TL;DR
Eosinophils are white blood cells that play a crucial role in the immune system. They are characterized by their distinctive bilobed nucleus and large, eosinophilic granules.
Functions ▾
- Combating parasitic infections: Eosinophils release toxic substances that kill parasites.
- Allergic reactions: They are involved in allergic responses, such as asthma and allergic rhinitis.
- Tissue repair: They help in tissue repair and remodeling.
Eosinophilia ▾ and Eosinopenia ▾
- Eosinophilia: An elevated eosinophil count can be indicative of various conditions, including parasitic infections, allergic diseases, and hematological disorders.
- Eosinopenia: A decreased eosinophil count can be associated with factors such as corticosteroid use, stress, infections, and hematological disorders.
Laboratory Investigations ▾
- Complete blood count (CBC) with differential: Used to assess eosinophil count and percentage.
- Peripheral blood smear: Visualizes eosinophils and other blood cells.
- Bone marrow examination: May be necessary to evaluate eosinophil production in certain cases.
Eosinophil-Associated Disorders ▾
- Eosinophils can be involved in various inflammatory conditions, such as eosinophilic esophagitis and eosinophilic pneumonia.
*Click ▾ for more information
Introduction
Eosinophils are white blood cells that play a crucial role in the immune system. They are characterized by their distinctive bilobed nucleus and large, eosinophilic granules. The granules contain various enzymes and proteins that are involved in the eosinophil’s functions.
Eosinophils are primarily associated with:
- Combating parasitic infections: They release toxic substances that kill parasites.
- Allergic reactions: They are involved in allergic responses, such as asthma and allergic rhinitis.
Overview of the Immune System and Its Components
