TL;DR
Thrombosis are blood clots forming in blood vessels, blocking blood flow. It can occur in the veins (venous thrombosis) or arteries (arterial thrombosis).
What causes it? ▾
- Inherited factors (genetic mutations) – increase risk but not always a cause.
- Acquired factors (more common):
- Surgery and immobilization
- Cancer
- Pregnancy and postpartum period
- Inflammatory bowel disease (IBD)
- Infection
- Use of hormonal therapy (estrogen)
- Others (obesity, smoking, varicose veins)
What are the symptoms? ▾
- Often asymptomatic until a clot forms and blocks blood flow.
- Symptoms vary depending on the location of the clot:
- Deep Vein Thrombosis (DVT): Leg pain, swelling, redness, warmth.
- Pulmonary Embolism (PE): Sudden shortness of breath, chest pain, rapid heart rate, coughing (may bring up blood).
- Other types may have specific symptoms depending on the affected area.
How is it diagnosed? ▾
- Clinical suspicion by a healthcare professional is crucial.
- Various tests depending on the suspected type of thrombosis:
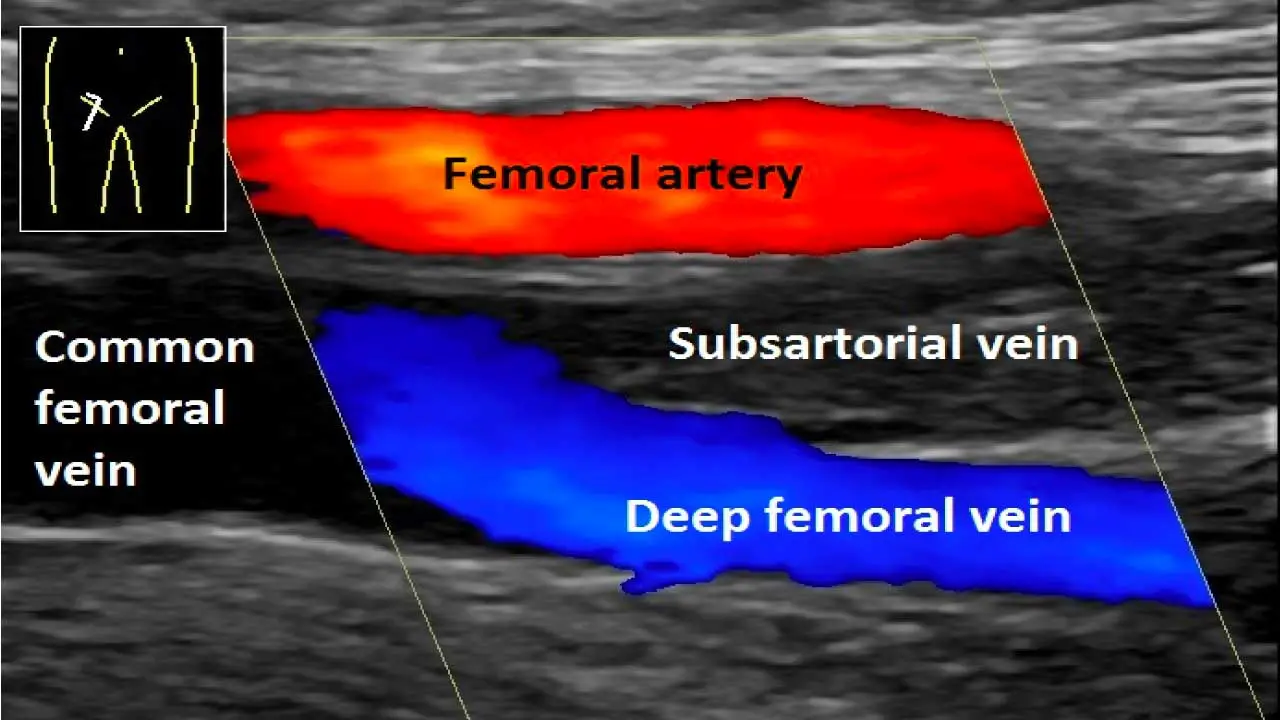
- Doppler ultrasound (DVT)
- Imaging tests (CT scan, V/Q scan) for PE
- Blood tests (D-dimer)
Why is early diagnosis important?
- Minimizes clot growth and risk of complications like breakaway clots (PE).
- Enables timely treatment to reduce long-term problems.
How is it treated? ▾
- Treating the existing clot
- Anticoagulant medications (blood thinners) – most common treatment.
- Clot busters (thrombolytics) – for severe cases.
- Preventing future clots
- Address underlying risk factors.
- Long-term anticoagulation therapy (in some cases).
- Compression stockings.
- Lifestyle modifications (diet, exercise).
*Click ▾ for more information
Introduction
Thrombosis refers to the formation of a blood clot (thrombus) inside a blood vessel. These clots can partially or completely block blood flow, leading to serious health consequences like tissue death, organ damage, and functional impairment. Sometimes, clots can break loose and travel through the bloodstream. If a clot lodges in a critical location like the lungs (pulmonary embolism) or brain (stroke), it can cause sudden death or permanent disability.
