TL;DR
Monocytes are a type of white blood cell that play a crucial role in the immune system. Here are the key points:
- Function ▾: Monocytes are responsible for phagocytosis (engulfing and destroying foreign particles), antigen presentation, and inflammation.
- Morphology ▾: They are large, irregular-shaped cells with a large, indented nucleus and abundant cytoplasm.
- Lifespan ▾: Monocytes have a short lifespan in the bloodstream, typically 1-3 days, before migrating into tissues.
- Differentiation ▾: Monocytes can differentiate into macrophages and dendritic cells, which have specialized functions in the immune system.
- Monocytosis (High Monocytes) ▾: An elevated monocyte count (monocytosis) can be associated with various conditions, including infections, inflammatory diseases, and malignancies.
- Monocytopenia (Low Monocytes) ▾: A decreased monocyte count (monocytopenia) can be caused by factors such as infections, bone marrow disorders, and autoimmune diseases.
- Laboratory tests ▾: Laboratory tests, such as complete blood count (CBC) and flow cytometry, can be used to assess monocyte count and function.
- Therapeutic implications ▾: Targeting monocytes has potential therapeutic implications in various diseases, including inflammatory disorders, cancer, and infectious diseases.
*Click ▾ for more information
Introduction
Monocytes are versatile immune cells that play a vital role in protecting the body from various threats. Their ability to perform phagocytosis, antigen presentation, and inflammatory responses contributes significantly to the overall immune defense.
A Brief Overview of the Immune System
The immune system is a complex network of organs, cells, and proteins that defends the body against infection, disease, and foreign substances. It acts as the body’s defense mechanism, identifying and neutralizing threats before they can cause harm.
Importance of White Blood Cells in Immune Defense
White blood cells, or leukocytes, are crucial components of the immune system. They are responsible for identifying and attacking pathogens like bacteria, viruses, fungi, and parasites. There are several types of white blood cells, each with its specific role in immune defense.
- Neutrophils: These are the most common type of white blood cell and are the first responders to infections. They engulf and destroy bacteria and other harmful microorganisms.
- Lymphocytes: These include B cells and T cells. B cells produce antibodies to neutralize pathogens, while T cells directly attack infected cells.
- Monocytes: These are large white blood cells that circulate in the bloodstream. They differentiate into macrophages and dendritic cells, which play key roles in both innate and adaptive immunity.
- Eosinophils and basophils: These cells are involved in allergic reactions and parasitic infections.
Role of Monocytes in the Immune Response
Monocytes are essential for both innate and adaptive immunity. They have a crucial role in:
- Phagocytosis: Monocytes can engulf and destroy foreign particles, bacteria, and dead cells.
- Antigen presentation: Monocytes can process and present antigens to T cells, initiating an adaptive immune response.
- Inflammation: Monocytes release inflammatory mediators, such as cytokines and chemokines, that help recruit other immune cells to the site of infection or injury.
- Tissue repair: After an immune response, monocytes can differentiate into macrophages, which help repair damaged tissues.
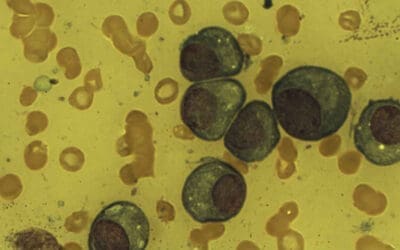
Monocyte Morphology
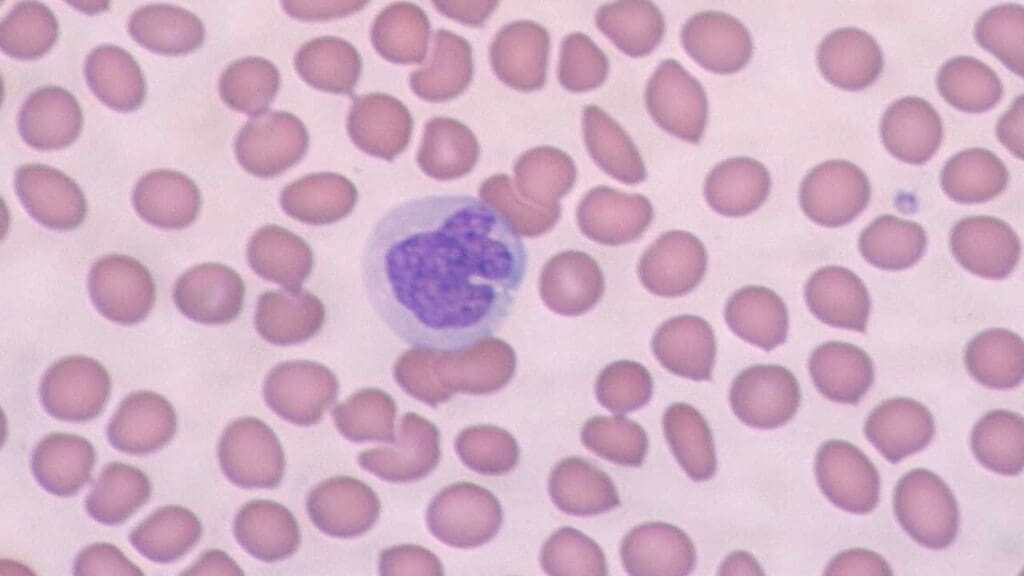
Monocytes are larger than other white blood cells and have a distinctive appearance.
