TL;DR
Non-Hodgkin Lymphoma (NHL) or previously known as Non-Hodgkin’s Lymphoma is a cancer of the lymphatic system, which is part of the immune system. It arises from lymphocytes that become abnormal and grow uncontrollably causing Non-Hodgkin Lymphoma (Non-Hodgkin’s Lymphoma) symptoms like lymphadenopathy, fatigue and unexplained weight loss.
- Classification ▾: Non-Hodgkin lymphoma is classified into subtypes based on the type of lymphocyte involved (B-cell or T-cell) and their growth rate (low-grade or high-grade).
- Common Non-Hodgkin’s Lymphoma Symptoms ▾:
- Enlarged lymph nodes (most common)
- Fatigue
- Night sweats
- Weight loss
- Fever
- Pain or discomfort near enlarged lymph nodes
- Other symptoms depending on involved organs
- Diagnosis ▾:
- Blood tests
- Imaging studies (X-ray, CT scan, PET scan)
- Lymph node biopsy (tissue examination)
- Treatment ▾: There is no single specific treatment for non-Hodgkin lymphoma. Treatment options depend on the specific subtype, stage, and patient factors.
*Click ▾ for more information
Introduction
Lymphomas, particularly Non-Hodgkin Lymphoma (NHL), are one of the most common types of cancers. They represent a considerable portion of diagnosed cancers, making them a major focus area in oncology research and treatment.
Non-Hodgkin Lymphoma (NHL) is a type of cancer that originates in the lymphatic system, which is part of the body’s immune system. The lymphatic system has a network of vessels and glands throughout the body that helps fight infection.
Non-Hodgkin Lymphoma arises from lymphocytes, which are white blood cells that are normally involved in fighting infection. In non-Hodgkin lymphoma, these lymphocytes develop abnormalities and multiply uncontrollably.
These abnormal lymphocytes can accumulate in lymph nodes, causing them to enlarge (lymphadenopathy). They can also spread to other organs.
This disorder encompasses a diverse range of subtypes, each with distinct characteristics, prognoses, and treatment approaches.
Lymphomas
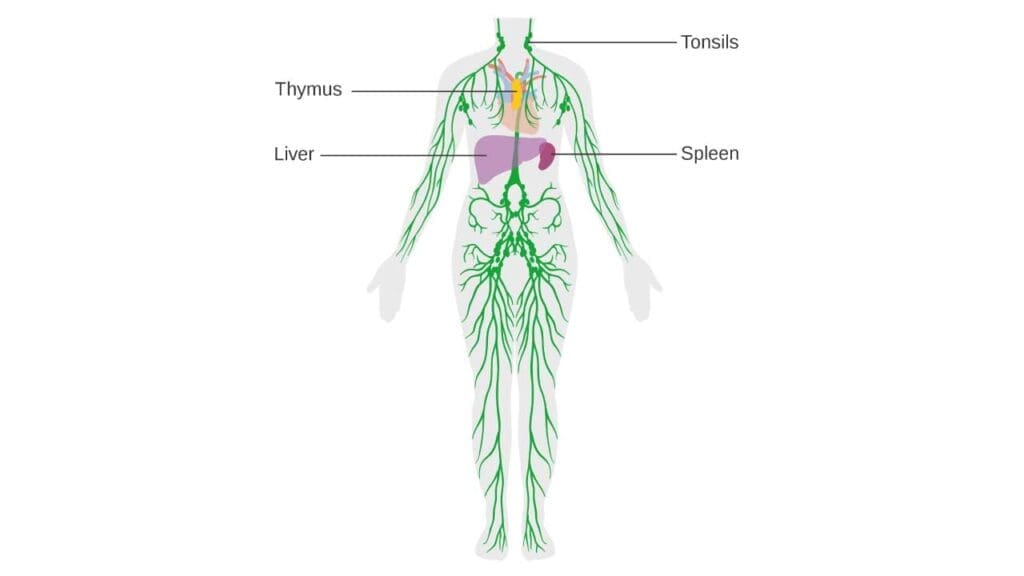
Lymphoma is a general term for a group of cancers that develop in the lymphatic system. The lymphatic system is a network of tissues and organs that help the body fight infection.
The lymphatic system is comprised of both primary and secondary lymphoid organs.
Primary Lymphoid Organs: These are the sites where lymphocytes are produced and mature.
- Bone Marrow: This is where all blood cells, including lymphocytes, are initially produced. B lymphocytes (B cells) mature in the bone marrow.
- Thymus: This gland is where T lymphocytes (T cells) mature after being produced in the bone marrow.
Secondary Lymphoid Organs: These organs are where mature lymphocytes encounter antigens and initiate immune responses.
- Lymph Nodes: These are small, bean-shaped clusters of white blood cells found throughout the lymphatic system, such as in the neck, armpits, and groin. They filter lymph and are sites where immune responses are mounted.
- Spleen: This organ filters blood, removes old or damaged blood cells, and plays a role in immune responses by housing lymphocytes and other immune cells.
- Tonsils and Adenoids: These are lymphoid tissues located in the throat and nasal cavity, respectively, that help protect against pathogens entering the body through the mouth and nose.
The lymphatic system also includes lymph channels (vessels) that transport lymph fluid throughout the body.
Types of Lymphoma
There are two main types of lymphoma: Hodgkin Lymphoma and Non-Hodgkin Lymphoma (NHL). Non-Hodgkin Lymphoma (NHL) is more common than Hodgkin Lymphoma.
Comparison between Hodgkin and Non-Hodgkin Lymphomas (NHL)
| Feature | Hodgkin Lymphoma (HL) | Non-Hodgkin Lymphoma (disease) |
| Cell Type | Reed-Sternberg cells | B-cells or T-cells (various subtypes) |
| Frequency | Less Common | More Common |
| Age of Diagnosis | Young Adults (15-40 yrs) & Older Adults (>55 yrs) | Adults over 60 (can occur any age) |
| Progression | Predictable spread pattern | Variable spread pattern |
| Treatment | Generally higher success rate | Varies depending on subtype, stage, and individual |
| Prognosis | Higher overall survival rate (around 89% at 5 years) | Lower overall survival rate (around 74% at 5 years) |
| Symptoms | Swollen lymph nodes, fever, night sweats, fatigue (may vary) | Swollen lymph nodes, fever, night sweats, fatigue (may vary depending on subtype and location) |
Epidemiology of Non-Hodgkin Lymphomas
Non-Hodgkin Lymphoma (NHL) is a significant public health concern with distinct epidemiological patterns. It is the most common hematological malignancy worldwide and is not a single disease but a group of related cancers affecting lymphocytes.
Prevalence and Incidence
Non-Hodgkin Lymphoma (NHL) is one of the most common cancers in the United States, accounting for approximately 4% of all new cancer cases.
In the US, over 80,000 new cases are projected for 2024. The American Cancer Society estimates that about 80,350 people (45,140 males and 35,210 females) will be diagnosed with Non-Hodgkin Lymphoma (NHL) in 2025. Globally, Non-Hodgkin Lymphoma (NHL) accounts for nearly 3% of cancer diagnoses and deaths.
The incidence of Non-Hodgkin Lymphoma (NHL) has increased significantly over time, with a 168% rise since 1975, though survival rates have also improved. However, incidence rates have shown a decline of about 1% per year for Non-Hodgkin Lymphoma (NHL) since 2015.
Demographic Trends
- Age: The risk of developing Non-Hodgkin Lymphoma (NHL) generally increases with age. More than half (57%) of Non-Hodgkin Lymphoma (NHL) cases are diagnosed in individuals over the age of 65. The average age of diagnosis is 67 years. Despite this, Non-Hodgkin Lymphoma (NHL) can develop at any age and is notably among the more prevalent cancers in children, teenagers, and young adults.
- Gender: Males have a slightly higher incidence rate of Non-Hodgkin Lymphoma (NHL) than women. Globally, men have over double the cumulative lifetime risk of developing Non-Hodgkin Lymphoma (NHL), being 39% more likely to be diagnosed and 60% more likely to die from the disease in high Human Development Index (HDI) nations. This disparity may be due to differences in environmental exposures and intrinsic immunological and hormonal factors.
- Race/Ethnicity: In the US, white and non-Hispanic individuals are at the highest risk of Non-Hodgkin Lymphoma (NHL). Incidence rates per 100,000 are higher in white men (25.0) and women (17.0) compared to other racial/ethnic groups. Asian/Pacific Islander, American Indian, and Black populations generally have lower risks. However, certain subtypes, like the T-cell lymphoma mycosis fungoides, show a higher incidence among African Americans. Geographic variations also exist, with East Asian nations and parts of West Africa and the Caribbean having higher rates of human T-cell lymphoma virus (HTLV-1) and subsequently higher incidence of T-cell lymphoma.
- Family History: A family history of hematological malignancy has been identified as a risk factor across various Non-Hodgkin Lymphoma (NHL) subtypes. While the likelihood of two first-degree relatives having Non-Hodgkin Lymphoma (NHL) remains very small, individuals with a family history appear to be at a slightly higher risk, often for the same subtype.
