TL;DR
Thrombophilia is an abnormal predisposition to thrombosis (blood clotting) due to abnormalities in the coagulation system.
Inherited Causes ▾: Factor V Leiden, Prothrombin gene mutation, deficiencies of Antithrombin, Protein C, or Protein S.
Acquired Causes ▾: Antiphospholipid Syndrome (APS), cancer, immobilization, surgery, pregnancy, oral contraceptives/HRT, obesity, smoking, SLE, IBD, MPNs.
Clinical Manifestations ▾: Depend on clot location; venous (DVT, PE, SVT) more common in inherited forms; arterial (stroke, MI) possible, especially in acquired conditions like APS. Recurrent miscarriages can also be a manifestation.
Investigations ▾: Clinical evaluation (history, exam) and laboratory tests (genetic testing for inherited forms, coagulation studies, antiphospholipid antibody tests).
Treatment ▾: Anticoagulation (heparin, warfarin, NOACs), management of underlying conditions (e.g., cancer), and thromboprophylaxis (anticoagulants, compression stockings).
Prognosis & Long-Term Risks ▾: Variable; depends on type of thrombophilia, other risk factors, and history of thrombotic events. Risks include recurrent thrombosis, post-thrombotic syndrome, PE, stroke, heart attack, and pregnancy complications.
*Click ▾ for more information
Introduction
Thrombophilia is a medical term that describes a condition in which the blood has an increased tendency to clot. This can lead to the formation of abnormal blood clots (thrombosis), which can block blood flow and cause serious health problems.
It is important to note that not everyone with thrombophilia will develop blood clots. In fact, most people with thrombophilia never have any symptoms at all. However, people with thrombophilia are at an increased risk of developing blood clots, so it is important to be aware of the condition and its potential complications.
Types of Thrombophilia
Inherited Thrombophilia
Inherited thrombophilia is caused by genetic mutations that are passed down from parents to their children.
The most common inherited thrombophilias are
- Factor V Leiden
- Prothrombin gene mutation
- Antithrombin deficiency
- Protein C deficiency
- Protein S deficiency
Acquired Thrombophilia
Acquired thrombophilia is not caused by genetic mutations. It can be caused by other medical conditions, such as cancer, surgery, or pregnancy.
The most common acquired thrombophilias are
- Antiphospholipid syndrome
- Cancer
- Surgery
- Pregnancy
- Oral contraceptives
Prothrombotic State
Prothrombotic state is a broader term that refers to any condition that increases the risk of blood clots. This can include thrombophilia, but it can also include other factors, such as smoking, obesity, and pregnancy.
There are many factors that can contribute to a prothrombotic state. Some of the most common risk factors are:
- Inherited thrombophilia: This is a genetic condition that makes the blood more likely to clot.
- Acquired thrombophilia: This is a condition that develops later in life that can be caused by cancer, surgery, or pregnancy.
- Age: The risk of blood clots increases with age.
- Obesity: People who are overweight or obese are more likely to develop blood clots.
- Smoking: Smoking damages the blood vessels and makes the blood more likely to clot.
- Oral contraceptives: Women who take oral contraceptives are at an increased risk of blood clots.
- Hormone replacement therapy: Women who take hormone replacement therapy are at an increased risk of blood clots.
- Immobilization: People who are immobile for long periods of time, such as after surgery or during a long flight, are at an increased risk of blood clots.
The distinction between thrombophilia and prothrombotic state is important because it can affect the way a patient is managed. For example, a patient with thrombophilia may need to take anticoagulants for the rest of their life, while a patient with a prothrombotic state due to smoking may be able to reduce their risk by quitting smoking.
Causes of Thrombophilia
Inherited Thrombophilia Disorders
- Factor V Leiden: This is the most common inherited thrombophilia, accounting for about 5% of all cases. The Factor V Leiden mutation causes a change in the Factor V protein that makes it resistant to inactivation by Protein C, a natural anticoagulant, leading to prolonged activation of the clotting cascade and an increased tendency to form clots.
- Prothrombin gene mutation: This is the second most common inherited thrombophilia, accounting for about 2% of all cases. A mutation in the prothrombin gene (G20210A) leads to increased production of prothrombin, a key clotting factor, resulting in a higher concentration of thrombin and a greater propensity for clot formation.