Physical Characteristics
- Size: Monocytes are the largest white blood cells, typically measuring 15-20 micrometers in diameter.
- Shape: They are irregular in shape, often appearing as kidney-shaped or horseshoe-shaped.
- Nucleus: The nucleus of a monocyte is large, indented, and often folded. It occupies a significant portion of the cell.
- Cytoplasm: The cytoplasm is abundant and contains numerous fine granules. It may also contain vacuoles or vesicles.
Differentiation from Other White Blood Cells
Monocytes can be distinguished from other white blood cells based on their size, shape, and nuclear characteristics.
- Neutrophils: Smaller than monocytes with a multilobed nucleus and a cytoplasm filled with granules.
- Lymphocytes: Smaller than monocytes with a large, round nucleus that occupies most of the cell and little cytoplasm.
- Eosinophils: Similar in size to neutrophils but with a bilobed nucleus and a cytoplasm filled with large, reddish-orange granules.
- Basophils: Similar in size to neutrophils but with a bilobed nucleus and a cytoplasm filled with large, dark blue granules.
Lifespan in Blood and Reference Range
Monocytes have a relatively short lifespan in the bloodstream. They typically circulate for a few days, around 2-3 days, before migrating into tissues. Once they enter tissues, they differentiate into macrophages, which have a longer lifespan.
Reference Range
The normal reference range for monocyte count in blood can vary slightly depending on the laboratory and the specific population being tested. However, a typical reference range is approximately:
Adults: 2-10% of total white blood cell count or 200-800 cells/μL
Children: The range may be slightly higher in children, especially infants.
It’s important to note that these are general guidelines, and individual variations may occur. Factors such as age, sex, and overall health can influence monocyte counts. Deviations from the normal reference range may indicate underlying health conditions.
Function of Monocytes
Monocytes play a crucial role in the immune system as professional phagocytes and antigen-presenting cells. Their primary function is to:
- Phagocytosis: Engulf and destroy foreign particles, bacteria, and dead cells.
- Antigen presentation: Process and present antigens to T cells, initiating an adaptive immune response.
How Monocytes Carry Out These Functions
- Chemotaxis: Monocytes are attracted to sites of infection or inflammation by chemical signals called chemokines.
- Phagocytosis: Once at the site, monocytes use their pseudopodia (cellular extensions) to engulf and internalize foreign particles or pathogens. The engulfed material is then enclosed in a membrane-bound vesicle called a phagosome.
- Intracellular killing: The phagosome fuses with lysosomes, which contain digestive enzymes. These enzymes break down the engulfed material, destroying the pathogen.
- Antigen presentation: Monocytes can also process and present antigens from the engulfed material on their cell surface using molecules called MHC class II. This allows them to activate T cells, which are essential for adaptive immunity.
Monocyte Differentiation into Macrophages and Dendritic Cells
Monocytes can differentiate into two important cell types: macrophages and dendritic cells.
- Macrophages: These are large, long-lived cells that are specialized for phagocytosis and antigen presentation. They play a crucial role in tissue repair and wound healing.
- Dendritic cells: These are highly specialized antigen-presenting cells that are found in various tissues, including the skin, mucosa, and lymphoid organs. They are particularly efficient at capturing and presenting antigens to T cells, initiating a strong immune response.
