TL;DR
The spleen is a vital organ for immunity and blood filtration.
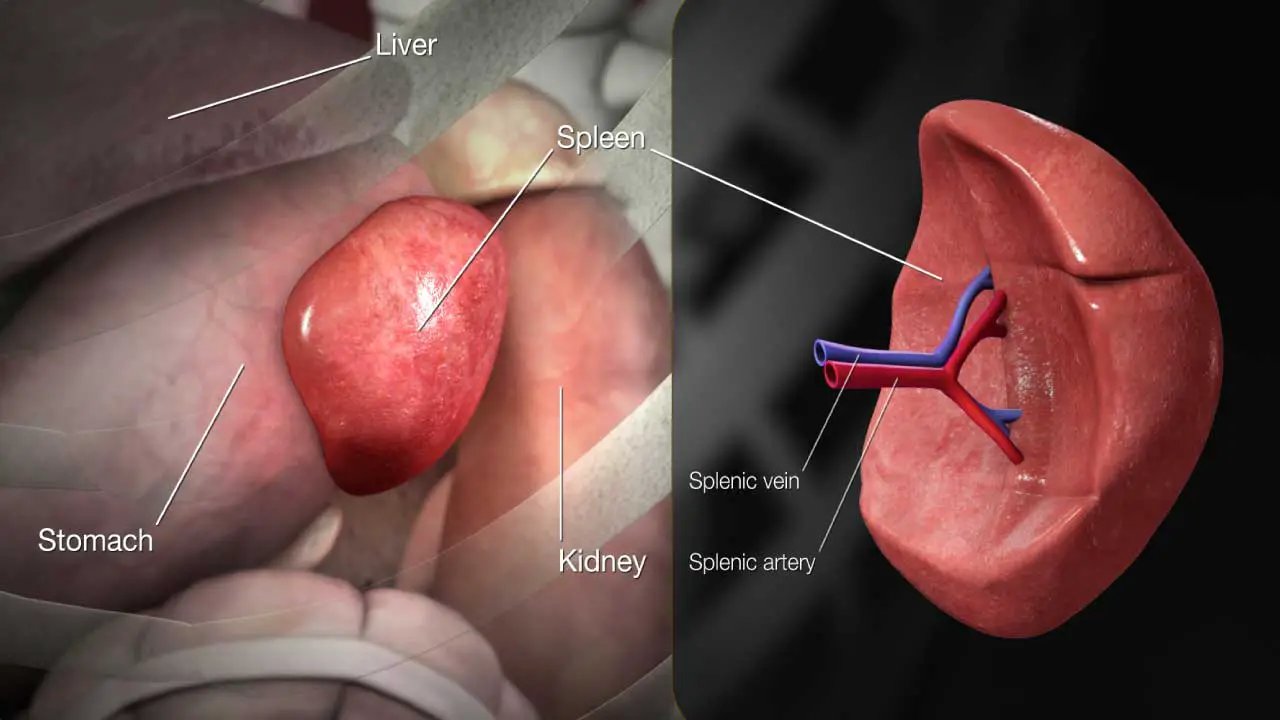
Location ▾: Upper left quadrant of the abdomen, under the rib cage, near the stomach, left kidney, and diaphragm.
- Capsule and trabeculae provide support.
- White pulp (lymphatic tissue) surrounds arteries and is key for immune responses (PALS is a key component).
- Red pulp filters blood, removes old/damaged red blood cells, and stores blood cells. Contains splenic cords and sinuses.
- Immune: Filters blood, fights infections, produces antibodies.
- Hematopoietic: Produces red blood cells in the fetus, recycles iron, stores blood.
- Enlargement of the spleen, caused by infections, liver disease, blood disorders, etc.
- Symptoms include left upper abdominal pain/fullness, feeling full quickly, fatigue, frequent infections, easy bleeding.
- Diagnosed via physical exam, imaging (ultrasound, CT, MRI), and blood tests.
- Usually caused by stretching of the capsule due to splenomegaly, rupture (emergency), infarction (blocked blood supply), or abscess.
- Diagnosed similarly to splenomegaly.
- Treatment depends on the cause; may include medications, pain management, or splenectomy (spleen removal).
*Click ▾ for more information
Introduction
The spleen is a vital organ located in the upper left side of the abdomen. It plays a crucial role in the body’s immune system and blood filtration. It acts as a filter, removing old, damaged, or abnormal red blood cells from circulation. Additionally, it helps produce antibodies to fight infection and stores white blood cells, platelets, and red blood cells.
Functions of the Spleen
The spleen is part of the lymphatic system, which is part of the immune system. The spleen has several important functions.
