TL;DR
A macrophage is a specialized white blood cell that play a crucial role in the immune system. They are known as “garbage collectors” because they engulf and digest foreign particles, such as bacteria, viruses, and cellular debris.
Key functions of macrophages ▾
- Phagocytosis: Engulfing and digesting foreign particles
- Antigen presentation: Presenting antigens to T cells to activate the adaptive immune response
- Cytokine and chemokine production: Regulating inflammation and attracting other immune cells
- Tissue repair and remodeling: Promoting tissue healing and regeneration
- Tissue macrophages: Found in specific tissues (e.g., alveolar macrophages, Kupffer cells, microglia)
- Inflammatory macrophages: Recruited to sites of inflammation (M1 and M2 subtypes)
- Originate from hematopoietic stem cells
- Differentiate from monocytes
- Involved in various diseases, including infections, inflammation, cancer, and autoimmune disorders
- CBC (indirectly)
- Flow cytometry
- Immunohistochemistry
- Cytokine measurements
- Phagocytosis assays
*Click ▾ for more information
Introduction
A macrophage is a specialized cell that plays a crucial role in the immune system. They are large white blood cells that engulf and digest foreign particles, such as bacteria and cellular debris. Essentially, they act as “garbage collectors” of the body, helping to maintain tissue health and fight off infections.
Overview of the Immune System
The immune system is a complex network of cells, tissues, and organs that work together to protect the body from harmful pathogens like bacteria, viruses, fungi, and parasites. It is essential for maintaining overall health and preventing diseases.
Key functions of the immune system include:
- Identifying and attacking foreign invaders: The immune system recognizes and targets harmful substances, such as bacteria and viruses, that enter the body.
- Eliminating damaged cells: It removes old or damaged cells that are no longer functioning properly.
- Preventing autoimmune diseases: The immune system helps to prevent the body from attacking its own tissues, which can lead to autoimmune diseases.
The immune system is composed of two main components:
- Innate immunity: This is a nonspecific defense system that provides a first line of defense against pathogens. It includes physical barriers like the skin and mucous membranes, as well as cells like neutrophils and macrophages that engulf and destroy invaders.
- Adaptive immunity: This is a more specific defense system that develops over time and can target specific pathogens. It involves lymphocytes, such as T cells and B cells, which can recognize and attack particular antigens.
By effectively carrying out these functions, the immune system helps to maintain a healthy balance within the body and protect against various diseases.
Role of Macrophages in Innate Immunity
Innate immunity is the body’s first line of defense against pathogens. It’s a rapid and non-specific response that helps to prevent infections from spreading. This system is crucial because it provides a quick response to potential threats, buying time for the adaptive immune system to develop a more targeted response.
Macrophages are key players in innate immunity. These specialized white blood cells are responsible for:
- Phagocytosis: Macrophages engulf and digest foreign particles, such as bacteria, viruses, and cellular debris. This process helps to eliminate harmful invaders before they can cause significant damage.
- Antigen presentation: Macrophages can present fragments of ingested pathogens to T cells, which are key cells of the adaptive immune system. This helps to activate the adaptive immune response, leading to a more targeted attack on the invading pathogen.
- Cytokine production: Macrophages produce various cytokines, which are signaling molecules that help to coordinate the immune response. These cytokines can attract other immune cells to the site of infection, promote inflammation, and stimulate the production of antibodies.