The formation of blood clots (thrombi) significantly contributes to the development of severe conditions like heart attacks (myocardial infarction), strokes (cerebrovascular disease), peripheral arterial disease (circulation problems in the legs), and deep vein thrombosis (blood clots in deep veins).
Normal Blood Clotting Process (Hemostasis)
Our bodies have a complex system called hemostasis that maintains a delicate balance between blood clotting and bleeding. The process of hemostasis includes:
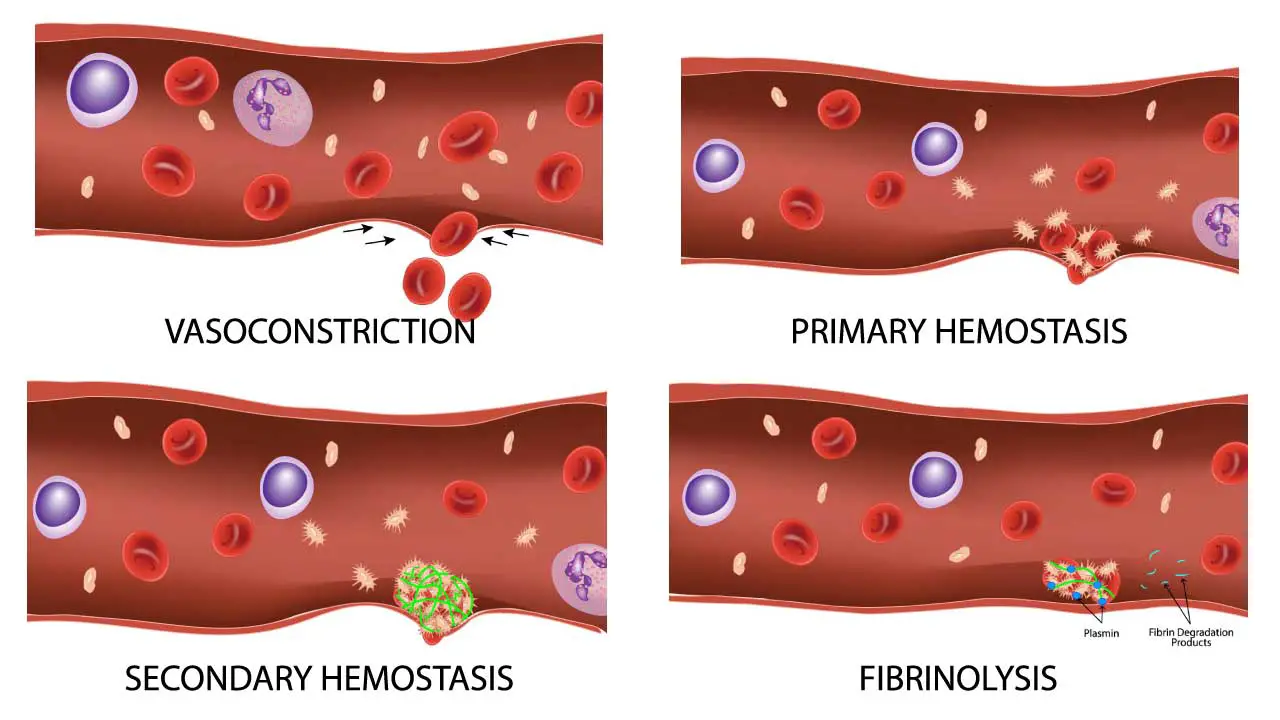
- Injury: When a blood vessel is damaged, platelets are activated and gather at the site.
- Platelet Plug: Platelets adhere to each other and the damaged vessel wall, forming a preliminary plug to stop immediate bleeding.
- Coagulation Cascade: A series of coagulation factors in the blood plasma are activated in a cascade-like fashion.
- Fibrin Formation: Fibrin, an insoluble protein mesh, is produced, trapping red blood cells and strengthening the platelet plug, forming a stable clot.
- Clot Resolution: Once the bleeding stops, the body activates another set of proteins to break down the clot and restore blood flow.
This finely tuned process ensures that bleeding is controlled after injury but doesn’t lead to unnecessary clot formation within intact vessels. Disruptions in this balance, either towards excessive clotting (thrombosis) or uncontrolled bleeding, can have serious health implications.
Causes of Thrombosis
Hereditary Disorders (Thrombophilia)
Inherited thrombophilia refers to a group of disorders where genetic mutations increase the risk of blood clot formation (thrombosis).
Factor V Leiden Mutation
- Cause: Factor V Leiden is caused by a mutation in the Factor V gene (F5). This gene provides instructions for creating Factor V, a protein that plays a crucial role in blood clotting. Normally, after a blood clot forms, another protein called protein C inactivates Factor V, preventing excessive clotting. However, the Factor V Leiden mutation alters the protein’s structure, making it resistant to inactivation by protein C. This increases the risk of blood clots forming and persisting longer than necessary.
- Characteristics:
- Increased Thrombosis Risk: Individuals with Factor V Leiden have a higher risk of developing blood clots, particularly deep vein thrombosis (DVT) and pulmonary embolism (PE).
- Incomplete Penetrance: Not everyone with the mutation will develop a clot. The risk depends on various factors like additional risk factors (surgery, pregnancy), lifestyle habits, and the specific type of mutation.
