself or splenic infarction.
- Symptoms related to other cell line abnormalities (often co-occurring with basophilia in MPNs):
- Anemia (low red blood cells): Pallor, shortness of breath, dizziness, weakness.
- Thrombocytosis (high platelets): Easy bruising or bleeding (paradoxically, very high platelets can impair clotting), erythromelalgia (burning pain and redness in hands and feet, often in PV), or a tendency towards blood clots (thrombosis).
- Leukocytosis (high white blood cells): Increased susceptibility to infections.
- Pruritus (Itching): Often a prominent symptom in MPNs, particularly Polycythemia Vera, and is thought to be partly due to histamine release from increased basophils and mast cells. It can be generalized and often worsens after a warm bath or shower.
- Bone or joint pain: Can occur, especially in primary myelofibrosis due to abnormal bone marrow activity.
Symptoms Related to Allergic and Hypersensitivity Reactions
If basophilia is part of an allergic response, the symptoms will be classic allergy symptoms, which are the direct result of basophil (and mast cell) degranulation and histamine release.
- Skin
- Urticaria (hives): Itchy, raised red welts on the skin.
- Angioedema: Swelling, often of the face, lips, eyelids, or throat.
- Pruritus: Generalized itching.
- Respiratory
- Sneezing, runny nose, nasal congestion in allergic rhinitis.
- Wheezing, shortness of breath, cough in allergic asthma.
- Gastrointestinal
- Abdominal cramping, nausea, vomiting, diarrhea in food allergies.
- Severe allergic reactions (Anaphylaxis – medical emergency)
- Difficulty breathing or swallowing due to airway swelling.
- Rapid drop in blood pressure (shock).
- Widespread hives and itching.
Symptoms Related to Chronic Inflammatory and Infectious Conditions
The symptoms here will reflect the specific inflammatory process or infection.
- Inflammatory Bowel Disease (IBD): Chronic abdominal pain, diarrhea (often bloody), weight loss, fatigue.
- Rheumatoid Arthritis (RA): Joint pain, stiffness, swelling, fatigue, malaise.
- Chronic Infections (e.g., Tuberculosis): Persistent cough, fever, night sweats, weight loss, fatigue.
Symptoms Related to Endocrine Disorders
- Hypothyroidism: Fatigue, weight gain, cold intolerance, constipation, dry skin, hair loss, slowed heart rate, depression, hoarseness.
Laboratory Investigations to Diagnose the Underlying Cause of Basophilia
Laboratory investigations for basophilia (high basophils) are crucial for identifying the underlying cause, as basophilia (high basophils) itself is a laboratory finding rather than a standalone disease. The diagnostic approach is sequential, starting with common, less invasive tests and progressing to more specialized investigations if an MPN or other serious condition is suspected.
Initial Screening Tests
Complete Blood Count (CBC) with Differential
This is the cornerstone. The automated cell counter will provide the absolute basophil count, which is the most important parameter.
Normal adult reference ranges for absolute basophil count can vary slightly between laboratories and regions, but typically range from 0.02 to 0.1 x 109/L (or 20 to 100 cells/mm3). An elevated absolute count indicates basophilia (high basophils).
Equally important are the counts of other blood cell types (red blood cells, hemoglobin, platelets, neutrophils, eosinophils, lymphocytes, monocytes). For example, basophilia alongside elevated neutrophils, eosinophils, and/or platelets strongly suggests a myeloproliferative neoplasm (MPN). Isolated basophilia (high basophils) is much less common and often points towards allergic or endocrine causes.
Anemia or thrombocytopenia may also be present in MPNs (e.g., myelofibrosis) or chronic inflammatory conditions.
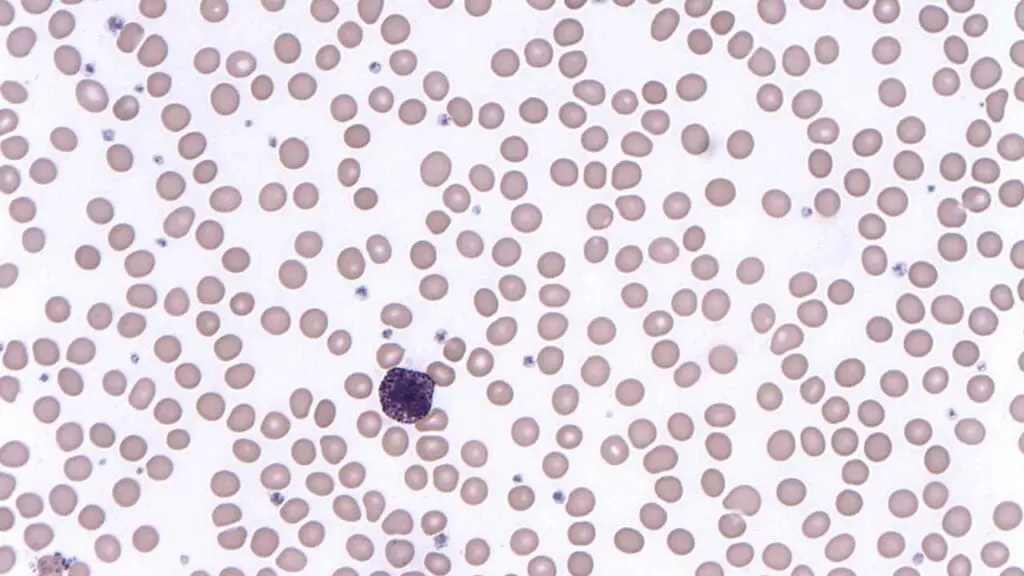
Peripheral Blood Smear Review
This microscopic examination of the blood smear by an experienced hematologist or medical laboratory scientist is critically important and provides morphological information that automated counters cannot.