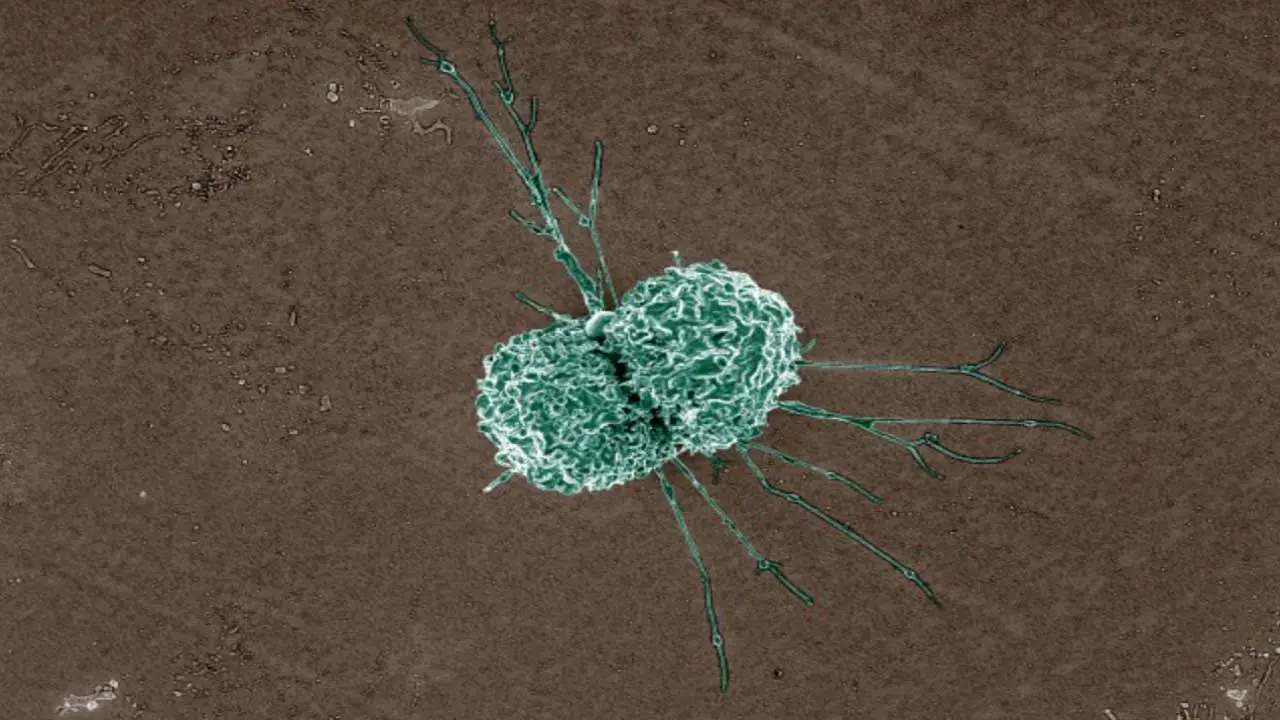
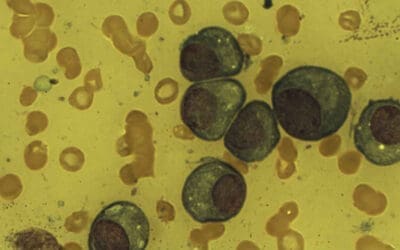
Morphology of Macrophage
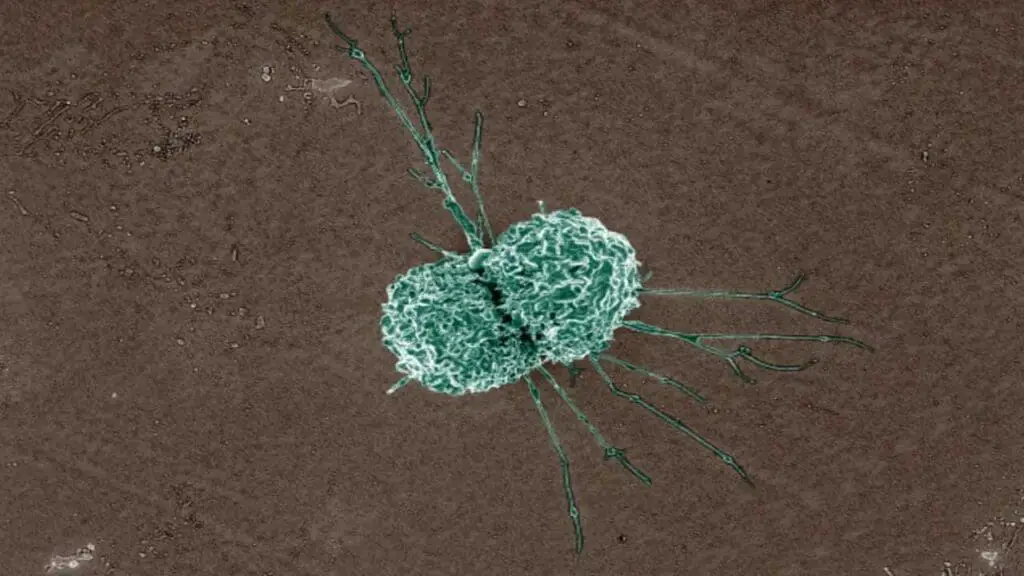
Macrophages are large, irregularly shaped white blood cells that are characterized by their ability to engulf and digest foreign particles. Their morphology is often described as “amoeboid,” meaning they have a flexible, constantly changing shape that allows them to move and engulf particles.