Functions of Macrophages and Dendritic Cells
Macrophages
- Phagocytosis of foreign particles and debris
- Antigen presentation to T cells
- Tissue repair and remodeling
- Production of inflammatory mediators
Dendritic Cells
- Capture and processing of antigens
- Migration to lymphoid organs
- Presentation of antigens to T cells
- Initiation of adaptive immune responses
Monopoiesis
Monopoiesis, like the production of other blood cells, occurs in the bone marrow. This process involves a series of steps, starting from a hematopoietic stem cell and culminating in the formation of mature monocytes.
Key Stages and Factors Involved
- Hematopoietic Stem Cell (HSC): The process begins with a hematopoietic stem cell, which is a multipotent cell capable of giving rise to all types of blood cells.
- Common Myeloid Progenitor (CMP): The HSC differentiates into a common myeloid progenitor, a cell that can produce various myeloid cell lineages, including monocytes.
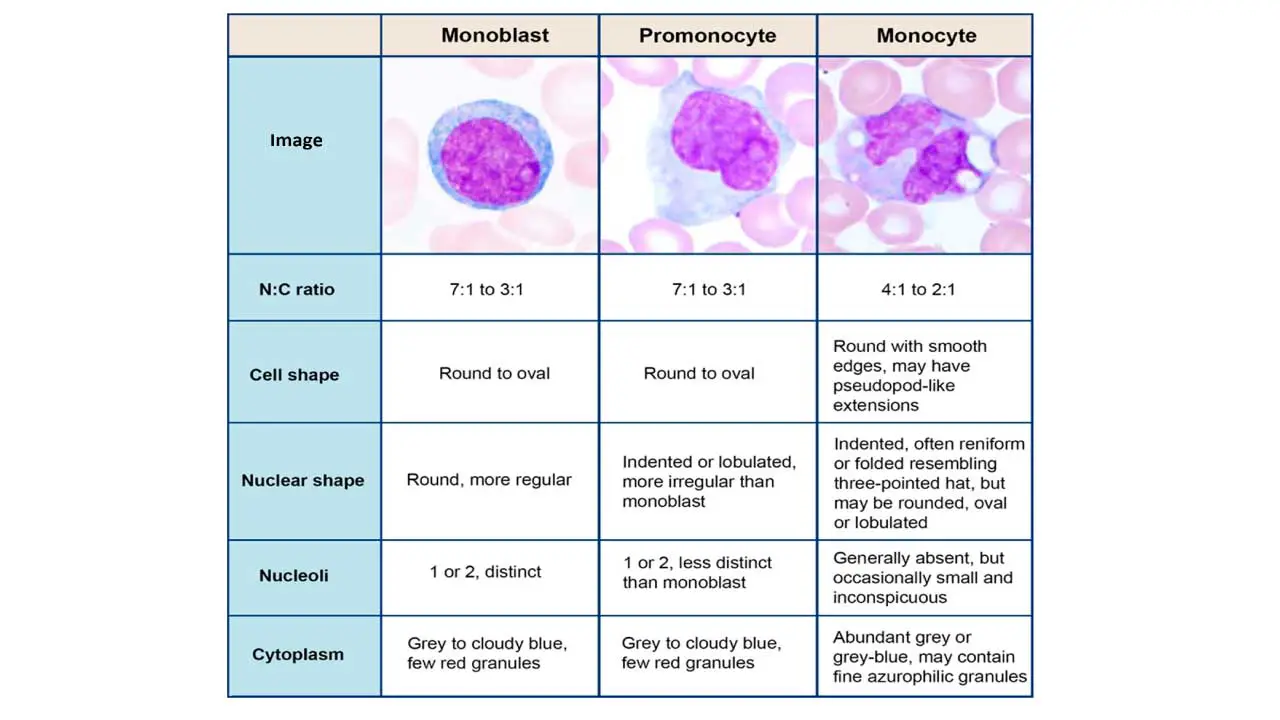
- Monoblast: The CMP further differentiates into a monoblast, a committed precursor cell for monocytes.
- Promonocyte: The monoblast undergoes maturation to become a promonocyte.
- Monocyte: The promonocyte eventually develops into a mature monocyte, which is released into the bloodstream.
