TL;DR
Lymphopenia is defined as abnormally low lymphocytes in the blood (e.g., <1.0 x 109/L in adults).
- Lymphocytes ▾: Crucial immune cells (T cells, B cells, NK cells) providing specific defense against pathogens and abnormal cells.
- Causes ▾:
- Decreased Production: Bone marrow suppression (chemo, radiation, aplastic anemia), congenital immunodeficiencies.
- Increased Destruction/Apoptosis: Infections (HIV, COVID-19, flu), autoimmune diseases (SLE), medications (corticosteroids).
- Redistribution: Acute stress, corticosteroid use.
- Loss: Protein-losing enteropathy.
- Cancers: Leukemias, lymphomas, multiple myeloma, and solid tumors (via bone marrow infiltration, systemic effects, or treatment).
- Symptoms ▾: Often non-specific. Increased susceptibility to recurrent, severe, or opportunistic infections and symptoms of the underlying cause (e.g., fatigue, fever, rash).
- Laboratory Investigations ▾:
- CBC with Differential: Confirms low Absolute Lymphocyte Count (ALC).
- Flow Cytometry (Lymphocyte Subsets): Identifies specific T, B, or NK cell deficiencies.
- Further tests based on suspicion: HIV, autoimmune markers, bone marrow biopsy, genetic tests.
- Treatment/Management ▾:
- Address Underlying Cause: Most crucial (e.g., treat infection, manage autoimmune disease, modify medication).
- Supportive Care: Prophylactic antimicrobials (for high infection risk), immunoglobulin replacement (if antibody levels are low).
- Advanced Therapies: Stem cell transplant (for severe cases), gene therapy.
*Click ▾ for more information
Introduction
Lymphopenia, also known as lymphocytopenia, is a condition characterized by a lower-than-normal number of lymphocytes in the peripheral blood. A low lymphocyte count can indicate an underlying medical condition, medication side effect, or stress response, and may increase a patient’s susceptibility to infections and other immune dysfunctions.
What are Lymphocytes?

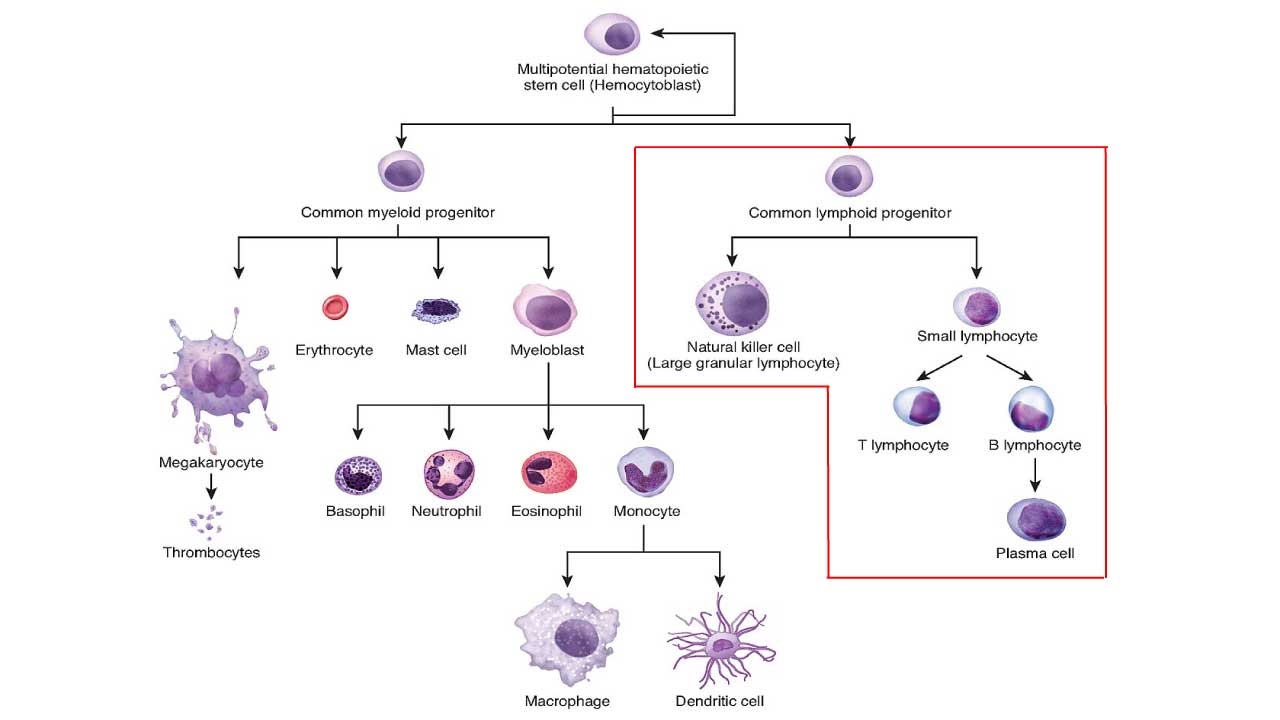
Lymphocytes are a vital type of white blood cell (leukocyte) that are central to the body’s immune system. They are responsible for providing specific immunity, meaning they can recognize and target particular pathogens (like viruses, bacteria, or fungi) or abnormal cells (like cancer cells).
All lymphocytes originate from hematopoietic stem cells in the bone marrow. They then undergo a maturation process where some remain in the bone marrow to mature into B lymphocytes (B cells), others migrate to the thymus (a gland located behind the breastbone) to mature into T lymphocytes (T cells) and a third major type, Natural Killer (NK) cells, are also lymphocytes and are part of the innate immune system.