- Size: Macrophages are significantly larger than most other white blood cells. They can vary in size depending on their activation state and the type of tissue they are in, but they are generally around 20-80 micrometers in diameter.
- Shape: Macrophages are highly irregular in shape and can change their shape rapidly. They often have pseudopodia, which are temporary projections of cytoplasm that allow them to move and engulf particles.
- Nucleus: The nucleus of a macrophage is typically large, round, or slightly indented, and often occupies a significant portion of the cell. It may contain multiple nucleoli.
- Cytoplasm: The cytoplasm of a macrophage is abundant and contains numerous organelles, including lysosomes, mitochondria, and rough endoplasmic reticulum. It also contains various granules and vacuoles that are involved in phagocytosis and other cellular functions.
Types of Macrophages
Macrophages are a diverse group of cells that can be classified based on their location or function.
Tissue Macrophages
These macrophages reside in specific tissues and organs, where they perform specialized functions.
- Alveolar macrophages: Found in the alveoli of the lungs, these cells are responsible for clearing the airways of debris, bacteria, and other foreign particles. They have a high phagocytic capacity and are able to produce a variety of inflammatory mediators. They play a crucial role in lung defense and can contribute to lung diseases like chronic obstructive pulmonary disease (COPD) and tuberculosis.
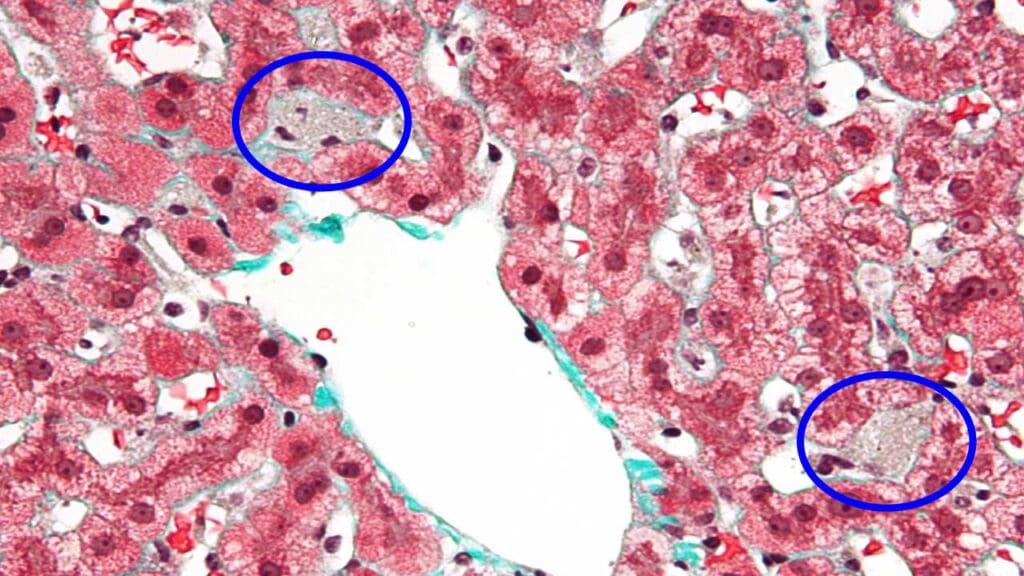
- Kupffer cells: Located in the liver, these macrophages play a crucial role in liver detoxification and metabolism. These macrophages are able to remove a wide range of substances from the blood, including bilirubin, drugs, and toxins. For example, they are involved in clearing the blood of old red blood cells and foreign substances.
- Microglia: Found in the brain, these are the resident macrophages of the central nervous system. They are responsible for surveillance of the brain tissue, removal of debris, and response to injury or infection. They also play a role in neuroinflammation and neurodegenerative diseases. They are able to rapidly respond to injury or inflammation by changing their morphology and function.