- Antithrombin deficiency: This is a rare but serious inherited thrombophilia. Antithrombin deficiency reduces the body’s ability to inhibit the clotting cascade, leading to uncontrolled thrombin generation and an increased risk of clot formation. Antithrombin deficiency is typically caused by a mutation in the SERPINC1 gene, which is the gene that codes for the antithrombin protein.
- Protein C deficiency: This is a rare inherited thrombophilia. Protein C deficiency impairs the body’s ability to inactivate clotting factors V and VIII, leading to an overactive clotting cascade and increased risk of thrombosis.
- Protein S deficiency: This is a rare inherited thrombophilia. Protein S deficiency reduces the effectiveness of Protein C, a natural anticoagulant, thus impairing the body’s ability to regulate the clotting cascade and increasing the risk of clot formation.
The prevalence of inherited thrombophilias varies depending on the population. In general, they are more common in people of European descent.
Acquired Thrombophilia Disorders
Acquired thrombophilias are conditions that increase the risk of blood clots. They are not caused by genetic mutations, but rather by other medical conditions or factors.
- Antiphospholipid syndrome (APS): This is an autoimmune disorder that causes the body to produce antibodies against its own phospholipids. Phospholipids are molecules that are found in the membranes of cells. APS can cause blood clots in both the arteries and veins.
- Cancer: Cancer can increase the risk of blood clots in several ways. Cancer cells can release substances that activate the blood clotting system. Cancer can also damage blood vessels, making them more likely to form clots.
- Surgery: Surgery can increase the risk of blood clots because it can damage blood vessels and slow down blood flow. The risk of blood clots is highest after major surgery, such as orthopedic surgery or abdominal surgery.
- Pregnancy: Pregnancy naturally shifts the body towards a prothrombotic state due to increased clotting factors, decreased anticoagulants, reduced clot breakdown, altered blood flow, and hormonal influences to minimize bleeding during childbirth, but this also elevates the risk of dangerous blood clots. The risk of blood clots is highest during the third trimester and the postpartum period.
- Oral contraceptives: Oral contraceptives, particularly those containing estrogen, can increase the risk of blood clots by affecting the production of clotting factors, reducing natural anticoagulants, and potentially impairing the breakdown of clots, thus shifting the balance towards a prothrombotic state. The risk of blood clots is highest in women who are taking oral contraceptives that contain both estrogen and progestin.
- Hormone replacement therapy: Hormone replacement therapy can increase the risk of blood clots because it contains hormones that can affect the blood clotting system, similar mechanisms to oral contraceptives. The risk of blood clots is highest in women who are taking hormone replacement therapy that contains both estrogen and progestin.
- Obesity: Obesity increases the risk of blood clots because it can damage blood vessels and slow down blood flow.
- Smoking: Smoking damages blood vessels and makes the blood more likely to clot.
- Immobilization: People who are immobile for long periods of time, such as after surgery or during a long flight, are at an increased risk of blood clots. Immobilization leads to venous stasis because lack of movement reduces muscle contractions that normally pump blood back to the heart, causing blood to pool and flow sluggishly in the veins, particularly in the legs.
- Systemic Lupus Erythematosus (SLE): This autoimmune disease can cause the body to produce antiphospholipid antibodies, which interfere with the normal clotting process and increase the risk of both arterial and venous thrombosis.
- Inflammatory Bowel Disease (IBD): Inflammation associated with IBD can activate the clotting system, leading to an increased risk of blood clots, particularly in the veins.
- Myeloproliferative Neoplasms (MPN): These conditions, such as polycythemia vera and essential thrombocythemia, involve an overproduction of blood cells, including platelets, which play a crucial role in clot formation. This can lead to a higher risk of thrombosis.
- Heparin-Induced Thrombocytopenia (HIT) is a different case. It’s a complication of heparin therapy, where the body produces antibodies against heparin-platelet complexes. This can paradoxically lead to both thrombocytopenia (low platelet count) and an increased risk of thrombosis.
The prevalence of acquired thrombophilias varies depending on the condition. For example, APS affects about 1% of the population, while cancer affects about 1 in 200 people.
Clinical Manifestations of Thrombophilia
Thrombophilia often presents without any noticeable symptoms until a blood clot actually forms.
