TL;DR
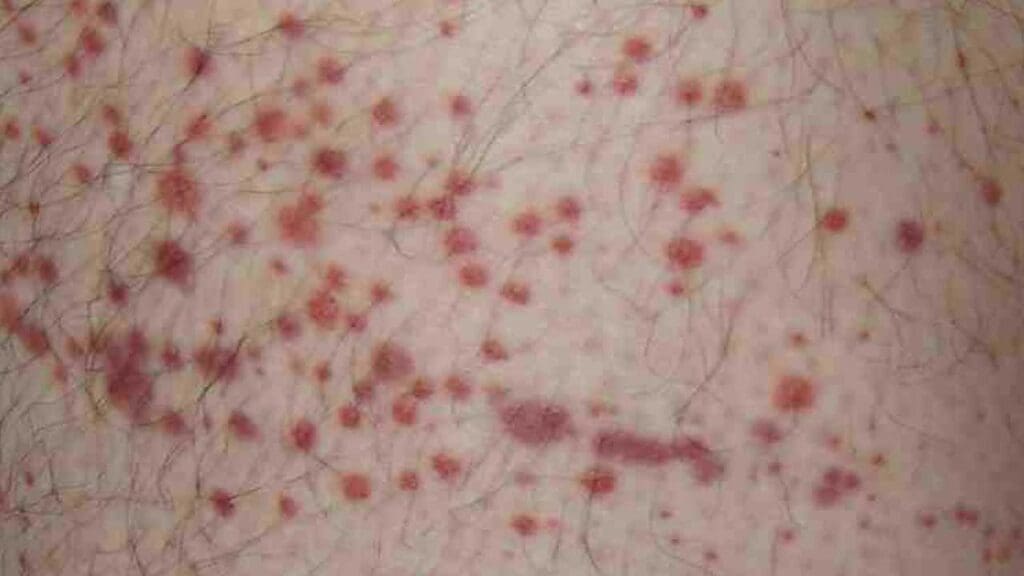
Purpura are purple/red skin spots due to bleeding under the skin. Size distinguishes them: petechiae (<4mm), purpura (4mm-1cm), ecchymoses (>1cm/bruises).
- Causes ▾: Broad, often categorized by platelet count (low or normal). Low platelets (thrombocytopenia) impair clotting, causing non-palpable purpura. Normal platelets with palpable purpura strongly suggest vasculitis (vessel inflammation).
- Symptoms ▾: Vary with the cause; may include bleeding elsewhere or systemic issues.
- Diagnosis ▾: Blood tests (especially platelet count) and sometimes more specific investigations.
- Treatment: Targets the underlying cause, ranging from supportive care to specific medications.
- Complications ▾: Depend heavily on the underlying condition.
*Click ▾ for more information
Introduction
Purpura refers to the appearance of purple or reddish spots on the skin and mucous membranes. These spots, typically ranging from pinpoint size (petechiae) to larger patches (ecchymoses or bruises), are caused by bleeding underneath the skin. It’s not a disease in itself, but rather a visible sign that can stem from a variety of underlying medical conditions affecting blood platelets, blood vessels, or the body’s clotting mechanisms.
The term “purpura” essentially means there’s bleeding under the skin causing that purple appearance, and the size of those spots or patches will further classify them as either petechiae or ecchymoses.
| Size Category | Diameter | Palpability | Common Associations and Significance |
| Petechiae | < 4 mm (pinpoint) | Non-palpable | Often associated with thrombocytopenia, impaired platelet function, or increased intravascular pressure. Widespread petechiae can be a serious sign. |
| Purpura (in a more intermediate or general usage) | 4 mm – 1 cm | Palpable or Non-palpable | Non-palpable: Can be related to platelet issues or vascular fragility. Palpable: Strongly suggests vasculitis (inflammation of blood vessels). |
| Ecchymoses | > 1 cm (bruises) | Non-palpable | Frequently due to trauma, but can also indicate coagulopathies, significant thrombocytopenia, or non-accidental injury. Easy bruising warrants investigation. |
Palpable vs. Non-palpable Purpura
Non-Palpable Purpura
These lesions are flat to the touch, level with the surrounding skin. The discoloration is solely due to the extravasation (leakage) of red blood cells into the dermis. There is no significant inflammation or swelling of the blood vessels themselves contributing to a raised texture.