Inflammatory Macrophages
These macrophages are recruited to sites of inflammation in response to signals from other immune cells. They are characterized by their increased expression of inflammatory markers and their role in tissue repair and remodeling.
- M1 macrophages: These are classically activated macrophages that promote inflammation and tissue damage. These macrophages are characterized by their production of inflammatory cytokines, such as TNF-alpha, IL-1, and IL-6. They are involved in the clearance of pathogens and cellular debris, but can also contribute to tissue damage if they are not properly regulated.
- M2 macrophages: These are alternatively activated macrophages that promote tissue repair and regeneration. These macrophages are characterized by their production of anti-inflammatory cytokines, such as IL-10 and TGF-beta. They are involved in tissue repair, angiogenesis, and the resolution of inflammation.
Monocyte-Derived Macrophages
These macrophages are derived from monocytes, which are circulating white blood cells. They can differentiate into various types of macrophages depending on the signals they receive.
- Tissue-resident macrophages: Monocytes can differentiate into tissue-resident macrophages, such as alveolar macrophages and Kupffer cells. These macrophages are long-lived and play essential roles in tissue homeostasis.
- Inflammatory macrophages: Monocytes can also differentiate into inflammatory macrophages in response to inflammatory signals.
Development of Macrophages
Macrophages, like most other immune cells, originate from hematopoietic stem cells (HSCs) in the bone marrow. These HSCs are pluripotent cells that can give rise to all types of blood cells, including red blood cells, white blood cells, and platelets.
Myeloid progenitor cells are a subset of HSCs that are committed to producing myeloid cell lineages, which include macrophages, neutrophils, eosinophils, basophils, and monocytes. These progenitor cells undergo a series of differentiation steps to give rise to mature macrophages.
Differentiation of Monocytes into Macrophages
Monocytes are immature white blood cells that circulate in the bloodstream. They are precursors to macrophages and other myeloid cell types. Under the influence of various factors, monocytes can differentiate into macrophages.
The differentiation process involves several key steps:
- Recruitment to tissues: Monocytes are recruited to tissues by various chemotactic factors, which are signaling molecules that attract cells to a specific location.
- Differentiation into macrophages: Once in the tissues, monocytes differentiate into macrophages. This process is influenced by a variety of factors, including cytokines, growth factors, and tissue-specific signals.
- Maturation and activation: Mature macrophages can further differentiate and become activated in response to various stimuli, such as pathogens, cytokines, and other signals.
Factors Influencing Macrophage Development
Several factors can influence the development and function of macrophages, including:
- Cytokines: Cytokines are signaling molecules that play a crucial role in macrophage development and activation. Different cytokines can promote the differentiation of monocytes into different types of macrophages and can influence the functions of mature macrophages. For example, colony-stimulating factors (CSFs) and interleukins (ILs) are important for macrophage development and activation.
- Growth factors: Growth factors, such as platelet-derived growth factor (PDGF) and transforming growth factor-beta (TGF-beta), can also influence macrophage development and function. These factors can promote tissue repair and remodeling, and can also modulate the inflammatory response.
- Microenvironment: The microenvironment in which macrophages reside can also influence their development and function. Factors such as the presence of pathogens, tissue damage, and the presence of other immune cells can all affect macrophage activation and behavior.
Lifespan of Macrophage in the Blood
Macrophages primarily reside in tissues, rather than circulating in the blood. Their lifespan in the bloodstream is relatively short, as they quickly migrate to tissues where they are needed. Once they have entered tissues, their lifespan can vary depending on the specific tissue and their function.
Functions of Macrophage
Macrophages are versatile cells that play essential roles in various aspects of immune function and tissue homeostasis. Their functions include:
Phagocytosis and Intracellular Killing of Pathogens
- Phagocytosis: Macrophages are highly efficient phagocytes, capable of engulfing and ingesting a wide range of particles, including bacteria, viruses, fungi, and cellular debris. They use their pseudopodia to surround and engulf target particles, which are then internalized in a membrane-bound vesicle called a phagosome.
- Intracellular killing: Once inside the phagosome, pathogens are exposed to a variety of antimicrobial mechanisms, including reactive oxygen species (ROS), reactive nitrogen species (RNS), and lysosomal enzymes. These mechanisms help to destroy the pathogen and prevent its replication.