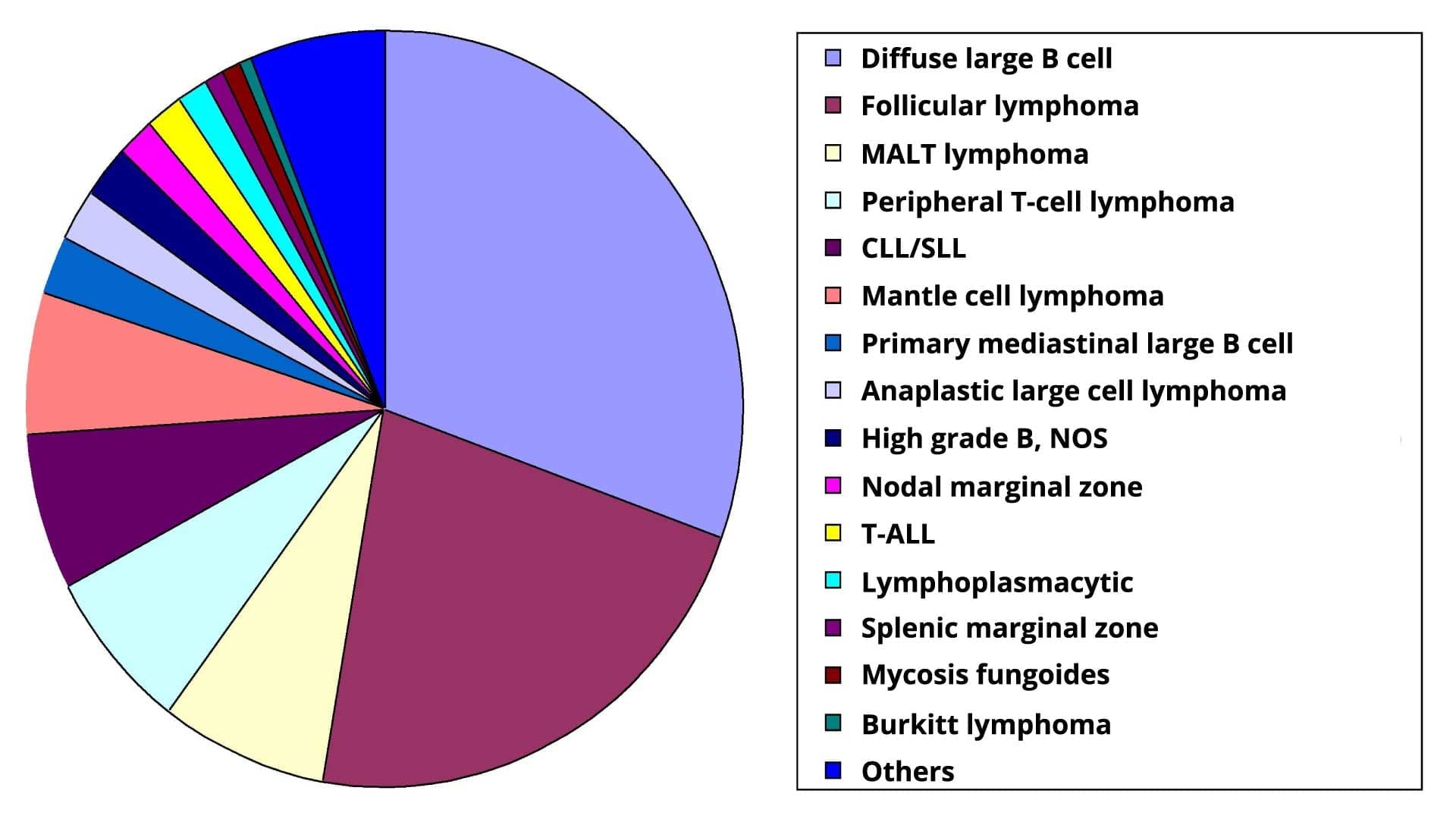
Classifications of Non-Hodgkin Lymphoma (NHL)
Non-Hodgkin Lymphoma is categorized based on two key features:
Cell of Origin
- B-cell NHL: This is the more common type, accounting for about 85-90% of all Non-Hodgkin Lymphoma (NHL) cases. B-cells are lymphocytes responsible for antibody production, a crucial part of the immune system’s defense against infections.
- T-cell NHL: Less frequent than B-cell Non-Hodgkin Lymphoma (NHL), these lymphomas develop from T-cells, which are lymphocytes directly involved in attacking infected cells and foreign invaders.
Growth Rate
- Low-grade Non-Hodgkin Lymphoma (Indolent): These lymphomas grow slowly and may not cause immediate Non-Hodgkin’s Lymphoma symptoms for years. They are often considered incurable but manageable with treatment aimed at controlling the disease and improving quality of life.
- High-grade Non-Hodgkin Lymphoma (Aggressive): These lymphomas grow rapidly and can cause noticeable non-Hodgkin lymphoma symptoms quickly. They are considered more serious and require aggressive treatment with curative intent (aiming for a complete cure).
Some subtypes don’t strictly fit into low-grade or high-grade categories. For example, mantle cell lymphoma (MCL) is a B-cell Non-Hodgkin Lymphoma (NHL) with an intermediate growth rate and aggressive behavior.
Distinguishing Lymphomas from Leukemias
While both lymphoma and leukemia are blood cancers affecting the lymphatic system and blood cells, they have distinct characteristics in origin, presentation, treatment, and other aspects.
| Feature | Lymphoma | Leukemia |
| Origin | Lymphatic System (lymph nodes, spleen, etc.) | Bone Marrow |
| Cell Type | Lymphocytes within lymphoid tissues | Abnormal white blood cells or precursors in bone marrow |
| Presentation (Symptoms) | Swollen lymph nodes, fatigue, fever, night sweats, weight loss (may vary by location) | Easy bruising/bleeding, frequent infections, bone pain, fatigue, fever, night sweats |
| Treatment | Chemotherapy, radiation therapy, surgery (localized), targeted therapies, stem cell transplant (varies by type & stage) | Chemotherapy, radiation therapy, stem cell transplant (varies by type & stage) |
| Prognosis | Varies by type and stage (some low-grade lymphomas have better prognosis than aggressive leukemias) | Varies by type and stage |
| Age | All ages (some types more common in adults/children) | All ages (some types more prevalent in children) |
| Genetic Factors | Yes (specific genes may differ from leukemia) | Yes |
| Diagnostic Tests | Blood test, lymph node biopsy | Blood test, bone marrow biopsy |
Pathogenesis of Non-Hodgkin Lymphoma (NHL)
The development of non-Hodgkin lymphoma (disease) is a complex process involving multiple factors that contribute to the uncontrolled growth of lymphocytes.
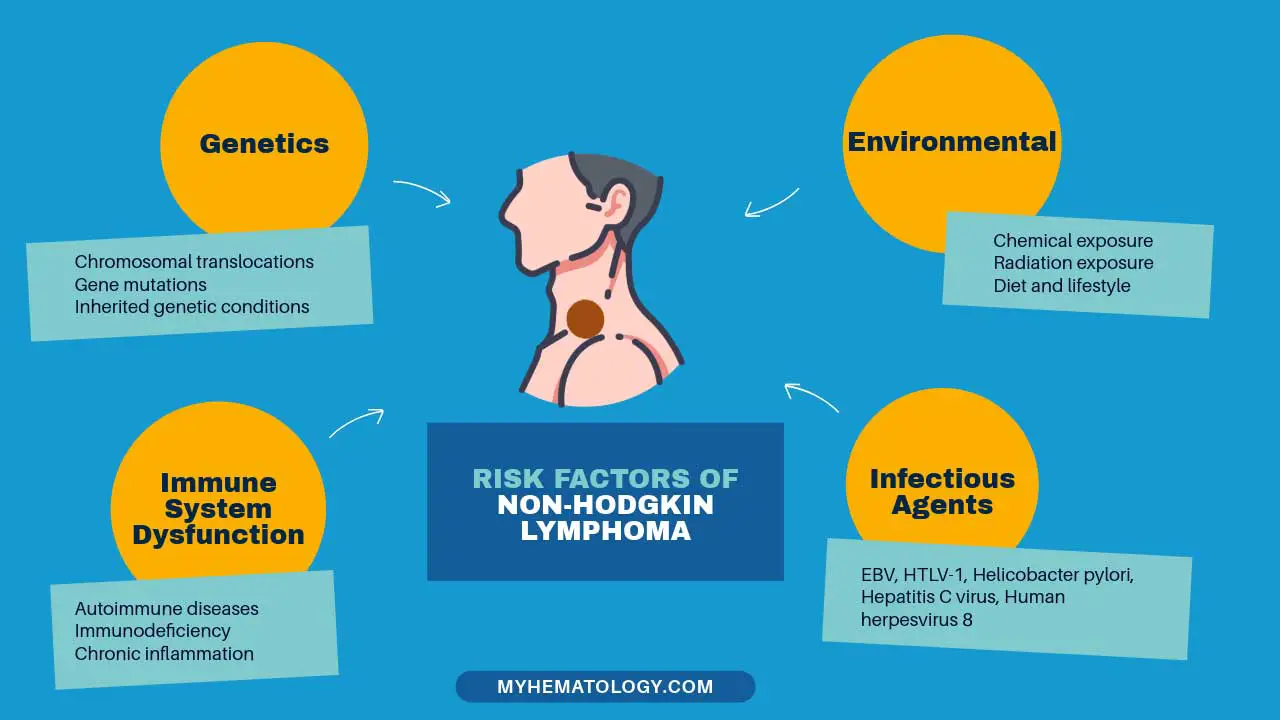
Genetic Mutations and Chromosomal Translocations
- Mutations in tumor suppressor genes: These genes normally control cell growth and division. Mutations inactivate these genes, allowing abnormal lymphocyte proliferation. Examples include mutations in p53 and PTEN genes.
