Introduction
Macrocytic anemia is a specific type of anemia that combines two conditions: macrocytosis and anemia. Macrocytosis refers to a condition where red blood cells are larger than normal. It’s itself not a disease, but rather an abnormality detected in a blood test called a complete blood count (CBC).
During a CBC, the size of your red blood cells is measured by a value called mean corpuscular volume (MCV). If your MCV is above the normal range (usually above 100 femtoliters), it indicates macrocytosis.
In macrocytic anemia, although the bone marrow produces red blood cells, they are larger than normal and often dysfunctional. These large, abnormal cells are unable to transport oxygen efficiently, leading to the anemia symptoms.
There are two main categories of macrocytic anemia based on the underlying cause:
- Megaloblastic anemia: This is the most common type and is caused by a deficiency in vitamin B12 or folate. These vitamins are crucial for healthy red blood cell production. Deficiencies can occur due to various reasons like dietary insufficiencies, malabsorption issues, or certain medications.
- Non-megaloblastic causes: Here, the underlying cause is not related to vitamin B12 or folate deficiency. Examples include liver disease, hypothyroidism, alcoholism, or myelodysplastic syndromes (MDS).
Significance of mean cell volume (MCV)
MCV (mean corpuscular volume) plays a crucial role in diagnosing anemia by providing information about the average size of red blood cells. It’s a valuable tool because different sizes of red blood cells can indicate different types of anemia, helping guide further diagnosis and treatment.
Anemia itself refers to a deficiency of healthy red blood cells. However, there are different types of anemia depending on the size, number, and hemoglobin content of red blood cells. MCV helps categorize anemia into three main types:
- Microcytic anemia: MCV is below the normal range (usually < 80 fL), indicating smaller than normal red blood cells. This is often associated with iron deficiency anemia and thalassemia.
- Normocytic anemia: MCV falls within the normal range (typically 80-100 fL). In this case, the size of red blood cells is normal, but there might be a deficiency in their number or hemoglobin content for example in aplastic anemia or hemolytic anemia.
- Macrocytic anemia: MCV is above the normal range (> 100 fL), signifying larger than normal red blood cells. This is a key indicator for further investigation into possible megaloblastic anemia (vitamin B12 or folate deficiency) or other causes.
Megaloblastic Anemia
Megaloblastic anemia is a specific type of macrocytic anemia characterized by the presence of abnormally large, immature red blood cells called megaloblasts in the bone marrow. These large cells are functionally impaired, leading to anemia despite the increased production by the bone marrow.
Vitamin B12 Deficiency
Vitamin B12, also known as cobalamin, is an essential nutrient that plays a crucial role in various bodily functions, including:
- Red blood cell production: B12 is necessary for the synthesis of DNA, a vital component for red blood cell development.
- Nervous system function: B12 helps maintain the health of nerve fibers and their protective sheath (myelin).
- Mood regulation: B12 is involved in the production of neurotransmitters that influence mood and cognitive function.
Causes of Vitamin B12 Deficiency
- Dietary deficiency: Strict vegetarians and vegans who don’t consume B12-fortified foods or supplements are at risk. B12 naturally occurs in animal products like meat, poultry, fish, eggs, and dairy.
- Malabsorption: Conditions like pernicious anemia, Crohn’s disease, celiac disease, or surgical removal of part of the stomach or intestine can hinder B12 absorption.
- Increased B12 needs: Pregnancy, breastfeeding, and certain medications can increase the body’s demand for B12, raising the risk of deficiency if intake is inadequate.
- Age-related absorption decline: As we age, the stomach produces less intrinsic factor, a protein essential for B12 absorption.
Signs and Symptoms
Vitamin B12 deficiency can develop gradually and manifest a wide range of symptoms, some non-specific. Early detection is crucial to prevent complications. Here are some common signs and symptoms:
- Fatigue and weakness: This is a hallmark symptom due to impaired red blood cell production leading to reduced oxygen delivery to tissues.
- Macrocytic anemia: Anemia characterized by large, abnormal red blood cells.
- Pale skin: Reduced oxygen-carrying capacity of blood can cause pallor.