Immune function
- Filtering blood: The spleen filters blood, removing old or damaged red blood cells and removing pathogens, such as bacteria and viruses.
- Fighting infection: The spleen contains white blood cells (i.e. lymphocytes and macrophages) that help fight infection.
- Producing antibodies: The spleen produces antibodies, which are proteins that help fight infection.
Hematopoietic function
- Storing blood: The spleen stores blood and releases it into the bloodstream when needed. This can be important in cases of blood loss or injury.
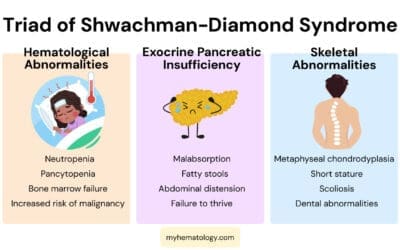
- Producing blood cells: In a developing fetus, the spleen produces red blood cells. After birth, this function is taken over by the bone marrow. However, the spleen can resume producing red blood cells if the bone marrow is damaged. This is called extramedullary hematopoiesis.
- Recycling iron: The spleen recycles iron from old red blood cells.
Structure
The spleen is a complex organ with a unique structure that enables it to perform its vital functions. The spleen is enclosed by a fibroelastic capsule, which is a layer of connective tissue that provides support and protection. The capsule is relatively thin, allowing the spleen to expand and contract as needed. The trabeculae which are extensions of the capsule project into the spleen’s interior, dividing it into compartments. The trabeculae provide structural support and carry blood vessels and nerves.
Within the spleen, the parenchyma is the functional tissue of the spleen where two main types of tissue are found.
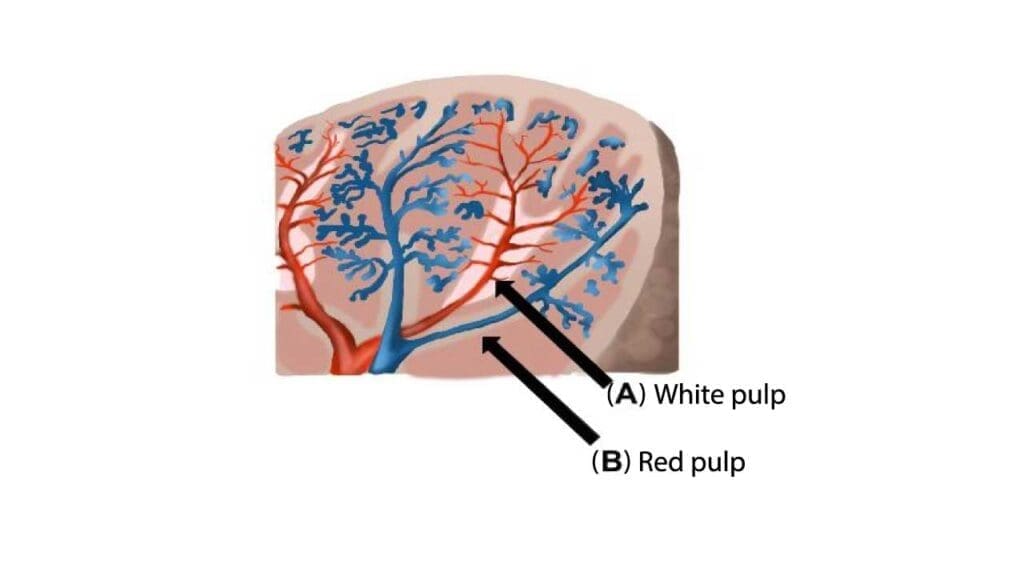
White Pulp
This is lymphatic tissue that surrounds arteries within the spleen. It appears as whitish nodules scattered throughout the spleen. It is composed mainly of lymphocytes (B and T cells) and macrophages and is responsible for the spleen’s immune functions.
The white pulp is organized into two main structures:
- Lymphoid follicles: They are located between the periarteriolar lymphoid sheaths (PALS) and the marginal zone (MZ). There are two types of lymphoid follicles: primary follicles and secondary nodules. Primary follicles are made up of small, immature lymphocytes, while secondary nodules are formed when primary follicles mature and increase in size. Lymphoid follicles are rich in B cells, which are responsible for producing antibodies. The germinal center in secondary nodules is where lymphocytes mature and acquire the ability to produce antibodies. The spleen reacts to antigens by releasing macrophages. The lymphoid follicles in the spleen play a key role in the immune response against foreign particulates.