- Chromosomal translocations: These rearrangements in chromosomes can activate oncogenes (genes that promote cancer) or disrupt tumor suppressor genes. Specific translocations are characteristic of some non-Hodgkin lymphoma (disease) subtypes. Examples include the t(14;18) translocation in follicular lymphoma and the t(4;11) translocation in some T-cell lymphomas.
Viral Infections
- Epstein-Barr virus (EBV): This virus is associated with Burkitt lymphoma, some cases of Hodgkin Lymphoma, and post-transplant lymphomas. EBV disrupts normal cell cycle control and can promote growth of infected lymphocytes.
- Human T-cell lymphotropic virus type 1 (HTLV-1): This virus is a major risk factor for Adult T-cell leukemia/lymphoma (ATLL). HTLV-1 integrates its genetic material into the host T-cell genome, promoting uncontrolled proliferation.
- Human herpesvirus 8 (HHV-8): This virus is linked to some cases of primary effusion lymphoma and Kaposi’s sarcoma-associated herpesvirus (KSHV)-positive multicentric Castleman disease. HHV-8 can interfere with immune regulation and cell survival pathways.
Environmental Factors
- Exposure to certain chemicals: Herbicides like glyphosate and certain industrial chemicals like benzene have been linked to an increased risk of Non-Hodgkin Lymphoma (NHL), although the exact mechanisms are not fully understood.
- Autoimmune diseases: Individuals with weakened immune systems due to autoimmune conditions like Sjogren’s syndrome may have a higher risk of developing some Non-Hodgkin Lymphoma (NHL) subtypes.
- Radiation exposure: High-dose radiation exposure, such as that experienced during atomic bomb blasts or certain medical treatments, can increase the risk of Non-Hodgkin Lymphoma (NHL).
Other Factors
- Immune dysfunction: Chronic inflammation or an impaired immune response can create an environment conducive to the development of Non-Hodgkin Lymphoma (NHL).
- Age: The risk of Non-Hodgkin Lymphoma (NHL) generally increases with age. However, certain subtypes like Burkitt lymphoma can occur in children.
- Family history: Having a close relative with Non-Hodgkin Lymphoma (NHL) may slightly increase the risk, suggesting a possible genetic predisposition in some cases.
Non-Hodgkin’s Lymphoma Symptoms
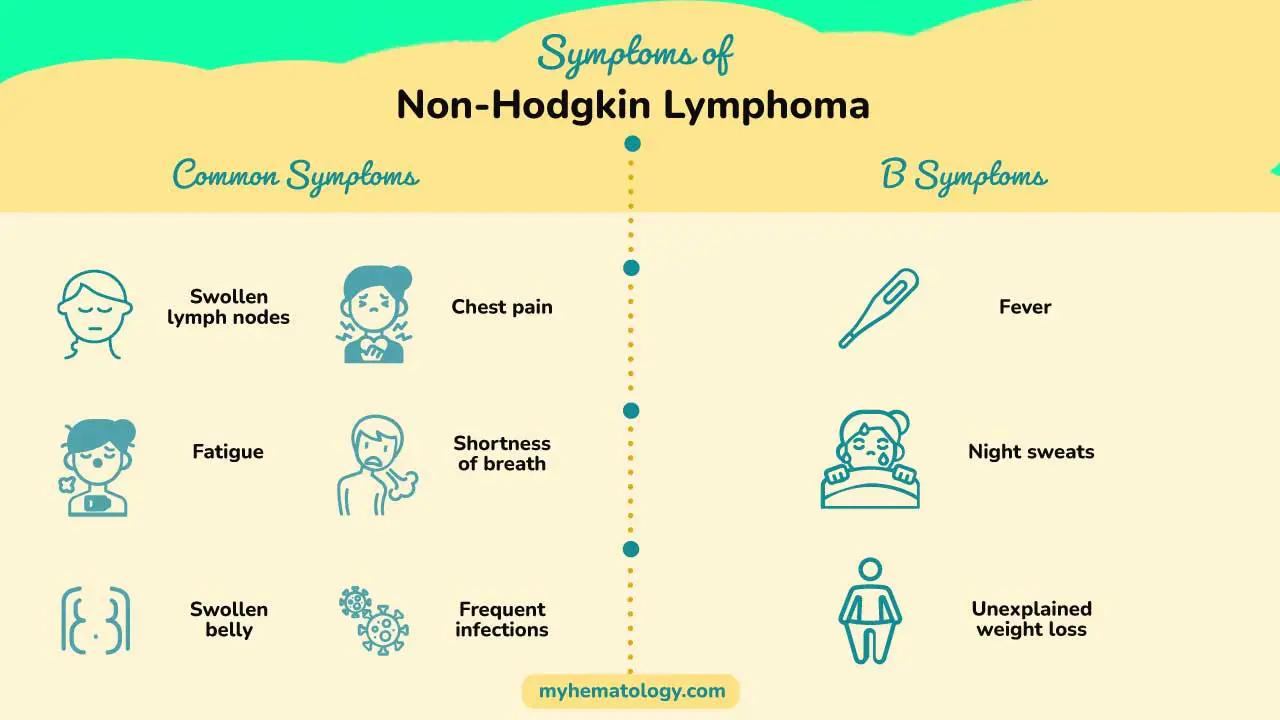
The Non-Hodgkin’s Lymphoma symptoms depend on the specific subtype, location of the involved lymph nodes, and the degree of extranodal involvement (spread beyond lymph nodes).
Common Non-Hodgkin Lymphoma Symptoms
- Lymphadenopathy: This is the most common symptom of Non-Hodgkin Lymphoma (NHL), presenting as painless, swollen lymph nodes in the neck, armpits, groin, or other locations. The size, consistency, and location of swollen lymph nodes can provide clues to the type of NHL.
- B symptoms: These constitutional symptoms, although not specific to Non-Hodgkin Lymphoma (NHL), can occur in some patients and include:
- Fever without a clear cause (often exceeding 100.4°F or 38°C for several days)
- Night sweats (drenching sweats during sleep)
- Unexplained weight loss (often exceeding 10% of body weight in 6 months)
Location-Specific Non-Hodgkin’s Lymphoma Symptoms
Enlarged lymph nodes in specific locations
- Mediastinal lymphadenopathy (chest) can cause cough, shortness of breath, or chest pain.
- Abdominal lymphadenopathy can lead to abdominal pain, nausea, or early satiety (feeling full after eating a small amount).
- Pelvic lymphadenopathy may cause leg swelling or urinary symptoms.
Extranodal Involvement
Depending on the subtype, Non-Hodgkin Lymphoma (NHL) can involve organs beyond the lymphatic system. This can cause various symptoms specific to the affected organ. For example, involvement of the spleen can lead to left upper abdominal discomfort, while bone marrow involvement may cause fatigue, anemia, or increased risk of infections.
Other Non-Hodgkin’s Lymphoma Symptoms
- Bone pain can occur in some cases, particularly with aggressive lymphomas.
- Skin rashes or itching can be associated with certain subtypes of Non-Hodgkin Lymphoma (NHL).
- Pressure on nerves by enlarged lymph nodes can lead to numbness, tingling, or weakness in specific areas.
Additional Features
The rate of symptom development can vary. Low-grade lymphomas may present with vague symptoms that progress slowly, while aggressive lymphomas can cause rapid symptom onset.
Some patients, particularly those with low-grade disease, may not experience any noticeable symptoms for an extended period.
Laboratory Investigations for Non-Hodgkin Lymphoma (NHL)

Diagnosing Non-Hodgkin Lymphoma (NHL) involves a multi-pronged approach, and laboratory investigations play a vital role in this process.