Antigen Presentation to T Cells
- Antigen processing: Macrophages can process antigens derived from ingested pathogens or damaged cells. This involves breaking down the antigens into smaller peptides, which are then loaded onto major histocompatibility complex (MHC) molecules.
- Antigen presentation: Macrophages present these MHC-peptide complexes on their cell surface, where they can be recognized by T cells. This process is essential for activating the adaptive immune response.
Secretion of Cytokines and Chemokines
- Cytokines: Macrophages produce a variety of cytokines, which are signaling molecules that play important roles in both innate and adaptive immunity. These cytokines can recruit other immune cells to the site of inflammation, promote or suppress inflammation, and influence the development and function of other cell types. For example, interleukin-1 (IL-1) is a well-known cytokine produced by macrophages. It plays a crucial role in the inflammatory response, stimulating the production of other cytokines, promoting fever, and increasing the permeability of blood vessels. IL-1 is also involved in the activation of T cells and B cells.
- Chemokines: Macrophages also produce chemokines, which are small proteins that attract other immune cells to the site of inflammation. Chemokines play a crucial role in guiding the migration of neutrophils, monocytes, and lymphocytes to sites of infection or injury. For example, monocyte chemoattractant protein-1 (MCP-1) is a chemokine produced by macrophages. It is a potent chemoattractant for monocytes and other leukocytes, drawing them to sites of inflammation. MCP-1 plays a crucial role in the recruitment of immune cells to areas of infection or injury.
Tissue Repair and Remodeling
- Tissue repair: Macrophages play a key role in tissue repair and regeneration. They can clear debris, promote angiogenesis (the formation of new blood vessels), and stimulate the proliferation of fibroblasts and other cells involved in tissue repair.
- Remodeling: Macrophages can also help to remodel tissues by removing damaged or old extracellular matrix components and promoting the deposition of new matrix.
Role in Inflammation and Immune Regulation
- Inflammation: Macrophages are central players in the inflammatory response. They can produce a variety of inflammatory mediators, including cytokines, chemokines, and prostaglandins, which help to recruit other immune cells to the site of inflammation and promote tissue repair.
- Immune regulation: Macrophages can also play a role in regulating the immune response. They can produce both pro-inflammatory and anti-inflammatory cytokines, which can help to balance the immune response and prevent excessive inflammation.
Causes of High and Low Macrophage Counts
Conditions Associated with High Macrophage Counts
An elevated macrophage count, often indicated by an increase in monocyte numbers (which differentiate into macrophages), can be a sign of various conditions and diseases.
Infectious Diseases
- Bacterial infections: Macrophages play a crucial role in fighting bacterial infections. Conditions like pneumonia, tuberculosis, and sepsis can lead to increased macrophage production and activity.
- Viral infections: Viral infections, such as HIV, hepatitis, and influenza, can also trigger an increase in macrophage numbers as the immune system responds to the infection.
- Parasitic infections: Macrophages are involved in combating parasitic infections, so conditions like malaria, leishmaniasis, and toxoplasmosis can lead to elevated macrophage counts.
Inflammatory Conditions
- Chronic inflammation: Chronic inflammatory diseases, such as rheumatoid arthritis, systemic lupus erythematosus (SLE), and inflammatory bowel disease (IBD), often involve increased macrophage activity and numbers.
- Autoimmune diseases: In autoimmune diseases, where the immune system mistakenly attacks the body’s own tissues, macrophages can contribute to inflammation and tissue damage.
- Allergic reactions: Allergic reactions can trigger an increase in macrophage numbers as part of the immune response to allergens.
Cancer
- Tumor growth: Macrophages are often found in and around tumors, where they can play a role in both promoting and inhibiting tumor growth. In some cases, an increase in macrophage numbers can be associated with cancer progression.
- Cancer therapy: Certain cancer treatments, such as chemotherapy and radiation therapy, can cause inflammation and tissue damage, leading to an increase in macrophage numbers.
Other Conditions
- Granulomatous diseases: Conditions characterized by the formation of granulomas, which are collections of macrophages and other immune cells, can lead to elevated macrophage counts. Examples include sarcoidosis and tuberculosis.