Once mature, lymphocytes circulate in the blood and lymphatic system (lymph nodes, spleen, tonsils, etc.), constantly surveying for foreign invaders or abnormal cells. Their function include:
- B cells: Primarily responsible for humoral immunity. When they encounter a specific antigen (a unique marker on a pathogen or abnormal cell), they can differentiate into plasma cells that produce and secrete large amounts of antibodies. These antibodies then bind to the antigens, neutralizing the threat or marking it for destruction by other immune cells.
- T cells: Primarily responsible for cell-mediated immunity.
- Helper T cells (CD4+ T cells): Act as “coordinators” of the immune response, helping to activate B cells, other T cells, and macrophages.
- Cytotoxic T cells (CD8+ T cells): Directly identify and kill infected cells (e.g., virus-infected cells) or cancer cells.
- Regulatory T cells: Help to suppress or regulate immune responses, preventing the immune system from attacking healthy body tissues.
- NK cells: Part of the innate immune system, meaning they provide immediate, non-specific defense. They can recognize and kill virus-infected cells and some tumor cells without needing prior activation or specific antigen recognition like T and B cells.
Differences between Innate and Adaptive Immunity
| Feature | Innate Immunity | Adaptive Immunity |
| Speed | Immediate (minutes to hours) | Slower (days for primary response, faster for secondary) |
| Specificity | Non-specific (recognizes general pathogen patterns) | Highly specific (targets particular antigens) |
| Memory | No immunological memory | Develops immunological memory |
| Components | Physical barriers, phagocytes, NK cells, complement, etc. | B cells, T cells, antibodies, MHC molecules |
| Evolutionary Age | Older, found in most multicellular organisms | Newer, primarily in vertebrates |
| Main Function | First line of defense, rapid response | Tailored, long-lasting, specific protection |
Absolute vs Relative Lymphopenia (Low Lymphocytes)
Understanding the normal range of lymphocytes and the distinction between absolute lymphopenia and relative lymphopenia (low lymphocytes) is crucial for medical students.
Normal Range of Lymphocytes
The “normal range” for lymphocyte counts can vary slightly between laboratories and is significantly influenced by age.
- Adults: The generally accepted normal range for an Absolute Lymphocyte Count (ALC) in adults is typically between 1.0 x 109/L to 4.8 x 109/L (or 1000 to 4800 cells/µL). Some labs might use a slightly wider or narrower range, so it’s always important to refer to the specific reference range provided by the performing laboratory.
- Children: Lymphocyte counts are naturally higher in children, especially in infants and young children, and gradually decrease to adult levels as they age.
- Infants (<2 years): Normal absolute lymphocyte count can be as high as 3.0 x 109/L to 9.5 x 109/L (or 3000 to 9500 cells/µL).
- Children (e.g., 6 years old): The lower limit of normal might be around 1.5 x 109/L (or 1500 cells/µL).
These values are obtained from a Complete Blood Count (CBC) with differential, which provides the total white blood cell count and the percentages and absolute numbers of each type of white blood cell, including lymphocytes.
Absolute Lymphopenia
Absolute lymphopenia (low lymphocytes) is diagnosed when the total number of lymphocytes in the blood (the Absolute Lymphocyte Count – ALC) falls below the established lower limit of the normal range for that age group.
- For adults, this is typically defined as an Absolute Lymphocyte Count (ALC) < 1.0 x 109/L (or < 1000 cells/µL).
- For children, the threshold of Absolute Lymphocyte Count (ALC) is higher and age-dependent (e.g., < 3.0 x 109/L for children under 2 years).
Absolute lymphopenia is the most clinically significant type of lymphopenia (low lymphocytes), as it directly reflects a true reduction in the circulating lymphocyte population and is associated with increased risk of infections and other immune-related complications.
Relative Lymphopenia
Relative lymphopenia (low lymphocytes) occurs when the percentage of lymphocytes among the total white blood cell (WBC) count is low, even if the absolute lymphocyte count (ALC) is within the normal range.
To understand this, remember that the “differential” part of a complete blood count tells you the percentage of each white blood cell type. For example, if the total WBC count is very high (e.g., due to a significant increase in neutrophils, a condition called neutrophilia), the percentage of lymphocytes might appear low, even if the absolute lymphocyte count is normal.
Example:
- A patient has a total WBC count of 20.0 x 109/L (normal: 4.0-11.0 x 109/L).
- Their lymphocyte percentage is 10% (normal: 20-40%).
- Their Absolute Lymphocyte Count (ALC) would be 10% of 20.0 x 109/L = 2.0 x 109/L.
In this scenario:
- The ALC (2.0 x 109/L) is within the normal range for an adult (1.0-4.8 x 109/L). So, there is no absolute lymphopenia (low lymphocytes).
- However, the lymphocyte percentage (10%) is low compared to the normal percentage (20-40%). This indicates relative lymphopenia.
Relative lymphopenia (low lymphocytes) often suggests that another type of white blood cell is disproportionately elevated, “diluting” the percentage of lymphocytes. While not as immediately concerning as absolute lymphopenia (low lymphocytes), it can still provide clues about underlying conditions, such as severe bacterial infections (which cause neutrophilia) or acute stress, where other white blood cell lines proliferate. However, for assessing immune competence and risk of infection, the absolute lymphocyte count is always the primary indicator.