- Often Asymptomatic: Many individuals with Factor V Leiden don’t experience any symptoms until a triggering event (surgery, pregnancy) causes a clot to form.
- Family History: A family history of blood clots can increase the suspicion of Factor V Leiden.
- Symptoms: Often asymptomatic until a triggering event (surgery, pregnancy) causes a clot. These can vary depending on the location of the clot:
- Deep Vein Thrombosis (DVT): Leg pain, swelling, redness, and warmth.
- Pulmonary Embolism (PE): Sudden shortness of breath, chest pain, rapid heart rate, coughing (may bring up blood).
- Diagnosis: Blood test for Factor V Leiden mutation. This test is usually recommended for individuals with a personal or family history of blood clots, or those at high risk for thrombosis due to other factors (surgery, pregnancy).
- Treatment: Depends on risk factors. Anticoagulants like warfarin or newer medications like dabigatran or rivaroxaban, help prevent blood clots from forming or growing larger may be used for high-risk individuals or during high-risk periods (surgery, pregnancy). Use of compression stockings may help improve blood flow and reduce the risk of DVT and lifestyle modification could be recommended.
- Other considerations: Pregnant women with Factor V Leiden may require close monitoring and specific blood thinners to manage the increased risk of blood clots during pregnancy and postpartum.
Prothrombin Gene Mutation (G20210A)
- Cause: This mutation occurs in the gene that provides instructions for creating prothrombin, a protein essential for blood clotting. The mutation, located at position 20210 on the gene (hence the name G20210A), alters the protein’s structure. This altered prothrombin is more easily converted to its active form, thrombin, which drives clot formation. Consequently, individuals with this mutation have a higher tendency to form blood clots.
- Characteristics:
- Increased Thrombosis Risk: Similar to Factor V Leiden, individuals with the G20210A mutation have a higher risk of developing blood clots, particularly DVT and PE.
- Incomplete Penetrance: Not everyone with the mutation will experience a clot. The risk depends on various factors like additional risk factors (surgery, pregnancy), lifestyle habits, and the specific type of mutation.
- Often Asymptomatic: Many individuals with G20210A don’t experience any symptoms until a triggering event causes a clot to form.
- Family History: A family history of blood clots can increase the suspicion of this mutation.
- Symptoms: Similar to Factor V Leiden, often asymptomatic.
- Diagnosis: Blood test for the G20210A mutation.
- Treatment: Similar to Factor V Leiden, based on individual risk assessment.
Antithrombin Deficiency
- Cause: Antithrombin deficiency is an inherited blood disorder characterized by a lack of sufficient antithrombin, a critical protein that regulates blood clotting. Mutations in the SERPINC1 gene, responsible for antithrombin production, cause antithrombin deficiency. These mutations can be inherited from one or both parents. This deficiency weakens the body’s natural ability to break down clots, increasing the risk of blood clots forming and persisting.
- Characteristics:
- Increased Thrombosis Risk: Individuals with antithrombin deficiency have a significantly higher risk of developing blood clots, particularly DVT and PE.
- Severity Varies: The severity of the deficiency and the risk of thrombosis can vary depending on the specific mutation and the amount of antithrombin present.
- Early Onset: Unlike some other inherited thrombophilias, antithrombosis deficiency can cause blood clots at a younger age, even in childhood.
- Family History: A family history of blood clots, especially at a young age, can increase suspicion of antithrombin deficiency.
- Symptoms: May cause recurrent thrombosis at a young age, often with a family history. Similar to other clotting disorders, antithrombin deficiency is often asymptomatic until a clot forms. Symptoms then depend on the location of the clot.
- Diagnosis: Blood test to measure antithrombin levels.
- Treatment: Long-term anticoagulant therapy with medications like heparin or warfarin. For women with antithrombin deficiency and a history of blood clots related to hormonal changes (pregnancy, birth control pills), stopping HRT and considering alternative methods may be necessary. In some cases, medications to dissolve existing clots may be used, but these carry a higher risk of bleeding complications.
Protein C and S Deficiencies
- Cause: Protein S and C deficiency refers to a group of inherited disorders where deficiencies in either protein S or protein C, or both, increase the risk of blood clots. These proteins play a vital role in the body’s natural anticoagulation system, working together to regulate clot formation and breakdown. Mutations in the respective genes, PROS1 for Protein S and PROC for Protein C, are responsible for these deficiencies. These mutations can be inherited from one or both parents.
- Characteristics:
- Increased Thrombosis Risk: Individuals with protein S or C deficiency have a significantly higher risk of developing blood clots, particularly DVT and PE.
- Severity Varies: The severity of the deficiency and the risk of thrombosis can vary depending on the specific mutation, the protein affected (S or C), and the degree of deficiency.
- Early Onset: Similar to antithrombin deficiency, protein S or C deficiency can cause blood clots at a younger age, even in childhood.
- Family History: A family history of blood clots, especially at a young age, can increase suspicion of protein S or C deficiency.
- Symptoms: As with other clotting disorders, protein S or C deficiency is often asymptomatic until a clot forms. Symptoms then depend on the location of the clot.
