TL;DR
Jaundice is a condition characterized by a yellowish discoloration of the skin, eyes, and mucous membranes. It occurs when there is an excessive buildup of bilirubin (hyperbilirubinemia), a yellow pigment produced by the breakdown of red blood cells, in the blood.
Types of Jaundice ▾
- Prehepatic Jaundice: Caused by excessive red blood cell destruction (e.g., hemolytic anemias).
- Hepatic Jaundice: Caused by liver damage or dysfunction (e.g., viral hepatitis, cirrhosis).
- Posthepatic Jaundice: Caused by obstruction of the bile ducts (e.g., gallstones, pancreatic cancer).
Symptoms ▾
- Yellowing of the skin, eyes, and mucous membranes
- Dark urine
- Pale stools
- Fatigue
- Abdominal pain
- Itching
- Weight loss
Causes ▾
- Prehepatic: Hemolytic anemias, ineffective erythropoiesis
- Hepatic: Viral hepatitis, cirrhosis, drug-induced liver injury, autoimmune hepatitis
- Posthepatic: Gallstones, pancreatic cancer, strictures of the bile ducts
Laboratory Tests ▾
- Liver function tests (LFTs)
- Bilirubin fractionation
- Complete blood count (CBC)
- Coagulation profile
- Imaging studies (e.g., ultrasound, CT scan, MRI)
Treatment ▾
- Depends on the underlying cause
- May involve medications, surgery, or lifestyle changes
Complications ▾
- Liver failure
- Cirrhosis
- Liver cancer
- Hepatic encephalopathy
- Peripheral neuropathy
- Kidney failure
- Bleeding and bruising
- Malnutrition
- Infection
- Infertility
*Click ▾ for more information
Introduction
Jaundice, a condition manifesting as yellowing of the skin, eyes, and mucous membranes, is frequently associated with liver or biliary tract disorders. The primary cause of jaundice is hyperbilirubinemia, an abnormally high concentration of bilirubin in the blood. Bilirubin is a yellowish pigment produced by the breakdown of red blood cells.
Underlying Pathophysiology (Hyperbilirubinemia)
Hyperbilirubinemia occurs when there is an imbalance between the production and clearance of bilirubin. This can happen due to:
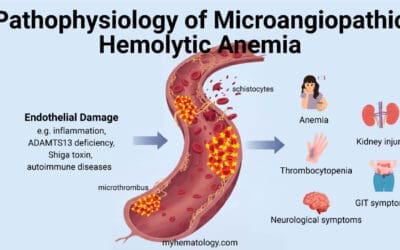
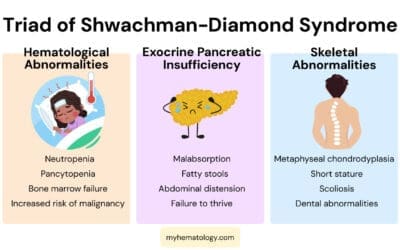
- Increased bilirubin production: This often occurs in conditions like hemolytic anemias where red blood cells are destroyed at an accelerated rate.
- Decreased bilirubin conjugation: The liver is responsible for converting bilirubin into a water-soluble form that can be excreted in bile. If the liver’s ability to conjugate bilirubin is impaired, as in certain liver diseases, hyperbilirubinemia can occur.
- Impaired bile flow: Obstructions in the biliary tract, such as gallstones or tumors, can prevent bilirubin from being excreted, leading to its accumulation in the blood.
Types of Jaundice
Prehepatic Jaundice
Prehepatic jaundice occurs when there is an excessive production of bilirubin (hyperbilirubinemia) that the liver cannot adequately process. This typically happens due to increased red blood cell destruction.
Common Causes of Prehepatic Jaundice
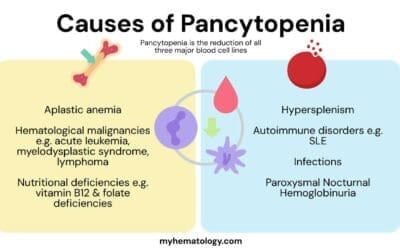
Hemolytic Anemias
Ineffective Erythropoiesis
- Megaloblastic Anemias
- Lead Poisoning
- Pyridoxine (Vitamin B6) Deficiency
Others
- Massive Blood Transfusion: In some cases, a massive blood transfusion can overload the liver’s ability to process bilirubin, leading to prehepatic jaundice.
- Certain Infections: Some infections, such as malaria and babesiosis, can cause red blood cell destruction and lead to prehepatic jaundice.
Hepatic jaundice
Hepatic jaundice occurs when the liver is unable to process bilirubin effectively leading to hyperbilirubinemia. The underlying mechanisms of hepatic jaundice involve reduced bilirubin uptake, impaired conjugation, or decreased excretion.