- Periarteriolar lymphoid sheaths (PALS): Periarteriolar lymphoid sheaths (PALS) are cylindrical structures in the spleen’s white pulp that are made up of tightly packed T-cells and surround the spleen’s central arteries. These arteries are branches of the splenic artery that enter the spleen at the hilum. Within the PALS, T cells are organized into distinct zones, with different subsets of T cells residing in specific areas. The PALS provides a site for immune surveillance, where T cells can encounter antigens (foreign substances) present in the blood. As blood flows through the central arteries, antigens are captured by specialized cells called dendritic cells, which then present these antigens to T cells within the PALS. When T cells recognize an antigen, they become activated and initiate an immune response.
Red Pulp
The red pulp is a spongy tissue in the spleen that filters blood and removes waste, such as old or damaged red blood cells, bacteria, and viruses. It makes up the majority of the spleen’s volume.
The red pulp has a unique structure that facilitates its filtering function.
- Splenic cords (of Billroth): Also known as connective tissue, these cords contain many types of blood cells, including red blood cells, platelets, granulocytes, and plasma.
- Splenic sinuses: These are specialized blood vessels with wide lumens and discontinuous walls. They are lined by unique endothelial cells that allow blood cells to pass through easily.
In addition to these tissues, the spleen also contains blood vessels and nerves.
- Blood Vessels: The splenic artery supplies blood to the spleen, branching into smaller vessels within the organ. Blood exits the spleen through the splenic vein.
- Nerves: The spleen is innervated by the celiac plexus, which provides sympathetic and parasympathetic nerve fibers.
Location of the Spleen
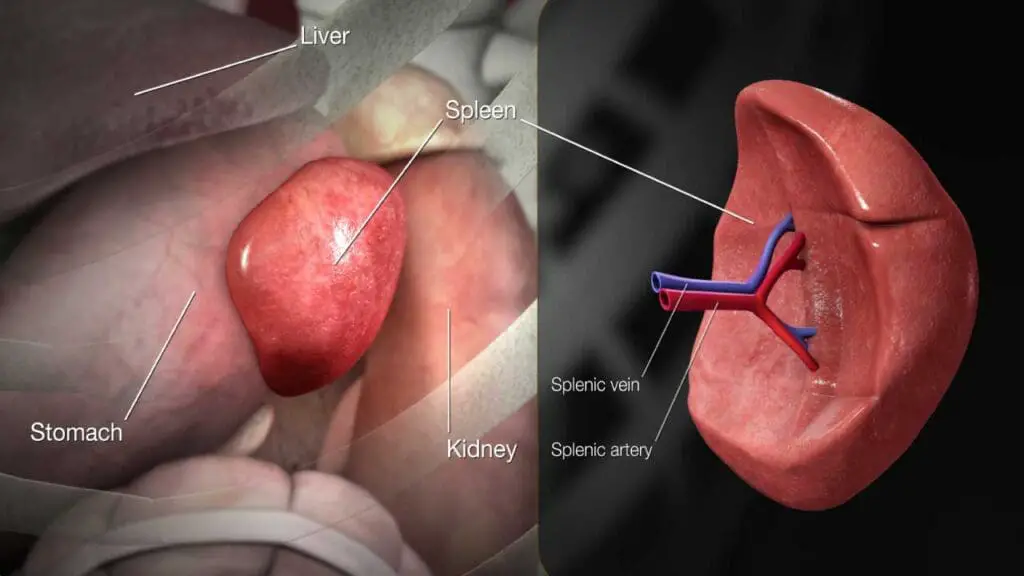
The spleen is located in the upper left quadrant (ULQ) of the abdomen, nestled under the rib cage and diaphragm.
Anatomical Position of the Spleen
The spleen resides in the left hypochondriac region of the abdomen, which is the upper left portion of the abdominal cavity. It is well-protected by the rib cage, specifically the 9th to 11th ribs, making it difficult to palpate (feel) in a healthy individual.
The spleen’s long axis lies along the 10th rib, with its upper pole pointing posteriorly, superiorly, and medially, and its lower pole pointing anteriorly, inferiorly, and laterally.
Relationship to Other Organs
The spleen’s location brings it into close proximity with several important organs.
- Stomach: The spleen lies posterior and lateral to the stomach. The anterior surface of the spleen is related to the posterior wall of the stomach. The splenic artery runs along the superior border of the pancreas and reaches the spleen by passing through the lienorenal ligament (a peritoneal fold connecting the spleen to the left kidney).
- Left Kidney: The spleen is located superior and lateral to the left kidney. The medial surface is related to the upper part of the left kidney. The lienorenal ligament also contains the splenic vein, which drains blood from the spleen and empties into the portal vein.