The immune system is a complex network of cells, tissues, and organs that work together to protect the body from harmful pathogens, such as bacteria, viruses, fungi, and parasites. It is divided into two main components.
Innate (Non-specific) Immunity
- First line of defense: Physical barriers like skin and mucous membranes
- Cellular components: Neutrophils, monocytes, macrophages, natural killer cells
- Humoral components: Complement system, acute-phase proteins
Adaptive (Specific) Immunity
- Humoral immunity: B cells produce antibodies to target specific antigens
- Cell-mediated immunity: T cells (helper T cells and cytotoxic T cells) directly attack infected cells
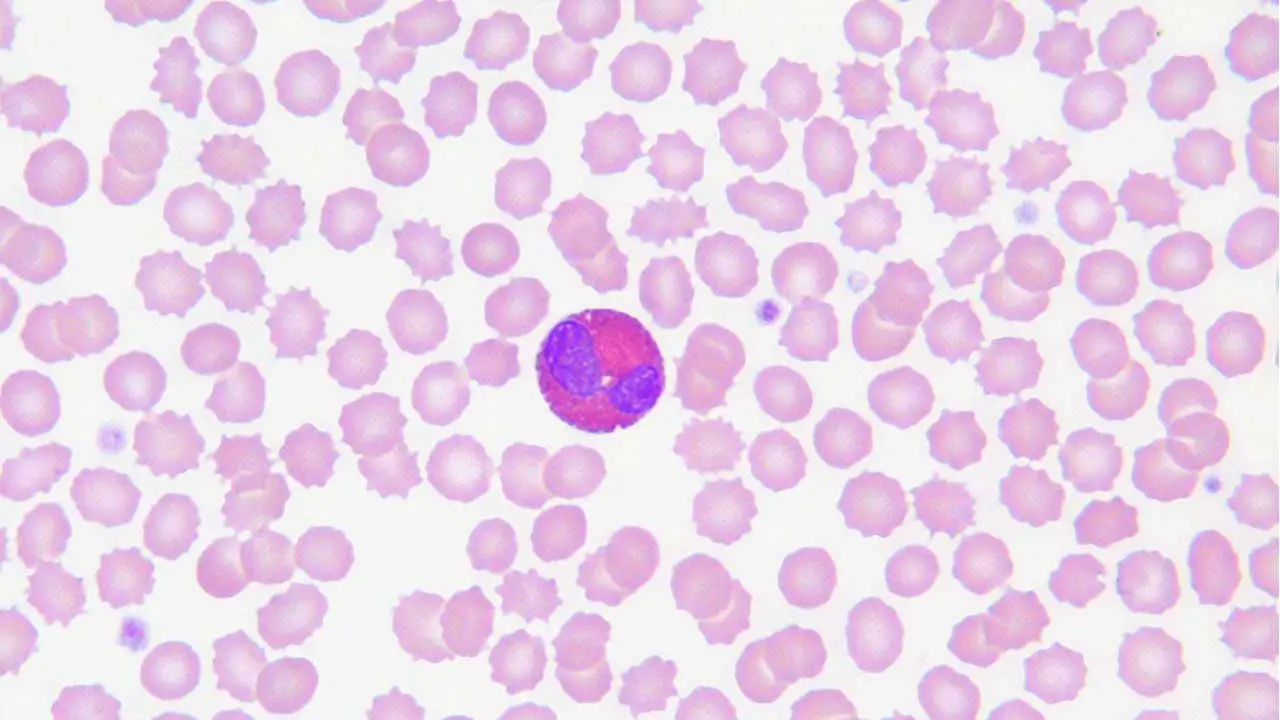
Morphology of Eosinophils
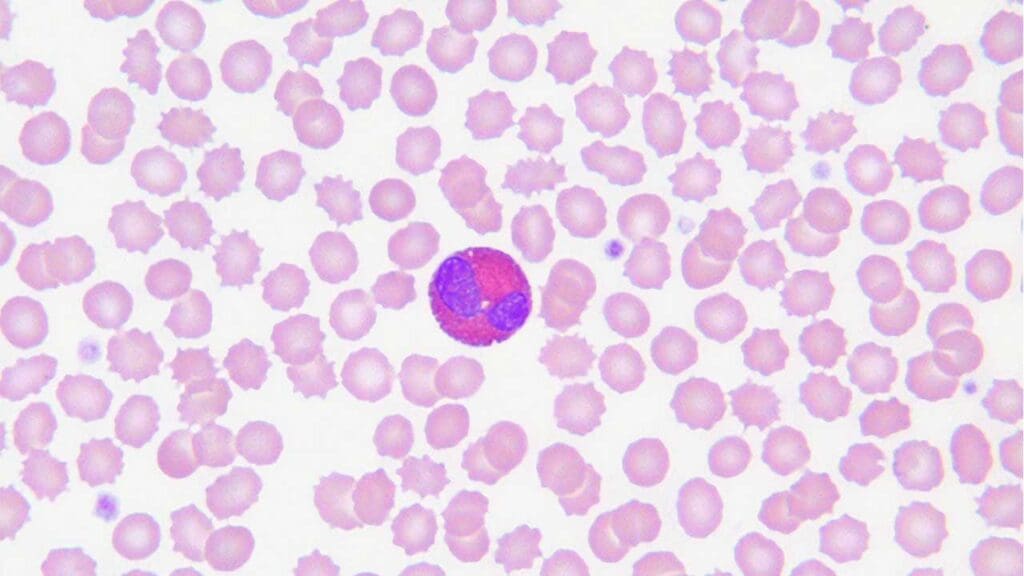
Eosinophils are easily recognizable due to their distinctive morphology. They have a bilobed nucleus, which means the nucleus is divided into two lobes connected by a thin strand of chromatin. This bilobed shape is a characteristic feature of eosinophils and helps to differentiate them from other white blood cells.
Another prominent feature of eosinophils is their large, eosinophilic granules. These granules are filled with various enzymes and proteins that play a crucial role in the eosinophil’s functions. The term “eosinophilic” refers to the granules’ affinity for eosin stains, which causes them to appear red or pink under the microscope.
Role of Granules in Eosinophil Function
The granules in eosinophils contain a variety of substances, including:
- Major basic protein (MBP): This is a highly toxic protein that is particularly effective against helminths. It can disrupt the parasite’s cell membranes and cause cell death.
- Eosinophil cationic protein (ECP): Another toxic protein with antiparasitic and cytotoxic properties.
- Eosinophil peroxidase (EPO): An enzyme involved in the production of reactive oxygen species, which can damage cells and kill parasites.
- Histaminase: An enzyme that breaks down histamine, a key mediator of allergic reactions.