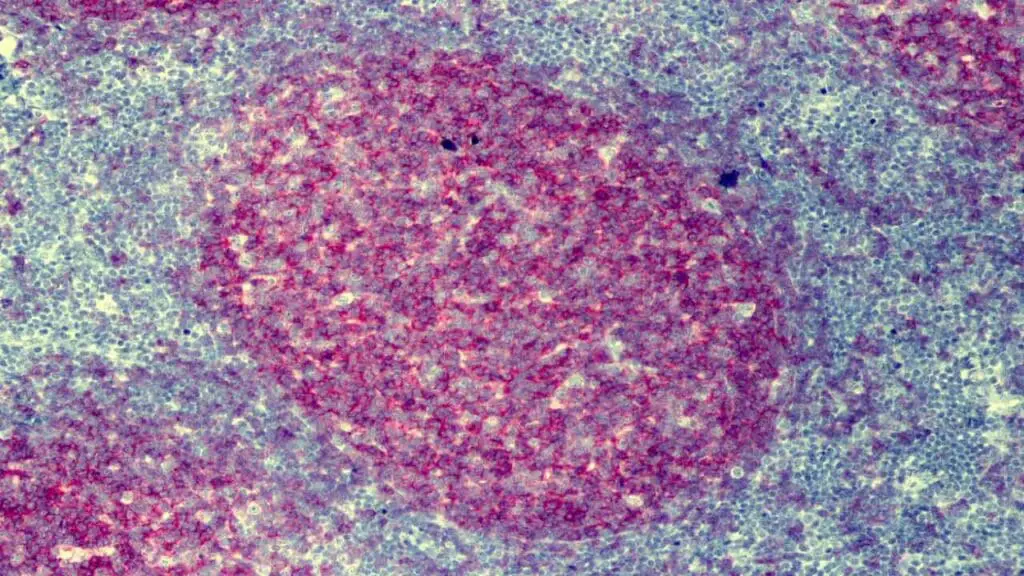
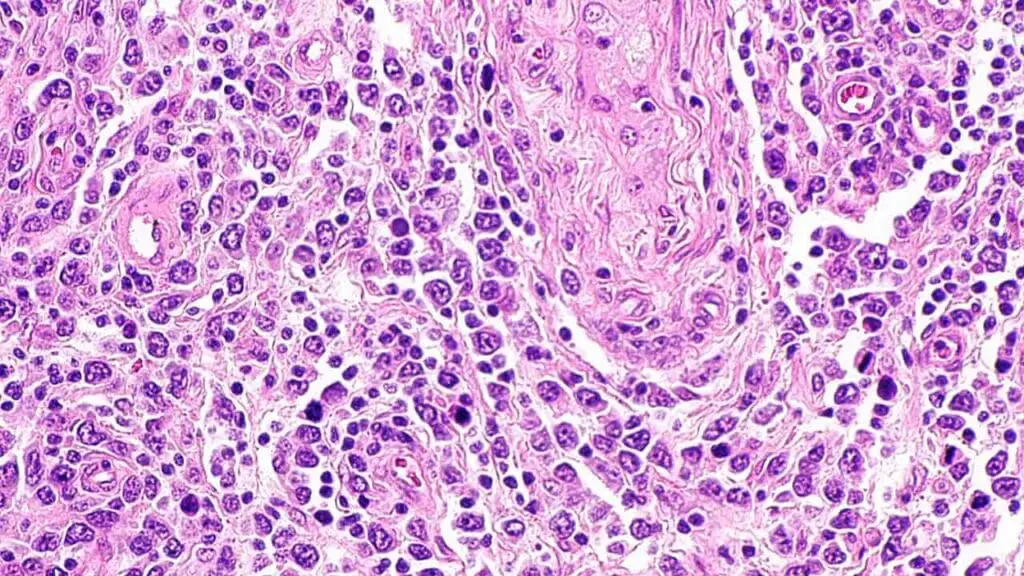
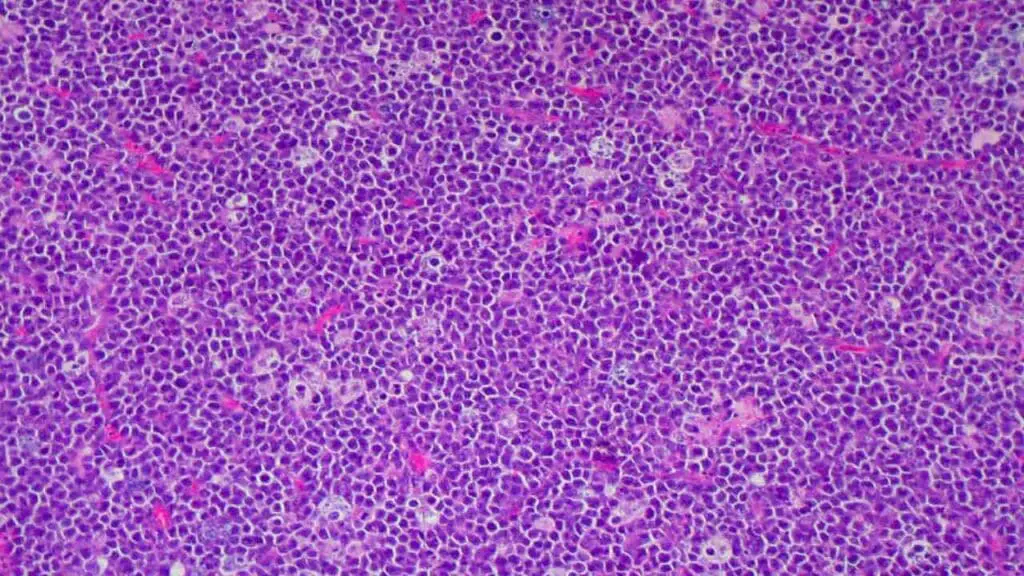
Histology
Lymph node biopsy is the cornerstone of Non-Hodgkin Lymphoma (NHL) diagnosis. A tissue sample from an enlarged lymph node is extracted using a needle or surgical procedure.
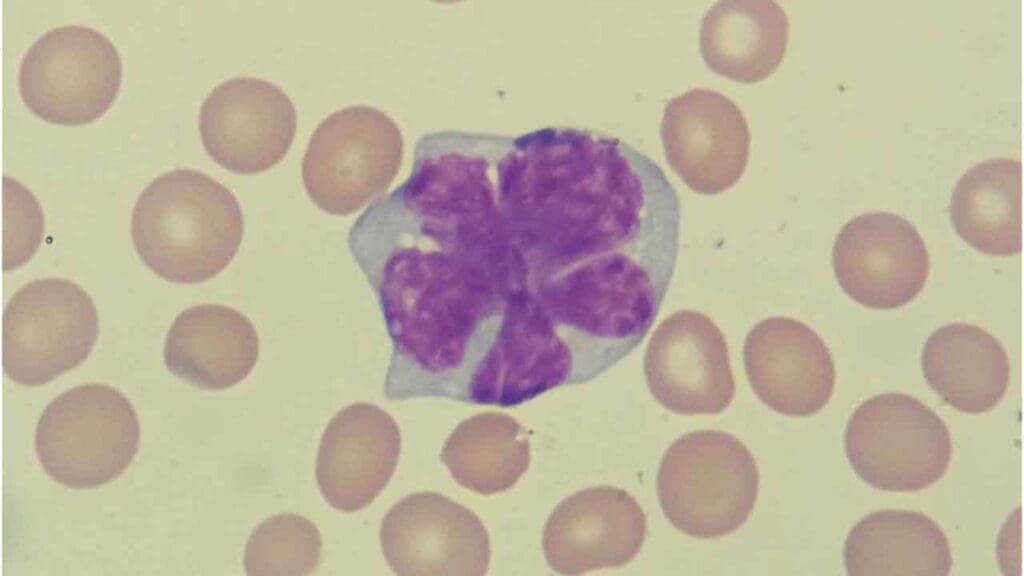
Then a pathologist analyzes the tissue sample under a microscope to identify the specific type of lymphoma cell and its characteristics. This is crucial for accurate diagnosis, subtyping, and determining the stage of non-Hodgkin lymphoma (disease).
Special stains and immunophenotyping techniques help identify cell surface markers that distinguish different types of lymphocytes (B-cells vs. T-cells). This aids in subtyping Non-Hodgkin Lymphoma (NHL) and guiding treatment decisions.
Laboratory Investigations
- Complete blood count (CBC): A CBC evaluates red blood cells, white blood cells (including lymphocyte count), and platelets. Abnormalities like low red blood cell count (anemia) or low platelet count (thrombocytopenia) can be seen in some Non-Hodgkin Lymphoma (NHL) cases.
- Liver function tests (LFTs): These tests assess liver function and can be helpful, particularly for specific treatments or to rule out underlying liver issues. In some cases, particularly with involvement of specific subtypes like Burkitt lymphoma, markedly elevated bilirubin levels on LFTs can be a poor prognostic indicator.
- Lactate dehydrogenase (LDH): LDH levels may be elevated in some patients, potentially indicating a more aggressive disease course. However, LDH can be elevated due to other factors, so it’s interpreted in conjunction with other findings.
Cytogenetic and Genetic Analysis
- Karyotyping: This technique analyzes chromosome structure to identify chromosomal translocations, a hallmark of some Non-Hodgkin Lymphoma (NHL) subtypes.
- t(14;18): This translocation is a hallmark of follicular lymphoma, a common B-cell NHL subtype.
- t(4;11): This translocation is often seen in some T-cell lymphomas.
- Fluorescence in situ hybridization (FISH): FISH can detect specific gene rearrangements associated with certain Non-Hodgkin Lymphoma (NHL) types, providing additional diagnostic and prognostic information.
- Follicular Lymphoma: FISH is a cornerstone for confirming the presence of the t(14;18) translocation, a hallmark of follicular lymphoma.
- Mantle Cell Lymphoma: FISH helps detect the t(11;14) translocation, a defining feature of mantle cell lymphoma.
- Burkitt Lymphoma: FISH can identify specific translocations involving the MYC gene, a crucial diagnostic marker for Burkitt lymphoma subtypes.
- Anaplastic Large Cell Lymphoma (ALCL): FISH is used to detect rearrangements in the ALK gene, which is present in a subset of ALCL cases and has therapeutic implications.
Other Relevant Tests Based on Suspicion
- Serum protein electrophoresis (SPEP) and immunofixation: Although less common in classic Non-Hodgkin Lymphoma (NHL) subtypes, some lymphomas, particularly those involving B-cells, can also produce an M-protein. A positive SPEP finding might raise suspicion of plasma cell involvement or a less common Non-Hodgkin Lymphoma (NHL) subtype requiring further investigation.
- Bone marrow aspiration and biopsy: If bone marrow involvement is suspected, a sample is extracted and analyzed for the presence of lymphoma cells.
- Viral serology: Tests for viruses like EBV, HTLV-1, or HHV-8 may be conducted, as some are associated with specific non-Hodgkin lymphoma (disease) subtypes.
- Imaging studies: X-rays, CT scans, PET scans, or MRIs can help assess the extent of lymph node involvement, identify extranodal disease spread, and evaluate for potential complications.
Importance of Combining Investigations
No single test is definitive for diagnosing Non-Hodgkin Lymphoma (NHL). Combining the information from lymph node biopsy, laboratory investigations, imaging studies, and potentially cytogenetic/genetic analysis allows for a comprehensive evaluation and accurate diagnosis of the specific Non-Hodgkin Lymphoma (NHL) subtype and stage.