- Glossitis: Inflammation of the tongue, which can appear smooth, red, and painful.
- Mouth ulcers: Canker sores or mouth ulcers may develop.
- Numbness and tingling: B12 deficiency can damage nerves, causing tingling, numbness, or burning sensations in the hands and feet.
- Balance problems: Nerve damage can affect balance and coordination.
- Mood changes: Depression, anxiety, irritability, and memory problems can occur.
- Vision problems: Blurred vision or other visual disturbances may develop in severe cases.
Complications
Untreated vitamin B12 deficiency can lead to serious complications, including:
- Permanent nerve damage: This can cause irreversible neurological problems like weakness, difficulty walking, and incontinence.
- Mental health issues: Severe B12 deficiency can contribute to dementia, psychosis, or depression.
- Heart problems: An increased risk of heart disease is associated with long-term B12 deficiency.
- Pregnancy complications: B12 deficiency during pregnancy can increase the risk of birth defects in the baby.
Laboratory Investigations
Diagnosing vitamin B12 deficiency often involves a combination of tests:
- Complete blood count (CBC): Anemia with macrocytosis (elevated MCV) can be indicative of B12 deficiency.
- Peripheral blood smear: This can reveal abnormally large red blood cells (macrocytosis).
- Serum vitamin B12 level: Directly measures the amount of B12 in the blood. However, normal B12 levels don’t always rule out deficiency.
- Schilling test: This test is less commonly used now and assesses B12 absorption.
- Methylmalonic acid (MMA) and homocysteine levels: Elevated levels of these substances can indicate B12 deficiency.
Treatment and Management
The primary treatment for vitamin B12 deficiency involves replacing the missing nutrient.
- Vitamin B12 injections: This is the most common and effective way to replenish B12 stores, especially in cases of severe deficiency or malabsorption issues.
- Vitamin B12 tablets: High-dose oral B12 supplements may be prescribed for mild deficiencies or maintenance therapy after initial correction with injections.
- Dietary changes: For individuals who can consume animal products, incorporating B12-rich foods like meat, poultry, fish, eggs, and dairy into their diet becomes crucial.
- Treating underlying conditions: If a medical condition is causing B12 malabsorption, addressing that condition is also essential.
Prognosis
With early diagnosis and proper treatment, most people with vitamin B12 deficiency can recover fully. However, nerve damage caused by severe or long-standing deficiency might be irreversible. Early detection and prompt intervention are key to preventing complications.
Folate Deficiency
Folate, also known as vitamin B9, is a crucial B vitamin involved in various essential processes in the body, particularly:
- DNA synthesis and cell division: Folate plays a critical role in creating DNA, the genetic blueprint for cells. This is especially important for rapidly dividing cells like red blood cells.
- Amino acid metabolism: Folate is involved in converting certain amino acids, the building blocks of proteins, into usable forms.
- Homocysteine regulation: Folate helps regulate homocysteine levels in the blood. Elevated homocysteine has been linked to an increased risk of cardiovascular disease.
Causes of Folate Deficiency
- Dietary deficiency: Inadequate intake of folate-rich foods like leafy green vegetables, fruits, legumes, nuts, and fortified grains can lead to deficiency.
- Malabsorption: Conditions like celiac disease, Crohn’s disease, or short bowel syndrome can hinder folate absorption from food.
- Increased folate needs: Pregnancy, breastfeeding, and certain medications can increase the body’s demand for folate, raising the risk of deficiency if intake is inadequate.
- Alcohol abuse: Alcohol can interfere with folate absorption and metabolism.
Signs and Symptoms
Folate deficiency can develop gradually and cause a variety of symptoms, some overlapping with other vitamin deficiencies. Early detection and treatment are important to prevent complications. Here are some common signs and symptoms:
- Fatigue and weakness: This is a hallmark symptom due to impaired red blood cell production leading to reduced oxygen delivery to tissues.
- Macrocytic anemia: Similar to B12 deficiency, folate deficiency can also lead to anemia with large, abnormal red blood cells.
- Pale skin: Reduced oxygen-carrying capacity of blood due to anemia can cause pallor.