Several factors influence monopoiesis, including:
- Cytokines: These signaling molecules regulate cell growth, differentiation, and survival. Cytokines such as granulocyte-macrophage colony-stimulating factor (GM-CSF) and macrophage colony-stimulating factor (M-CSF) play important roles in monocyte development.
- Growth factors: Growth factors also influence monopoiesis, including stem cell factor and interleukin-3.
- Transcription factors: These proteins control gene expression and are essential for cell differentiation. Transcription factors such as PU.1 and C/EBPα are involved in monocyte development.
- Microenvironment: The bone marrow microenvironment, including the extracellular matrix and interactions with other cells, also plays a role in monopoiesis.
Causes of High Monocytes (Monocytosis)
Monocytosis, or a high monocyte count, can be a sign of various underlying conditions. Here are some common causes and the mechanisms involved:
Infectious Diseases
- Bacterial infections: Monocytes are essential for combating bacterial infections. Conditions like tuberculosis, typhoid fever, and endocarditis can lead to high monocyte production.
- Viral infections: Certain viral infections, such as infectious mononucleosis, HIV, and hepatitis, can stimulate the immune system, resulting in monocytosis (high monocyte count).
- Parasitic infections: Monocytes play a role in defense against parasitic infections. Conditions like malaria, visceral leishmaniasis, and toxoplasmosis can be associated with high monocyte counts.
Inflammatory Conditions
- Chronic inflammation: Chronic inflammatory diseases like rheumatoid arthritis, systemic lupus erythematosus, and inflammatory bowel disease can cause monocytosis (high monocyte count).
- Autoimmune disorders: These conditions involve the immune system attacking the body’s own tissues. Monocytes are involved in inflammatory processes and can be elevated in autoimmune diseases.
Malignancies
- Leukemias: Certain types of leukemia, such as chronic myeloid leukemia and chronic lymphocytic leukemia, can involve abnormal monocyte production.
- Lymphomas: Lymphomas, cancers of the lymphatic system, can also be associated with monocytosis (high monocyte count).
Other Conditions
- Stress: Psychological stress can trigger the release of hormones that stimulate the immune system, leading to high monocyte production.
- Tissue damage: Injury or tissue necrosis can cause inflammation and increase the need for monocytes to clear debris and promote healing.
- Certain medications: Some medications, such as corticosteroids and interferon, can affect monocyte production.
Underlying Mechanisms
The mechanisms leading to monocytosis (high monocyte count) can vary depending on the underlying condition. However, some common mechanisms include:
- Increased production: The bone marrow may produce more monocytes in response to infections, inflammation, or other stimuli.
- Decreased destruction: Monocytes may be destroyed at a slower rate, leading to an accumulation in the bloodstream.
- Release from tissues: Monocytes stored in tissues may be released into the bloodstream, contributing to an elevated count.
- Abnormal differentiation: In some cases, abnormal differentiation of monocytes or their precursors can lead to an increased number of circulating monocytes.
It is important to note that monocytosis (high monocyte count) is often a secondary finding and may not be the primary cause of a patient’s symptoms.
Causes of Low Monocytes (Monocytopenia)
Monocytopenia, or a decreased monocyte count, can be caused by various factors. Here are some potential causes:
Infections
- Overwhelming infections: Severe infections, especially those caused by bacteria or fungi, can lead to a depletion of monocytes as they are used to fight the infection.
- Viral infections: Certain viral infections, such as HIV and measles, can impair monocyte production or survival.
Bone Marrow Disorders
- Aplastic anemia: This is a condition characterized by the failure of bone marrow to produce blood cells, including monocytes.
- Myelodysplastic syndromes: These are a group of disorders that affect bone marrow function and can lead to decreased production of various blood cells, including monocytes.
- Leukemia: Some types of leukemia, such as acute myelogenous leukemia, can involve the replacement of normal bone marrow cells by cancerous cells, leading to a decrease in monocyte production.
Autoimmune Diseases
- Autoimmune cytopenias: These are conditions where the immune system attacks and destroys blood cells. Autoimmune monocytopenia can occur in some cases.
Medications
- Chemotherapy: Medications used to treat cancer can suppress bone marrow function, leading to decreased monocyte production.
- Corticosteroids: Long-term use of corticosteroids can suppress the immune system, including monocyte production.