Staging of Non-Hodgkin Lymphoma
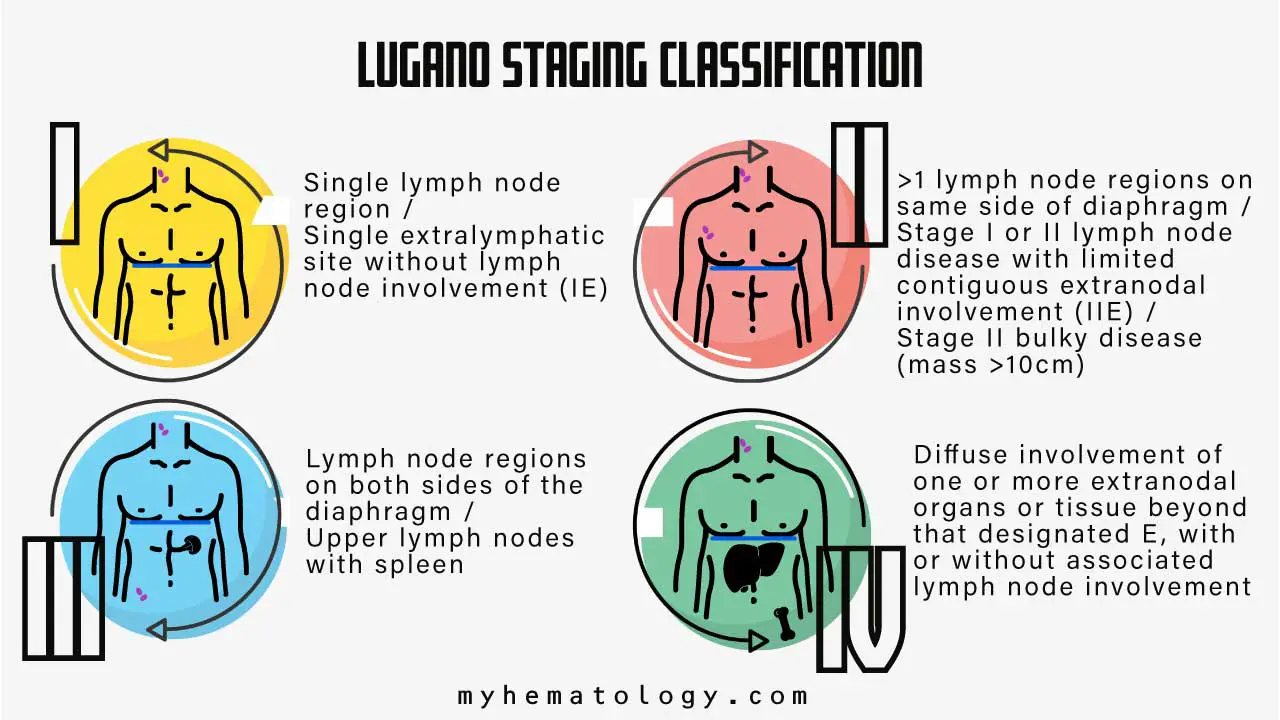
Staging in Non-Hodgkin Lymphoma (NHL) refers to a system that categorizes the extent and severity of the disease. This information is crucial for determining the most appropriate treatment course, predicting potential outcomes, and monitoring treatment response. The most widely used staging system for adults with Non-Hodgkin Lymphoma (NHL) is the Lugano classification, which is a modification of the older Ann Arbor system.
Lugano Classification
The Lugano classification uses Roman numerals (I-IV) to designate the stage of Non-Hodgkin Lymphoma (NHL). Higher stages indicate a more advanced and widespread disease. The system also incorporates letters (E, S, B) to provide additional details about extranodal involvement, specific sites of involvement and bulky disease.
- Stage I: Early-stage Non-Hodgkin Lymphoma (NHL) confined to a single lymph node region (e.g., cervical, inguinal) or a single extralymphatic organ (e.g., spleen, stomach).
- Stage II: Involvement of two or more lymph node regions on the same side of the diaphragm (the muscle separating the chest from the abdomen). Extranodal involvement in an organ or tissue adjacent to an involved lymph node region can also fall under this stage.
- Stage III: This stage involves lymph node regions on both sides of the diaphragm. This may also include involvement of the spleen, extranodal organs/tissues beyond those considered in Stage II, or primary involvement of the spleen, thymus, or Waldeyer’s ring (lymphoid tissue in the throat).
- Stage IV: This advanced stage signifies widespread disease dissemination beyond lymph nodes and other organs. This can involve bone marrow, distant lymph nodes (not contiguous with initially involved regions), multiple or disseminated extranodal organs, or specific sites like the pleura (lining of the lungs) or meninges (membranes surrounding the brain and spinal cord).
Additional Considerations
- Extranodal Involvement (E): The letter “E” is added to the stage if there’s involvement of an organ or tissue outside the lymphatic system.
- Specific Sites (S): This can be used to further specify the location of extranodal involvement (e.g., Spleen (S), Bone (S)).
- Bulky Disease (B): The letter “B” indicates a single lymph node mass larger than 7.5 cm or multiple lymph nodes adding up to a total size exceeding 10 cm. This can influence treatment decisions.
Importance of Staging
Accurate staging guides treatment decisions. Early-stage Non-Hodgkin Lymphoma (NHL) may be treated with curative intent (aiming for a complete cure), while advanced stages may necessitate a palliative approach (focusing on symptom management and disease control).
Staging helps predict potential outcomes. Patients with early-stage non-Hodgkin lymphoma (disease) generally have a better prognosis than those with advanced stages. It also allows for monitoring treatment response. Assessing changes in stage after treatment can indicate disease progression or effectiveness of therapy.
Additional Notes
Imaging studies like CT scans or PET scans are often used in conjunction with clinical evaluation to determine the stage of Non-Hodgkin Lymphoma (NHL). Bone marrow biopsy may be performed in some cases to assess for bone marrow involvement.
The Lugano classification is a simplified explanation. There are additional subcategories within some stages for further refinement of disease extent.
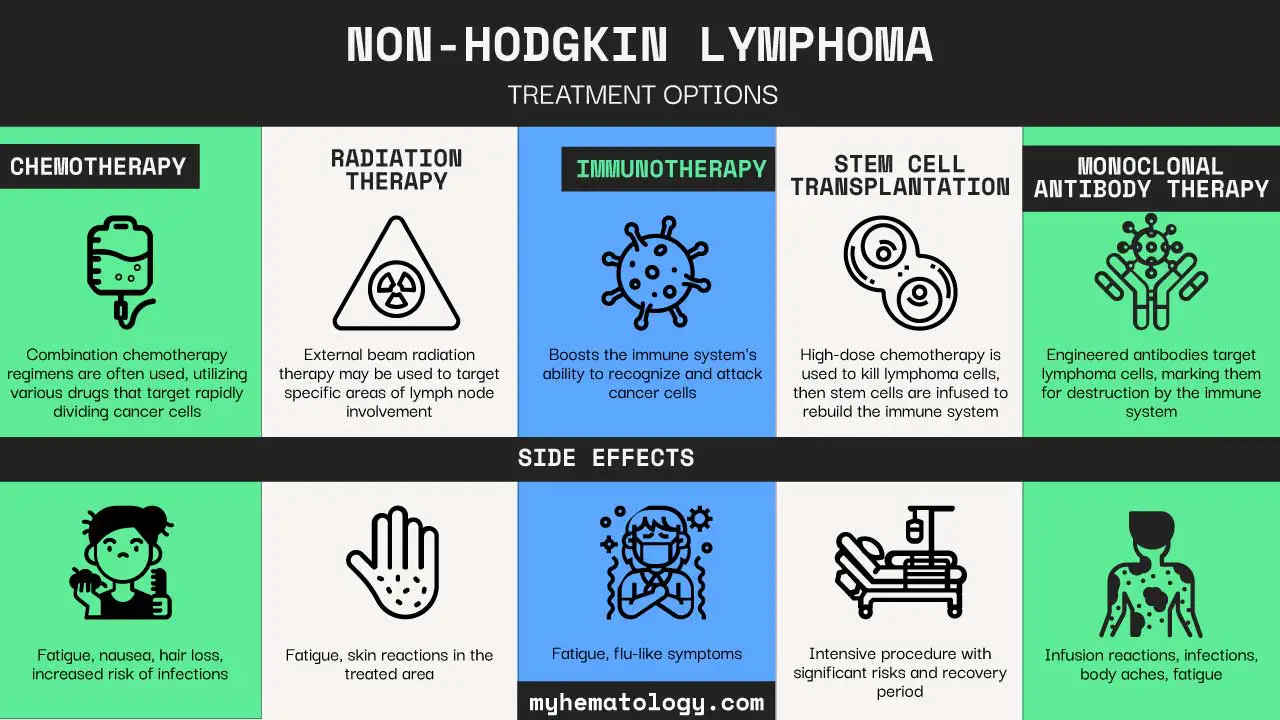
Common Treatment Approaches for NHL
Non-Hodgkin Lymphoma (NHL) treatment approaches are highly individualized, depending on the specific subtype of Non-Hodgkin Lymphoma (NHL), its stage, the patient’s overall health, and their symptoms. Non-Hodgkin Lymphoma (NHL) is broadly categorized into indolent (slow-growing) and aggressive (fast-growing) types, which significantly influences the treatment strategy.