- Diaphragm: The spleen lies inferior to the diaphragm, the large muscle that separates the chest cavity from the abdominal cavity. The diaphragmatic surface of the spleen is convex and fits snugly against the undersurface of the diaphragm. This close relationship explains why spleen injuries can sometimes cause referred pain to the left shoulder (Kehr’s sign) due to irritation of the diaphragm.
- Left Colic Flexure: The spleen’s inferior border rests on the left colic flexure, which is the sharp bend in the colon where the transverse colon becomes the descending colon.
- Pancreas: The tail of the pancreas is located close to the spleen’s hilum (the region where blood vessels and nerves enter and exit the spleen).
Splenomegaly
Splenomegaly is defined as the enlargement of the spleen measured by size or weight.
Common Causes of Splenomegaly
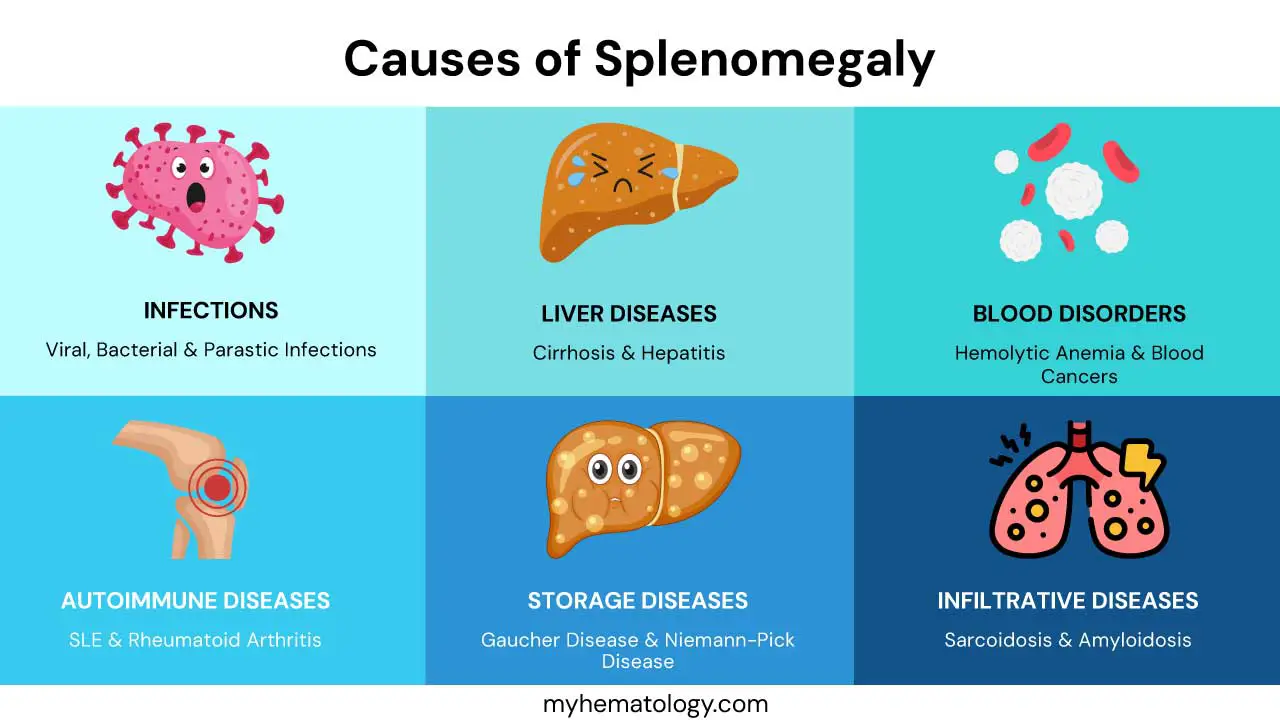
Splenomegaly can arise from a variety of underlying conditions.
Infections
- Viral infections
- Mononucleosis (Epstein-Barr virus): This is a very common cause of splenomegaly, particularly in adolescents and young adults.
- Cytomegalovirus (CMV)
- HIV
- Bacterial infections
- Endocarditis: Infection of the inner lining of the heart can spread to the spleen.
- Tuberculosis: This bacterial infection can affect various organs.
- Syphilis: A sexually transmitted infection that can cause splenomegaly in its later stages.
- Parasitic infections
- Malaria: A mosquito-borne parasitic disease that can cause significant splenomegaly.
- Leishmaniasis
- Toxoplasmosis
Liver Diseases
- Cirrhosis: This chronic liver disease can cause portal hypertension, which is increased pressure in the portal vein that carries blood from the digestive organs to the liver. This increased pressure can lead to blood backing up into the spleen, causing it to enlarge.