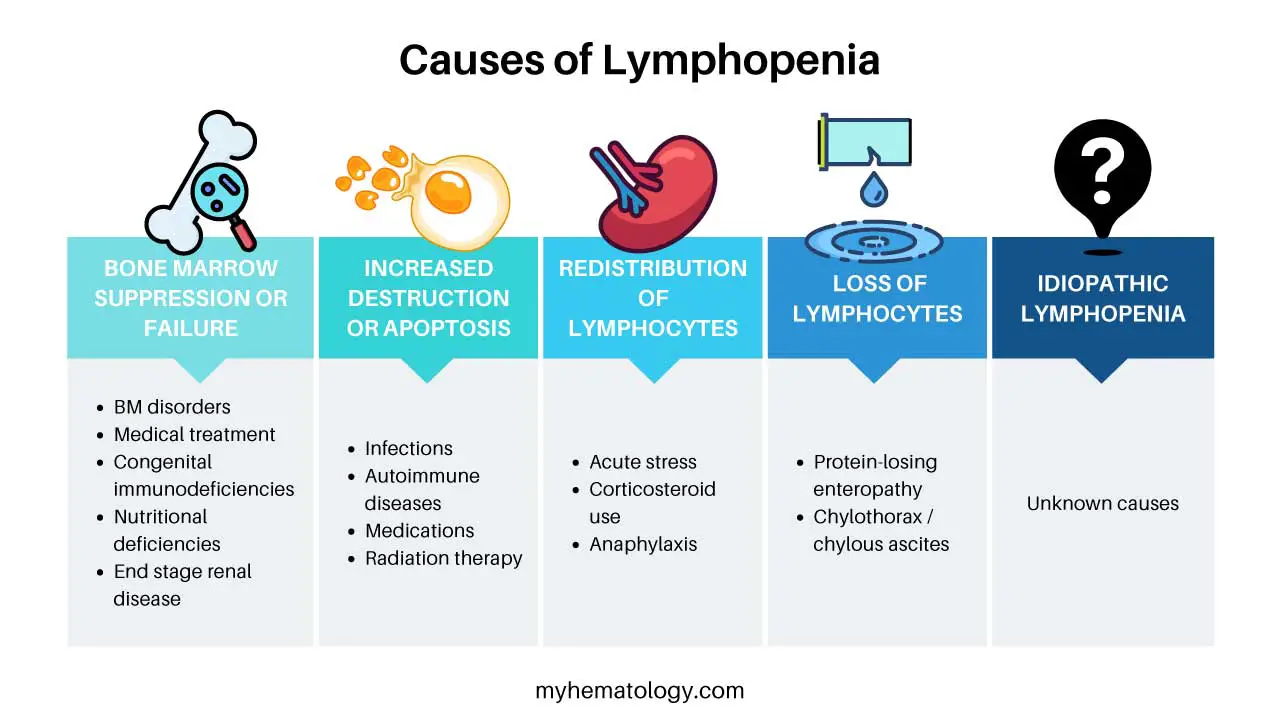
Causes of Lymphopenia (Low Lymphocytes)
Lymphopenia, a reduction in the absolute lymphocyte count, can stem from a wide array of causes, broadly categorized into issues with lymphocyte production, increased destruction or redistribution, and loss from the body. Understanding these categories is key to diagnosing and managing the condition.
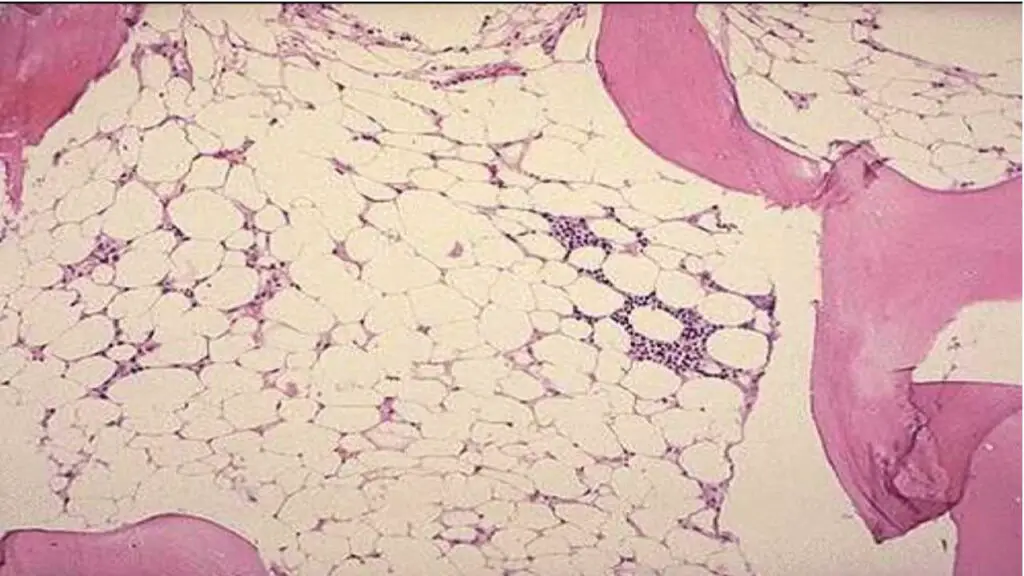
Decreased Production of Lymphocytes (Bone Marrow Suppression/Failure)
This category involves problems where the bone marrow, the primary site of lymphocyte production, is unable to generate enough lymphocytes.
Bone Marrow Disorders
- Aplastic Anemia
- Myelodysplastic Syndromes (MDS)
- Leukemias and Lymphomas
- Bone Marrow Failure Syndromes
Medical Treatments
- Chemotherapy: Many chemotherapeutic agents target rapidly dividing cells, including lymphocyte precursors in the bone marrow, leading to significant and often transient lymphopenia (low lymphocytes).