Watchful Waiting (Active Surveillance)
For patients with indolent (slow-growing) types of NHL who do not exhibit any significant signs or symptoms, a “watchful waiting” or “active surveillance” approach may be adopted.
This involves regular check-ups and monitoring the disease without immediate treatment, deferring therapy until the patient develops symptoms or the lymphoma progresses. This is a standard of care for advanced follicular lymphoma.
Chemotherapy
Chemotherapy involves using strong drugs to stop the growth of or kill cancer cells. These drugs can be given intravenously (through a vein) or in pill form. It is a common first-line treatment for many types of Non-Hodgkin Lymphoma (NHL), especially for aggressive forms or when the lymphoma progresses after watchful waiting.
Common Regimens
- R-CHOP: This is a widely used first-line treatment for most types of Non-Hodgkin Lymphoma (NHL), particularly Diffuse Large B-cell Lymphoma (DLBCL), which is an aggressive subtype. R-CHOP combines rituximab (a monoclonal antibody) with four chemotherapy drugs: cyclophosphamide, doxorubicin, vincristine, and prednisone.
- DA-EPOCH-R: Dose-adjusted etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, plus rituximab, is another recommended regimen. This regimen might be used for advanced DLBCL and often does not require additional radiation.
- Other regimens like Pola-R-CHP (polatuzumab vedotin, rituximab, cyclophosphamide, doxorubicin, prednisone) are also used for advanced DLBCL.
- For specific subtypes like Mantle Cell Lymphoma (MCL), which can be challenging to treat, the standard induction therapy regimen is still being established.
- Intrathecal Chemotherapy: For patients at high risk of lymphoma spreading to the brain and spinal cord (Central Nervous System or CNS), chemotherapy may be injected directly into the spinal fluid.
Immunotherapy
Immunotherapy uses medicines to help the body’s own immune system identify and destroy cancer cells. Cancer cells can often evade the immune system, and immunotherapy helps immune cells find and kill them.
- Monoclonal Antibody Therapy (MAB): Rituximab is a key monoclonal antibody often combined with chemotherapy regimens (e.g., R-CHOP). Other anti-CD20 mAB-based regimens and CD19-targeted mABs like tafasitamab are also used, especially for relapsed or refractory follicular lymphoma.
- Targeted Drugs: These drugs focus on specific vulnerabilities in cancer cells. Examples include BTK inhibitors (e.g., ibrutinib, acalabrutinib, zanubrutinib) and BCL-2 inhibitors (e.g., venetoclax). These can be used alone or in combination with monoclonal antibodies or chemotherapy.
- CAR T-cell Therapy: Chimeric Antigen Receptor (CAR) T-cell therapy is an advanced immunotherapy option, particularly for relapsed or refractory disease, where a patient’s own T-cells are genetically modified to better fight the cancer. Examples include brexu-cel and liso-cel.
- Bispecific Antibodies: Novel immunotherapy options, such as CD20 x CD3 bispecific antibodies, are also available as preferred regimens in later lines of therapy.
Radiation Therapy
Radiation therapy uses high-energy rays to kill cancer cells. It may be used for localized tumors, often in combination with chemotherapy. For instance, localized follicular lymphoma (in one or two nearby lymph node groups) may be treated with radiation therapy to the affected areas.
Stem Cell Transplant
Stem cell transplantation (often autologous, using the patient’s own stem cells) can be an option for certain types of NHL, particularly for relapsed or refractory cases after initial treatments.
The choice of treatment is highly dependent on the specific subtype of NHL (e.g., Diffuse Large B-cell Lymphoma, Follicular Lymphoma, Mantle Cell Lymphoma), as well as the stage of the disease (how far it has spread). For example, most patients with localized DLBCL can be cured with chemotherapy alone or with immunomodulatory agents, while advanced disease often requires doxorubicin-based combination therapy with rituximab. If an indolent lymphoma relapses, a biopsy may be performed to check for a more aggressive histology, which would then guide a change in therapy.y
Differential Diagnosis of Non-Hodgkin Lymphoma
Non-Hodgkin Lymphoma (NHL) can present with a wide range of symptoms, many of which are non-specific and can overlap with other, often less serious, medical conditions. This makes a thorough differential diagnosis crucial for accurate identification and appropriate management.
Hodgkin Lymphoma
Both Hodgkin Lymphoma and Non-Hodgkin Lymphoma are types of lymphoma, originating in the lymphatic system and affecting lymphocytes. While they share some common symptoms like swollen lymph nodes and “B symptoms” (fever, night sweats, unexplained weight loss), they are distinct diseases with different clinical characteristics and microscopic features.
The definitive distinction is made through a lymph node biopsy, where Hodgkin lymphoma is characterized by the presence of Reed-Sternberg cells, which are absent in NHL.
Acute Lymphoblastic Leukemia (ALL)
ALL is a cancer of the blood and bone marrow that affects immature lymphocytes. While NHL primarily involves lymph nodes and other lymphoid tissues, ALL is characterized by the proliferation of lymphoblasts in the bone marrow and peripheral blood.
However, some aggressive forms of NHL, particularly lymphoblastic lymphomas, can have features that overlap with leukemia, including bone marrow involvement and changes in blood counts.
Infectious Mononucleosis
Often caused by the Epstein-Barr virus (EBV), infectious mononucleosis can cause symptoms strikingly similar to NHL, including swollen, often painful, lymph nodes (lymphadenopathy), fever, and fatigue.
Unlike the typically painless lymph nodes in NHL, those in infectious mononucleosis are frequently tender.
Other Infections and Inflammatory Conditions
Viral Infections: Many common viral infections can cause enlarged and tender lymph nodes, which can be mistaken for lymphoma.
Bacterial Infections: Localized bacterial infections can also lead to swollen lymph nodes in the affected area.
Autoimmune Diseases: Certain autoimmune conditions can cause lymphadenopathy and systemic symptoms that might mimic lymphoma.
Specific Subtypes of Non-Hodgkin Lymphoma
Low-Grade Non-Hodgkin Lymphoma (NHL)
Low-grade NHLs are a group of non-Hodgkin lymphomas that grow slowly. While they are generally less aggressive than high-grade non-Hodgkin lymphoma (disease), they can still cause significant health problems.
Small Lymphocytic Lymphoma (SLL)
- Characteristics:
- Most common type of low-grade non-Hodgkin lymphoma (disease), affecting B-cells.
- Slow-growing, often with a stable course for years before progression.
- Can involve lymph nodes, blood, and bone marrow.
- Causes: Exact cause unknown, but risk factors include advanced age, family history of lymphoma, and certain autoimmune conditions.
- Symptoms: Often asymptomatic in early stages. Later symptoms may include enlarged painless lymph nodes, fatigue, weight loss, and night sweats.
- Diagnosis: Blood tests (CBC), lymph node biopsy, bone marrow aspiration and biopsy, immunophenotyping to identify specific cell markers.
- Treatment: Depends on stage and symptoms. Watch and wait approach may be common initially. Treatment options include chemotherapy, targeted therapies, and immunotherapy.
Waldenstrom Macroglobulinemia (WM)
- Characteristics:
- Rare low-grade B-cell non-Hodgkin lymphoma (disease) affecting bone marrow.
- Characterized by production of an abnormal protein (M-protein) by cancerous plasma cells.
- Can lead to complications like hyperviscosity syndrome (thickening of blood) and neuropathy (nerve damage).
- Causes: Unknown, but risk factors include advanced age and being male.
- Symptoms: Often asymptomatic initially. Later symptoms may include fatigue, weakness, bleeding tendency, bone pain, and vision problems.
- Diagnosis: Blood tests (CBC, protein electrophoresis), bone marrow biopsy, imaging studies to assess bone involvement.
- Treatment: Depends on stage and symptoms. Watch and wait approach may be used initially. Treatment options include chemotherapy, immunotherapy, and stem cell transplantation in some cases.
Marginal Zone Lymphomas (MZL)
- Characteristics:
- Group of low-grade B-cell non-Hodgkin lymphomas originating from the marginal zone of lymphoid organs (spleen, lymph nodes).
- Several subtypes exist, each with slightly different characteristics and presentations.
- Can involve the spleen, lymph nodes, or extranodal organs (e.g., stomach, lungs).
- Causes: Unknown, but some subtypes may be associated with autoimmune conditions like Sjogren’s syndrome.
- Symptoms: Often asymptomatic in early stages. Later symptoms may include enlarged spleen (splenomegaly), fatigue, weight loss, and abdominal discomfort depending on the involved organ.
- Diagnosis: Blood tests (CBC), lymph node or extranodal tissue biopsy, immunophenotyping.
- Treatment: Depends on stage, symptoms, and subtype. Watch and wait approach may be common. Treatment options include surgery (splenectomy for splenic involvement), radiation therapy, and chemotherapy.
Follicular Lymphoma (FL)
- Characteristics:
- Second most common type of Non-Hodgkin Lymphoma overall, can be low-grade or transformed into a more aggressive form.
- Characterized by the presence of abnormal structures called follicles within involved lymph nodes.
- Primarily affects lymph nodes, but can involve other organs in advanced stages.
- Causes: Unknown, but risk factors include family history of lymphoma, certain autoimmune conditions, and exposure to herbicides.
- Symptoms: Often asymptomatic initially. Later symptoms may include enlarged painless lymph nodes, fatigue, night sweats, and weight loss.
- Diagnosis: Blood tests (CBC), lymph node biopsy, immunophenotyping, PET scan to assess overall disease burden.