- Glossitis: Inflammation of the tongue, which can appear smooth, red, and painful.
- Mouth ulcers: Canker sores or mouth ulcers may develop.
- Diarrhea: Folate deficiency can sometimes cause nausea, vomiting, and diarrhea.
- Hair loss: Brittle hair and hair loss can occur.
- Neurological problems: In severe cases, folate deficiency can lead to numbness, tingling, and even neurological problems like dementia or depression.
Complications
Untreated folate deficiency can lead to serious complications, especially for pregnant women:
- Neural tube defects in babies: Folate is crucial for the proper development of the fetal neural tube, which forms the brain and spinal cord. Deficiency during pregnancy significantly increases the risk of neural tube defects like spina bifida and anencephaly.
- Increased risk of heart disease: Elevated homocysteine levels associated with folate deficiency have been linked to an increased risk of cardiovascular disease.
- Mental health issues: Severe folate deficiency can contribute to depression or cognitive decline.
Laboratory Investigations
Diagnosing folate deficiency often involves a combination of tests:
- Complete blood count (CBC): Anemia with macrocytosis (elevated MCV) can be indicative of folate deficiency.
- Peripheral blood smear: This can reveal abnormally large red blood cells (macrocytes).
- Serum folate level: Directly measures the amount of folate circulating in the blood. However, levels can be misleading due to recent dietary intake.
- Red blood cell folate level: A more accurate reflection of folate stores in the body.
Treatment and Management
The primary treatment for folate deficiency involves replenishing the missing nutrient.
- Folate supplements: Folic acid supplements are readily available and effective in treating and preventing folate deficiency.
- Dietary changes: Increasing intake of folate-rich foods like leafy green vegetables, fruits, legumes, nuts, and fortified grains is crucial for long-term management.
- Treating underlying conditions: If a medical condition is causing folate malabsorption, addressing that condition is also essential.
Prognosis
With early diagnosis and proper treatment, most people with folate deficiency recover fully. However, some neurological problems caused by severe deficiency might be irreversible. Pregnant women should prioritize sufficient folate intake to prevent birth defects in their babies.
Non-Megaloblastic Anemia
Liver Disease
Causes
- Impaired nutrient absorption: A damaged liver struggles to absorb essential vitamins like vitamin B12 and folate, crucial for healthy red blood cell production.
- Abnormal red blood cell production: Liver damage disrupts the bone marrow’s ability to produce normal-sized red blood cells.
- Increased cholesterol and phospholipids: In some liver diseases, these substances accumulate on red blood cell membranes, making them appear larger.
Signs and Symptoms
However, the underlying liver disease might present with:
- Fatigue
- Weakness
- Loss of appetite
- Nausea
- Jaundice (yellowing of skin and eyes)
- Dark urine
- Abdominal pain
Complications
- Anemia: Macrocytosis can contribute to anemia, a deficiency in red blood cells leading to fatigue and shortness of breath.
- Increased risk of infections: A compromised immune system due to liver disease can make you more susceptible to infections.
Laboratory Investigations
- Complete blood count (CBC): This test measures red blood cell size (MCV) and other parameters to identify macrocytosis and potential anemia.
- Liver function tests: These assess liver function and can indicate underlying liver damage.
- Vitamin B12 and folate levels: Low levels suggest deficiencies contributing to macrocytosis.
Treatment and Management
- Treating the underlying liver disease: The specific treatment depends on the cause of liver damage.
- Vitamin supplementation: Vitamin B12 and folate supplements can help correct deficiencies and promote healthy red blood cell production.
- Lifestyle modifications: Maintaining a healthy weight, eating a balanced diet, and avoiding alcohol can improve liver health.
Hypothyroidism
Hypothyroidism is a condition where the thyroid gland doesn’t produce enough thyroid hormones. Interestingly, hypothyroidism can be linked to macrocytosis.
Causes
The exact reason why hypothyroidism causes macrocytosis is still being researched. However, two main theories exist:
- Direct effect of thyroid hormones: Thyroid hormones seem to play a role in red blood cell production and maturation. When these hormones are deficient, red blood cells may mature incompletely, resulting in larger size.