These granules play a vital role in eosinophil function, particularly in:
- Combating parasitic infections: MBP and ECP are released from the granules to kill parasites.
- Allergic reactions: Eosinophils can release histamine and other mediators of allergic reactions. However, they also produce histaminase, which can help to regulate allergic responses.
Lifespan in Blood and Reference Range
Eosinophils have a relatively short lifespan in the bloodstream compared to other white blood cells. They typically circulate for 8-18 hours before migrating to tissues. In the tissues, eosinophils typically survive from 2 – 5 days, depending on the tissue. This shorter lifespan is likely due to their active role in immune responses and their susceptibility to damage.
Normal Reference Range for Eosinophils
The normal reference range for eosinophils in the blood can vary slightly depending on the laboratory and the specific population being tested. However, a typical range is 100-400 eosinophils per microliter (cells/μL).
Function of Eosinophils
Eosinophils and Parasitic Infections
Eosinophils play a crucial role in combating parasitic infections, particularly those caused by helminths (intestinal worms). Their primary function in this context is to release toxic proteins that can damage and kill parasites.
Eosinophils are often found in tissues infected with parasites, where they can directly attack and destroy the invaders.
Eosinophils and Allergic Reactions
Eosinophils are also involved in allergic reactions, such as asthma and allergic rhinitis. While they are typically associated with inflammation, they can also play a role in regulating allergic responses.
- Histamine release: Eosinophils can release histamine, a substance involved in allergic reactions. However, they also contain histaminase, an enzyme that breaks down histamine, which can help to limit the severity of allergic symptoms.
- Other mediators: Eosinophils can release other mediators, such as leukotrienes and prostaglandins, that contribute to allergic inflammation.
- Tissue damage: Chronic eosinophilic inflammation can lead to tissue damage, as seen in conditions like asthma and eosinophilic esophagitis.
Eosinopoiesis
Eosinophils, like other white blood cells, originate from hematopoietic stem cells in the bone marrow. The process of eosinophil development, known as eosinopoiesis, involves several stages.
Stages of Eosinopoiesis
- Hematopoietic stem cell: The process begins with a hematopoietic stem cell, which has the potential to differentiate into all types of blood cells.
- Common myeloid progenitor: The hematopoietic stem cell differentiates into a common myeloid progenitor.
- Basophil/eosinophil progenitor: The common myeloid progenitor gives rise to a basophil/eosinophil progenitor.
- Eosinophilic colony-forming unit (CFU-eo): The basophil/eosinophil progenitor further differentiates into an eosinophilic colony-forming unit.
- Eosinophilic blast: The CFU-eo develops into an eosinophilic blast.
- Promyelocyte: The eosinophilic blast matures into a promyelocyte.
- Myelocyte: The promyelocyte becomes a myelocyte, which is characterized by the appearance of specific granules.
- Metamyelocyte: The myelocyte develops into a metamyelocyte.
- Band cell: The metamyelocyte matures into a band cell, which has a horseshoe-shaped nucleus.
- Mature eosinophil: The band cell finally differentiates into a mature eosinophil, with its characteristic bilobed nucleus and large, eosinophilic granules.
Factors Regulating Eosinophil Production
Several factors can influence the production of eosinophils, including:
- Interleukins: Interleukin-5 (IL-5) is a key cytokine that promotes eosinophil development and survival. Other interleukins, such as IL-3 and GM-CSF, can also contribute to eosinophil production.
- Growth factors: Growth factors like granulocyte-macrophage colony-stimulating factor (GM-CSF) can stimulate the proliferation and differentiation of eosinophils.
- Hormones: Corticosteroids can suppress eosinophil production, while certain hormones, such as thyroid hormones, may influence eosinophil levels.
- Infections and allergens: Parasitic infections and allergic reactions can lead to increased eosinophil production as part of the immune response.
- Hematopoietic disorders: Certain hematological disorders, such as eosinophilic leukemia, can result in excessive eosinophil production.