Common Causes of Hepatic Jaundice
Liver Damage or Dysfunction
- Viral Hepatitis: Infections with hepatitis A, B, C, D, or E viruses can cause liver inflammation and damage, leading to impaired bilirubin processing.
- Cirrhosis: Chronic liver damage, often caused by excessive alcohol consumption or chronic hepatitis, can lead to scarring and impaired liver function.
- Alcoholic Liver Disease: Excessive alcohol consumption can cause liver inflammation, fatty liver, and eventually cirrhosis.
- Non-Alcoholic Fatty Liver Disease (NAFLD): This condition is associated with obesity and metabolic syndrome. It can lead to liver inflammation and damage.
- Drug-Induced Liver Injury: Certain medications can cause liver damage, including acetaminophen overdose, antibiotics, and anti-seizure medications.
- Autoimmune Hepatitis: This is a chronic inflammatory condition caused by the body’s immune system attacking the liver.
- Wilson Disease: This genetic disorder causes copper to accumulate in the liver, leading to damage.
- Hemochromatosis: This genetic disorder causes excess iron to accumulate in the liver, leading to damage.
- Alpha-1 Antitrypsin Deficiency: This inherited disorder can cause liver damage, particularly in smokers.
Impaired Bilirubin Metabolism
- Gilbert Syndrome: This inherited condition causes mild unconjugated hyperbilirubinemia due to a deficiency in the enzyme UDP-glucuronyltransferase.
- Crigler-Najjar Syndrome: This rare genetic disorder is characterized by severe unconjugated hyperbilirubinemia due to a complete or partial deficiency of UDP-glucuronyltransferase.
- Dubin-Johnson Syndrome: This inherited disorder is characterized by conjugated hyperbilirubinemia due to an impaired secretion of bilirubin into the bile ducts.
- Rotor Syndrome: This inherited disorder is similar to Dubin-Johnson syndrome but without the dark pigmentation of the liver.
Posthepatic Jaundice
Posthepatic jaundice occurs when there is an obstruction of the bile ducts, preventing the flow of bile into the intestines. This can lead to the buildup of bilirubin in the blood leading to hyperbilirubinemia, causing jaundice.
Common Causes of Posthepatic Jaundice
- Gallstones: Gallstones are hard, stone-like formations that can form in the gallbladder. If a gallstone blocks the common bile duct, it can cause posthepatic jaundice.
- Pancreatic Cancer: Pancreatic cancer can compress the common bile duct, leading to obstruction.
- Strictures of the Bile Ducts: Strictures are narrowings of the bile ducts that can be caused by inflammation, scarring, or tumors.
- Ampullary Carcinoma: This type of cancer can occur at the junction of the common bile duct and the pancreatic duct, leading to obstruction.
- Parasitic Infections: Certain parasitic infections, such as liver flukes, can cause inflammation and scarring of the bile ducts.
- Congenital Biliary Atresia: This is a rare congenital condition that affects newborns, causing the bile ducts to be absent or narrowed.
Jaundice Symptoms
Jaundice, characterized by a yellowish discoloration of the skin, eyes, and mucous membranes, is a symptom of underlying hyperbilirubinemia. While the most visible symptom is the yellowing of tissues, jaundice can also be accompanied by other symptoms.
Common Symptoms

- Yellowing of the skin, eyes, and mucous membranes: This is the most classic symptom of jaundice due to the hyperbilirubinemia.
- Dark urine: Bilirubin can darken urine, giving it a tea-colored appearance.
- Pale stools: When bilirubin is unable to reach the intestines, stools may become pale or clay-colored.
- Fatigue: Jaundice (hyperbilirubinemia) can lead to fatigue due to the underlying liver disease or anemia.
- Abdominal pain or discomfort: In some cases, jaundice (hyperbilirubinemia) may be associated with abdominal pain or discomfort, particularly if it is caused by liver inflammation or obstruction of the bile ducts.
Other Potential Symptoms
- Itching: Itching is a common symptom of jaundice, especially in cases of obstructive jaundice.
- Weight loss: If jaundice is caused by an underlying chronic liver disease, weight loss may occur.
- Fever: Fever may be present if jaundice (hyperbilirubinemia) is caused by an infection, such as viral hepatitis.
- Nausea and vomiting: Nausea and vomiting can be symptoms of liver disease or gallbladder problems that may lead to jaundice (hyperbilirubinemia).
- Confusion or altered mental status: In severe cases of liver disease, jaundice (hyperbilirubinemia) can be accompanied by confusion or altered mental status.
Laboratory Investigations
Several laboratory tests are typically performed to determine the underlying cause and assess the severity of the condition. These tests help to measure bilirubin levels, evaluate liver function, and identify potential underlying diseases.
Common Laboratory Tests
- Liver Function Tests (LFTs)
- Alanine aminotransferase (ALT) and aspartate aminotransferase (AST): Elevated levels of these enzymes suggest liver cell damage.
