TL;DR
Hereditary spherocytosis is an inherited hemolytic anemia due to a defect in a red cell membrane protein. It has mainly an autosomal dominant inheritance pattern.
Signs and symptoms ▾
- Mild to moderate anemia
- Intermittent jaundice precipitated by pregnancy, fatigue or infection
- Moderate splenomegaly
- Presence of pigment gallstones
- Aplastic crises triggered by an acute parvovirus B19 infection.
Causes of hereditary spherocytosis ▾
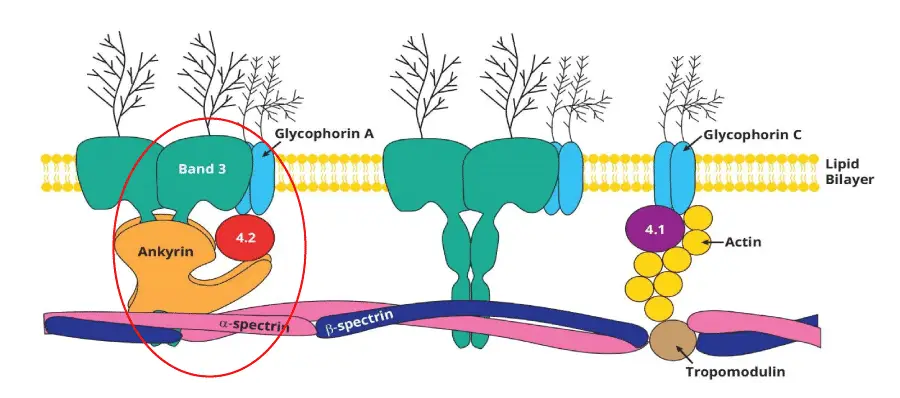
Genetic mutations. Most common mutations are mutations found in the ankyrin, spectrin, band 3 or band protein 4.2.
Pathophysiology ▾
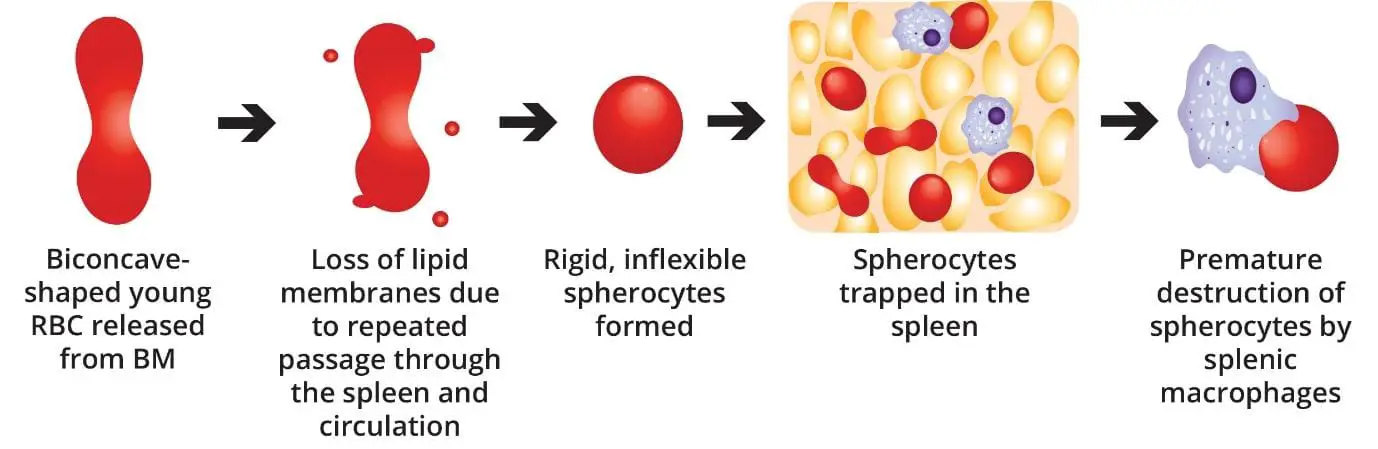
Normal-shaped young RBCs are produced by the bone marrow → repeated passage through the spleen and circulation leads to loss of membrane surface area releasing bilayer lipids in the form of cytoskeleton-free vesicles → spherocytes (rigid, inflexible and less deformable) → premature destruction of spherocytes by splenic macrophages (extravascular hemolysis).
Laboratory Investigations ▾
- Full blood count: variable hemoglobin level and reticulocytosis.