- Radiation Therapy: Especially if large areas of bone marrow are irradiated.
- Immunosuppressive Drugs (non-corticosteroid): Some immunosuppressants used in transplant patients or for autoimmune diseases can directly suppress lymphocyte production (e.g., azathioprine, methotrexate, cyclosporine, tacrolimus).
Congenital Immunodeficiencies (Primary Immunodeficiencies – PIDs)
These are genetic disorders that affect the development and function of the immune system from birth. They often involve a direct defect in lymphocyte production or maturation.
- Severe Combined Immunodeficiency (SCID): A group of life-threatening disorders characterized by absent or severely impaired T and B cell function, leading to very low lymphocyte counts.
- DiGeorge Syndrome (22q11.2 deletion syndrome): Characterized by hypoplasia or aplasia of the thymus, leading to severe T-cell deficiency.
- Wiskott-Aldrich Syndrome: An X-linked disorder characterized by immunodeficiency, thrombocytopenia, and eczema, often with T-cell lymphopenia (low lymphocytes).
- Ataxia-Telangiectasia: A genetic disorder affecting multiple systems, including the immune system, leading to T and B cell deficiencies.
- Common Variable Immunodeficiency (CVID): While often presenting with low immunoglobulins, a subset of patients can have associated lymphopenia (low lymphocytes), particularly B cell lymphopenia.
Nutritional Deficiencies
- Protein-Energy Malnutrition: Severe malnutrition can significantly impair lymphocyte production and function. This is a common cause of lymphopenia (low lymphocytes) worldwide.
- Specific Micronutrient Deficiencies: Deficiencies in essential vitamins and minerals like zinc, vitamin B12, and folic acid can impair lymphocyte development and function.
Chronic Diseases
- End-stage Kidney Disease: Can contribute to lymphopenia (low lymphocytes) through various mechanisms, including uremic toxins affecting lymphocyte production.
Increased Destruction or Apoptosis of Lymphocytes
This involves mechanisms where lymphocytes are produced but are then rapidly destroyed or undergo programmed cell death (apoptosis).
Infections
Many infections can cause lymphopenia (low lymphocytes), often temporarily, through various mechanisms (direct viral infection and lysis of lymphocytes, cytokine-induced apoptosis, or redistribution).
- Viral Infections
- HIV (Human Immunodeficiency Virus): A classic cause, where the virus directly infects and destroys CD4+ T cells, leading to AIDS.
- Influenza (Flu): Common cause of acute, often transient lymphopenia (low lymphocytes).
- SARS-CoV-2 (COVID-19): Significant lymphopenia is a hallmark of moderate to severe COVID-19, often correlating with disease severity.
- Hepatitis Viruses (e.g., HBV, HCV)
- Epstein-Barr Virus (EBV): While typically causing lymphocytosis (increase), some phases or severe infections can lead to lymphopenia (low lymphocytes).
- Measles: Can cause profound and prolonged lymphopenia (low lymphocytes) due to direct infection and destruction of lymphocytes.
- Bacterial Infections
- Sepsis/Severe Bacterial Infections: The systemic inflammatory response can lead to massive lymphocyte apoptosis and redistribution.
- Tuberculosis (especially miliary TB)
- Other Infections: Fungal infections (e.g., histoplasmosis) and parasitic infections (e.g., malaria) can also cause lymphopenia.
Autoimmune Diseases
The immune system mistakenly attacks the body’s own tissues, and sometimes its own lymphocytes.
- Systemic Lupus Erythematosus (SLE): Lymphopenia (low lymphocytes) is a common feature and is often part of the diagnostic criteria. Mechanisms include anti-lymphocyte antibodies and increased apoptosis.
- Rheumatoid Arthritis (RA)
- Myasthenia Gravis
- Sjögren’s Syndrome
- Autoimmune Lymphoproliferative Syndrome (ALPS): A genetic disorder leading to defective lymphocyte apoptosis, paradoxically sometimes associated with lymphopenia (low lymphocytes) in certain subsets.
Medications (especially those inducing apoptosis or destruction)
- Corticosteroids (e.g., prednisone, dexamethasone): A very common cause of acute, often transient lymphopenia (low lymphocytes) due to their direct apoptotic effect on lymphocytes and redistribution into lymphoid organs.
- Certain Biologic Therapies: Some monoclonal antibodies used in cancer or autoimmune diseases (e.g., anti-thymocyte globulin, alemtuzumab, rituximab) directly deplete lymphocytes.
- Chemotherapy (again, some agents cause destruction as well as reduced production).
Radiation Therapy
Can directly destroy circulating lymphocytes.
Redistribution of Lymphocytes
Lymphocytes are temporarily moved out of the peripheral blood into other lymphoid tissues or organs.
- Acute Stress (e.g., severe trauma, major surgery, burns, critical illness): The body’s acute stress response, often involving elevated cortisol levels, can cause lymphocytes to redistribute from the bloodstream into the lymphoid organs, leading to transient lymphopenia (low lymphocytes) in the peripheral blood.
- Corticosteroid Use: As mentioned, corticosteroids not only induce apoptosis but also cause redistribution of lymphocytes (especially T cells) into lymphoid tissues.
- Anaphylaxis/Severe Allergic Reactions: Can cause transient redistribution.
Loss of Lymphocytes
This involves the physical loss of lymphocytes from the body.
- Protein-Losing Enteropathy: Conditions that cause significant protein loss from the gastrointestinal tract can also lead to the loss of lymphocytes, as lymphocytes circulate through the gut-associated lymphoid tissue (GALT). Examples include severe inflammatory bowel disease (Crohn’s disease, ulcerative colitis) or intestinal lymphangiectasia.