The clinical manifestations largely depend on the location of the clot.
Venous Thrombosis
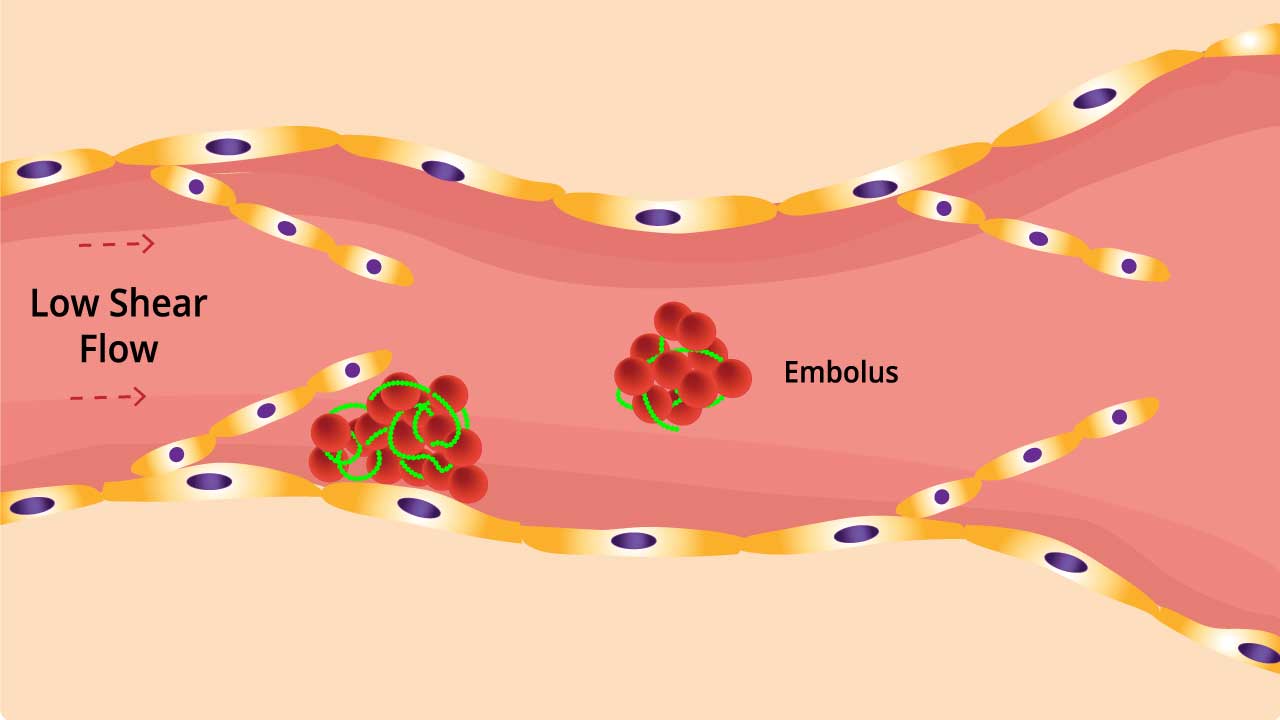
- Deep Vein Thrombosis (DVT): This occurs when a clot forms in a deep vein, usually in the leg. Symptoms include:
- Pain, swelling, and tenderness in the affected leg
- Warmth and redness of the skin
- Heaviness or cramping in the leg
- Enlarged superficial veins
- Pulmonary Embolism (PE): This is a potentially life-threatening condition that occurs when a clot breaks off from a DVT and travels to the lungs. Symptoms include:
- Sudden shortness of breath
- Chest pain, often sharp and stabbing, that worsens with deep breathing
- Cough, which may produce bloody sputum
- Rapid heart rate
- Sweating
- Lightheadedness or fainting
- Superficial Vein Thrombosis: This occurs when a clot forms in a vein close to the surface of the skin. Symptoms include:
- Pain, redness, and tenderness along the affected vein
- Warmth and swelling in the area
- The vein may feel hard and cord-like
Arterial Thrombosis
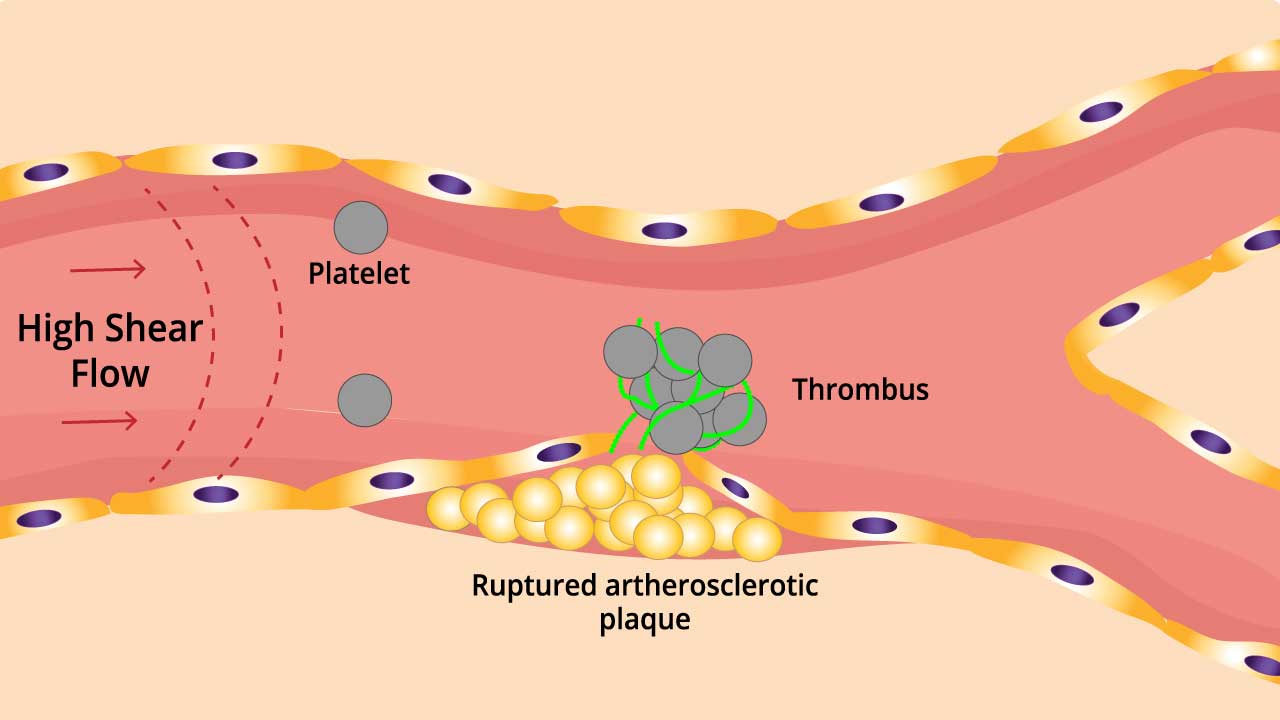
While less common in inherited thrombophilias, arterial clots can occur in some acquired conditions like antiphospholipid syndrome. Symptoms vary depending on the affected artery.
- Stroke: Sudden weakness or numbness in the face, arm, or leg, especially on one side of the body; difficulty speaking or understanding speech; vision problems; dizziness; severe headache.
- Heart Attack: Chest pain or discomfort, often described as pressure, squeezing, fullness, or pain that may spread to the arms, back, neck, jaw, or stomach; shortness of breath; sweating; nausea; lightheadedness.
- Peripheral Arterial Disease: Pain, cramping, or weakness in the legs or arms during activity; coldness or numbness in the affected limb; slow-healing sores.
Other Manifestations
- Recurrent Miscarriages: Some thrombophilias, particularly antiphospholipid syndrome, can increase the risk of recurrent miscarriages.
- Unusual Clot Locations: Clots can occur in less common sites, such as the cerebral venous sinuses (brain), mesenteric veins (intestines), or portal vein (liver). Symptoms depend on the affected area.
Laboratory Investigations for Thrombophilia
Diagnosing thrombophilia involves a combination of clinical evaluation and laboratory testing. It’s important to note that testing is not done routinely for everyone; it’s usually reserved for individuals with specific risk factors or a history of thrombotic events.