Common Causes
- Platelet abnormalities
- Thrombocytopenia: A reduced number of platelets, making it harder to plug small vessel leaks. This is a common cause of petechiae and can also lead to larger areas of non-palpable purpura.
- Platelet dysfunction: Even with a normal platelet count, if the platelets don’t function correctly (e.g., due to medications or underlying conditions), they may not effectively stop bleeding.
- Increased intravascular pressure: Sudden increases in pressure within small blood vessels (e.g., from forceful coughing, vomiting, or straining) can cause them to rupture, leading to petechiae in the affected areas (face, neck, upper chest).
- Vascular fragility: Weakened blood vessel walls that are more prone to rupture with minimal trauma. This is seen in conditions like:
- Senile purpura (Bateman’s purpura): In older adults, the supporting tissues of blood vessels thin, making them fragile and easily bruised, often on the forearms and hands.
- Scurvy (Vitamin C deficiency): Vitamin C is essential for collagen production, which supports blood vessel structure. Deficiency leads to fragile capillaries and bleeding.
- Corticosteroid use: Long-term use can thin the skin and blood vessel walls.
- Simple bruising (purpura simplex): Easy bruising in some individuals without an identifiable underlying disorder.
- Coagulopathies (bleeding disorders): While often associated with larger ecchymoses, subtle bleeding tendencies can also manifest as non-palpable purpura.
Palpable Purpura
These lesions are raised and can be felt upon palpation. The elevation is due to inflammation of the blood vessel walls (vasculitis), in addition to the extravasated red blood cells. The inflammatory process causes swelling and thickening of the vessel walls.
Palpable purpura is a hallmark of vasculitis, where the blood vessels become inflamed and damaged. This inflammation leads to:
- Increased permeability of the vessel walls, allowing red blood cells to leak out.
- Swelling and thickening of the vessel walls, making the lesions palpable.
- Potential for other inflammatory signs and symptoms.
Common Causes
- Henoch-Schönlein Purpura (IgA Vasculitis): A common childhood vasculitis affecting small vessels, typically presenting with palpable purpura on the buttocks and lower extremities, often accompanied by abdominal pain, joint pain, and kidney involvement.
- Hypersensitivity Vasculitis (Allergic Vasculitis): Triggered by various antigens like medications or infections, leading to inflammation of small blood vessels in the skin and often palpable purpura.
- Cryoglobulinemic Vasculitis: Associated with abnormal proteins (cryoglobulins) that precipitate in cold temperatures, causing vessel inflammation and palpable purpura, often with systemic symptoms.
- Vasculitis associated with connective tissue diseases: Such as systemic lupus erythematosus (SLE) or rheumatoid arthritis.
- Infections: Certain infections can trigger vasculitis.
- Drug-induced vasculitis: Some medications can cause inflammation of small blood vessels.
While not the primary organizational structure for causes, palpability is a crucial descriptive characteristic that helps further refine the differential diagnosis within each platelet count category.
- Thrombocytopenic Purpura: Typically presents as non-palpable petechiae and ecchymoses. Palpable purpura is less common but can occur if there’s an accompanying vasculitis or inflammatory process.
- Non-Thrombocytopenic Purpura: Can be either palpable (strongly suggesting vasculitis) or non-palpable (often due to vascular fragility, increased pressure, or other non-inflammatory vascular issues).
Causes of Purpura
Thrombocytopenic Purpura
This category involves conditions where there is a reduced number of platelets, which are essential for blood clotting. With fewer platelets, the body’s ability to plug damaged blood vessels is impaired, leading to bleeding under the skin.
Decreased Platelet Production
- Bone Marrow Disorders: Conditions like aplastic anemia, leukemia, myelodysplastic syndromes, and metastatic cancer can damage the bone marrow, hindering its ability to produce sufficient platelets.
- Nutritional Deficiencies: Deficiencies in vitamin B12 or folate can impair bone marrow function and platelet production.
- Infections: Certain infections, such as HIV, hepatitis C, and parvovirus, can suppress bone marrow activity.
- Medications: Chemotherapy drugs, certain antibiotics, and other medications can have a toxic effect on the bone marrow, reducing platelet production.
- Alcohol Abuse: Chronic alcohol use can interfere with platelet production.