- Alkaline phosphatase (ALP) and gamma-glutamyl transferase (GGT): Increased levels of these enzymes are often associated with cholestatic jaundice.
- Bilirubin: Elevated bilirubin levels confirm the presence of jaundice (hyperbilirubinemia).
- Albumin: Decreased albumin levels may indicate chronic liver disease.
- Bilirubin Fractionation
- Direct bilirubin: Elevated direct bilirubin levels suggest obstructive or hepatocellular jaundice.
- Indirect bilirubin: Elevated indirect bilirubin levels suggest prehepatic or unconjugated hyperbilirubinemia.
- Complete Blood Count (CBC)
- Hemoglobin: Decreased hemoglobin levels may indicate hemolytic anemia, a common cause of prehepatic jaundice.
- White blood cell count: An elevated white blood cell count may suggest an infection or inflammatory process.
- Platelet count: A decreased platelet count may indicate an underlying bleeding disorder.
- Coagulation Profile
- Prothrombin time (PT) and international normalized ratio (INR): Prolonged PT and INR can indicate impaired liver function, particularly in cases of chronic liver disease.
Other Laboratory Investigations
- Imaging Studies
- Ultrasound: This is often the first imaging test performed to evaluate the liver, gallbladder, and biliary ducts. It can help to identify gallstones, bile duct obstructions, and liver abnormalities.
- Computed Tomography (CT) Scan: A CT scan can provide more detailed images of the liver, gallbladder, and biliary ducts, especially if ultrasound findings are inconclusive. It can also help to detect pancreatic cancer or other tumors that may be causing jaundice.
- Magnetic Resonance Imaging (MRI): MRI is particularly useful for evaluating the bile ducts and detecting subtle abnormalities. It can also be used to assess the extent of liver damage.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): This procedure involves inserting a thin tube with a camera through the mouth and into the small intestine to visualize the bile ducts and pancreas. It can be used to diagnose and treat biliary duct obstructions.
- Other Tests
- Viral Markers: If viral hepatitis is suspected, blood tests can be performed to detect antibodies to hepatitis A, B, C, D, or E viruses.
- Autoimmune Markers: If autoimmune hepatitis is suspected, blood tests can be performed to detect antibodies associated with autoimmune diseases.
- Genetic Testing: Genetic testing may be performed to diagnose inherited disorders such as Wilson disease or hemochromatosis.
- Liver Biopsy: A liver biopsy can be performed to obtain a tissue sample for examination under a microscope. This can help to diagnose specific liver diseases and assess the extent of liver damage.
The choice of imaging studies and other tests will depend on the clinical presentation, suspected diagnosis, and the results of initial laboratory tests.
Expected Findings in Hyperbilirubinemia
- Prehepatic Jaundice
- Elevated indirect bilirubin
- Normal or slightly elevated AST and ALT
- Normal ALP and GGT
- Evidence of hemolysis on CBC
- Hepatocellular Jaundice
- Elevated direct and indirect bilirubin
- Elevated AST and ALT
- Normal or slightly elevated ALP and GGT
- Possible evidence of liver inflammation or damage on imaging studies
- Posthepatic Jaundice
- Elevated direct bilirubin
- Normal or slightly elevated AST and ALT
- Elevated ALP and GGT
- Evidence of biliary obstruction on imaging studies
It’s important to note that these are general guidelines, and specific findings may vary depending on the individual case.
Treatment and Management
The treatment and management of jaundice depend on the underlying cause. However, there are some general principles that apply to most cases.
General Management
- Hydration: Ensuring adequate hydration is important, especially in cases of dehydration or vomiting.
- Nutrition: A balanced diet can help support liver function and overall health. In some cases, dietary restrictions may be necessary.
- Rest: Adequate rest can help the liver recover and function properly.
- Pain Management: If jaundice is associated with pain, over-the-counter pain relievers can be used. However, it’s important to consult a healthcare professional before taking any medications.
Specific Treatments Based on Cause
- Prehepatic Jaundice: Treatment often focuses on addressing the underlying cause, such as treating hemolytic anemias or correcting vitamin deficiencies.
- Hepatic Jaundice: Treatment may involve medications to address the underlying cause, such as antiviral therapy for viral hepatitis or immunosuppressive therapy for autoimmune hepatitis. In severe cases, a liver transplant may be necessary.
- Posthepatic Jaundice: Treatment often involves addressing the underlying obstruction, which may require surgery, endoscopic procedures, or medications.
Medications
- Antiviral Therapy: For viral hepatitis, antiviral medications can help suppress the virus and improve liver function.
- Corticosteroids: Corticosteroids may be used to treat autoimmune hepatitis or certain types of cholestasis.