Clinical Evaluation
- Detailed Medical History: This includes personal history of thrombosis (blood clots), recurrent miscarriages, family history of thrombosis, use of medications (like oral contraceptives or hormone replacement therapy), recent surgeries, prolonged immobilization, and other relevant medical conditions.
- Physical Examination: A physical exam may reveal signs of current blood clots (like swelling, redness, warmth in a limb) but won’t directly diagnose thrombophilia itself.
Laboratory Investigations
These tests are typically done in a stepwise approach, starting with more common and readily available tests, and progressing to more specific ones if indicated.
- Initial Blood Tests (to assess general clotting function and rule out other causes):
- Complete Blood Count (CBC): A complete blood count (CBC) is generally normal in most inherited thrombophilias, but may show abnormalities in some acquired thrombophilias (like elevated platelets in myeloproliferative neoplasms) or if a clotting event has occurred (like anemia from blood loss).
- Prothrombin Time (PT) and Activated Partial Thromboplastin Time (aPTT): They are more useful for monitoring anticoagulant therapy than for diagnosing most inherited thrombophilias. They may be prolonged in some conditions like antiphospholipid syndrome.
- Specific Thrombophilia Tests (if indicated based on history/initial tests):
- Factor V Leiden Mutation Analysis
- Prothrombin G20210A Mutation Analysis
- Antithrombin Activity: Measures the level and function of antithrombin. Low levels suggest antithrombin deficiency.
- Protein C Activity and Protein S Activity: Measure the levels and function of these vitamin K-dependent proteins that act as natural anticoagulants. Deficiencies increase clotting risk.
- Lupus Anticoagulant (LA): A type of antiphospholipid antibody. It’s important to note that despite its name, it can actually prolong clotting times in some lab tests, but in the body it increases the risk of clots.
- Anticardiolipin Antibodies (aCL) and Anti-beta2 Glycoprotein I Antibodies: Other types of antiphospholipid antibodies. These, along with LA, are used to diagnose Antiphospholipid Syndrome (APS).
When to Test
Testing for thrombophilia is generally not recommended for everyone with a single, unprovoked DVT. It’s more useful in the following situations:
- Unprovoked Venous Thromboembolism (VTE): A blood clot in a vein that occurs without any obvious risk factors (like surgery, trauma, or immobilization).
- Recurrent VTE: Two or more episodes of blood clots.
- Family History of Thrombosis: A first-degree relative (parent, sibling, child) with a history of blood clots, especially at a young age.
- VTE at an Unusual Site: Blood clots in unusual locations (e.g., cerebral venous sinus thrombosis, mesenteric vein thrombosis).
- Recurrent Pregnancy Loss: Especially in the second or third trimester.
- Women considering or using oral contraceptives or hormone replacement therapy, especially if they have other risk factors for thrombosis.
Interpretation of Results
It’s crucial to interpret thrombophilia test results in the context of the individual’s clinical history and other risk factors. A positive test result doesn’t necessarily mean someone will definitely develop a blood clot, but it indicates an increased risk. A negative test doesn’t completely rule out the possibility of a thrombotic event in the future.
Treatment and Management of Thrombophilia
The treatment and management of thrombophilia aim to prevent blood clots from forming, treat existing clots, and reduce the risk of future clots. The management of thrombophilia is complex and requires a personalized approach based on the individual’s specific circumstances.
Anticoagulation
This is the cornerstone of thrombophilia management. Anticoagulants are medications that help to prevent blood clots by interfering with the clotting process. The choice of anticoagulant and the duration of treatment depend on the individual’s risk factors, the type of thrombophilia, and the presence of any active clots. Common anticoagulants include:
- Heparin: This is typically used for initial treatment of blood clots and is given by injection.
- Warfarin: This is a long-term oral anticoagulant that requires regular monitoring of blood clotting levels.
- Newer Oral Anticoagulants (NOACs): These are newer oral anticoagulants that offer similar protection to warfarin but with less monitoring required.
Management of Specific Conditions
- Antiphospholipid Syndrome (APS): In addition to anticoagulation, low-dose aspirin is often used to prevent blood clots and pregnancy complications in individuals with APS.
- Cancer-Associated Thrombosis: Treatment focuses on managing the underlying cancer, and anticoagulation is typically continued for as long as the cancer is active.