- Congenital Thrombocytopenia: Rare genetic disorders can result in lifelong low platelet counts.
Increased Platelet Destruction
- Immune Thrombocytopenia (ITP): An autoimmune disorder where the body’s immune system mistakenly attacks and destroys platelets. This can be triggered by viral infections in children (acute ITP) or can be a chronic condition in adults.
- Drug-Induced Immune Thrombocytopenia: Certain medications (e.g., heparin, quinine, sulfonamides) can trigger an immune response that leads to platelet destruction. Heparin-induced thrombocytopenia (HIT) is a well-known example.
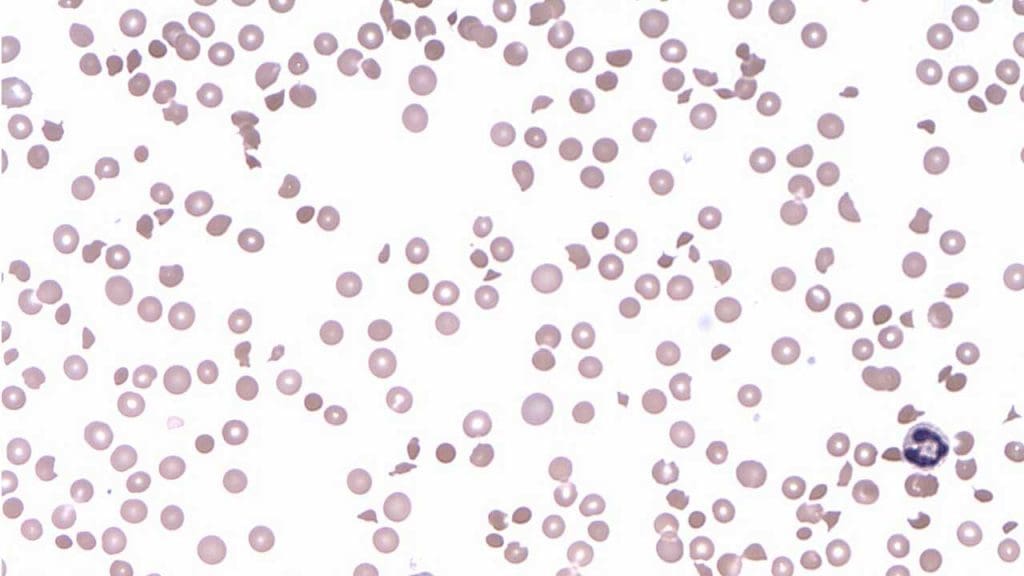
- Thrombotic Thrombocytopenic Purpura (TTP): A rare but serious blood disorder characterized by the formation of small blood clots throughout the body, leading to the consumption and depletion of platelets. It’s often due to a deficiency in the ADAMTS13 enzyme.
- Hemolytic-Uremic Syndrome (HUS): Often associated with E. coli infection, HUS involves the destruction of red blood cells and platelets, leading to purpura and kidney damage.
- Autoimmune Diseases: Conditions like systemic lupus erythematosus (SLE) and rheumatoid arthritis can be associated with increased platelet destruction.
- Neonatal Alloimmune Thrombocytopenia (NAIT): Occurs when a mother’s immune system attacks the platelets of her fetus.
Increased Platelet Sequestration
- Hypersplenism: An enlarged spleen can trap and destroy a larger than normal number of platelets, leading to thrombocytopenia and purpura. This can occur in conditions like cirrhosis, lymphoma, and some infections.
Non-Thrombocytopenic Purpura
In this category, the purpura arises despite a normal number of platelets. The underlying issues typically involve problems with the blood vessels themselves or the surrounding tissues.
Vascular Disorders
- Vasculitis: Inflammation of the blood vessels can make them fragile and prone to leaking. Causes of vasculitis include:
- Henoch-Schönlein Purpura (IgA Vasculitis): Often seen in children, characterized by inflammation of small blood vessels, leading to palpable purpura, abdominal pain, joint pain, and kidney involvement.
- Hypersensitivity Vasculitis (Allergic Vasculitis): Triggered by medications, infections, or other allergens.
- Cryoglobulinemic Vasculitis: Associated with abnormal proteins that precipitate in cold temperatures.
- Vasculitis associated with autoimmune diseases.