- Treatment: Depends on stage, symptoms, and risk factors. Watch and wait approach may be common initially. Treatment options include chemotherapy, immunotherapy with rituximab, and radiation therapy.
Mantle Cell Lymphoma (MCL)
- Characteristics:
- Less common low-grade non-Hodgkin lymphoma (disease) with a more aggressive course than other subtypes listed here.
- Affects B-cells and often progresses to a more aggressive form over time.
- Primarily involves lymph nodes, but can involve other organs in advanced stages.
- Causes: Unknown, but risk factors include advanced age and being male.
- Symptoms: Often symptomatic at diagnosis. Symptoms may include enlarged lymph nodes, fatigue, night sweats, weight loss, and bone pain.
- Diagnosis: Blood tests (CBC), lymph node biopsy, immunophenotyping, genetic testing for specific abnormalities.
- Treatment: Depends on stage and symptoms. Treatment options include chemotherapy, targeted therapy with drugs like ibrutinib, and stem cell transplantation.
High-Grade Non-Hodgkin Lymphomas
High-grade Non-Hodgkin Lymphomas are a group of Non-Hodgkin Lymphomas that grow rapidly and are more aggressive than low-grade non-Hodgkin lymphomas.
Diffuse Large B-Cell Lymphoma (DLBCL)
- Characteristics:
- Most common type of high-grade non-Hodgkin lymphoma (disease), affecting B-cells.
- Rapidly growing, often presenting with widespread lymph node involvement.
- Can involve extranodal organs like the spleen, bone marrow, and digestive tract.
- Causes: Unknown, but risk factors include weakened immune system due to HIV/AIDS or medications, exposure to certain herbicides, and family history of lymphoma.
- Symptoms: May include enlarged lymph nodes, fatigue, night sweats, weight loss, fever, and pain in affected areas.
- Diagnosis: Blood tests (CBC), lymph node biopsy, immunophenotyping, PET scan to assess disease burden.
- Treatment: Typically involves intensive chemotherapy regimens (e.g., R-CHOP) with rituximab, an antibody therapy. In some cases, radiation therapy may be used in combination.
Primary Central Nervous System Lymphoma (PCNSL)
- Characteristics:
- Rare, aggressive non-Hodgkin lymphoma (disease) arising from lymphoid tissue within the brain or spinal cord.
- Symptoms are often neurological and can mimic other conditions.
- Causes: Unknown, but association with Epstein-Barr virus (EBV) is suspected in some cases.
- Symptoms: Headache, confusion, memory problems, seizures, vision changes, weakness, and numbness depending on the location of the tumor.
- Diagnosis: MRI scan with contrast, cerebrospinal fluid (CSF) analysis, and sometimes brain biopsy.
- Treatment: Often involves high-dose methotrexate chemotherapy with or without radiation therapy. Clinical trials are exploring newer treatment options.
Primary Mediastinal B-Cell Lymphoma (PMBCL)
- Characteristics:
- Aggressive B-cell non-Hodgkin lymphoma (disease) primarily affecting the mediastinum (area behind the breastbone).
- Often presents with symptoms related to compression of nearby structures.
- Causes: Unknown, but association with infections like Human immunodeficiency virus (HIV) and Human T-cell lymphotropic virus type 1 (HTLV-1) is possible in some cases.
- Symptoms: Chest pain, cough, shortness of breath, difficulty swallowing (dysphagia), and superior vena cava syndrome (vein blockage causing facial swelling and neck vein distention) due to mass effect.
- Diagnosis: Chest X-ray, CT scan, PET scan, and mediastinoscopy or mediastinotomy (tissue sampling procedures) to obtain tissue for diagnosis.
- Treatment: Generally involves intensive chemotherapy regimens (e.g., DA-EPOCH) with or without radiation therapy depending on the extent of disease.
Burkitt Lymphoma
- Characteristics:
- Highly aggressive B-cell non-Hodgkin lymphoma (disease) with rapid growth and potential for rapid spread.
- Can involve lymph nodes, bone marrow, central nervous system, and other organs.
- Causes: Epstein-Barr virus (EBV) is associated with some cases, while others have a chromosomal translocation involving the MYC gene.
- Symptoms: Rapidly growing tumors, fever, night sweats, weight loss, bone pain, and facial swelling (especially in jaw Burkitt lymphoma) depending on the affected sites.
- Diagnosis: Blood tests (CBC), lymph node or bone marrow biopsy, immunophenotyping, genetic testing for MYC translocation.
- Treatment: Requires intensive chemotherapy regimens (often including high-dose methotrexate) with curative intent. Supportive care plays a crucial role in managing rapid tumor lysis and potential complications.
Lymphoblastic Lymphomas
- Characteristics:
- Group of aggressive NHLs originating from immature lymphocyte precursors (lymphoblasts).
- Can be of T-cell or B-cell lineage, with slightly different presentations.
- Often involve widespread lymph node involvement, bone marrow, and blood.
- Causes: Unknown, but genetic predispositions may play a role in some cases.
- Symptoms: Rapidly growing tumors, fever, night sweats, weight loss, bone pain, fatigue, and increased risk of infections due to bone marrow involvement.
- Diagnosis: Blood tests (CBC showing lymphoblasts), lymph node or bone marrow biopsy, immunophenotyping to determine T-cell or B-cell lineage.
- Treatment: Intensive chemotherapy regimens similar to those used for acute lymphoblastic leukemia (ALL) are employed due to the highly aggressive nature.
T-Cell Non-Hodgkin Lymphoma
T-cell non-Hodgkin lymphomas (NHL) are a group of lymphomas arising from mature T-cells or natural killer (NK) cells. They are less common than B-cell non-Hodgkin lymphoma (disease), but present a diverse range of subtypes with varying clinical presentations.
Peripheral T-Cell Non-Hodgkin Lymphoma, Unspecified (PTCL-U)
- Characteristics:
- Most common type of T-cell non-Hodgkin lymphoma (disease), encompassing various subtypes that don’t fit neatly into defined categories.
- Can be aggressive or indolent (slow-growing).
- Often involves lymph nodes, but can also have extranodal involvement.
- Causes: Unknown, but risk factors include weakened immune system, exposure to certain chemicals, and Epstein-Barr virus (EBV) infection in some cases.
- Symptoms: Variable depending on the specific subtype and stage. May include enlarged lymph nodes, fatigue, night sweats, weight loss, skin rash, or other organ involvement symptoms.
- Diagnosis: Blood tests (CBC), lymph node biopsy, immunophenotyping to identify specific T-cell markers, genetic testing in some cases.
- Treatment: Varies depending on subtype, stage, and patient factors. May involve chemotherapy, immunotherapy, or radiation therapy.
Angioimmunoblastic T-Cell Lymphoma (AITL)
- Characteristics:
- Relatively rare, aggressive T-cell non-Hodgkin lymphoma (disease) with characteristic enlargement of lymph nodes and blood vessels.
- Can cause a variety of systemic symptoms due to immune system dysfunction.
- Causes: Unknown, but EBV infection may be a contributing factor in some cases.
- Symptoms: Enlarged lymph nodes, fatigue, night sweats, weight loss, skin rash, fever, recurrent infections due to immune suppression.
- Diagnosis: Blood tests (CBC, elevated eosinophils), lymph node biopsy, immunophenotyping, PET scan to assess disease burden.
- Treatment: Combination chemotherapy with drugs like steroids and sometimes targeted therapies.
Mycosis Fungoides (MF) and Sezary Syndrome (SS)
- Characteristics:
- Represent a spectrum of cutaneous T-cell lymphoma (CTCL) primarily affecting the skin.
- Mycosis fungoides (MF) is the early stage with patches and plaques on the skin.
- Sezary syndrome (SS) is the advanced stage with widespread skin involvement and abnormal T-cells in the blood.
- Causes: Unknown, but genetic factors and environmental exposures may play a role.
- Symptoms: Itchy, scaly patches or plaques on the skin, which can become red and thickened in later stages. In SS, erythroderma (reddening of most of the body surface) and swollen lymph nodes can occur.
- Diagnosis: Skin biopsy, immunophenotyping of skin cells, blood tests to assess for Sezary syndrome.
- Treatment: Varies depending on the stage. May involve topical steroids, phototherapy (light therapy), chemotherapy, or other targeted therapies.
Adult T-Cell Leukemia/Lymphoma (ATLL)
- Characteristics:
- Aggressive T-cell malignancy associated with Human T-cell lymphotropic virus type 1 (HTLV-1) infection.
- Can present as leukemia (involving blood) or lymphoma (involving lymph nodes and other organs).
- Causes: HTLV-1 infection is the primary cause.
- Symptoms: Varies depending on the presentation (leukemia or lymphoma). May include fatigue, fever, night sweats, weight loss, enlarged lymph nodes, skin rash, and leukemic symptoms like anemia or increased risk of infections.
- Diagnosis: Blood tests (identifying abnormal T-cells and checking for HTLV-1 antibodies), lymph node biopsy if present, bone marrow biopsy.
- Treatment: Limited curative options. Treatment focuses on managing symptoms and prolonging survival with chemotherapy, antiretroviral therapy (if HTLV-1 positive), and other supportive measures.
Enteropathy-Associated T-Cell Lymphoma (EATL)
- Characteristics:
- Rare, aggressive T-cell non-Hodgkin lymphoma (disease) primarily affecting the small intestine.
- Can cause significant digestive problems and malnutrition.
- Causes: Unknown, but gluten sensitivity (celiac disease) may be a risk factor in some cases.