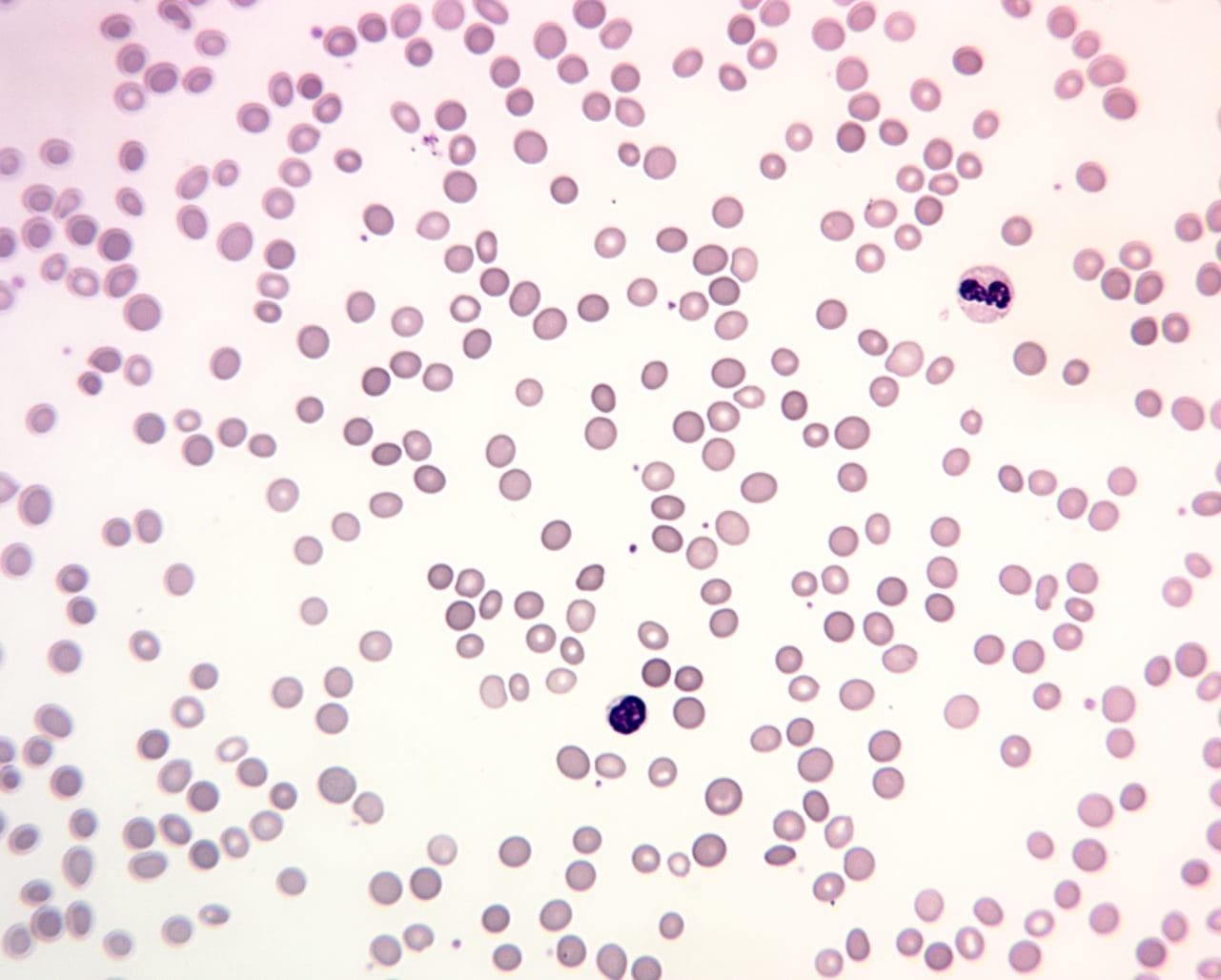
- Peripheral blood smear: Numerous polychromatic spherocytes.
- Bone marrow smear: Markedly hypercellular with erythroid hyperplasia
- ↑ serum bilirubin.
- ↑ urine urobilinogen.
- ↓ serum haptoglobin.
- Negative direct antiglobulin (Coombs) test.
- ↑ Osmotic fragility test
- ↓ fluorescent signal in flow cytometric analysis of eosin-5-maleimide binding.
- Positive family history
Treatment and management of hereditary spherocytosis ▾
- Folic acid supplement
- Splenectomy in severe cases
- Prophylactic penicillin V lifelong post splenectomy
*Click ▾ for more information
What is hereditary spherocytosis?
Hereditary spherocytosis is the most common hereditary (inherited) hemolytic anemia in northern Europeans. Hemolytic anemias are defined as those anemias that result from an increase in red cell destruction rate.
There are two main mechanisms whereby red cells are destroyed in hemolytic anemia. There may be excessive removal of red cells by cells of the reticuloendothelial system or they may be broken down directly in the circulation in a process known as intravascular hemolysis.