- Infections (e.g., meningococcemia, Rocky Mountain spotted fever).
- Increased Intravascular Pressure: Forceful coughing, vomiting, straining, or prolonged tourniquet use can increase pressure in small blood vessels, causing them to rupture and result in non-palpable purpura, often petechiae.
- Connective Tissue Disorders: Conditions affecting the structure and support of blood vessels, such as:
- Senile Purpura (Bateman’s Purpura): Fragile blood vessels in older adults lead to easy bruising.
- Scurvy (Vitamin C Deficiency): Weakened collagen in blood vessel walls makes them prone to rupture.
- Ehlers-Danlos Syndrome: A group of genetic disorders affecting connective tissue, leading to fragile skin and blood vessels.
- Hereditary Hemorrhagic Telangiectasia (Osler-Weber-Rendu Syndrome): A genetic disorder causing abnormal blood vessel formation, which can easily bleed.
- Amyloidosis: Deposition of abnormal proteins in blood vessel walls, increasing their fragility.
Other Causes
- Drug Effects: Certain medications can weaken blood vessel walls or affect their integrity without directly impacting platelet count. Corticosteroids are a notable example.
- Infections: Some infections can directly damage blood vessel walls for example meningococcemia (Neisseria meningitidis) and Rocky Mountain spotted fever (Rickettsia rickettsii).
- Childbirth: Pressure changes during vaginal delivery can cause petechiae on the face and upper chest.
- Pigmented Purpuric Dermatoses: A group of chronic skin conditions characterized by petechiae and hyperpigmentation, often due to mild capillaritis (inflammation of capillaries).
Signs and Symptoms Associated with Purpura
When purpura presents, it’s crucial to look beyond just the purple spots themselves. The associated signs and symptoms can provide vital clues about the underlying cause and the overall clinical picture.
Appearance of Purpura
- Location: Note where the purpura is located.
- Widespread: Suggests a systemic issue like thrombocytopenia, disseminated intravascular coagulation (DIC), or a systemic vasculitis.
- Localized: Might indicate trauma, increased local pressure, or a localized vascular problem like senile purpura on the forearms.
- Distribution: Certain patterns can be suggestive. For example, palpable purpura on the buttocks and lower extremities is characteristic of Henoch-Schönlein purpura. Petechiae on the face and upper chest might suggest increased pressure from vomiting or coughing.
- Size: As discussed earlier, the size (petechiae, purpura, ecchymoses) can point towards different mechanisms.
- Evolution of Lesions: Observe how the lesions change over time. Do they appear suddenly or gradually? Do they fade like typical bruises? Do new lesions continue to appear? Palpable purpura may evolve with changes in inflammation.
- Palpability: Is it flat (non-palpable) or raised (palpable)? This is a key differentiator, as discussed previously.
- Color: Fresh purpura is typically red or purple, evolving to bluish-black and then greenish-yellow as the blood breaks down, similar to a bruise. However, in conditions like vasculitis, the color might remain more consistently purplish due to ongoing inflammation.
Associated Symptoms
The symptoms accompanying purpura can be highly variable depending on the underlying etiology.
- Bleeding Manifestations
- Epistaxis (nosebleeds): Common in platelet disorders and some forms of vasculitis.
- Gingival bleeding (bleeding gums): Suggestive of platelet issues or poor oral hygiene exacerbated by a bleeding tendency.
- Menorrhagia (heavy menstrual bleeding): Can be a sign of thrombocytopenia or other bleeding disorders in women.
- Gastrointestinal bleeding: Manifesting as melena (dark, tarry stools) or hematemesis (vomiting blood), which can occur in severe thrombocytopenia, vasculitis, or coagulopathies.
- Hematuria (blood in the urine): Can be seen in Henoch-Schönlein purpura (kidney involvement), vasculitis, or severe thrombocytopenia.
- Easy bruising: A history of bruising easily or spontaneously, especially without significant trauma, is important.
- Prolonged bleeding after minor cuts or procedures: Suggests a problem with hemostasis (blood clotting).
- Systemic Symptoms
- Fever: May indicate an infection (e.g., meningococcemia, Rocky Mountain spotted fever, sepsis) or an inflammatory condition (e.g., vasculitis, autoimmune disease).