- Bile Acid Sequestrants: These medications can help reduce the amount of bile acids in the bloodstream, which can be beneficial in some cases of cholestatic jaundice.
- Antibiotics: Antibiotics may be used to treat infections that can contribute to jaundice, such as bacterial cholangitis.
- Pain Relievers: Over-the-counter pain relievers can be used to manage pain associated with jaundice.
Surgical Procedures
- Cholecystectomy: If gallstones are causing obstructive jaundice, surgery to remove the gallbladder may be necessary.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): This procedure can be used to remove gallstones from the bile ducts or to place stents to relieve obstructions.
- Liver Transplant: In severe cases of liver disease, a liver transplant may be necessary.
Complications
Jaundice (hyperbilirubinemia), if left untreated or poorly managed, can lead to a variety of complications. These complications can affect multiple organ systems and have serious consequences.
Liver-Related Complications
- Liver Failure: Severe jaundice can progress to liver failure, a life-threatening condition characterized by the liver’s inability to function properly.
- Cirrhosis: Chronic liver damage caused by jaundice (hyperbilirubinemia) can lead to cirrhosis, a condition characterized by the formation of scar tissue in the liver. Cirrhosis can impair liver function and increase the risk of liver cancer.
- Liver Cancer: Jaundice (hyperbilirubinemia) can be a symptom of liver cancer, which is a serious condition that can be fatal.
Neurological Complications
- Hepatic Encephalopathy: This condition is characterized by brain dysfunction due to liver failure. It can cause confusion, disorientation, and even coma.
- Peripheral Neuropathy: Jaundice can sometimes be associated with nerve damage, leading to numbness, tingling, or weakness in the extremities.
Other Complications
- Kidney Failure: Jaundice (hyperbilirubinemia) can sometimes lead to kidney failure, especially if the underlying cause is severe liver disease.
- Bleeding and Bruising: Impaired liver function can affect blood clotting, leading to bleeding and bruising.
- Malnutrition: Jaundice (hyperbilirubinemia) can interfere with digestion and absorption of nutrients, leading to malnutrition.
- Infection: People with jaundice (hyperbilirubinemia) may be more susceptible to infections due to a weakened immune system.
- Infertility: In some cases, jaundice (hyperbilirubinemia) can affect fertility, particularly in men.
Preventing Complications
- Early Diagnosis and Treatment: Early diagnosis and treatment can help prevent complications.
- Regular Follow-up: Patients should follow up with their healthcare provider for regular monitoring and assessment.
- Lifestyle Modifications: Making lifestyle changes, such as avoiding alcohol and maintaining a healthy weight, can help reduce the risk of complications.
It’s important to note that the risk of complications associated with jaundice (hyperbilirubinemia) varies depending on the underlying cause and the severity of the condition.
Frequently Asked Questions (FAQs)
Can jaundice (hyperbilirubinemia) recover by itself?
Yes, in some cases, jaundice (hyperbilirubinemia) can recover by itself. However, the ability for jaundice (hyperbilirubinemia) to resolve on its own depends on the underlying cause. For example, mild cases of jaundice (hyperbilirubinemia) caused by viral infections or transient hemolysis may resolve without medical intervention. However, more severe cases, such as those caused by chronic liver disease or biliary obstruction, may require medical treatment to prevent complications.
Can the liver heal after jaundice (hyperbilirubinemia)?
Yes, in many cases, the liver can heal after jaundice (hyperbilirubinemia). However, the extent of healing depends on the underlying cause and the severity of the liver damage. If the jaundice (hyperbilirubinemia) is caused by a reversible condition, such as a viral infection or gallstones, the liver may be able to recover fully. However, if it is caused by chronic liver disease or cirrhosis, the damage may be irreversible.
What is the danger stage of jaundice (hyperbilirubinemia)?
The danger stage of jaundice depends on the underlying cause and the severity of the condition.
In general, jaundice becomes more dangerous when it is accompanied by:
- Severe liver damage: This can lead to liver failure, which is a life-threatening condition.
- Complications: Jaundice (hyperbilirubinemia) can cause complications such as bleeding, infections, kidney failure, and brain damage.
- Lack of treatment: If jaundice (hyperbilirubinemia) is left untreated or poorly managed, it can worsen and increase the risk of complications.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Joseph A, Samant H. Jaundice. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK544252/
- Stevens S, Rivas H, Cacchione RN, O’Rourke NA, Allen JW. Jaundice due to extrabiliary gallstones. JSLS. 2003 Jul-Sep;7(3):277-9. PMID: 14558721; PMCID: PMC3113212.
- Chen, HL., Wu, SH., Hsu, SH. et al. Jaundice revisited: recent advances in the diagnosis and treatment of inherited cholestatic liver diseases. J Biomed Sci 25, 75 (2018). https://doi.org/10.1186/s12929-018-0475-8