- Vitamin B12 deficiency: Hypothyroidism can indirectly lead to vitamin B12 deficiency. This can happen because:
- Impaired stomach acid production: Low thyroid function can decrease stomach acid production, hindering vitamin B12 absorption from food.
- Autoimmune issues: Some people with hypothyroidism also have autoimmune conditions that can attack cells in the stomach, further affecting B12 absorption.
Signs and Symptoms
Macrocytosis itself often doesn’t cause specific symptoms. However, hypothyroidism can present with:
- Fatigue
- Weakness
- Weight gain or difficulty losing weight
- Feeling cold intolerance
- Dry skin
- Hair loss
- Constipation
- Irregular periods
- Depression
Complications
- Anemia: Macrocytosis can contribute to anemia, leading to fatigue and shortness of breath.
- Worsening hypothyroidism symptoms: Anemia caused by macrocytosis can further exacerbate hypothyroidism symptoms like fatigue and weakness.
Laboratory Investigations
- Thyroid function tests: These tests measure thyroid hormone levels to diagnose hypothyroidism.
- Complete blood count (CBC): This test measures red blood cell size (MCV) and other parameters to identify macrocytosis and potential anemia.
- Vitamin B12 levels: A low level suggests a deficiency that might be contributing to macrocytosis.
Treatment and Management
- Thyroid hormone replacement therapy: This is the mainstay of treatment for hypothyroidism. Synthetic thyroid hormone medication helps regulate hormone levels and alleviate symptoms.
- Vitamin B12 supplementation: If a vitamin B12 deficiency is identified, supplements can help correct it and promote healthy red blood cell production.
- Monitoring: Regular blood tests are crucial to monitor thyroid function and red blood cell health.
Alcohol Abuse
Alcohol abuse disrupts healthy red blood cell production in several ways:
- Nutrient deficiencies: Alcohol interferes with the absorption of essential vitamins, particularly vitamin B12 and folate, crucial for red blood cell production.
- Direct toxic effect: Alcohol directly damages bone marrow, the site of red blood cell production, leading to abnormal and larger cells.
- Poor nutrition: Alcoholics often have poor dietary habits, further contributing to vitamin deficiencies and impaired red blood cell production.
Signs and Symptoms
Macrocytosis itself often doesn’t cause specific symptoms. However, the underlying alcohol abuse and potential anemia (due to macrocytosis) can present with:
- Fatigue
- Weakness
- Pale skin
- Shortness of breath
- Dizziness
- Loss of appetite
- Difficulty concentrating
- Sleep problems
- Jaundice (yellowing of skin and eyes) in severe cases
Complications
- Anemia: Macrocytosis can contribute to anemia, leading to fatigue, shortness of breath, and a weakened immune system.
- Increased risk of infections: Anemia due to macrocytosis can further weaken the immune system, making you more susceptible to infections.
- Liver damage: Chronic alcohol abuse is a leading cause of liver damage, which can further worsen macrocytosis and anemia.
- Neurological problems: Alcohol abuse can damage nerves, leading to problems like numbness, tingling, and weakness.
Laboratory Investigations
- Complete blood count (CBC): This test measures red blood cell size (MCV) and other parameters to identify macrocytosis and potential anemia.
- Liver function tests: These assess liver function and can indicate underlying liver damage caused by alcohol abuse.
- Vitamin B12 and folate levels: Low levels suggest deficiencies linked to alcohol abuse and contributing to macrocytosis.
- GGT (gamma-glutamyl transferase) test: This test can be helpful in detecting alcohol abuse, although it’s not specific to alcohol and can be elevated due to other reasons.
Treatment and Management
- Abstinence from alcohol: This is the most crucial step towards recovery. Stopping alcohol consumption allows the body to heal and improves red blood cell production.
- Nutritional support: A balanced diet rich in essential vitamins and minerals is vital for overall health and red blood cell production. In some cases, vitamin B12 and folate supplements might be needed.
- Treating underlying liver damage: If present, addressing liver damage is essential for overall health and proper red blood cell production.
- Medications: In severe cases of anemia, medications like erythropoietin might be used to stimulate red blood cell production.