The presence of blast cells, promyelocytes, or myelocytes is a strong indicator of an underlying myeloproliferative disorder, especially CML.
Other Cell Abnormalities:
- Eosinophilia: Often accompanies basophilia (high basophils), especially in MPNs or parasitic infections.
- Dysplastic features in other lineages: Abnormal neutrophils, red blood cells (e.g., teardrop cells in myelofibrosis), or platelets (e.g., giant platelets).
- Presence of nucleated red blood cells (NRBCs): Can be seen in severe stress hematopoiesis or MPNs.
Targeted Investigations (Based on Clinical Suspicion)
Bone Marrow Examination (Aspiration and Biopsy)
This is generally performed if a myeloproliferative neoplasm (MPN) is suspected, particularly in cases of persistent basophilia (high basophils) combined with other cytopenias or cytoses, or if immature cells are seen on the peripheral smear.
Chromosomal analysis can be performed on bone marrow aspirate to look for specific chromosomal abnormalities, most notably the Philadelphia chromosome (t(9;22)) for CML.
Immunohistochemistry stains can be used on the biopsy to quantify mast cells (e.g., tryptase stain if mastocytosis is considered) or assess other cellular markers.
Molecular Genetic Testing
Essential for diagnosing MPNs.
- BCR-ABL1 fusion gene: This is the hallmark of CML and is typically tested via PCR (polymerase chain reaction) on blood or bone marrow. Its presence confirms CML.
- JAK2 V617F mutation: Common in PV, ET, and PMF.
- CALR and MPL mutations: Tested in cases of suspected ET or PMF, especially if JAK2 V617F is negative.
- Other gene mutations (e.g., CSF3R, SRSF2, ASXL1) may be tested depending on the specific MPN subtype suspected.
Allergy Testing
If allergic reactions are suspected as the cause, particularly if other MPN markers are negative.
- Total Serum IgE: Elevated levels suggest an allergic or atopic predisposition.
- Specific IgE (RAST testing): Measures IgE antibodies to specific allergens.
- Skin Prick Tests: Used to identify specific environmental or food allergens.
- Basophil Activation Test (BAT): A functional test that measures the activation of basophils in response to specific allergens.
Thyroid Function Tests (TFTs)
If hypothyroidism is suspected based on clinical symptoms, TFTs can assess thyroid gland function.
Inflammatory Markers
Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP): Non-specific markers of inflammation that can be elevated in chronic inflammatory conditions (e.g., IBD, RA). While not diagnostic of basophilia’s cause, they support the presence of a chronic inflammatory process.
Parasitology/Infectious Disease Testing
If parasitic infection is suspected (e.g., travel history, eosinophilia), stool ova and parasite exam or serological tests for specific parasites may be indicated.
Treatment and Management of Basophilia (High Basophils)
The treatment and management of basophilia (high basophils) are almost entirely directed at addressing the underlying cause with specific therapies like TKIs for CML, antihistamines for allergies, or hormone replacement for hypothyroidism.
Basophilia (high basophils) itself is rarely symptomatic or harmful enough to require direct treatment unless it’s exceptionally severe (which is extremely rare) or contributes significantly to an underlying condition’s symptoms (e.g., pruritus in MPNs due to histamine release).
If, after a thorough investigation, no underlying cause is identified and the basophilia (high basophils) is mild and asymptomatic, a “watch and wait” approach with regular monitoring of CBC may be adopted. Intervention is usually not necessary unless symptoms or other blood count abnormalities develop.
Frequently Asked Questions (FAQs)
Can high basophils make you tired?
No, high basophils themselves don’t directly “make you tired.” Fatigue is a symptom of the underlying condition that is causing the basophilia, not a direct result of the elevated basophil count itself.
Can COVID increase basophils?
During the acute phase of COVID-19 infection, especially in severe cases, basopenia (low basophils) is more commonly observed than basophilia, and this decrease can even serve as a prognostic indicator for worse outcomes. However, as patients recover from COVID-19, basophil counts tend to rebound and may even temporarily increase, sometimes leading to basophilia, as the immune system reconstitutes and develops adaptive responses to the virus. While basophils play an active role in the immune response to SARS-CoV-2 by influencing cytokine production and antibody responses, in some severe instances, their activation could potentially contribute to the hyperinflammatory “cytokine storm” seen in critical COVID-19.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Goldberg S, Hoffman J. Clinical Hematology Made Ridiculously Simple, 1st Edition: An Incredibly Easy Way to Learn for Medical, Nursing, PA Students, and General Practitioners (MedMaster Medical Books). 2021.
- Keohane EM, Otto CN, Walenga JM. Rodak’s Hematology 6th Edition (Saunders). 2019.
- Sticco, K. L., Pandya, N. K., Zubair, M., & Lynch, D. T. (2024). Basophilia. In StatPearls. StatPearls Publishing.
- Feriel, J., Depasse, F., & Geneviève, F. (2020). How I investigate basophilia in daily practice. International journal of laboratory hematology, 42(3), 237–245. https://doi.org/10.1111/ijlh.13146
- Dingli, S., Fathima, S., Faldu, P. et al. Basophilia and eosinophilia in primary myelofibrosis: phenotype, genotype, and prognostic correlates. Blood Cancer J. 15, 72 (2025). https://doi.org/10.1038/s41408-025-01285-x