- Fatigue: Can be associated with chronic bleeding, anemia, underlying autoimmune diseases, or infections.
- Joint pain (arthralgia) or swelling (arthritis): Common in vasculitides like Henoch-Schönlein purpura and connective tissue diseases.
- Abdominal pain: Can occur in Henoch-Schönlein purpura (gastrointestinal involvement), vasculitis, or thrombotic microangiopathies (TTP, HUS).
- Neurological changes: Headaches, confusion, seizures, or focal neurological deficits might suggest thrombotic thrombocytopenic purpura (TTP), vasculitis affecting the central nervous system, or severe infections.
- Lymphadenopathy (swollen lymph nodes): Can be present in infections, autoimmune disorders, and some hematological malignancies.
- Weight loss: May suggest a chronic underlying condition like an autoimmune disease or malignancy.
- Other Specific Symptoms
- Rash (other than purpura): The presence of other types of skin lesions (e.g., vesicles, maculopapular rash, urticaria) can help narrow the diagnosis.
- Pallor (paleness): May indicate anemia due to chronic blood loss or decreased red blood cell production.
- Jaundice (yellowing of the skin and eyes): Can be seen in liver disease or hemolytic conditions.
- Splenomegaly (enlarged spleen): May suggest hypersplenism, hematological malignancies, or certain infections.
- Hemoptysis (coughing up blood): Can occur in severe vasculitis or other lung-related conditions.
Importance of History and Physical Examination
A thorough history and physical examination are crucial for interpreting the significance of purpura and guiding further investigations.
- Medication History: Certain drugs can cause thrombocytopenia, vasculitis, or platelet dysfunction.
- Recent Infections: Many conditions causing purpura can be triggered by recent viral or bacterial infections.
- Family History: A family history of bleeding disorders or autoimmune diseases may be relevant.
- Allergies: Drug allergies can sometimes manifest as purpura due to vasculitis or thrombocytopenia.
- Systemic Review: Asking about symptoms in different organ systems (e.g., musculoskeletal, gastrointestinal, renal, neurological) can provide important clues.
- Physical Examination: A complete physical exam, including careful skin inspection, palpation of lymph nodes and spleen, and assessment of vital signs, is essential.
Laboratory Assessment of Purpura
Interpreting laboratory results must always be done in the context of the patient’s clinical presentation. Isolated abnormalities may not be diagnostic, and a pattern of results is often more informative.
- Thrombocytopenia with normal coagulation studies: Suggests a platelet production, destruction, or sequestration issue.
- Normal platelet count with abnormal coagulation studies: Points towards a clotting factor deficiency or inhibitor.
- Thrombocytopenia with schistocytes on peripheral smear: Highly suggestive of a thrombotic microangiopathy (TTP or HUS).
- Palpable purpura with elevated inflammatory markers and abnormal renal function: Raises suspicion for vasculitis.
Potential Complications of Purpura
The complications of purpura also depend heavily on the underlying cause and the severity of the bleeding.
Complications related to Thrombocytopenia
- Increased risk of bleeding: The most significant complication of low platelet count is an increased risk of bleeding, which can range from minor skin and mucous membrane bleeding (e.g., nosebleeds, gum bleeding, easy bruising) to more serious internal bleeding (e.g., gastrointestinal hemorrhage, intracranial hemorrhage). The risk of serious bleeding generally increases with lower platelet counts.
- Anemia: Chronic or significant bleeding can lead to iron deficiency anemia.
- Intracranial hemorrhage: A rare but potentially fatal complication of severe thrombocytopenia or head trauma in someone with low platelets.
Complications related to Vasculitis (Palpable Purpura)
- Organ damage: Vasculitis can affect various organs, leading to complications such as kidney damage (glomerulonephritis), gastrointestinal involvement (abdominal pain, bleeding, perforation), neurological complications (neuropathy, stroke), and lung involvement.
- Skin ulceration and necrosis: Severe vasculitis can lead to tissue damage and ulceration of the skin.
- Systemic inflammation: Can cause fever, fatigue, and other constitutional symptoms.
- Scarring: Skin lesions from vasculitis can sometimes leave scars.
Complications related to other causes of purpura
- Complications of the underlying disease: For example, complications of severe infections (sepsis, organ failure), autoimmune diseases, or hematological malignancies.