- Hematological disorders: Some hematological disorders, such as leukemia and lymphoma, can involve an increase in monocyte and macrophage numbers.
It’s important to note that an elevated macrophage count is not a specific diagnosis. It is often a secondary finding that can be associated with a variety of underlying conditions. Further testing is usually required to determine the specific cause of the increased macrophage count.
Conditions Associated with Low Macrophage Counts
A low macrophage count, also known as macrophage deficiency, can be a sign of various underlying conditions.
Immunodeficiency Disorders
- Primary immunodeficiency diseases: These are inherited conditions that affect the immune system’s ability to fight off infections. Some primary immunodeficiency diseases can lead to a decrease in macrophage numbers or function.
- Acquired immunodeficiency syndrome (AIDS): HIV infection can lead to a depletion of macrophages, particularly those in the lungs and gastrointestinal tract. This contributes to the susceptibility to opportunistic infections seen in AIDS patients.
Bone Marrow Disorders
- Bone marrow aplasia: This is a condition characterized by a failure of the bone marrow to produce blood cells. It can lead to a decrease in macrophage production.
- Leukemia and lymphoma: Some types of leukemia and lymphoma can involve the replacement of normal bone marrow cells with cancerous cells, leading to a decrease in macrophage production.
Drug-Induced Macrophage Depletion
- Certain medications: Some medications, such as corticosteroids and certain chemotherapy drugs, can suppress the immune system and lead to a decrease in macrophage numbers.
Other Conditions
- Sepsis: In severe cases of sepsis, an overwhelming infection can lead to a decrease in macrophage numbers and function.
- Malnutrition: Inadequate nutrition can impair immune function, including macrophage production and function.
It’s important to note that a low macrophage count is not a specific diagnosis. It is often a secondary finding that can be associated with a variety of underlying conditions. Further testing is usually required to determine the specific cause of the decreased macrophage count.
Common Laboratory Tests to Assess Macrophage Function or Count
Complete Blood Count (CBC)
- Indirect assessment: While a CBC primarily measures red and white blood cells, it can provide an indirect indication of macrophage activity. An increase in monocytes, which are precursors to macrophages, might suggest increased macrophage production or activation.
- Limitations: A CBC cannot directly measure macrophage function or specific subsets.
Flow Cytometry
- Direct measurement: Flow cytometry is a powerful technique that can directly measure the number and function of different cell types, including macrophages.
- Applications: By using specific antibodies labeled with fluorescent markers, flow cytometry can:
- Count different macrophage subsets based on their surface markers (e.g., CD14, CD16)
- Assess macrophage activation status by measuring the expression of activation markers (e.g., CD40, CD86)
- Evaluate macrophage phagocytic function by measuring the uptake of fluorescently labeled particles
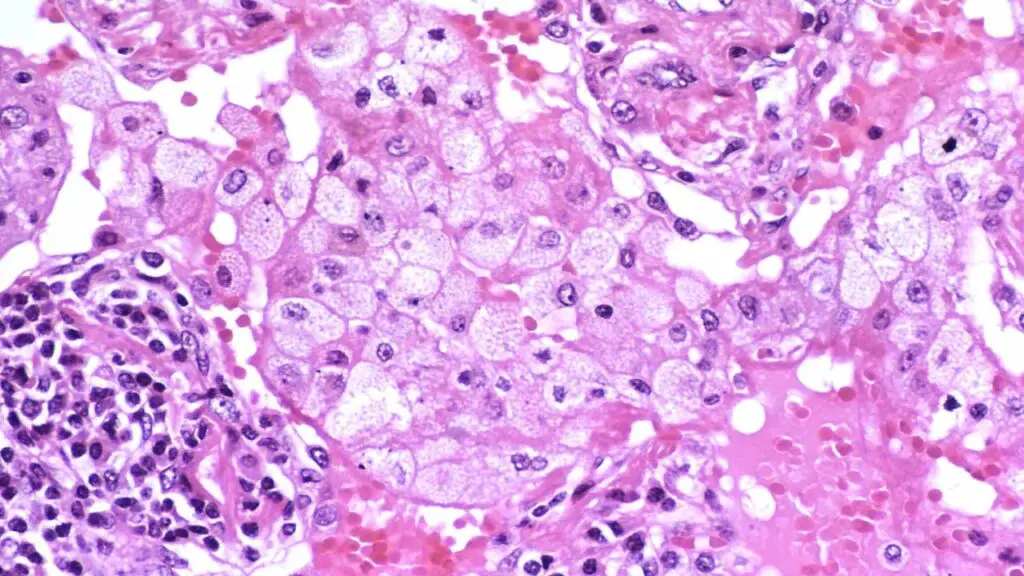
Immunohistochemistry
- Tissue-based assessment: Immunohistochemistry is used to visualize specific proteins or antigens in tissue samples.