- Diagnosis: Blood tests to measure Protein C and S levels.
- Treatment: Anticoagulant therapy, with options depending on individual needs and severity. For women with protein S or C deficiency and a history of blood clots related to hormonal changes (pregnancy, birth control pills), stopping HRT and considering alternative methods may be necessary. In some severe cases, protein S or C concentrates may be used to supplement the deficient protein. In others, medications to dissolve existing clots may be used, but these carry a higher risk of bleeding complications.
Hyperhomocysteinemia
- Cause: Hyperhomocysteinemia refers to a condition where you have abnormally high levels of homocysteine, an amino acid, in your blood. While homocysteine is a natural byproduct of protein metabolism, elevated levels are associated with an increased risk of various health problems, including blood clots.There are two main causes of hyperhomocysteinemia:
- Genetic Defects: Mutations in genes involved in homocysteine metabolism can lead to its buildup in the blood. This is a less common cause.
- Dietary Deficiencies: Deficiencies in vitamins B6, B12, and folic acid are the most common cause. These vitamins are essential for processing homocysteine and converting it to other compounds.
- Characteristics:
- Elevated Homocysteine Levels: The defining feature is having homocysteine levels exceeding 15 micromoles per liter (µmol/L) of blood.
- Often Asymptomatic: In many cases, hyperhomocysteinemia itself doesn’t cause any noticeable symptoms.
- Increased Risk of Blood Clots: Elevated homocysteine levels are associated with an increased risk of developing blood clots, particularly DVT and PE.
- May Contribute to Other Conditions: Some research suggests a link between hyperhomocysteinemia and an increased risk of heart disease, stroke, and certain types of dementia. However, the exact cause-and-effect relationship is still under investigation.
- Symptoms: Since hyperhomocysteinemia is often asymptomatic, symptoms may not be present unless a related health condition develops, such as a blood clot or cardiovascular issue.
- Diagnosis: Blood test to measure homocysteine levels.
- Treatment: Treatment for hyperhomocysteinemia aims to lower homocysteine levels and potentially reduce the associated health risks.
- Vitamin Supplementation: If dietary deficiencies are the cause, supplementing with vitamin B6, B12, and folic acid can significantly lower homocysteine levels.
- Lifestyle Modifications: Maintaining a healthy diet rich in fruits, vegetables, and whole grains can help ensure adequate vitamin intake.
- Medications: In some cases, depending on the severity and cause, specific medications may be used to lower homocysteine levels.
Others
- Fibrinogen Disorders: Abnormal fibrinogen (the protein that forms the clot structure) can increase clot formation risk.
- Thrombomodulin Deficiency: This protein regulates clot formation on the surface of endothelial cells lining blood vessels. Deficiency can increase clot risk.
Acquired Disorders
While inherited factors can increase the risk of blood clots (thrombosis), several acquired conditions can also significantly contribute. Acquired causes of thrombosis rarely occur in isolation. The risk of thrombosis increases significantly when multiple acquired factors are present. A combination of factors like surgery and obesity can significantly increase the risk.
Surgery and Immobilization
- Cause: Surgery, particularly major procedures, disrupts the normal blood flow and can cause tissue damage, both of which increase clot formation risk. Additionally, prolonged periods of inactivity (e.g., bed rest after surgery, long plane flights) can lead to blood stasis (slow flow) in veins, facilitating clot formation.
- Symptoms: May not cause any symptoms until a clot forms (DVT: leg pain, swelling, redness; PE: sudden shortness of breath, chest pain, rapid breathing).
- Diagnosis: Doppler ultrasound, D-dimer blood test (measures clot breakdown products) to detect DVT. Imaging tests (chest X-ray, CT scan) may be used for suspected PE.
- Treatment: Early mobilization, compression stockings, and anticoagulant medications to prevent clot formation or growth.
Cancer
- Cause: Cancer cells can release substances that activate clotting mechanisms and damage blood vessel walls, increasing the risk of clots. Additionally, some cancer treatments (chemotherapy) can further elevate the risk.
- Symptoms: Similar to surgery and immobilization, symptoms may not appear until a clot forms.
- Diagnosis: Similar diagnostic tests as above may be used, along with tests to identify the underlying cancer.
- Treatment: Depends on the type of cancer and the presence of clots. Anticoagulant medications, catheter-directed therapies to remove clots, and addressing the underlying cancer are important aspects of management.
Pregnancy and Postpartum Period
- Cause: Hormonal changes during pregnancy and the postpartum period increase clotting factors in the blood, raising the risk of thrombosis. Additionally, increased blood volume and pressure on veins in the pelvis further contribute.
- Symptoms: Similar to above-mentioned scenarios.
- Diagnosis: Similar diagnostic tests are used, with adjustments for pregnancy considerations.
- Treatment: Low-dose anticoagulant medications specifically chosen for safety during pregnancy and breastfeeding are often used. Compression stockings and early mobilization are also crucial.
Inflammatory Bowel Disease (IBD)
- Cause: Chronic inflammation associated with IBD can damage blood vessel walls and increase levels of clotting factors, promoting clot formation.