- Antiviral medications: Some antiviral drugs can have side effects that affect monocyte count.
Other Factors
- Splenomegaly: An enlarged spleen can remove monocytes from the bloodstream at a faster rate than normal.
- Genetic disorders: Certain inherited disorders can affect monocyte production or function.
Clinical Implications of Monocytopenia
Monocytopenia can increase the risk of infections, as monocytes are crucial for fighting pathogens. Patients with monocytopenia may be more susceptible to:
- Bacterial infections: Monocytes play a key role in combating bacterial infections.
- Fungal infections: Monocytes are also important for defending against fungal infections.
- Viral infections: Although some viral infections can cause monocytopenia, patients with this condition may be more susceptible to opportunistic infections.
In addition to infections, monocytopenia can have other clinical implications:
- Delayed wound healing: Monocytes are involved in tissue repair, and a decreased monocyte count can impair wound healing.
- Increased risk of bleeding: Monocytes can differentiate into macrophages, which help regulate blood clotting. A decrease in monocytes may contribute to a higher risk of bleeding.
- Fatigue and weakness: Monocytopenia can be a sign of an underlying bone marrow disorder or other systemic illness, which can lead to fatigue and weakness.
It is important to note that the clinical implications of monocytopenia can vary depending on the underlying cause and the severity of the monocytopenia.
Laboratory Investigations
Several laboratory tests can be used to assess monocyte count and function:
Complete Blood Count (CBC)
- Monocyte count: A CBC provides the absolute number of monocytes in the blood.
- Monocyte percentage: It also shows the percentage of monocytes relative to total white blood cells.
Flow Cytometry
- Monocyte subsets: Flow cytometry can be used to identify different subsets of monocytes based on their expression of surface markers. This can help in diagnosing certain diseases.
Immunohistochemistry
- Tissue macrophages: Immunohistochemistry can be used to detect and quantify macrophages in tissue samples. This is helpful in studying inflammatory processes and diseases.
Phagocytosis Assay
- Functional assessment: This test measures the ability of monocytes to engulf and destroy foreign particles. It can be used to assess monocyte function in certain conditions.
Cytokine Measurement
- Inflammatory markers: Measuring the levels of cytokines produced by monocytes can provide insights into their activation and role in inflammation.
Other Tests
- Bone marrow biopsy: In some cases, a bone marrow biopsy may be performed to evaluate monocyte production and the presence of abnormal cells.
Significance of Monocyte-Related Laboratory Findings
Monocyte-related laboratory findings can be significant for various reasons:
- Diagnosis: An elevated monocyte count (monocytosis) or a decreased monocyte count (monocytopenia) can be a clue to underlying diseases.
- Monitoring disease progression: Monitoring changes in monocyte count and function can help track the progression of certain diseases, such as infections or inflammatory conditions.
- Assessing treatment response: Evaluating the response of monocyte count and function to treatment can help determine the effectiveness of therapy.
- Identifying risk factors: Abnormal monocyte findings may identify individuals at increased risk for certain diseases or complications.
Therapeutic Implications of Targeting Monocytes
Monocytes play a crucial role in various diseases, making them a potential target for therapeutic interventions. Here are some therapeutic implications of targeting monocytes.
Inflammatory Diseases
- Rheumatoid arthritis: Targeting monocytes can help reduce inflammation and joint damage in rheumatoid arthritis.
- Atherosclerosis: Monocytes contribute to atherosclerotic plaque formation. Targeting them could potentially prevent or slow the progression of atherosclerosis.
- Multiple sclerosis: Monocytes play a role in the inflammatory processes underlying multiple sclerosis. Targeting them may be beneficial in managing this condition.
Cancer
- Tumor-associated macrophages: Monocytes can differentiate into tumor-associated macrophages, which promote tumor growth and metastasis. Targeting these cells could potentially inhibit tumor progression.
- Cancer immunotherapy: Monocytes can be used as a platform for cancer immunotherapy, by engineering them to deliver therapeutic agents or stimulate anti-tumor immune responses.
Infectious Diseases
- Tuberculosis: Monocytes are involved in the pathogenesis of tuberculosis. Targeting them could potentially be beneficial in treating this disease.
- HIV: Monocytes can be infected by HIV, and targeting them may be a potential strategy for reducing viral load and preventing disease progression.