- Pregnancy-Related Thrombophilia: Pregnant women with thrombophilia require careful monitoring and may need anticoagulation throughout pregnancy and the postpartum period.
Thromboprophylaxis
This involves preventive measures to reduce the risk of blood clots in high-risk situations. Common thromboprophylaxis strategies include:
- Anticoagulants: Low-dose heparin or NOACs may be used before and after surgery or during prolonged immobilization.
- Compression Stockings: These help to improve blood flow in the legs and reduce the risk of DVT.
- Intermittent Pneumatic Compression Devices: These devices inflate and deflate cuffs around the legs to promote blood circulation.
Lifestyle Modifications
- Maintaining a healthy weight
- Regular exercise
- Avoiding smoking
- Staying hydrated
- Moving regularly during prolonged periods of sitting or standing
Monitoring and Follow-Up
Individuals with thrombophilia require regular monitoring to assess their risk of blood clots and adjust treatment as needed. This may involve periodic blood tests to check clotting levels and imaging studies to assess for any new clots.
Patient Education
It’s crucial for individuals with thrombophilia to understand their condition, the importance of adherence to treatment, and the signs and symptoms of blood clots. They should also be aware of situations that may increase their risk of clotting and take appropriate preventive measures.
Prognosis and Long-Term Considerations
The prognosis and long-term risks associated with thrombophilia vary depending on several factors, including the type of thrombophilia, the presence of other risk factors, and whether any blood clots have occurred.
In general, the prognosis for individuals with thrombophilia is good, especially if they have not experienced any thrombotic events. Many people with thrombophilia never develop any blood clots and live normal, healthy lives. However, those who have had a blood clot are at an increased risk of recurrence, and some individuals may experience long-term complications.
Potential long-term risks associated with thrombophilia
- Recurrent Thrombosis: The most significant risk is the recurrence of blood clots. The risk is highest in the first few years after an initial clot but can persist throughout life.
- Post-thrombotic Syndrome (PTS): This is a long-term complication that can develop after a DVT. It is characterized by chronic pain, swelling, and skin changes in the affected limb.
- Pulmonary Embolism (PE): A PE can cause permanent damage to the lungs and can even be fatal.
- Stroke: Some types of thrombophilia, particularly those associated with arterial thrombosis, can increase the risk of stroke.
- Heart Attack: Similarly, certain thrombophilias can increase the risk of heart attack.
- Pregnancy Complications: Women with thrombophilia are at an increased risk of pregnancy complications, such as recurrent miscarriages, preeclampsia, and stillbirth.
- Medication-Related Risks: Long-term use of anticoagulants carries a risk of bleeding complications.
It’s important to note that the overall risk of these complications varies greatly depending on the individual. Some people with thrombophilia may have a very low risk of future clots, while others may be at a higher risk.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Stevens SM, Woller SC, Bauer KA, Kasthuri R, Cushman M, Streiff M, Lim W, Douketis JD. Guidance for the evaluation and treatment of hereditary and acquired thrombophilia. J Thromb Thrombolysis. 2016 Jan;41(1):154-64. doi: 10.1007/s11239-015-1316-1. PMID: 26780744; PMCID: PMC4715840.
- Dautaj A, Krasi G, Bushati V, Precone V, Gheza M, Fioretti F, Sartori M, Costantini A, Benedetti S, Bertelli M. Hereditary thrombophilia. Acta Biomed. 2019 Sep 30;90(10-S):44-46. doi: 10.23750/abm.v90i10-S.8758. PMID: 31577252; PMCID: PMC7233636.
- Moll S. Thrombophilia: clinical-practical aspects. J Thromb Thrombolysis. 2015 Apr;39(3):367-78. doi: 10.1007/s11239-015-1197-3. PMID: 25724822.
- Colucci G, Tsakiris DA. Thrombophilia screening revisited: an issue of personalized medicine. J Thromb Thrombolysis. 2020 May;49(4):618-629. doi: 10.1007/s11239-020-02090-y. PMID: 32248336; PMCID: PMC7182628.
- Linnemann B, Hart C. Laboratory Diagnostics in Thrombophilia. Hamostaseologie. 2019 Feb;39(1):49-61. doi: 10.1055/s-0039-1677840. Epub 2019 Jan 31. PMID: 30703819.