- Symptoms: Abdominal pain, diarrhea, weight loss, nausea, vomiting, malnutrition.
- Diagnosis: Endoscopy with biopsy of the small intestine, blood tests, imaging studies (CT scan) to assess for extent of involvement.
- Treatment: Challenging to treat due to its aggressive nature. May involve surgery, chemotherapy, and sometimes stem cell transplantation.
Anaplastic Large Cell Lymphoma (ALCL)
- Characteristics:
- A heterogeneous group of T-cell lymphomas with characteristic large, abnormal cells.
- Can be primary cutaneous (skin only) or systemic (involving lymph nodes and other organs).
- ALK-positive ALCL is a subtype with a specific genetic abnormality and may have a better prognosis with targeted therapy.
- Causes: Unknown, but some cases, particularly ALK-positive ALCL, have specific genetic translocations.
- Symptoms: Variable depending on the type (cutaneous or systemic). Cutaneous ALCL presents with red, raised skin lesions that may ulcerate. Systemic ALCL can cause enlarged lymph nodes, fever, fatigue, night sweats, and weight loss.
- Diagnosis: Skin or lymph node biopsy, immunophenotyping to identify T-cell markers, ALK testing for specific genetic abnormality.
- Treatment: Varies depending on the type and stage. May involve chemotherapy, radiation therapy, or targeted therapy (e.g., Brentuximab vedotin for ALK-positive ALCL).
Extranodal NK/T-Cell Lymphoma
- Characteristics:
- Uncommon, aggressive lymphoma arising from natural killer (NK) cells or nasal-type T-cells.
- Primarily affects the upper aerodigestive tract (especially the nasal cavity and sinuses) but can involve other extranodal sites like skin, gastrointestinal tract, or testes.
- Causes: Epstein-Barr virus (EBV) infection is strongly associated with this type of lymphoma.
- Symptoms: Nasal congestion, facial swelling, nosebleeds, sinusitis, difficulty breathing, facial pain, can also cause skin lesions or symptoms related to other extranodal sites involved.
- Diagnosis: Biopsy of the affected tissue (nasal cavity, skin, etc.), immunophenotyping to identify NK/T-cell markers, EBV testing to assess for viral association.
- Treatment: Often involves a combination of chemotherapy, radiation therapy, and potentially immunotherapy.
Prognosis and Survival Rate
Certainly, here is the information on the prognosis and survival of Non-Hodgkin Lymphoma (NHL) presented in a table format:
| Factor | Description/Impact on Prognosis | Survival Statistics (5-Year or more, if applicable) |
| Type of NHL (Histologic Subtype) | Highly variable; B-cell lymphomas often have a better prognosis than T-cell lymphomas. Indolent types are slow-growing but typically not curable; aggressive types are fast-growing but often curable. | |
| Follicular Lymphoma (Indolent) | Generally better prognosis than DLBCL. | Around 85% survive for 5 years or more. Low-risk group: almost 100%; Intermediate-risk: around 90%; High-risk: almost 75%. |
| Marginal Zone Lymphoma (Indolent) | Almost 80% survive for 5 years or more. | |
| Mycosis Fungoides (CTCL) | Almost 80% survive for 5 years or more. | |
| Diffuse Large B-cell Lymphoma (Aggressive) | Rapidly progressive, but often responsive to chemotherapy and curable. | Around 60% survive for 5 years or more. |
| Burkitt Lymphoma (Aggressive) | Rapidly progressive, but often responsive to chemotherapy and curable. | Around 55% survive for 5 years or more. |
| Mantle Cell Lymphoma (Aggressive) | Can be difficult to treat, often more aggressive course. | More than 45% survive for 5 years or more. |
| Anaplastic Large-Cell Lymphoma (ALCL) | ALK-positive has a better prognosis than ALK-negative. | ALK-positive: 80%; ALK-negative: around 45% survive for 5 years or more. |
| Peripheral T-cell Lymphoma (PTCL) | Generally less favorable prognosis than B-cell lymphomas. | Around 35% survive for 5 years or more (PTCL NOS: around 30%). |
| Age | Younger patients (under 60) generally have a better prognosis. | For DLBCL: <40 years: almost 90%; 40-59 years: >50%; 60+ years: 30% survive for 5 years or more. |
| Lactate Dehydrogenase (LDH) Level | Normal LDH levels indicate a better prognosis; higher levels suggest more advanced or fast-growing cancer. | |
| Stage of NHL | Lower stages (1 and 2) have a better prognosis than higher stages (3 and 4). | |
| Performance Status | Good performance status (ability to perform daily tasks) is associated with a better prognosis. | |
| Spread Outside of Lymph Nodes (Extranodal Disease) | NHL confined to lymph nodes has a better prognosis and is more likely to be successfully treated. | |
| Bulky Disease | Presence of a large tumor (>10 cm) indicates a less favorable prognosis, as smaller tumors respond better to treatment. | |
| B Symptoms | Presence of unexplained fever, drenching night sweats, and unexplained weight loss indicates a less favorable prognosis. | |
| Hemoglobin Levels | Normal hemoglobin levels are associated with a better prognosis. |
Frequently Asked Questions (FAQs)
What are the first signs of non-Hodgkin’s lymphoma?
The first signs of Non-Hodgkin Lymphoma (NHL) can vary, but the most common initial symptom is often the painless swelling of lymph nodes. Other signs include:
B Symptoms are a group of systemic symptoms that can indicate lymphoma. These B symptoms are more commonly seen in patients with high-grade (aggressive) variants of NHL.
- Unexplained Fever: A fever over 38°C that doesn’t go away.
- Drenching Night Sweats: Sweats severe enough to soak bedding and night clothes.
- Unexplained Weight Loss: Losing more than 10% of body weight within the last 6 months without trying.
Fatigue: A persistent feeling of being very tired or a general lack of energy.
Itchiness: Severe or unexplained itchiness, sometimes accompanied by reddened patches on the skin. NHL can also manifest as itchy, red or purple lumps under the skin.
Is non-Hodgkin’s lymphoma a serious cancer?
Yes, Non-Hodgkin Lymphoma (NHL) is considered a serious cancer. It is a type of blood cancer that originates in the lymphatic system, affecting white blood cells called lymphocytes. However, NHL is not a single disease, but rather a heterogeneous group of closely related cancers.
Is non-Hodgkin’s lymphoma 100% curable?
No, Non-Hodgkin Lymphoma (NHL) is not 100% curable. The curability of NHL depends significantly on its specific subtype and how quickly it is growing.
- Indolent (Slow-Growing) NHL: These types of NHL are generally responsive to therapy, meaning they can be managed effectively, but they are typically not curable with standard treatment approaches. For instance, Follicular Lymphoma, a common indolent type, is usually slow-growing and responsive to treatment, but often not curable.
- Aggressive (Fast-Growing) NHL: These types are rapidly progressive, but they are often responsive to chemotherapy and frequently curable. For example, Diffuse Large B-cell Lymphoma (DLBCL), a common aggressive type, can often be cured, especially when localized. More than half of patients with advanced DLBCL are cured with doxorubicin-based combination therapy and rituximab.
Can you get non-Hodgkin’s lymphoma twice?
Yes, it is possible to experience Non-Hodgkin Lymphoma (NHL) more than once, either as a relapse of the original cancer or as a new, distinct second primary NHL.
Can you have non-Hodgkin’s lymphoma for years without knowing?
Yes, it is possible to have Non-Hodgkin Lymphoma (NHL) for years without knowing, particularly with indolent (slow-growing) NHL.
These types of NHL tend to grow very slowly. Patients with low-grade (indolent) NHL may experience symptoms like painless swelling of lymph nodes, often in the neck, armpit, or groin, but otherwise appear healthy. This swelling might even come and go for a period. Because of their slow progression and sometimes subtle or intermittent symptoms, indolent lymphomas can go undetected for years. They are often managed with “watchful waiting” if they are not causing significant symptoms, as they may not require immediate treatment.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. WHO Classification of Tumours, Revised 4th Edition, Volume 2. 2017.
- Adler EM. Living with Lymphoma: A Patient’s Guide (Johns Hopkins Press Health Books (Paperback)). 2016.
- Leukemia & Lymphoma Society (LLS)
- Denlinger N, Bond D, Jaglowski S. CAR T-cell therapy for B-cell lymphoma. Curr Probl Cancer. 2022 Feb;46(1):100826. doi: 10.1016/j.currproblcancer.2021.100826. Epub 2021 Dec 25. PMID: 35012754; PMCID: PMC9284423.
- Sehn LH, Herrera AF, Flowers CR, Kamdar MK, McMillan A, Hertzberg M, Assouline S, Kim TM, Kim WS, Ozcan M, Hirata J, Penuel E, Paulson JN, Cheng J, Ku G, Matasar MJ. Polatuzumab Vedotin in Relapsed or Refractory Diffuse Large B-Cell Lymphoma. J Clin Oncol. 2020 Jan 10;38(2):155-165. doi: 10.1200/JCO.19.00172. Epub 2019 Nov 6. PMID: 31693429; PMCID: PMC7032881.
- Minson A, Tam C, Dickinson M, Seymour JF. Targeted Agents in the Treatment of Indolent B-Cell Non-Hodgkin Lymphomas. Cancers (Basel). 2022 Mar 1;14(5):1276. doi: 10.3390/cancers14051276. PMID: 35267584; PMCID: PMC8908980.
- Sapkota S, Shaikh H. Non-Hodgkin Lymphoma. [Updated 2023 Feb 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559328/