- Chylothorax/Chylous Ascites: Leakage of lymphatic fluid (chyle), which is rich in lymphocytes, into the pleural or peritoneal cavity.
Idiopathic Lymphopenia
In some cases, despite a thorough investigation, no clear cause for lymphopenia (low lymphocytes) can be identified. This is termed idiopathic lymphopenia (low lymphocytes). Sometimes, specific subsets of lymphocytes, like CD4+ T cells, may be low without an apparent underlying cause (idiopathic CD4+ lymphocytopenia).
Signs and Symptoms of Lymphopenia
Lymphopenia (low lymphocytes) itself often doesn’t have specific, direct symptoms. Instead, the signs and symptoms related to lymphopenia (low lymphocytes) usually stem from two main sources.
- The consequences of a weakened immune system (due to the low lymphocyte count), primarily an increased susceptibility to infections.
- The underlying disease or condition that is causing the lymphopenia (low lymphocytes).
Signs and Symptoms Due to Compromised Immune Function (Consequences of Lymphopenia)
When lymphocyte counts are significantly low, especially for prolonged periods, the body’s ability to mount an effective immune response is impaired.
- Increased Susceptibility to Infections: This is the most common and significant clinical manifestation. Patients with lymphopenia are prone to:
- Recurrent Infections
- Severe Infections
- Opportunistic Infections: Infections caused by microorganisms that usually don’t cause disease in people with healthy immune systems (e.g., Pneumocystis jirovecii pneumonia, cytomegalovirus – CMV, atypical mycobacteria, fungal infections like candidiasis).
- Unusual Pathogens: Infections with less common or rare pathogens.
- Poor Response to Treatment
- Specific Infection Patterns:
- Viral Infections: Often recurrent or severe herpes simplex, varicella-zoster (shingles), CMV, EBV.
- Fungal Infections: Oral thrush (candidiasis), invasive aspergillosis, cryptococcosis.
- Bacterial Infections: Atypical pneumonia, persistent skin infections.
- Failure to Thrive (in children): In infants and young children with severe congenital lymphopenia (e.g., SCID), recurrent infections can lead to poor growth and development.
- Increased Risk of Malignancies: Lymphocytes play a crucial role in immune surveillance, identifying and eliminating abnormal cells before they develop into cancers. Chronic or severe lymphopenia (low lymphocytes) can increase the risk of certain cancers, particularly:
- Lymphomas: Non-Hodgkin lymphoma.
- Skin Cancers: Especially squamous cell carcinoma.
- Virally-associated Cancers: e.g., Kaposi’s sarcoma (associated with HHV-8 in HIV patients), EBV-associated lymphomas.
Signs and Symptoms Related to the Underlying Cause of Lymphopenia
In many cases, the patient’s presenting symptoms are actually due to the primary condition causing the lymphopenia, rather than the low lymphocyte count itself. Therefore, a comprehensive history and physical examination are essential.
- Systemic Illnesses/Chronic Diseases
- Fatigue, Weight Loss, Malaise: General symptoms often seen in chronic infections (e.g., HIV, tuberculosis), autoimmune diseases (e.g., SLE), or malignancies.
- Fever: Suggests infection or inflammatory processes.
- Generalized Weakness
- Autoimmune Diseases
- Joint Pain and Swelling (Arthralgia/Arthritis): Common in SLE, rheumatoid arthritis.
- Skin Rashes: Malar rash (butterfly rash) in SLE, photosensitivity.
- Hair Loss: In SLE.
- Dry Eyes/Mouth: In Sjögren’s syndrome.
- Organ-specific Symptoms: Depending on the organ system affected by the autoimmune process (e.g., nephritis in SLE).
- Infections
- Specific Symptoms of the Infection: Cough, shortness of breath (pneumonia), diarrhea (gastroenteritis), skin lesions (viral exanthems, fungal infections).
- Lymphadenopathy (swollen lymph nodes) or Splenomegaly (enlarged spleen): Can be present in some infections (e.g., HIV, EBV) or lymphomas.
- Malignancies
- Unexplained Weight Loss
- Night Sweats
- Persistent Fever
- Fatigue
- Easy Bruising/Bleeding or Pallor: If bone marrow is affected (due to other cytopenias).
- Swollen Lymph Nodes (non-tender, firm)
- Drug-Induced Lymphopenia
- Often asymptomatic, detected incidentally on routine blood tests.
- Symptoms might appear if the lymphopenia (low lymphocytes) is severe enough to cause infections.
- Congenital Immunodeficiencies (in infants/children)
- Recurrent Severe Infections from early age: Often with unusual pathogens.
- Chronic Diarrhea
- Failure to gain weight/grow (Failure to Thrive)
- Skin Rashes/Eczema
- Unusual Facial Features/Developmental Delay: (e.g., DiGeorge syndrome).
Laboratory Investigations for Lymphopenia (Low Lymphocytes)
Laboratory investigations for lymphopenia (low lymphocytes) are crucial for confirming the diagnosis, determining the severity, and, most importantly, identifying the underlying cause. A systematic approach is typically followed, starting with basic blood tests and progressing to more specialized investigations based on clinical suspicion.
Initial Diagnostic Workup
Complete Blood Count (CBC) with Differential
This is the foundational test. It provides the Absolute Lymphocyte Count (ALC), which is the direct measurement used to diagnose lymphopenia (low lymphocytes). It also gives counts for other white blood cells (neutrophils, monocytes, eosinophils, basophils), red blood cells, and platelets.