- Symptoms: Symptoms of IBD (abdominal pain, diarrhea, rectal bleeding) might overshadow initial clot symptoms.
- Diagnosis: Tests to diagnose IBD (colonoscopy, blood tests) combined with tests to detect clots as needed.
- Treatment: Management of IBD to control inflammation, along with anticoagulant medications to prevent clots.
Infection
- Cause: The body’s inflammatory response to infection can activate clotting mechanisms, increasing the risk of thrombosis.
- Symptoms: Symptoms of the underlying infection might be prominent, and clot symptoms may not be readily apparent.
- Diagnosis: Tests to identify the specific infection along with tests for DVT/PE, if suspected.
- Treatment: Treatment of the underlying infection with antibiotics or other medications, along with potential use of anticoagulants depending on the severity of the infection and clot risk.
Use of Hormonal Therapy (Estrogen)
- Cause: Hormonal therapy, particularly with estrogen-containing medications (birth control pills, hormone replacement therapy for menopause), can increase the risk of thrombosis.
- Symptoms: Similar to other scenarios.
- Diagnosis: Evaluation of risk factors and potential clot symptoms, followed by diagnostic tests as needed.
- Treatment: Depending on individual needs and risk factors, alternative hormonal therapy options without estrogen or discontinuation of hormonal therapy altogether might be considered. Anticoagulant medications may be used if a clot is present.
Other Acquired Causes
- Obesity: Excess weight can increase pressure on veins and contribute to blood stasis, promoting clots.
- Smoking: Damages blood vessel walls and increases clotting factors, raising the risk of thrombosis.
- Varicose Veins: Weakened and enlarged veins can lead to blood pooling and clot formation.
- Central Venous Catheters: These devices used for medication delivery can irritate the vein wall and increase clot risk.
- Certain Medications: Some medications, like some anti-seizure drugs, can increase the risk of blood clots.
Characteristics of Different Thrombotic Events
Arterial Vs Venous Thrombosis
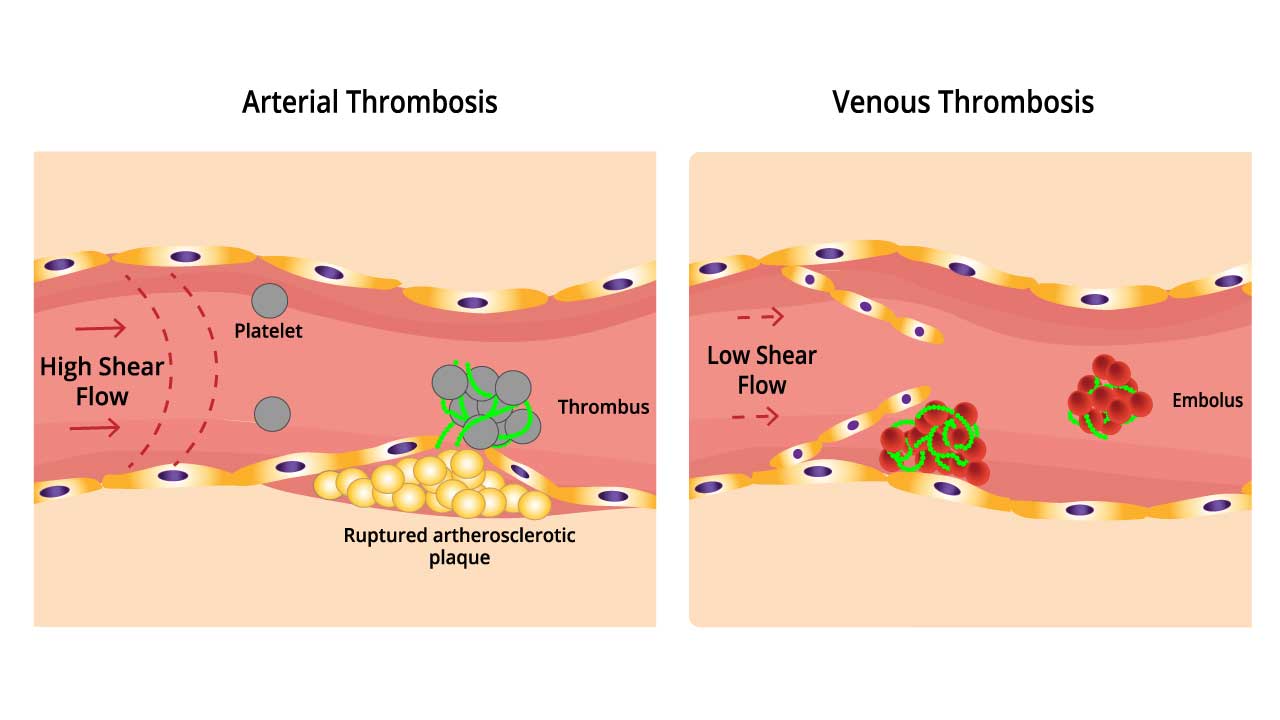
Thrombosis, the formation of blood clots within blood vessels, can occur in either arteries or veins. While both are serious conditions, they differ significantly in their characteristics, causes, and consequences.