Long-term Management
- Monitoring: Regular blood tests are necessary to track red blood cell health and ensure vitamin deficiencies are addressed.
- Lifestyle changes: Maintaining a healthy diet, exercising regularly, and getting enough sleep are crucial for overall health and preventing future complications.
- Addiction treatment: If needed, seeking professional help for alcohol dependence can significantly improve long-term health outcomes.
Myelodysplastic Syndromes (MDS)
MDS is a group of bone marrow disorders where abnormal blood cell production occurs.
Causes
The exact cause of MDS is unknown, but several factors are believed to contribute, including:
- Genetic mutations: Mutations in genes that control blood cell production can lead to MDS.
- Exposure to certain chemicals or radiation: Benzene, certain chemotherapy drugs, and high-dose radiation therapy can increase the risk of MDS.
- Age: MDS is more common in older adults.
In MDS, the abnormal bone marrow produces fewer and functionally impaired blood cells, including red blood cells. This abnormal production can sometimes lead to red blood cells being larger than normal (macrocytosis). However, it’s important to note that not everyone with MDS will have macrocytosis.
Signs and Symptoms
- Fatigue due to anemia (low red blood cells)
- Increased risk of infections due to low white blood cells
- Easy bleeding or bruising due to low platelets
- Feeling short of breath
- Pale skin
Complications
- Anemia: Macrocytosis can contribute to anemia, leading to fatigue and shortness of breath.
- Increased risk of infections: Low white blood cells due to MDS can weaken the immune system, making you more susceptible to infections.
- Bleeding problems: Low platelets can lead to easy bleeding or bruising.
- Transformation to acute myeloid leukemia (AML): In some cases, MDS can progress to AML, a more aggressive type of blood cancer.
Laboratory Investigations
- Complete blood count (CBC): This test measures red blood cell size (MCV) and other parameters to identify macrocytosis and potential anemia.
- Bone marrow aspiration and biopsy: These tests examine bone marrow directly to assess cell production and diagnose MDS.
- Cytogenetic analysis: This analysis looks for specific chromosomal abnormalities in bone marrow cells, which can help classify and risk-stratify MDS.
Treatment and Management
There’s no cure for MDS, but treatment options can help manage symptoms, improve quality of life, and potentially slow disease progression. Treatment options depend on the type and severity of MDS.
- Supportive care: This includes blood transfusions to manage anemia, antibiotics to prevent infections, and medications to stimulate red blood cell production.
- Hypomethylating agents: These drugs can help regulate abnormal gene activity in MDS cells.
- Bone marrow transplant: This is a potentially curative option for younger patients with suitable donors.
- Clinical trials: New treatment approaches and therapies are constantly being investigated in clinical trials.
Laboratory Investigations
Macrocytic anemia, characterized by abnormally large red blood cells, requires a comprehensive approach to pinpoint the underlying cause.
Clinical History
- Symptoms: Determining the presence and nature of symptoms like fatigue, weakness, shortness of breath, pale skin, or digestive issues (diarrhea, constipation) can provide clues.
- Dietary Habits: A poor diet lacking essential vitamins like vitamin B12 and folate can be a contributing factor.
- Alcohol Consumption: Chronic alcohol abuse can disrupt nutrient absorption and red blood cell production.
- Medications: Certain medications, such as anticonvulsants or metformin, can contribute to macrocytosis.
- Medical History: Previous diagnoses of liver disease, autoimmune disorders, or stomach problems can be relevant.
Physical Examination
- General appearance: Pallor (pale skin) can be a sign of anemia.
- Jaundice: Yellowing of the skin and eyes can indicate liver problems that might contribute to macrocytosis.
- Neurological examination: Vitamin B12 deficiency can cause neurological symptoms like numbness, tingling, or weakness.
Laboratory Investigations
- Complete Blood Count (CBC): This is the initial test to confirm macrocytosis (MCV > 100 fL) and identify anemia (low hemoglobin or hematocrit).