- Interpretation
- Absolute Lymphocyte Count (ALC): An ALC below the age-specific normal range (e.g., typically <1.0 x 109/L in adults) confirms lymphopenia (low lymphocytes).
- Other Cell Lines: Look for concomitant cytopenias (anemia, thrombocytopenia, neutropenia) which might point to bone marrow suppression or a systemic process affecting multiple cell lines.
- Other WBC Trends: An elevated neutrophil count (neutrophilia) with a low lymphocyte percentage could indicate relative lymphopenia (as discussed previously), common in acute infections or stress. Atypical lymphocytes may also be noted, suggestive of viral infections (e.g., dengue, EBV, CMV).
Peripheral Blood Smear Review
A manual microscopic examination of the blood smear by a hematologist or trained technologist.
- Interpretation
- Morphology of Lymphocytes: Can reveal abnormal lymphocyte shapes (e.g., atypical lymphocytes in viral infections like CMV or EBV, or large granular lymphocytes which can be associated with certain disorders).
- Other Cell Abnormalities: Presence of immature cells (blasts), dysplastic features, or abnormal inclusions in other cell lines can point to underlying bone marrow disorders or hematological malignancies.
- Parasites: Rarely, intracellular parasites might be seen.
Targeted Investigations (Based on Clinical Suspicion)
Once lymphopenia (low lymphocytes) is confirmed, the next steps are guided by the patient’s history, physical examination, and initial CBC findings to determine the cause.
To Assess Immune Status and Lymphocyte Subsets
Lymphocyte Subset Analysis (Flow Cytometry)
This test helps identify which specific lymphocyte subset is deficient, narrowing down the potential causes (e.g., isolated CD4 lymphopenia in HIV, pan-lymphopenia in severe SCID, or selective B cell deficiency). It is essential for diagnosing HIV, congenital immunodeficiencies, certain autoimmune lymphoproliferative disorders, and monitoring patients on immunosuppressive therapies.
This is a critical test that quantifies specific populations of lymphocytes.
- CD3+ T cells (total T cells)
- CD4+ T cells (Helper T cells)
- CD8+ T cells (Cytotoxic T cells)
- CD19+/CD20+ B cells (total B cells)
- CD16+/CD56+ Natural Killer (NK) cells
Immunoglobulin Levels (IgG, IgA, IgM)
This test measures the levels of antibodies produced by B cells. Low levels (hypogammaglobulinemia) can indicate impaired B cell function or loss, and may be associated with conditions like CVID or severe combined immunodeficiencies, especially when combined with B cell lymphopenia.
Vaccine Titers/Specific Antibody Responses
This test assesses the functional capacity of the adaptive immune system to produce antibodies in response to specific antigens (e.g., tetanus, diphtheria, pneumococcal polysaccharide vaccine). Failure to mount an appropriate antibody response despite vaccination suggests a functional defect in B cell immunity.
Lymphocyte Proliferation Assays
This test measures the ability of T cells to proliferate (multiply) in response to mitogens (non-specific activators) or specific antigens. Reduced proliferation indicates a functional defect in T cells, often seen in various immunodeficiencies.
To Investigate Specific Underlying Causes
Infection Screening
- HIV testing (e.g., HIV-1/2 antibody and p24 antigen combination immunoassay): Mandatory given HIV is a classic cause of CD4 lymphopenia.
- Viral Serologies: For CMV, EBV, Hepatitis viruses, Measles, SARS-CoV-2 (COVID-19), etc., based on clinical suspicion.
- Tuberculosis (TB) Testing: (e.g., Tuberculin Skin Test – TST, Interferon-Gamma Release Assay – IGRA) if TB is suspected.
- Cultures (blood, urine, sputum, CSF): If active infection is suspected.
Autoimmune Markers
- Antinuclear Antibodies (ANA): Screening test for various autoimmune diseases like SLE.
- Anti-dsDNA, Anti-Sm, Anti-Ro/SSA, Anti-La/SSB: Specific antibodies for SLE and Sjögren’s syndrome.
- Rheumatoid Factor (RF), Anti-CCP antibodies: For rheumatoid arthritis.
Bone Marrow Aspiration and Biopsy
Indicated if there is suspicion of a primary bone marrow disorder (aplastic anemia, MDS, leukemia, lymphoma infiltration) or unexplained pancytopenia.
Imaging Studies
- Chest X-ray (CXR) or CT scan: To look for thymic abnormalities (e.g., in DiGeorge syndrome), opportunistic infections (e.g., Pneumocystis pneumonia), or signs of malignancy (lymphadenopathy, masses).
- Abdominal/Pelvic CT or Ultrasound: To assess for lymphadenopathy, splenomegaly, or signs of protein-losing enteropathy.
Genetic Testing
For suspected congenital immunodeficiencies (e.g., SCID panels, DiGeorge syndrome deletion analysis).
Gastrointestinal Workup
If protein-losing enteropathy or severe inflammatory bowel disease is suspected.
Medication Review
A thorough review of all current and recent medications is crucial, as many drugs can cause lymphopenia. This isn’t a lab test, but often the first “investigation” that yields a diagnosis.
The laboratory investigation of lymphopenia (low lymphocytes) is an iterative process, guided by the clinical context. It requires careful consideration of the patient’s age, symptoms, medical history, and risk factors to select the most appropriate and cost-effective tests.
Treatment and Management of Lymphopenia
The treatment and management of lymphopenia (low lymphocytes) are highly dependent on its underlying cause and the severity of the immune compromise. Since lymphopenia (low lymphocytes) is often a manifestation of another condition, addressing the primary problem is paramount.