| Feature | Arterial Thrombosis | Venous Thrombosis |
| Pathogenesis (Clot Formation) | Primarily driven by atherosclerosis; plaque rupture triggers platelet aggregation and clot formation. High blood pressure and inflammation contribute. | Initiated by Virchow’s Triad: Endothelial damage, Venous stasis, Hypercoagulability |
| Main Risk Factors | Age, High blood pressure, High cholesterol, Diabetes, Smoking, Family history of heart disease/stroke | Age, High blood pressure, Smoking, Surgery, Immobilization, Pregnancy, Hormonal therapy (estrogen), Obesity, Chronic inflammatory conditions (IBD), Certain cancers |
| Clot Composition | Rich in platelets (whitish appearance). Often form at sites of atherosclerotic plaques in arteries with high blood flow. | Predominantly red blood cells and fibrin (reddish appearance). Develop in veins with slower blood flow. |
| Location | Arteries supplying vital organs (heart, brain, kidneys, legs) | Deep veins of the legs (DVT) |
| Consequences | Reduced blood flow to organs, myocardial infarction (heart attack), stroke, peripheral arterial disease | Leg pain, swelling, skin discoloration, pulmonary embolism (PE) |
| Treatment | Anticoagulants, thrombolytic therapy (clot busters) in some cases, minimally invasive clot removal procedures | Anticoagulants, thrombolytic therapy in some cases |
| Prevention | Healthy lifestyle (diet, exercise, weight management), manage blood pressure/cholesterol, smoking cessation | Early mobilization after surgery, compression stockings, address underlying risk factors (obesity, inflammation) |
Virchow’s Triad:
- Endothelial damage: Injury to the vein wall exposes underlying tissues, promoting platelet activation and clot formation.
- Venous stasis: Slow blood flow in veins, particularly during prolonged sitting or immobilization, allows clotting factors to interact and form clots.
- Hypercoagulability: Increased tendency of the blood to clot, often due to inherited factors, hormonal changes, or inflammatory conditions.
Blood clots (thrombi) can form in various parts of the circulatory system, leading to different conditions with distinct characteristics.
Deep Vein Thrombosis (DVT)

- Location: Blood clots form in deep veins, typically in the legs (thighs, calves).
- Symptoms:
- Leg pain, often described as a cramping or aching sensation.
- Swelling in the affected leg.
- Redness or discoloration of the skin.
- Warmth to the touch.
- In some cases, no noticeable symptoms may be present.
- Diagnosis: Doppler ultrasound is the primary diagnostic tool to assess blood flow and identify clots in deep veins.
- Treatment:
- Anticoagulant medications to prevent further clot growth and new clot formation.
- Compression stockings to improve blood flow in the legs.
- In some cases, medications to dissolve existing clots (thrombolytic therapy) may be used.
Pulmonary Embolism (PE)
- Location: A blood clot breaks off from a DVT (most common) or forms elsewhere in the body and travels through the bloodstream to lodge in the arteries of the lungs.
- Symptoms:
- Sudden shortness of breath, often described as coming on at rest or with minimal exertion.
- Chest pain, sharp or stabbing, that may worsen with deep breaths or coughing.
- Rapid heart rate.
- Coughing, may bring up blood in some cases.
- Anxiety or sweating.
- Diagnosis: Imaging tests like CT scan with pulmonary angiography or V/Q scan are used to visualize blood flow in the lungs and identify blockages caused by the clot.
- Treatment:
- Urgent administration of anticoagulant medications to prevent further clot growth and potentially dissolve the existing clot.
- Oxygen therapy to improve oxygen delivery if blood oxygen levels are low.
- In some cases, clot removal procedures using catheters may be necessary.
Superficial Thrombophlebitis
- Location: Blood clots form in superficial veins located just beneath the skin’s surface, often in the legs.
- Symptoms:
- Redness, tenderness, and swelling along the affected vein.
- A hardened cord-like feeling along the vein.
- In some cases, mild pain or burning sensation in the area.
- Diagnosis: Physical examination and ultrasound may be used to confirm the location and extent of the clot.
- Treatment:
- Compression stockings to improve blood flow and reduce swelling.
- Over-the-counter pain relievers for discomfort.
- In some cases, topical medications or antibiotics may be used depending on the cause.
Cerebral Venous Thrombosis (CVT)
- Location: Blood clots form in the dural sinuses or veins draining blood from the brain.
- Symptoms:
- Headache (often described as the worst headache of your life)
- Seizures
- Loss of vision or blurred vision
- Weakness or paralysis on one side of the body
- Difficulty speaking or understanding speech
- Confusion or decreased alertness
- Diagnosis: Imaging tests like MRI scan with venography are used to visualize blood flow in the brain and identify blockages caused by the clot.
- Treatment:
- Urgent administration of anticoagulant medications to prevent further clot growth and potentially dissolve the existing clot.
- In some cases, clot removal procedures using catheters may be necessary.
Mesenteric Ischemia
- Location: Blood clots form in the arteries supplying blood to the intestines.
- Symptoms:
- Severe abdominal pain, often described as constant and worsening.
- Nausea and vomiting.
- Diarrhea or bloody stools.
- Abdominal distention (swelling).
- Diagnosis: Imaging tests like CT angiography or angiography are used to visualize blood flow in the abdominal arteries and identify blockages caused by the clot.