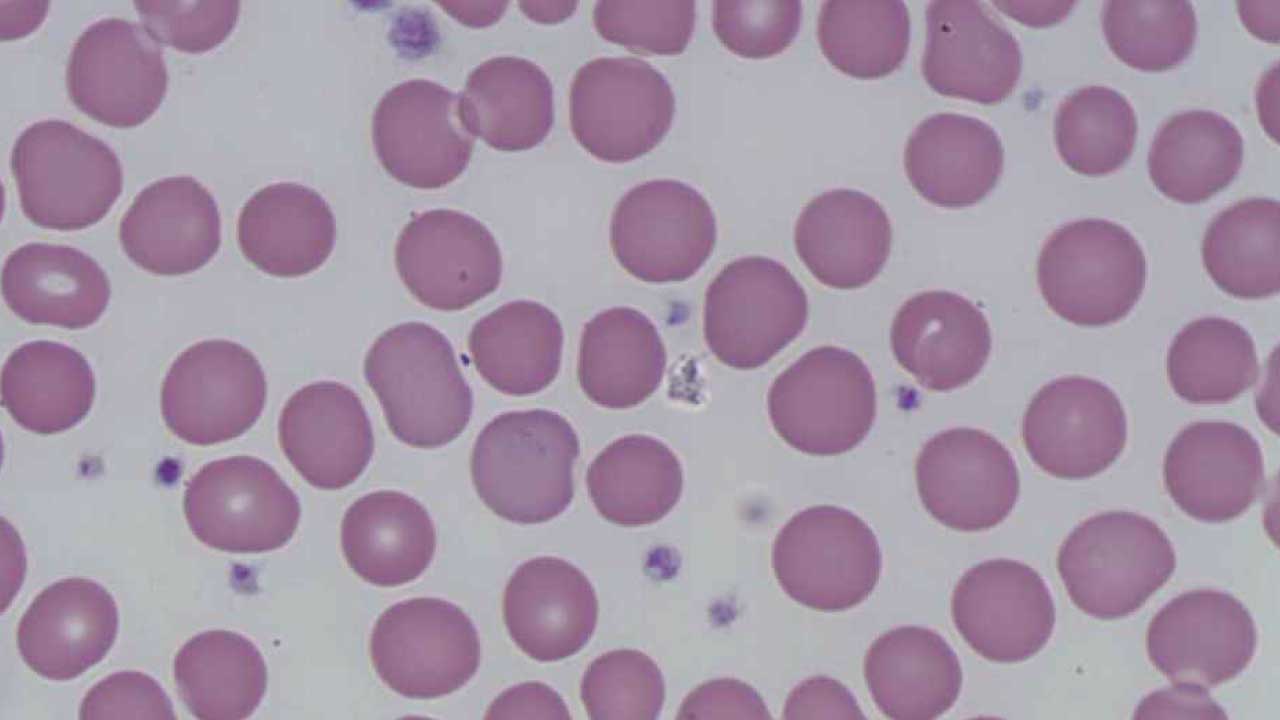
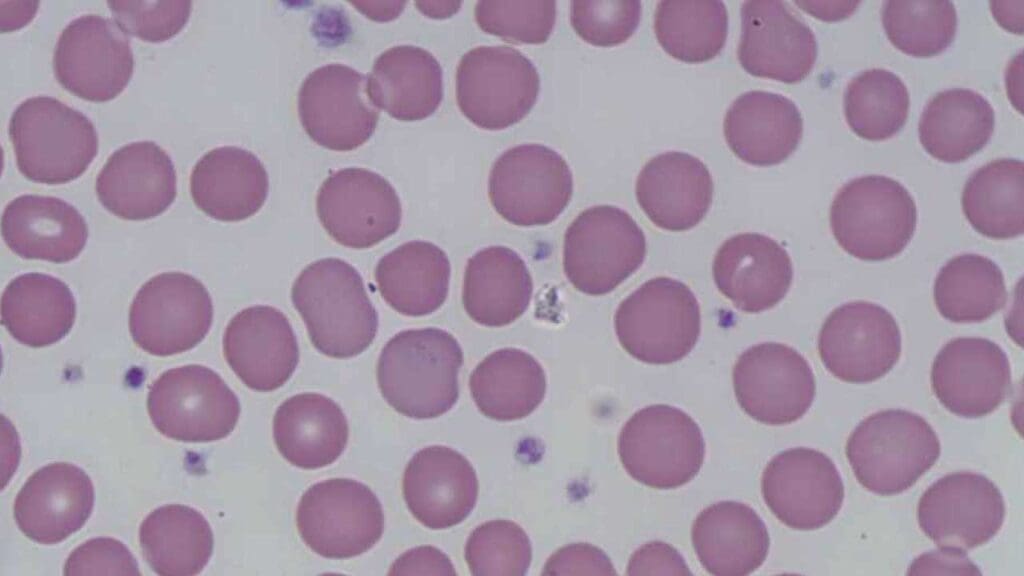
- Peripheral Blood Smear: Examining blood cells under a microscope can reveal the size and shape of red blood cells. Macro-ovalocytes (large oval red blood cells) suggest a possible megaloblastic anemia (impaired DNA synthesis in red blood cell precursors). Presence of hypersegmented neutrophils, leucopenia and thrombocytopenia is suggestive of megaloblastic anemia.