Causes of High Eosinophils (Eosinophilia)
Eosinophilia, an elevated eosinophil count in the blood, can be caused by a variety of factors. Here are some of the most common causes:
Parasitic Infections
Eosinophils play a crucial role in combating parasitic infections, particularly those caused by helminths (intestinal worms). When the body is infected with parasites, the immune system responds by increasing the production of eosinophils to help eliminate the invaders. Some examples of parasitic infections that can cause eosinophilia include:
- Hookworm
- Strongyloides
- Ascaris
- Trichinella
- Schistosomiasis
- Toxocara
Allergic Diseases
Allergic diseases, such as asthma, allergic rhinitis, and atopic dermatitis, can also lead to eosinophilia. In these conditions, the immune system overreacts to allergens, leading to inflammation and increased eosinophil production.
- Asthma: A chronic respiratory condition characterized by airway inflammation and narrowing.
- Allergic rhinitis: A condition characterized by nasal inflammation and symptoms such as sneezing, runny nose, and itchy eyes.
- Atopic dermatitis: A skin condition characterized by itchy, red, and inflamed skin.
Drug Reactions
Certain drugs can cause eosinophilia as a side effect. These drugs may include:
- Antibiotics (e.g., penicillin, sulfa drugs)
- Anticonvulsants (e.g., phenytoin, carbamazepine)
- Anti-inflammatory drugs (e.g., nonsteroidal anti-inflammatory drugs, corticosteroids)
- Antihistamines
- Anti-thyroid drugs
Hematological Disorders
Eosinophilia can also be a sign of certain hematological disorders, such as:
- Eosinophilic leukemia: A rare type of leukemia characterized by the abnormal proliferation of eosinophils.
- Chronic myelomonocytic leukemia (CMML): A myeloproliferative disorder that can involve eosinophilia.
- Polycythemia vera: A disorder characterized by an overproduction of red blood cells, which can also lead to increased eosinophil production.
Inflammatory Conditions
Inflammatory conditions can also contribute to eosinophilia. Examples include:
- Vasculitis: A group of diseases characterized by inflammation of blood vessels.
- Rheumatoid arthritis: An autoimmune disease characterized by joint inflammation.
- Systemic lupus erythematosus (SLE): An autoimmune disease that can affect multiple organs.
Other Causes
Other potential causes of eosinophilia include:
- Endocrine disorders: Conditions such as hyperthyroidism and adrenal insufficiency can affect eosinophil production.
- Infections: Certain infections, such as viral infections, can cause eosinophilia.
- Stress: Psychological stress can influence the immune system and lead to eosinophilia.
Causes of Low Eosinophils (Eosinopenia)
Eosinopenia, a decrease in the number of eosinophils in the blood, can be caused by various factors. Here are some of the most common causes:
Corticosteroid Use
Corticosteroids are a class of drugs that can suppress the immune system, including the production of eosinophils. This is why corticosteroids are often used to treat conditions with eosinophilia, such as asthma and allergic rhinitis. However, prolonged use of corticosteroids can lead to eosinopenia.
Stress
Psychological stress can have a significant impact on the immune system, including the production of eosinophils. Studies have shown that acute stress can lead to a decrease in eosinophil counts. Chronic stress may also contribute to eosinopenia.
Infections
Certain infections, particularly acute bacterial infections, can cause eosinopenia. This is thought to be due to the release of inflammatory mediators that can suppress eosinophil production.
Hematological Disorders
- Aplastic anemia: A condition characterized by the failure of bone marrow to produce blood cells.
- Hypereosinophilic syndrome: A rare condition characterized by an abnormally high number of eosinophils in the blood.
- Paroxysmal nocturnal hemoglobinuria (PNH): A rare blood disorder that can lead to the destruction of red blood cells, as well as other blood cells.
Other Causes
- Hypereosinophilic syndrome: A condition characterized by an abnormally high number of eosinophils in the blood and tissues. Paradoxically, this can sometimes lead to eosinopenia due to the increased consumption of eosinophils.
- Hypothyroidism: A condition characterized by an underactive thyroid gland can affect eosinophil production.
- Certain medications: Some medications, such as beta-blockers and antihistamines, can have a suppressive effect on eosinophils.
Laboratory Investigations
Several laboratory tests can be used to assess eosinophil count and function.