Other Diseases
- Autoimmune diseases: Monocytes are involved in autoimmune diseases, and targeting them could potentially reduce inflammation and disease symptoms.
- Bone diseases: Monocytes play a role in bone metabolism. Targeting them may be beneficial in treating certain bone diseases.
Therapeutic Approaches
- Monoclonal antibodies: Targeting specific surface markers on monocytes with monoclonal antibodies can be used to deplete or modulate their function.
- Small molecules: Small molecules that inhibit monocyte activation or function can be developed as potential therapeutic agents.
- Cell-based therapies: Monocytes can be engineered to deliver therapeutic agents or stimulate anti-tumor immune responses.
It is important to note that targeting monocytes is a complex area of research, and more studies are needed to fully understand the potential benefits and risks of these approaches. However, the role of monocytes in various diseases suggests that targeting them could be a promising therapeutic strategy in the future.
Frequently Asked Questions (FAQs)
Which cancer in particular has high monocytes?
Chronic myelomonocytic leukemia (CMML) is a type of myeloproliferative disorder characterized by the overproduction of monocytes. This excessive production often leads to monocytosis, meaning a higher-than-normal number of monocytes in the blood.
CMML is often associated with other blood cell abnormalities, such as anemia or neutrophilia. It can also progress to acute myeloid leukemia (AML) in some cases.
What are the symptoms of high monocytes?
Monocytosis itself typically does not cause symptoms. It’s often a secondary finding on a blood test, meaning it’s discovered as part of a larger medical evaluation.
The symptoms individuals experience are usually related to the underlying condition causing the monocytosis. For example, if there is an infection, the infection itself may cause symptoms like fever, fatigue, and joint pain, while the monocytosis is simply a sign of the body’s immune response.
What medications cause high monocytes?
Certain medications can contribute to increased monocyte counts (monocytosis). However, it’s important to note that monocytosis is often a secondary effect and can be caused by various underlying factors, such as infections, inflammatory conditions, and cancers.
Here are some medications that may be associated with monocytosis:
- Corticosteroids: Long-term use of corticosteroids, such as prednisone, can suppress the immune system, which can lead to increased monocyte production.
- Interferon: Interferon, a protein produced by cells in response to viral infection, can also stimulate the immune system and increase monocyte levels.
- Anti-TNF agents: These medications are used to treat inflammatory conditions like rheumatoid arthritis and Crohn’s disease. They can sometimes affect monocyte levels.
- Certain antiretrovirals: Some medications used to treat HIV can increase monocyte counts.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Gordon S, Taylor PR. Monocyte and macrophage heterogeneity. Nat Rev Immunol. 2005 Dec;5(12):953-64. doi: 10.1038/nri1733. PMID: 16322748.
- Guilliams M, Mildner A, Yona S. Developmental and Functional Heterogeneity of Monocytes. Immunity. 2018 Oct 16;49(4):595-613. doi: 10.1016/j.immuni.2018.10.005. PMID: 30332628.
- Woollard KJ, Geissmann F. Monocytes in atherosclerosis: subsets and functions. Nat Rev Cardiol. 2010 Feb;7(2):77-86. doi: 10.1038/nrcardio.2009.228. Epub 2010 Jan 12. PMID: 20065951; PMCID: PMC2813241.
- Ma WT, Gao F, Gu K, Chen DK. The Role of Monocytes and Macrophages in Autoimmune Diseases: A Comprehensive Review. Front Immunol. 2019 May 24;10:1140. doi: 10.3389/fimmu.2019.01140. PMID: 31178867; PMCID: PMC6543461.
- Álvarez K, Rojas M. Nanoparticles targeting monocytes and macrophages as diagnostic and therapeutic tools for autoimmune diseases. Heliyon. 2023 Sep 7;9(9):e19861. doi: 10.1016/j.heliyon.2023.e19861. PMID: 37810138; PMCID: PMC10559248.
- Lee SY, Fierro J Jr, Dipasquale J, Bastian A, Tran AM, Hong D, Chin B, Nguyen-Lee PJ, Mazal S, Espinal J, Thomas T, Dou H. Engineering Human Circulating Monocytes/Macrophages by Systemic Deliverable Gene Editing. Front Immunol. 2022 May 18;13:754557. doi: 10.3389/fimmu.2022.754557. PMID: 35663976; PMCID: PMC9159279.