- Reticulocyte Count: This measures the number of immature red blood cells and helps assess the bone marrow’s response to anemia.
- Vitamin B12 and Folate Levels: Measuring these essential vitamins helps identify deficiencies contributing to macrocytosis.
- Liver Function Tests: These tests assess liver function and can reveal underlying liver disease that might be affecting red blood cell production.
- Other Tests (Depending on Suspicion): Additional tests like thyroid function tests, autoimmune workup, or bone marrow biopsy might be needed in specific cases.
Importance of Accurate Diagnosis
Diagnosing the underlying cause of macrocytic anemia is critical for ensuring proper treatment, preventing complications, and managing the long-term health of the individual.
- Targeted Treatment: Macrocytosis itself is a symptom, not a disease. Different underlying conditions require different treatment approaches. For example, vitamin B12 deficiency requires B12 supplementation, while treatment for autoimmune pernicious anemia (a cause of B12 deficiency) focuses on managing the autoimmune process.
- Preventing Complications: Left untreated, the underlying cause of macrocytosis can lead to serious complications. Vitamin B12 deficiency, for instance, can cause irreversible nerve damage if left untreated. Early diagnosis allows for prompt intervention and prevents these complications.
- Long-Term Prognosis: The prognosis for macrocytic anemia depends heavily on the underlying cause. Vitamin B12 deficiency anemia, with proper treatment, can be effectively managed. However, some causes like MDS (Myelodysplastic Syndromes) require ongoing management and monitoring.
- Identifying Risk Factors: Understanding the cause can help identify potential risk factors for future recurrence. For example, a dietary deficiency of B12 might prompt dietary modifications or B12 supplementation to prevent future issues.
- Cascade Effect: Macrocytosis can sometimes be a sign of a more significant underlying condition. Diagnosing the root cause allows for a more comprehensive approach to managing overall health.
Here’s a breakdown of some specific examples:
- Vitamin B12 Deficiency: Early diagnosis prevents neurological complications and ensures proper treatment with B12 supplementation.
- Autoimmune Pernicious Anemia: Identifying the autoimmune cause allows for management of the autoimmune process and ensures adequate B12 absorption.
- Alcohol Abuse: Diagnosing alcohol abuse as the culprit paves the way for addressing the addiction and preventing further damage to the body.
- Liver Disease: Early detection of liver disease allows for treatment and management, potentially improving red blood cell production.
- MDS: A prompt diagnosis of MDS allows for the implementation of appropriate treatment plans to improve blood cell counts and manage symptoms.
Frequently Asked Questions (FAQs)
What is the difference between macrocytic and megaloblastic anemia?
Macrocytic anemia and megaloblastic anemia are related but not identical conditions. Here’s the key difference:
- Macrocytic anemia: This is a general term referring to any condition where red blood cells are larger than normal (high MCV on a blood test). It can be caused by various factors, including vitamin B12 and folate deficiencies, liver disease, and bone marrow problems.