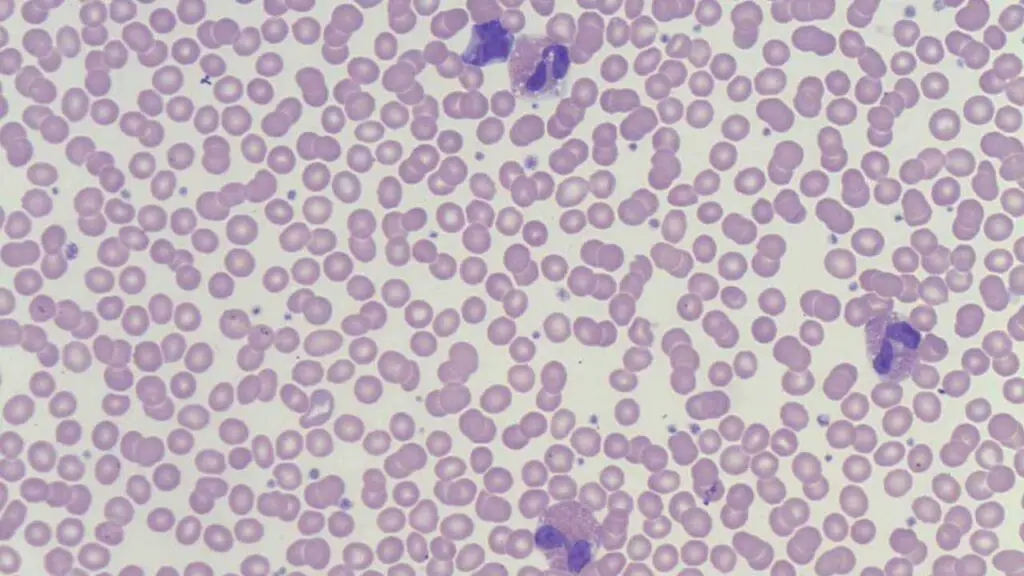
Complete Blood Count (CBC) with Differential
- Eosinophil count: This provides the absolute number of eosinophils in the blood.
- Eosinophil differential: This indicates the percentage of eosinophils among all white blood cells. The eosinophil differential count is a valuable tool for evaluating eosinophilia. It helps to determine the severity of eosinophilia and can provide clues about the underlying cause. A significantly elevated eosinophil differential count (e.g., >5%) suggests a more active inflammatory or allergic process.
Other Relevant Laboratory Tests
- Peripheral blood smear: A microscopic examination of a blood smear can help visualize eosinophils and other blood cells. It can also reveal abnormal eosinophil morphology or the presence of other blood cell abnormalities.
- Bone marrow examination: In some cases, a bone marrow biopsy may be necessary to evaluate the production of eosinophils and rule out hematological disorders.
- Specific eosinophil markers: Some laboratories may measure specific eosinophil markers, such as eosinophil cationic protein (ECP) or eosinophil peroxidase (EPO), to assess eosinophil activity.
- Allergy testing: If allergic diseases are suspected, allergy testing (e.g., skin prick tests, RAST) can be performed to identify specific allergens.
- Parasitic antigen tests: If parasitic infections are suspected, specific antigen tests can be performed to identify the causative parasite.
Eosinophil-Associated Disorders
Eosinophils play a crucial role in various inflammatory conditions, and their excessive accumulation in specific tissues can lead to a number of disorders. These conditions are collectively referred to as eosinophil-associated disorders.