Addressing the Underlying Cause (Primary Treatment)
This is the most critical aspect of managing lymphopenia (low lymphocytes). Eliminating or controlling the root cause will often lead to a resolution or improvement of the lymphocyte count.
Discontinuation or Modification of Offending Medications
- Corticosteroids: If lymphopenia (low lymphocytes) is due to corticosteroids, gradual tapering (if clinically feasible) may help lymphocyte counts recover. However, the benefits of the corticosteroid for the underlying condition (e.g., severe inflammation) must be weighed against the risks of lymphopenia (low lymphocytes).
- Immunosuppressants/Chemotherapy: For patients undergoing these treatments, lymphopenia (low lymphocytes) is often an expected side effect. Dosage adjustments or temporary cessation may be necessary if lymphopenia (low lymphocytes) is severe or leads to complications, but this must be managed by the treating oncologist or transplant physician.
- Biologic Therapies: Certain biologics (e.g., alemtuzumab, rituximab) directly deplete lymphocytes. Management involves monitoring and prophylactic measures.
Treatment of Underlying Infections
- Antiretroviral Therapy (ART) for HIV: Effective ART can significantly increase CD4+ T cell counts in HIV-infected individuals, improving their immune function.
- Antiviral, Antibacterial, Antifungal, or Antiparasitic Medications: Treating active infections (e.g., severe bacterial sepsis, specific viral infections like CMV, or fungal infections) can lead to resolution of infection-induced lymphopenia (low lymphocytes).
Management of Autoimmune Diseases
Controlling the autoimmune disease with appropriate immunosuppressive or immunomodulatory therapy (e.g., for SLE, rheumatoid arthritis) can often lead to an improvement in lymphocyte counts that were affected by the disease itself.
Treatment of Malignancies
Chemotherapy, radiation therapy, immunotherapy, or stem cell transplantation for leukemias, lymphomas, or other cancers that cause lymphopenia will be aimed at eradicating the malignancy, which may indirectly or directly improve lymphocyte counts.
Correction of Nutritional Deficiencies
Addressing severe protein-energy malnutrition or specific micronutrient deficiencies (e.g., zinc, vitamin B12, folic acid) can help restore lymphocyte production.
Management of Other Chronic Diseases
Optimizing management of conditions like end-stage kidney disease or inflammatory bowel disease can indirectly improve immune function and lymphocyte counts.
Supportive Care and Prophylactic Measures (Mitigating Consequences)
These strategies aim to protect the patient from the consequences of lymphopenia (low lymphocytes), especially increased susceptibility to infections.
Prophylactic Antimicrobials
- Antiviral Prophylaxis: For patients at high risk (e.g., post-transplant, severe T-cell lymphopenia), antiviral medications (e.g., acyclovir for herpes simplex/zoster, ganciclovir for CMV) may be prescribed.
- Antifungal Prophylaxis: For severe lymphopenia, especially T-cell deficiency, prophylaxis against fungal infections like Pneumocystis jirovecii pneumonia (PJP) with trimethoprim-sulfamethoxazole (Bactrim) is common. Other antifungals may be used for other specific fungal risks.
- Antibacterial Prophylaxis: Less common than antiviral or antifungal but may be considered for specific bacterial risks in severely immunocompromised patients.
Immunoglobulin Replacement Therapy (IVIG or SCIG)
Indicated if lymphopenia (low lymphocytes) is accompanied by hypogammaglobulinemia (low antibody levels) and recurrent bacterial infections. It provides passive immunity by supplying exogenous antibodies, thereby reducing the risk of bacterial infections. It does not increase lymphocyte counts.
Granulocyte Colony-Stimulating Factor (G-CSF)
While primarily used to increase neutrophil counts (e.g., in neutropenia following chemotherapy), G-CSF is generally not used to increase lymphocyte counts. However, in the context of bone marrow suppression affecting all cell lines, it might be part of the overall supportive care.
Nutritional Support
Ensuring adequate nutrition is crucial for immune function, particularly in patients with chronic illness or malignancy.
Vaccinations
- Killed/Inactivated Vaccines: Generally safe for most lymphopenic patients and should be administered if appropriate to reduce the risk of vaccine-preventable diseases.
- Live Attenuated Vaccines: Generally contraindicated in patients with severe lymphopenia due to the risk of vaccine-induced infection (e.g., MMR, varicella, live attenuated influenza vaccine, rotavirus). This decision must be carefully made by an immunologist.
Infection Control Measures
- Hand Hygiene: Emphasizing strict hand hygiene for patients and caregivers.
- Avoiding Crowds/Sick Individuals: Reducing exposure to infectious agents.
- Masking: May be recommended in high-risk environments.
- Dietary Precautions: Avoiding raw or undercooked foods in severely immunocompromised patients.
Specific Therapeutic Interventions (for Severe Cases)
- Hematopoietic Stem Cell Transplantation (HSCT): The definitive treatment for severe congenital immunodeficiencies (e.g., SCID) and some severe acquired bone marrow failures or hematologic malignancies.
- Gene Therapy: For specific genetic immunodeficiencies, gene therapy aims to correct the underlying genetic defect in the patient’s own cells, leading to functional lymphocyte production. This is still largely experimental but has shown success in certain SCID types.
- Thymic Transplantation: For severe T-cell lymphopenia due to thymic aplasia (e.g., complete DiGeorge syndrome), transplantation of thymic tissue can help restore T-cell development. This is a highly specialized procedure.