- Megaloblastic anemia: This is a specific type of macrocytic anemia caused by impaired DNA synthesis in developing red blood cells. This abnormal development leads to the characteristically large, immature red blood cells called megaloblasts. Vitamin B12 and folate deficiencies are the most common culprits behind megaloblastic anemia.
Who is at the highest risk for macrocytic anemia?
Several groups of people are at higher risk for developing macrocytic anemia though this list is not exhaustive:
- Individuals with nutritional deficiencies: This includes people with strict vegan or vegetarian diets who might lack vitamin B12, pregnant or breastfeeding women with increased B12 needs, and those with eating disorders or poor dietary habits.
- People with malabsorption conditions: Conditions like celiac disease, Crohn’s disease, or short bowel syndrome can hinder the absorption of essential vitamins like B12 and folate, leading to macrocytosis.
- Elderly population: As we age, vitamin B12 absorption can become less efficient, increasing the risk of deficiency.
- Individuals with chronic alcoholism: Alcohol abuse can interfere with vitamin B12 absorption and red blood cell production.
- People with liver disease: Liver damage can impair vitamin B12 storage and metabolism, contributing to macrocytosis.
- Those with certain medications: Some medications can interfere with vitamin B12 absorption or folate metabolism, potentially leading to macrocytosis.
- People with autoimmune conditions: Certain autoimmune diseases can attack stomach cells involved in vitamin B12 absorption, increasing the risk of deficiency.
Is macrocytic anemia serious or curable?
The seriousness and curability of macrocytic anemia depend on the underlying cause:
Seriousness
Macrocytosis itself isn’t inherently serious. However, it can be a sign of an underlying condition that could be serious if left untreated. These underlying conditions can range from vitamin deficiencies to bone marrow disorders.
Curability
The good news is that many causes of macrocytic anemia are treatable, and with proper diagnosis and treatment, the condition itself can often be cured.
- Vitamin B12 and folate deficiencies: These are common causes and can be effectively addressed with dietary changes or supplementation, leading to a cure.
- Alcohol abuse: If alcohol abuse is the culprit, stopping alcohol consumption and addressing any related nutritional deficiencies can often reverse macrocytosis.
- Certain medications: If a medication is causing macrocytosis, changing medications might be the solution.
However, some underlying causes are more complex:
- Liver disease: While macrocytosis due to liver disease might improve with treatment of the underlying liver condition, the liver damage itself might not be completely reversible.
- Bone marrow disorders: The prognosis for macrocytic anemia caused by bone marrow disorders like MDS (Myelodysplastic Syndromes) depends on the specific type and severity. While there might not be a cure, treatment options can manage symptoms and improve quality of life.
Can macrocytic anemia cause blood clots?
Macrocytic anemia itself is not directly linked to an increased risk of blood clots. Blood clots require a complex interplay between platelets, clotting factors, and the health of blood vessel walls. Macrocytic anemia primarily affects red blood cells, which are responsible for oxygen transport, not clot formation.
Can macrocytic anemia cause cancer?
Macrocytic anemia is a blood condition, not a form of cancer. However, the underlying cause behind the macrocytosis might be associated with a higher risk of certain cancers like myelodysplastic syndrome (MDS).
Which drugs cause macrocytic anemia?
Macrocytosis has been reported as a side effect of various medications, including:
- Antiviral medications: Reverse transcriptase inhibitors like zidovudine, lamivudine, and stavudine.
- Anticonvulsant medications: Valproic acid and phenytoin.
- Folate antagonists: Methotrexate.
- Chemotherapy drugs: Alkylating agents, pyrimidine and purine inhibitors.
- Other medications: Sulfasalazine (anti-inflammatory), pyrimethamine, trimethoprim, sulfamethoxazole, metformin, and nitrous oxide.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Anemia: Diagnosis and Treatment (Willis, 2016).
- Management of Anemia: A Comprehensive Guide for Clinicians (Provenzano et al., 2018)
- Goldberg S, Hoffman J. Clinical Hematology Made Ridiculously Simple, 1st Edition: An Incredibly Easy Way to Learn for Medical, Nursing, PA Students, and General Practitioners (MedMaster Medical Books). 2021.