Eosinophilic Esophagitis
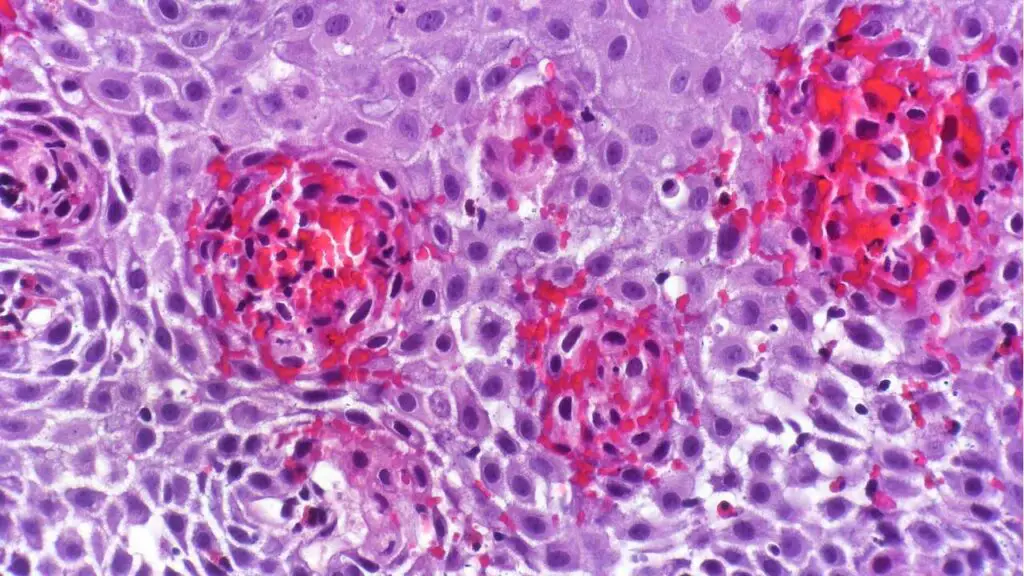
- Definition: A chronic inflammatory condition characterized by the infiltration of eosinophils into the esophageal mucosa.
- Symptoms: Difficulty swallowing, chest pain, heartburn, and food impaction.
- Diagnosis: Endoscopy with biopsy to confirm the presence of eosinophils in the esophageal tissue.
- Treatment: Often involves dietary modifications, proton pump inhibitors, or topical corticosteroids.
Eosinophilic Pneumonia
- Definition: A lung condition characterized by the accumulation of eosinophils in the lung tissue.
- Symptoms: Cough, shortness of breath, fever, and chest pain.
- Diagnosis: Chest X-ray, CT scan, and bronchoalveolar lavage to identify eosinophils in the lung tissue.
- Treatment: Often involves corticosteroids or other immunosuppressive medications.
Other Eosinophil-Associated Disorders
- Eosinophilic myocarditis: Inflammation of the heart muscle associated with eosinophil infiltration.
- Eosinophilic gastroenteritis: Inflammation of the gastrointestinal tract characterized by eosinophil accumulation.
- Eosinophilic fasciitis: A rare condition characterized by inflammation of the fascia, the connective tissue surrounding muscles.
- Eosinophilic meningitis: Inflammation of the meninges, the membranes surrounding the brain and spinal cord, associated with eosinophil infiltration.
These disorders can have varying degrees of severity and may require different treatment approaches. Understanding the role of eosinophils in these conditions is crucial for accurate diagnosis and effective management.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Valent P, Degenfeld-Schonburg L, Sadovnik I, Horny HP, Arock M, Simon HU, Reiter A, Bochner BS. Eosinophils and eosinophil-associated disorders: immunological, clinical, and molecular complexity. Semin Immunopathol. 2021 Jun;43(3):423-438. doi: 10.1007/s00281-021-00863-y. Epub 2021 May 30. PMID: 34052871; PMCID: PMC8164832.
- Tao Z, Zhu H, Zhang J, Huang Z, Xiang Z, Hong T. Recent advances of eosinophils and its correlated diseases. Front Public Health. 2022 Jul 25;10:954721. doi: 10.3389/fpubh.2022.954721. PMID: 35958837; PMCID: PMC9357997.
- Kanuru S, Sapra A. Eosinophilia. [Updated 2023 Jun 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560929/
- Ramirez GA, Yacoub MR, Ripa M, Mannina D, Cariddi A, Saporiti N, Ciceri F, Castagna A, Colombo G, Dagna L. Eosinophils from Physiology to Disease: A Comprehensive Review. Biomed Res Int. 2018 Jan 28;2018:9095275. doi: 10.1155/2018/9095275. PMID: 29619379; PMCID: PMC5829361.
- Weaver, M.D.; Glass, B.; Aplanalp, C.; Patel, G.; Mazhil, J.; Wang, I.; Dalia, S. Review of Peripheral Blood Eosinophilia: Workup and Differential Diagnosis. Hemato 2024, 5, 81-108. https://doi.org/10.3390/hemato5010008
- Cianferoni A, Spergel J. Eosinophilic Esophagitis: A Comprehensive Review. Clin Rev Allergy Immunol. 2016 Apr;50(2):159-74. doi: 10.1007/s12016-015-8501-z. PMID: 26194940.