- Treatment:
- Emergency surgery to remove the clot and restore blood flow to the intestines.
- Anticoagulant medications to prevent further clot formation.
Additional Thrombotic Events
- Splanchnic Vein Thrombosis (SVT): Blood clot in a vein draining the abdominal organs (liver, spleen, intestines).
- Renal Vein Thrombosis (RVT): Blood clot in a vein draining the kidney.
- Superior Mesenteric Venous Thrombosis (SMVT): Blood clot in a vein draining the small intestine.
Diagnosis of Thrombosis
Diagnosing a blood clot (thrombosis) involves a combination of clinical suspicion, patient history, physical examination, and various diagnostic tools.
Clinical Suspicion
- A healthcare professional plays a crucial role in suspecting thrombosis based on the patient’s symptoms and risk factors.
- Common symptoms suggestive of thrombosis can vary depending on the location of the clot.
- Risk factors like recent surgery, immobilization, pregnancy, personal or family history of blood clots, and certain medical conditions (cancer, inflammatory bowel disease) increase suspicion.
Patient History and Physical Examination
- A detailed discussion about symptoms, duration, and any potential risk factors is crucial.
- The physical examination focuses on areas where clots commonly occur (legs for DVT, lungs for PE).
Blood Tests
- D-dimer: A protein marker elevated in most, but not all, cases of thrombosis. A negative result can often help rule out thrombosis, but a positive result requires further investigation.
- Complete blood count: May show abnormalities suggestive of infection or inflammation.
- Coagulation tests: May be used to evaluate underlying clotting disorders.
Diagnostic Tools
Several tools aid in diagnosing thrombosis, depending on the suspected location and severity.
| Diagnostic Tool | Type of Thrombosis Typically Used For | Advantages | Disadvantages |
| Doppler Ultrasound | Deep Vein Thrombosis (DVT) | Non-invasive, painless, readily available, good for assessing blood flow | May not be conclusive in all cases |
| Venography (X-ray with contrast dye) | DVT, sometimes PE | Provides detailed visualization of veins | Invasive, involves radiation exposure, potential for allergic reaction to contrast dye |
| Ventilation-perfusion (V/Q) Scan | Pulmonary Embolism (PE) | Non-invasive, relatively safe | May not be definitive, can be inconclusive |
| CT scan with pulmonary angiography | PE | Detailed images of lungs and blood vessels, more definitive than V/Q scan | Involves radiation exposure, contrast dye injection |
| Imaging Tests (CT scan, MRI) | Cerebral Venous Thrombosis (CVT), Mesenteric Ischemia | Provide detailed views of the brain, abdomen, or intestines | May require contrast dye, radiation exposure (CT scan) |
Importance of Clinical Suspicion and Prompt Diagnosis
Early diagnosis and treatment of thrombosis are crucial for several reasons:
- Minimizing Clot Growth: Prompt intervention prevents the clot from enlarging, reducing the risk of complications.
- Preventing Breakaway Clots: Early treatment can help prevent a piece of the clot from breaking off and traveling to other organs (e.g., PE).
- Reducing Long-Term Complications: Early treatment can minimize the risk of long-term complications like chronic leg pain, swelling (post-thrombotic syndrome), or permanent organ damage.
Treatment of Thrombosis
The general treatment of thrombosis focuses on two main goals:
- Treating the Existing Clot: This aims to prevent the clot from growing further, dissolving existing clots (in some cases), and minimizing the risk of complications.
- Preventing Future Blood Clots: This involves addressing underlying risk factors and using medications to prevent new clots from forming.
Here’s a breakdown of the common treatment approaches for thrombosis:
Anticoagulant Medications (Blood Thinners)
These medications are the mainstay of treatment for most types of thrombosis. They work by interfering with the blood clotting cascade, preventing new clots from forming and promoting the breakdown of existing ones (depending on the medication).
Common types include warfarin (Coumadin), newer oral anticoagulants (dabigatran, rivaroxaban, apixaban), and injectable medications (enoxaparin, heparin). The specific type, dose, and duration of treatment will depend on the severity and location of the clot, as well as individual risk factors.
Clot Busters (Thrombolytics)
In some cases, medications like alteplase (tissue plasminogen activator) can be used to dissolve existing clots. These are typically used for severe PE or large clots in critical areas where rapid intervention is necessary. Due to the increased risk of bleeding, they are not suitable for everyone and require careful evaluation by a healthcare professional.
Compression Stockings
These specialized stockings apply graduated pressure to the legs, helping to improve blood flow and reduce swelling. They are particularly beneficial in treating and preventing DVT.
Catheter-Directed Interventions
In some cases, minimally invasive procedures using catheters may be used to remove or bypass a clot. This is an option for specific types of thrombosis, such as large clots in major veins or arteries.
Surgery
In rare cases, surgery may be necessary to remove a large clot or repair damaged blood vessels.
Addressing Underlying Risk Factors
Identifying and managing underlying conditions that increase the risk of thrombosis is crucial for long-term prevention. This may involve weight management, smoking cessation, managing high blood pressure, or controlling diabetes.