- Hepatitis: Chronic hepatitis B or C infections can also lead to cirrhosis and subsequently splenomegaly.
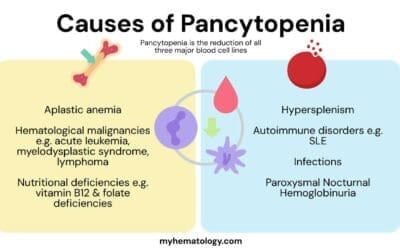
Blood Disorders
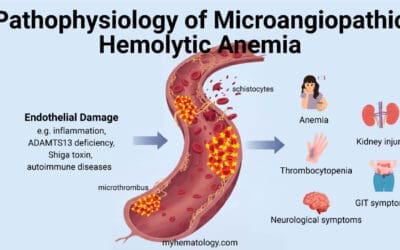
- Hemolytic anemias: These are conditions in which red blood cells are destroyed prematurely. The spleen works harder to remove these damaged cells, leading to splenomegaly. Examples include:
- Blood cancers
Other Conditions
- Autoimmune diseases
- Systemic lupus erythematosus (SLE): A chronic autoimmune disease that can affect various organs.
- Rheumatoid arthritis: An autoimmune disease that primarily affects the joints but can also cause splenomegaly.
- Storage diseases: These are genetic disorders in which certain substances accumulate in the body.
- Gaucher disease: A deficiency in an enzyme that breaks down certain fatty substances.
- Niemann-Pick disease: A group of genetic disorders affecting lipid metabolism.
- Infiltrative diseases: These are conditions in which abnormal cells or substances accumulate in the spleen.
- Sarcoidosis: A condition characterized by the growth of tiny collections of inflammatory cells (granulomas) in various organs.
- Amyloidosis: A condition in which abnormal proteins (amyloid) build up in organs and tissues.
Signs and Symptoms of Splenomegaly

While some people with splenomegaly may not experience any symptoms, others can develop a range of signs and symptoms depending on the underlying cause and the degree of splenomegaly.
Left Upper Abdominal Pain or Fullness
This is one of the most common symptoms. Patients may describe a vague discomfort, a feeling of pressure, or a sharp pain in the upper left part of their abdomen, just below the rib cage. The pain may sometimes radiate to the left shoulder (Kehr’s sign), which is a classic sign of spleen irritation.
Feeling Full After Eating a Small Amount
Splenomegaly can press on the stomach, leading to a sensation of fullness even after consuming a small amount of food. This can result in loss of appetite and unintentional weight loss.
Fatigue
Splenomegaly can sometimes be associated with anemia (low red blood cell count), which can cause fatigue, weakness, and shortness of breath.
Frequent Infections
Filtering function may be impaired in splenomegaly, making individuals more susceptible to infections.
Easy Bleeding or Bruising
Splenomegaly can sometimes trap platelets. This can lead to a reduced platelet count (thrombocytopenia), making individuals more prone to bleeding and bruising.
Splenomegaly on Physical Examination
In some cases, a doctor may be able to feel the splenomegaly during a physical examination. However, in most healthy individuals, the spleen is not palpable.
Other Symptoms
Depending on the underlying cause of splenomegaly, other symptoms may be present e.g. in lymphomas.
- Fever
- Night sweats
- Weight loss
- Swollen lymph nodes
Diagnosis of Splenomegaly
Diagnosing splenomegaly involves a combination of physical examination, medical history, and various diagnostic tests to confirm spleen enlargement and identify the underlying cause.
Medical History and Physical Examination
- Medical history: Symptoms, past medical history, recent illnesses, travel history, medications, and family history of relevant conditions will be collected.
- Physical examination: Physical examination may include:
- Palpation: Gentle feeling of the abdomen to assess the size and consistency of the spleen. In a healthy individual, the spleen is usually not palpable. However, if it’s enlarged, it can be felt below the left costal margin (rib cage).
- Percussion: Tapping on the abdomen to assess the size of the spleen by listening to the sounds produced.
- Checking for other signs: Any other signs that may suggest an underlying cause, such as swollen lymph nodes, pale skin (indicating anemia), or signs of liver disease.
Imaging Tests
- Ultrasound: This is a non-invasive imaging technique that uses sound waves to create images of the spleen. It can confirm spleen enlargement and assess its size and shape.
- CT scan: This imaging technique uses X-rays to create detailed cross-sectional images of the abdomen. It can provide more detailed information about the spleen and surrounding organs.
- MRI: This imaging technique uses magnetic fields and radio waves to create detailed images of the spleen. It can be useful for assessing blood flow through the spleen and identifying certain abnormalities.