Monitoring
- Serial CBC with Differential: Regular monitoring of the ALC is essential to assess the response to treatment and detect any worsening.
- Lymphocyte Subset Analysis: May be repeated to track specific lymphocyte populations, especially CD4+ T cells in HIV or after stem cell transplant.
- Clinical Surveillance: Close monitoring for signs and symptoms of infection or complications of the underlying disease.
Frequently Asked Questions (FAQ)
Is lymphopenia life threatening?
While mild or transient lymphopenia (low lymphocytes) may not pose an immediate threat, severe and/or persistent lymphopenia is a serious concern because it indicates a significantly compromised immune system, making the individual highly susceptible to life-threatening infections and increasing the risk of certain cancers. The prognosis and severity depend heavily on the underlying cause and the extent of the lymphocyte reduction.
What are the different gradings of lymphopenia (low lymphocytes)?
CTCAE Grading for Lymphopenia (Low Lymphocytes)
| CTCAE Grade | Absolute Lymphocyte Count (ALC) | Description (General CTCAE) | Clinical Significance |
| Normal | Typically 1.0−4.8×109/L | – | Healthy immune function. |
| Grade 1 | < LLN (Lower Limit of Normal) to 0.8×109/L | Asymptomatic or mild symptoms; clinical or diagnostic observations only; no intervention indicated. | Mild reduction; may be incidental or transient (e.g., after minor viral infection, acute stress). Generally not associated with significant immediate risk of infection. |
| Grade 2 | <0.8×109/L to 0.5×109/L | Moderate; minimal, local, or noninvasive intervention indicated; limiting instrumental ADL. | Moderate reduction. Increased vigilance for infections advised. May prompt initial investigations into underlying cause. |
| Grade 3 | <0.5×109/L to 0.2×109/L | Severe or medically significant but not immediately life-threatening; hospitalization or prolongation of hospitalization indicated; disabling; limiting self-care ADL. | Severe reduction. Significantly increased risk of serious, opportunistic infections. Often requires medical intervention, such as dose modification of causative agents (e.g., chemotherapy) and/or initiation of prophylactic antimicrobials. A common threshold for clinical concern in oncology. |
| Grade 4 | ≤0.2×109/L | Life-threatening consequences; urgent intervention indicated. | Profound and life-threatening reduction. Places patient at extremely high risk for overwhelming, severe, and potentially fatal infections. Requires urgent and aggressive medical management, including source identification, broad-spectrum prophylactic antibiotics, and potentially admission. |
| Grade 5 | Death | Death related to the adverse event. | The lymphopenia directly led to the patient’s death (usually due to severe infection or complications of the underlying cause). |
Can stress cause lymphopenia?
Yes, stress can cause a temporary and often mild form of lymphopenia (low lymphocytes). This is a well-documented physiological response to both physical and psychological stress.
Can lack of sleep cause lymphopenia?
Yes, lack of sleep can cause lymphopenia (low lymphocytes), but the effect is often temporary and part of a broader impact on the immune system. The primary way that a lack of sleep affects lymphocyte count is by disrupting the body’s normal regulatory systems, particularly hormonal balance and circadian rhythms.
Can exercise cause lymphopenia?
Yes, exercise, particularly intense or prolonged exercise, can cause a temporary and expected decrease in the number of circulating lymphocytes. This is a normal physiological response to physical stress and is not typically a cause for concern.
Can not eating enough cause low lymphocytes?
Yes, not eating enough, particularly in the case of severe or long-term malnutrition, is a well-established cause of a low lymphocyte count. Lymphopenia (low lymphocytes) caused by nutritional deficiencies is a form of acquired immunodeficiency, which is one of the most common causes of immune system dysfunction worldwide.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Janeway CA Jr, Travers P, Walport M, et al. Immunobiology: The Immune System in Health and Disease. 5th edition. New York: Garland Science; 2001. Generation of lymphocytes in bone marrow and thymus. Available from: https://www.ncbi.nlm.nih.gov/books/NBK27123/
- Warny, M., Helby, J., Nordestgaard, B. G., Birgens, H., & Bojesen, S. E. (2020). Incidental lymphopenia and mortality: a prospective cohort study. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne, 192(2), E25–E33. https://doi.org/10.1503/cmaj.191024
- Warny, M., Helby, J., Nordestgaard, B. G., Birgens, H., & Bojesen, S. E. (2018). Lymphopenia and risk of infection and infection-related death in 98,344 individuals from a prospective Danish population-based study. PLoS medicine, 15(11), e1002685. https://doi.org/10.1371/journal.pmed.1002685
- Silzle, T., Blum, S., Schuler, E. et al. Lymphopenia at diagnosis is highly prevalent in myelodysplastic syndromes and has an independent negative prognostic value in IPSS-R-low-risk patients. Blood Cancer J. 9, 63 (2019). https://doi.org/10.1038/s41408-019-0223-7
- Zidar DA, Al-Kindi SG, Liu Y, et al. Association of Lymphopenia With Risk of Mortality Among Adults in the US General Population. JAMA Netw Open. 2019;2(12):e1916526. doi:10.1001/jamanetworkopen.2019.16526
- Guo, Z., Zhang, Z., Prajapati, M., & Li, Y. (2021). Lymphopenia Caused by Virus Infections and the Mechanisms Beyond. Viruses, 13(9), 1876. https://doi.org/10.3390/v13091876
- Wang, Z., Zhang, W., Chen, L. et al. Lymphopenia in sepsis: a narrative review. Crit Care 28, 315 (2024). https://doi.org/10.1186/s13054-024-05099-4