Lifestyle Modifications
Maintaining a healthy lifestyle with regular exercise, a balanced diet, and adequate hydration can significantly reduce the risk of future blood clots.
Frequently Asked Questions (FAQs)
What is the most common cause of thrombosis?
While inherited factors can elevate thrombosis risk, the most common cause lies in acquired conditions. This includes situations like surgery and prolonged immobility, where blood flow is compromised. Additionally, pregnancy, certain cancers, and even common infections can increase clotting factors or damage blood vessel walls, creating the perfect storm for clot formation.
What are the signs of thrombosis?
Thrombosis often goes unnoticed, but potential signs include leg pain, swelling, redness, and warmth, especially in the calf. However, sudden shortness of breath, chest pain, and rapid breathing could indicate a life-threatening complication (pulmonary embolism) and require immediate medical attention.
Is thrombosis life threatening?
Thrombosis itself isn’t necessarily life-threatening, but a potential complication called pulmonary embolism (PE) can be. PE occurs when a blood clot breaks off and travels to the lungs, blocking blood flow. This can lead to sudden shortness of breath, chest pain, and rapid breathing, and can be fatal if not treated promptly.
Can thrombosis go away?
Yes, thrombosis can go away! The body naturally has mechanisms to break down clots, and with proper treatment like blood thinners, most clots can be dissolved or prevented from growing further. Early intervention is key, and depending on the size and location of the clot, it can take weeks or even months for the clot to fully dissolve.
How to avoid thrombosis?
Here are some ways to avoid thrombosis:
- Move frequently: Get up and walk around every few hours, especially after sitting for long periods (e.g., on a plane or at work).
- Wear compression stockings: These can improve blood flow in your legs, especially if you’re at high risk for thrombosis.
- Maintain a healthy weight: Excess weight puts extra strain on your veins.
- Stay hydrated: Drink plenty of fluids throughout the day to keep your blood from becoming too thick.
- Eat a healthy diet: Choose a diet rich in fruits, vegetables, and whole grains, and limit unhealthy fats and processed foods.
- Don’t smoke: Smoking damages blood vessel walls and increases your risk of clots.
- Manage chronic conditions: If you have a condition like high blood pressure or diabetes, keeping it under control can help reduce your risk of thrombosis.
- Talk to your doctor about hormone therapy: If you’re considering hormone replacement therapy (HRT), discuss the risks and benefits with your doctor, especially if you have other risk factors for thrombosis.
- Be aware of your risk factors: If you have a family history of thrombosis or a medical condition that increases your risk, talk to your doctor about additional preventive measures.
How do they remove blood clots from legs?
There are several methods for removing blood clots from legs, depending on the size, location, and severity of the clot.
- Medications (Anticoagulants): This is the most common approach. Blood thinners like warfarin or newer medications (dabigatran, rivaroxaban) prevent new clots from forming and can help dissolve existing small or medium-sized clots over time.
- Clot Busters (Thrombolytics): In severe cases with large clots or if the clot is causing significant tissue damage, medications like alteplase can be used to dissolve the clot more rapidly. However, due to the increased risk of bleeding, this approach requires careful evaluation and isn’t suitable for everyone.
- Catheter-Directed Interventions: For specific cases involving large clots in major veins, minimally invasive procedures using catheters may be used. A catheter is inserted into a vein and used to remove the clot or create a new pathway for blood flow around the clot (mechanical thrombectomy).
- Surgery (Thrombectomy): In rare cases, surgery might be necessary to remove a large clot if other methods are not feasible. This is typically done when the clot is life-threatening or causing severe tissue damage.
Can thrombosis cause a stroke?
Yes, thrombosis can cause a stroke. When a blood clot forms in an artery supplying blood to the brain (cerebral thrombosis), it can block blood flow and oxygen delivery, leading to stroke symptoms like weakness, numbness, or speech difficulties. This is different from a hemorrhagic stroke caused by bleeding in the brain, but both highlight the importance of managing thrombosis risk to prevent serious complications.
Can thrombosis cause headaches?
Thrombosis can cause headaches in some cases, particularly cerebral venous thrombosis (CVT) where a clot forms in a vein draining blood from the brain. This can lead to headaches that are often severe and persistent, along with other neurological symptoms like vision problems, seizures, or weakness. However, a headache alone isn’t a specific sign of thrombosis, and other causes should be considered.
Should peroneal vein thrombosis be treated?
Absolutely, Peroneal vein thrombosis (PVT) should be treated to prevent complications. While PVT itself may not cause immediate problems, the clot can travel to larger veins and create a pulmonary embolism (PE) which can be life-threatening. Early diagnosis and treatment with blood thinners and compression stockings can prevent this and ensure proper clot resolution.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Saba HI, Roberts HR. Hemostasis and Thrombosis: Practical Guidelines in Clinical Management (Wiley Blackwell). 2014.
- DeLoughery TG. Hemostasis and Thrombosis 4th Edition (Springer). 2019.
- Keohane EM, Otto CN, Walenga JM. Rodak’s Hematology 6th Edition (Saunders). 2019.
- Kaushansky K, Levi M. Williams Hematology Hemostasis and Thrombosis (McGraw-Hill). 2017.