Blood Tests
- Complete blood count (CBC): This can help detect anemia, infections, and other blood disorders.
- Liver function tests: Abnormal results may suggest liver disease as a cause of splenomegaly.
- Blood smear: To identify abnormal blood cell morphology or signs of infection.
- Other blood tests: Depending on the suspected cause, other blood tests, such as tests for specific infections, autoimmune diseases, or storage diseases can be ordered.
Bone Marrow Biopsy
In some cases, a bone marrow biopsy may be necessary to diagnose certain blood cancers or other conditions affecting the bone marrow.
Other Tests
In rare cases, other tests may be needed, such as a lymph node biopsy or a spleen biopsy.
Splenic Pain
While the spleen itself doesn’t have many nerve endings, its capsule (outer covering) does. Stretching or irritation of this capsule is what leads to the sensation of splenic pain.
Common Causes of Splenic Pain
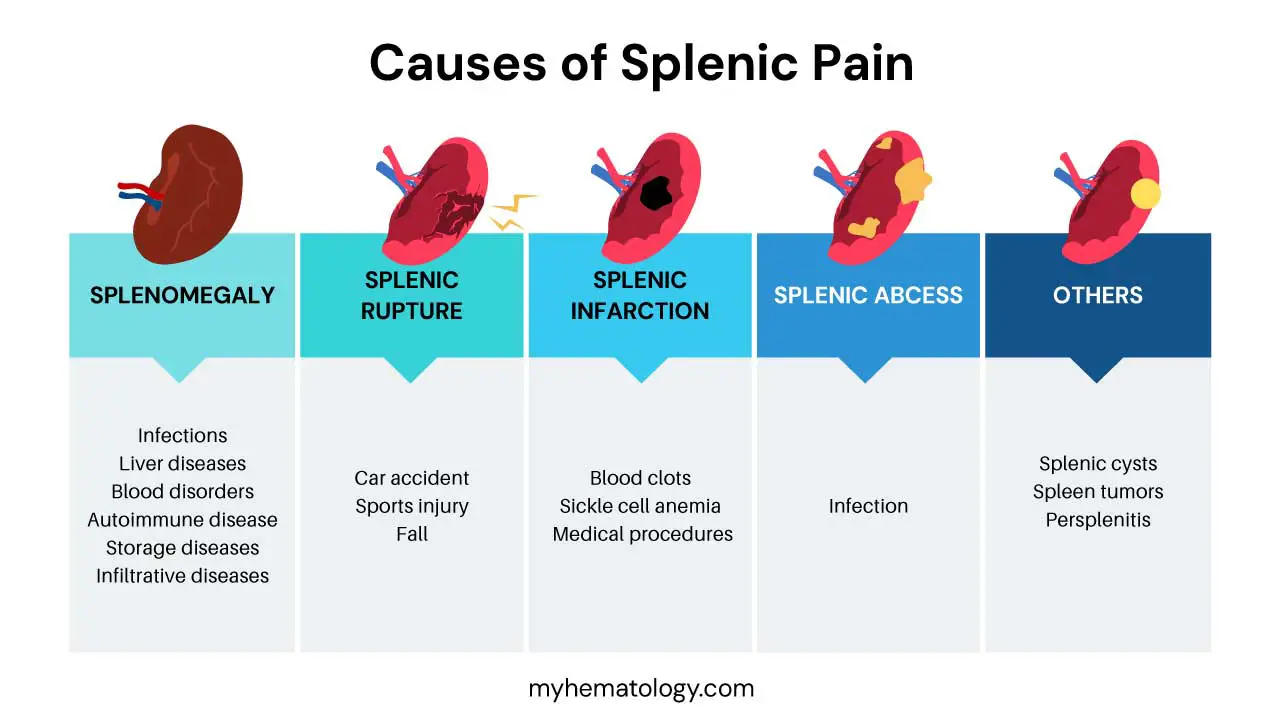
Splenic Enlargement (Splenomegaly)
This is the most common cause of splenic pain. When the spleen enlarges, it stretches the surrounding capsule, causing discomfort or pain in the left upper abdomen. As discussed previously, splenomegaly can be caused by various conditions, including:
- Infections (viral, bacterial, parasitic)
- Liver diseases
- Blood disorders
- Autoimmune diseases
- Storage diseases
- Infiltrative diseases
Splenic Rupture
This is a serious condition that occurs when the spleen’s capsule tears, causing internal bleeding. It is often caused by trauma to the abdomen such as a car accident, sports injury, or fall.