- Bleeding complications: Even with a normal platelet count, significant vascular fragility or clotting disorders can lead to excessive bleeding after trauma or procedures.
- Infection: Skin breakdown or invasive procedures in individuals with purpura can increase the risk of infection.
Frequently Asked Questions (FAQs)
What vitamin deficiency causes purpura?
A deficiency in vitamin C (ascorbic acid) is a well-known cause of purpura. Vitamin C is essential for the synthesis of collagen, a crucial protein for the structure and integrity of blood vessels. When vitamin C levels are insufficient (a condition called scurvy), the blood vessels become fragile and prone to rupture, leading to bleeding under the skin, manifesting as petechiae (small purpura) and ecchymoses (larger purpura or bruises), often characteristically perifollicular (around hair follicles).
Is purpura always leukemia?
No, purpura is not always leukemia. While leukemia, a type of blood cancer, can sometimes cause purpura, it is just one of many potential underlying causes. Purpura simply indicates bleeding under the skin, and this can occur due to various reasons affecting platelets, blood vessels, or clotting factors. Other common causes of purpura include low platelet count from other conditions (like Immune Thrombocytopenic Purpura or drug reactions), infections, vasculitis (inflammation of blood vessels), and even simple trauma. Therefore, the presence of purpura necessitates further investigation to determine the specific cause, and it is crucial not to immediately associate it solely with leukemia.
Can high BP cause purpura?
Generally, high blood pressure (hypertension) itself does not directly cause purpura. Purpura results from bleeding under the skin due to issues with platelets or blood vessels. However, in rare situations, severely elevated blood pressure (malignant hypertension) can potentially damage small blood vessels, making them more fragile and prone to rupture, which could theoretically contribute to purpura. Additionally, some conditions that cause purpura, such as Henoch-Schönlein purpura or thrombotic thrombocytopenic purpura (TTP), can sometimes be associated with hypertension. Therefore, while high BP is not a common or direct cause of purpura, it can be a contributing factor in specific severe circumstances or co-exist with conditions that do cause purpura.
How long will purpura last?
The duration of purpura is highly variable and depends entirely on the underlying cause.
- Simple bruising (ecchymoses) from minor trauma typically fades within 1-2 weeks as the body reabsorbs the blood.
- Petechiae caused by increased pressure (like from coughing) usually disappear relatively quickly, often within a few days.
- Purpura due to thrombocytopenia will persist as long as the platelet count is low. The duration can range from days to months depending on the cause (e.g., acute ITP in children often resolves within a few weeks to months, while chronic ITP in adults can last much longer or be lifelong).
- Palpable purpura due to vasculitis, such as in Henoch-Schönlein purpura (HSP), typically resolves within a few weeks (1-4 weeks) in most children, but can sometimes last longer or recur. In adults, HSP can sometimes have a more prolonged course.
Can stress cause purpura?
While direct causation of purpura by psychological stress is not a well-established or common medical understanding, there is a very rare condition known as psychogenic purpura (Gardner-Diamond syndrome) or autoerythrocyte sensitization syndrome. This idiopathic (of unknown cause) psychodermatologic condition is characterized by recurrent, painful purpura that appears to be precipitated by severe emotional stress or trauma in some individuals, predominantly young women. In this syndrome, it’s hypothesized that psychological stress might trigger an unusual sensitivity or autoimmune-like reaction to the patient’s own blood components. However, this condition is extremely rare and remains a diagnosis of exclusion after ruling out all other known causes of purpura. Therefore, while typical day-to-day stress is not considered a cause of purpura, severe psychological distress is implicated in this very specific and unusual syndrome.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Goldberg S, Hoffman J. Clinical Hematology Made Ridiculously Simple, 1st Edition: An Incredibly Easy Way to Learn for Medical, Nursing, PA Students, and General Practitioners (MedMaster Medical Books). 2021.
- Scott J, Clarke C, Marchell R. Petechiae, Purpura, and Hemorrhagic Vesicles. JAMA Dermatol. 2017 Jul 1;153(7):707-708. doi: 10.1001/jamadermatol.2016.5965. PMID: 28146222.
- Sweet JM, Mulkey BH. Lower Extremity Petechiae and Purpura. Am Fam Physician. 2020 May 1;101(9):567-568. PMID: 32352732.