- Applications: By using antibodies against macrophage markers (e.g., CD68, F4/80), immunohistochemistry can:
- Identifying macrophage distribution and localization in tissues
- Assessing macrophage activation and polarization (M1 vs. M2)
- Studying macrophage involvement in diseases like cancer and inflammation
Cytokine Measurements
- Functional assessment: Cytokines are signaling molecules produced by macrophages. Measuring cytokine levels can provide insights into macrophage function and activation.
- Applications: Various techniques, such as ELISA or multiplex assays, can be used to measure cytokines produced by macrophages.
- Assessing macrophage activation (e.g., increased production of pro-inflammatory cytokines like TNF-alpha and IL-1)
- Evaluating macrophage polarization (e.g., increased production of anti-inflammatory cytokines like IL-10 and TGF-beta)
- Monitoring the effectiveness of anti-inflammatory therapies
Phagocytosis Assays
- Functional assessment: Phagocytosis assays measure the ability of macrophages to engulf and ingest foreign particles.
- Applications: Various methods can be used to assess phagocytosis, including:
- Fluorescently labeled particles
- Bacteria or other pathogens
- Flow cytometry or microscopy to visualize phagocytosis
The choice of laboratory test depends on the specific research question or clinical scenario. For example, if the goal is to assess macrophage activation status in a blood sample, flow cytometry might be most appropriate. If the interest is in examining macrophage involvement in a tissue disease, immunohistochemistry would be more suitable.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Mass, E., Nimmerjahn, F., Kierdorf, K. et al. Tissue-specific macrophages: how they develop and choreograph tissue biology. Nat Rev Immunol 23, 563–579 (2023). https://doi.org/10.1038/s41577-023-00848-y
- Gordon S, Plüddemann A. Tissue macrophages: heterogeneity and functions. BMC Biol. 2017 Jun 29;15(1):53. doi: 10.1186/s12915-017-0392-4. PMID: 28662662; PMCID: PMC5492929.
- Shapouri-Moghaddam A, Mohammadian S, Vazini H, Taghadosi M, Esmaeili SA, Mardani F, Seifi B, Mohammadi A, Afshari JT, Sahebkar A. Macrophage plasticity, polarization, and function in health and disease. J Cell Physiol. 2018 Sep;233(9):6425-6440. doi: 10.1002/jcp.26429. Epub 2018 Mar 1. PMID: 29319160.
- Bied, M., Ho, W.W., Ginhoux, F. et al. Roles of macrophages in tumor development: a spatiotemporal perspective. Cell Mol Immunol 20, 983–992 (2023). https://doi.org/10.1038/s41423-023-01061-6
- Lee JW, Chun W, Lee HJ, Min JH, Kim SM, Seo JY, Ahn KS, Oh SR. The Role of Macrophages in the Development of Acute and Chronic Inflammatory Lung Diseases. Cells. 2021 Apr 14;10(4):897. doi: 10.3390/cells10040897. PMID: 33919784; PMCID: PMC8070705.
- Xia T, Fu S, Yang R, Yang K, Lei W, Yang Y, Zhang Q, Zhao Y, Yu J, Yu L, Zhang T. Advances in the study of macrophage polarization in inflammatory immune skin diseases. J Inflamm (Lond). 2023 Oct 12;20(1):33. doi: 10.1186/s12950-023-00360-z. PMID: 37828492; PMCID: PMC10568804.
- Mantovani, A., Allavena, P., Marchesi, F. et al. Macrophages as tools and targets in cancer therapy. Nat Rev Drug Discov 21, 799–820 (2022). https://doi.org/10.1038/s41573-022-00520-5