Symptoms of splenic rupture include:
- Severe pain in the left upper abdomen
- Tenderness to the touch in the area
- Left shoulder pain (Kehr’s sign)
- Dizziness
- Rapid heart rate
- Low blood pressure
Splenic Infarction
This occurs when the blood supply to the spleen is blocked, causing tissue death (infarction). It can be caused by:
- Blood clots
- Sickle cell anemia
- Certain medical procedures
Symptoms of splenic infarction include:
- Sudden, sharp pain in the left upper abdomen
- Tenderness to the touch in the area
- Fever
Splenic Abscess
This is a collection of pus within the spleen usually caused by an infection.
Symptoms of splenic abscess include:
- Pain in the left upper abdomen
- Fever
- Chills
- Nausea
- Vomiting
Other Causes of Splenic Pain
In rare cases, splenic pain can be caused by:
- Splenic cysts
- Tumors of the spleen
- Inflammation of the spleen’s capsule (perisplenitis)
Diagnosis of Splenic Pain
Diagnosing splenic pain involves a comprehensive approach to pinpoint the underlying cause and provide appropriate treatment.
Medical History and Physical Examination
- Detailed medical history
- The characteristics of the pain (location, intensity, duration, type)
- Any recent injuries or trauma to the abdomen
- Other symptoms: fever, fatigue, weight loss, easy bruising
- Past medical history, including any history of infections, liver disease, blood disorders, or autoimmune diseases
- Medications
- Physical examination
- Palpation: Gentle pressing on the abdomen, especially the left upper quadrant, to assess for tenderness, guarding, or splenomegaly.
- Percussion: Tapping on the abdomen to assess the size of the spleen.
- Listening with a stethoscope: To check for any abnormal sounds in the abdomen.
Imaging Tests
- Ultrasound: It can confirm splenomegaly, detect abnormalities in the spleen’s structure, such as cysts or abscesses as well as assess blood flow to the spleen.
- CT scan: This provides more detailed images of the spleen and surrounding organs. It can be helpful in identifying splenic rupture or infarction and detecting tumors or other abnormalities.
- MRI: This can provide even more detailed images than a CT scan and may be used in certain cases.
Blood Tests
- Complete blood count (CBC): This can reveal signs of infection (increased white blood cell count), anemia (low red blood cell count) and thrombocytopenia (low platelet count).
- Liver function tests: To assess liver health, as liver disease can cause splenomegaly.
- Blood smear: To examine blood cells under a microscope for abnormalities.
- Tests for specific infections: Such as mononucleosis, malaria, or other infections suspected based on your medical history.
Other Tests
- Bone marrow biopsy: This may be necessary if a blood cancer or other bone marrow disorder is suspected.
- Angiography: This is an imaging test that uses dye to visualize blood vessels. It may be used to diagnose splenic infarction or other vascular problems.
Diagnosis of Specific Causes of Splenic Pain
- Splenic rupture: This is usually diagnosed based on a combination of physical examination findings (severe abdominal pain and tenderness, signs of shock), imaging tests (CT scan), and a history of trauma.
- Splenic infarction: This is typically diagnosed with imaging tests (CT scan or MRI), which can show areas of tissue death in the spleen.
- Splenic abscess: This is diagnosed with imaging tests (CT scan or ultrasound) and blood tests that show signs of infection.
Treatment and Management of Splenic Pain
The treatment and management of splenic pain depend entirely on the underlying cause. Apart from those, there are more general management options.
Pain Management
- Over-the-counter pain relievers: Mild to moderate pain may be managed with over-the-counter pain relievers such as acetaminophen or ibuprofen.
- Prescription pain medications: For more severe pain.
Splenectomy (Spleen Removal)
In some cases, if the underlying cause cannot be treated or if the spleen is causing significant complications, surgical removal of the spleen (splenectomy) may be necessary.
Reasons for splenectomy
- Splenic rupture
- Severe splenomegaly causing significant symptoms
- Certain blood disorders
- Some types of cancer
- Splenic abscess that doesn’t respond to antibiotics
After splenectomy: The patient will be more susceptible to infections, so there will be recommended vaccinations and may prescribe prophylactic antibiotics.
Management of Specific Conditions
- Splenic rupture: This is a medical emergency that usually requires immediate surgery to repair or remove the spleen.
- Splenic infarction: Treatment focuses on managing the underlying cause of the blockage and may involve anticoagulants (blood thinners) or other medications.
- Splenic abscess: Treatment involves antibiotics and drainage of the abscess, either through a needle or surgery.
General Recommendations
- Avoid contact sports: If there is a splenomegaly, avoid contact sports to reduce the risk of splenic rupture.