Hereditary hemolytic anemias are the result of ‘intrinsic’ red cell defects whereas acquired hemolytic anemias are usually the result of an extracorpuscular or environmental change. Paroxysmal nocturnal haemoglobinuria is the exception because although it is an acquired disorder, the red cells have an intrinsic effect.
Normal red cell destruction
A red blood cell’s normal life span is 120 days, after which the cells will be removed extravascularly by the macrophages in the reticuloendothelial system.
The heme iron will be recycled to to produce more erythrocytes (red cells) in the bone marrow and the protoporphyrin is broken down into bilirubin and goes through a process and eventually excreted as urobilinogen in the urine and stercobilinogen in the feces.
Globin chains are broken down to amino acids which are reutilized for general protein synthesis in the body.
What causes hereditary spherocytosis?
Hereditary spherocytosis is usually caused by defects in the membrane proteins involved in the vertical interactions between the membrane skeleton and the lipid bilayer of the red cell, for example mutations found in the band 3 protein, ankyrin, protein 4.2 or alpha spectrin. The inheritance pattern of this disorder is autosomal dominant. Only 1 mutant allele needs to be inherited for the patient to be symptomatic.
Pathophysiology of hereditary spherocytosis
As the RBC travels at a very high speed in the vascular lumen, the RBC inadvertently knocks against the vascular lumen wall and also other cells. This causes multiple loss of the phospholipid bilayer. The loss of membrane may be caused by the release of parts of the lipid bilayer that are not supported by the skeleton. The marrow produces red cells that are normal biconcave shapes but these lose membrane and become increasingly spherical as they circulate through the spleen and the rest of the reticuloendothelial system. These spherocytes are rigid and inflexible. Ultimately, the spherocytes will be unable to pass through the splenic microcirculation where they are prematurely phagocytosed and destroyed by the splenic macrophages.
Features of hereditary spherocytosis
The anemia can present at any age with fluctuating jaundice. Splenomegaly is common as well as pigment gallstones. Aplastic crises may cause a sudden increase in severity of anemia when precipitated by a parvovirus infection.
How do I test for hereditary spherocytosis?
General laboratory tests
Laboratory investigations show decreased hemoglobin level with reticulocytosis in the full blood count. The blood films reveal anemia with numerous polychromatic spherocytes. The bone marrow smear indicates a hypercellular bone marrow with erythroid hyperplasia.
Specific laboratory tests
In specific tests, the cells are fragile thus have an increased osmotic fragility, with increased serum bilirubin levels and urine urobilinogen. Coombs’ test is negative as it is not an immune disorder and there should be a positive family history.
How is hereditary spherocytosis treated or managed?
Treatment and management of hereditary spherocytosis include prophylactic folic acid supplementation in severe cases to prevent folate deficiency. Splenectomy is indicated if in anemia or gallstones. Lifelong prophylactic penicillin is given post-splenectomy to prevent infections.
Frequently Asked Questions (FAQs)
What is the most common defect in hereditary spherocytosis?
The most common defect in hereditary spherocytosis is a deficiency in the spectrin protein. Spectrin is a crucial component of the red blood cell membrane, providing structural support and maintaining its normal biconcave shape. When spectrin is deficient or abnormal, the red blood cells become sphere-shaped, which makes them more susceptible to destruction by the spleen.
What four main complications can occur in patients with hereditary spherocytosis?
Hemolytic anemia: This is the most common complication, resulting from the premature destruction of red blood cells by the spleen. Symptoms include fatigue, weakness, shortness of breath, and pallor.
Splenomegaly: The spleen becomes enlarged due to its increased workload in destroying damaged red blood cells. This can cause abdominal discomfort, fullness, and sometimes pain.
Gallstones (Cholelithiasis): The breakdown of red blood cells releases bilirubin, which can accumulate in the gallbladder and form stones. This can lead to abdominal pain, nausea, and vomiting.
Aplastic crisis: In rare cases, patients with hereditary spherocytosis may experience a sudden decrease in red blood cell production, resulting in a severe form of anemia. This can require blood transfusions or other interventions.
What is the life expectancy of a person with hereditary spherocytosis?
The life expectancy of a person with hereditary spherocytosis can vary widely depending on the severity of the condition and the effectiveness of treatment.
In mild cases, individuals may experience few symptoms and have a normal life expectancy. However, in more severe cases, frequent blood transfusions or splenectomy (removal of the spleen) may be necessary, which can improve quality of life and extend survival.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Anemia: Diagnosis and Treatment (Willis, 2016).
- Management of Anemia: A Comprehensive Guide for Clinicians (Provenzano et al., 2018)
- Goldberg S, Hoffman J. Clinical Hematology Made Ridiculously Simple, 1st Edition: An Incredibly Easy Way to Learn for Medical, Nursing, PA Students, and General Practitioners (MedMaster Medical Books). 2021.