- Follow-up care: Regular follow-up appointments are important to monitor the condition and adjust treatment as needed.
Frequently Asked Questions (FAQs)
Can an enlarged spleen go back to normal?
Yes, an enlarged spleen, also known as splenomegaly, can often return to its normal size. This typically happens when the underlying condition causing the enlargement is successfully treated. For instance, if an infection like mononucleosis or a bacterial infection is the cause, the spleen will usually shrink back to normal once the infection resolves, sometimes with the help of antibiotics.
However, if the splenomegaly is due to a chronic condition, such as certain liver diseases or blood disorders, it might remain enlarged or require ongoing management of the primary illness to reduce its size. In some severe or complicated cases, or if the underlying cause cannot be cured, treatments like low-dose radiation therapy or even surgical removal (splenectomy) might be considered to manage the splenomegaly and prevent complications.
Can fatty liver cause enlarged spleen?
Yes, fatty liver can indirectly lead to a splenomegaly, especially as the liver disease progresses.
Fatty liver, particularly its more advanced form called non-alcoholic steatohepatitis (NASH), can cause inflammation and scarring (fibrosis) in the liver. Over time, this scarring can lead to cirrhosis, a severe form of liver damage. Cirrhosis significantly impairs blood flow through the liver, causing pressure to build up in the portal vein system, which carries blood from the digestive organs (including the spleen) to the liver. This increased pressure is known as portal hypertension. When blood can’t flow easily through the liver, it can back up into the spleen, causing it to swell and enlarge.
Can I live without a spleen?
Yes, you can absolutely live without a spleen. While the spleen is an important organ, particularly for your immune system and filtering blood, other organs, primarily the liver and bone marrow, can take over most of its functions.
However, living without a spleen does come with an increased, lifelong risk of developing serious infections, especially from certain types of bacteria. To mitigate this risk, individuals without a spleen are typically advised to take precautions such as getting specific vaccinations (e.g., against pneumonia, meningococcus, and Haemophilus influenzae type b), taking daily low-dose antibiotics, and being vigilant for any signs of infection.
What side to sleep on with an enlarged spleen?
When you have a splenomegaly, sleeping on your left side is often recommended.
The spleen is located in the upper left part of your abdomen, under your rib cage. When you lie on your left side, gravity can help facilitate drainage to the spleen, which is part of the lymphatic system that filters blood and lymph. This may help with comfort and potentially assist the spleen’s function.
However, the most important thing is to find a position that is comfortable and doesn’t cause pain or pressure. Splenomegaly can press on other organs, leading to discomfort or a feeling of fullness. If you’re experiencing significant pain or discomfort while sleeping due to splenomegaly, it’s best to consult your doctor for personalized advice. They can help identify the best sleeping position and other strategies to manage your symptoms.
What happens if you ignore spleenic pain?
Ignoring splenic pain, especially if it’s persistent or severe, can lead to serious complications because it often signals an underlying medical condition. A splenomegaly which is a common cause of spleen pain, is more fragile and susceptible to rupture, which can cause life-threatening internal bleeding and requires immediate emergency medical attention.
Furthermore, a dysfunctional or enlarged spleen can lead to a reduction in healthy red blood cells, white blood cells, and platelets, resulting in anemia, increased susceptibility to infections, and easy bleeding or bruising. Ultimately, unresolved spleen pain indicates that the underlying cause, whether it’s an infection, liver disease, blood disorder, or even cancer, is likely progressing and needs prompt medical diagnosis and treatment.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Jones JF. Development of the spleen. Lymphology. 1983 Jun;16(2):83-9. PMID: 6350736.
- Aldulaimi S, Mendez AM. Splenomegaly: Diagnosis and Management in Adults. Am Fam Physician. 2021 Sep 1;104(3):271-276. PMID: 34523897.
- Pozo AL, Godfrey EM, Bowles KM. Splenomegaly: investigation, diagnosis and management. Blood Rev. 2009 May;23(3):105-11. doi: 10.1016/j.blre.2008.10.001. Epub 2008 Dec 4. PMID: 19062140.
- Lucas CE. Splenic trauma. Choice of management. Ann Surg. 1991 Feb;213(2):98-112. doi: 10.1097/00000658-199102000-00002. PMID: 1992948; PMCID: PMC1358380.
- Bouzat P, Thony F, Arvieux C. Management of splenic injury after blunt abdominal trauma: insights from the SPLASH trial. Anaesth Crit Care Pain Med. 2020 Dec;39(6):747-748. doi: 10.1016/j.accpm.2020.10.009. Epub 2020 Oct 26. PMID: 33122040.