Disclaimer: This article provides a general overview of the phlebotomy procedure. It is not intended as a substitute for proper phlebotomy training. All staff performing phlebotomy must undergo comprehensive training and certification to ensure patient safety and optimal blood sample collection.
Introduction
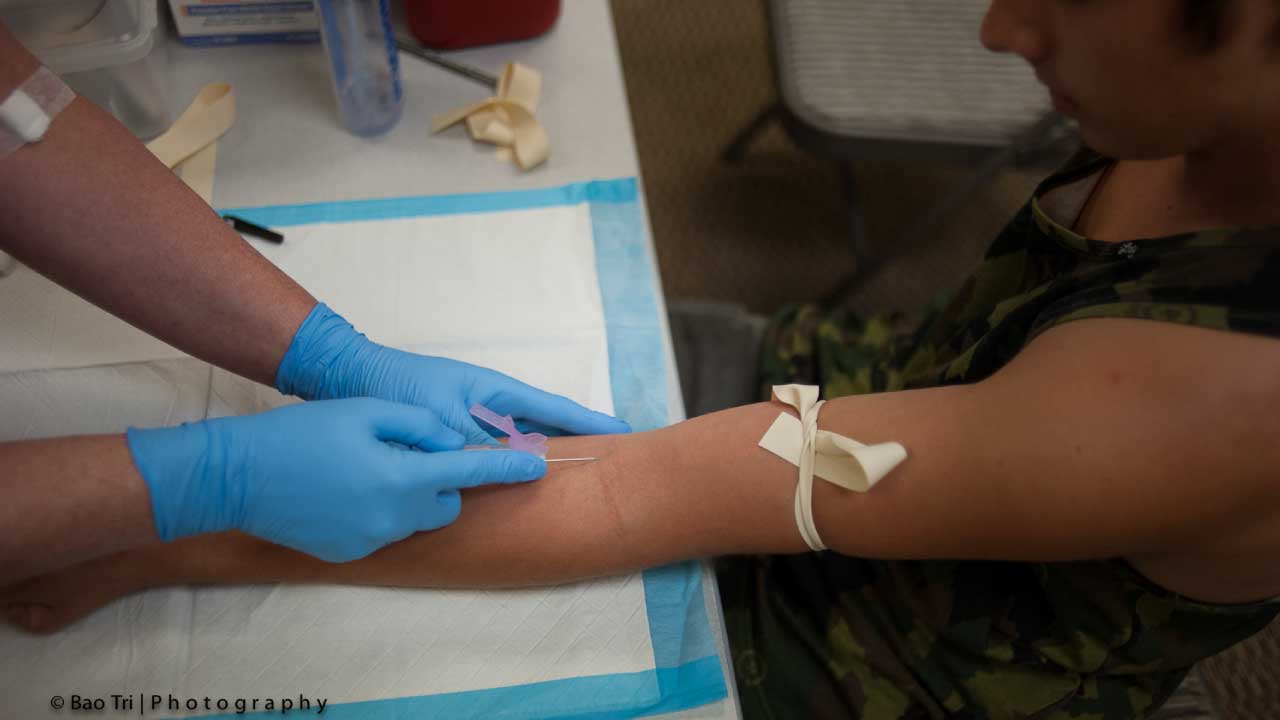
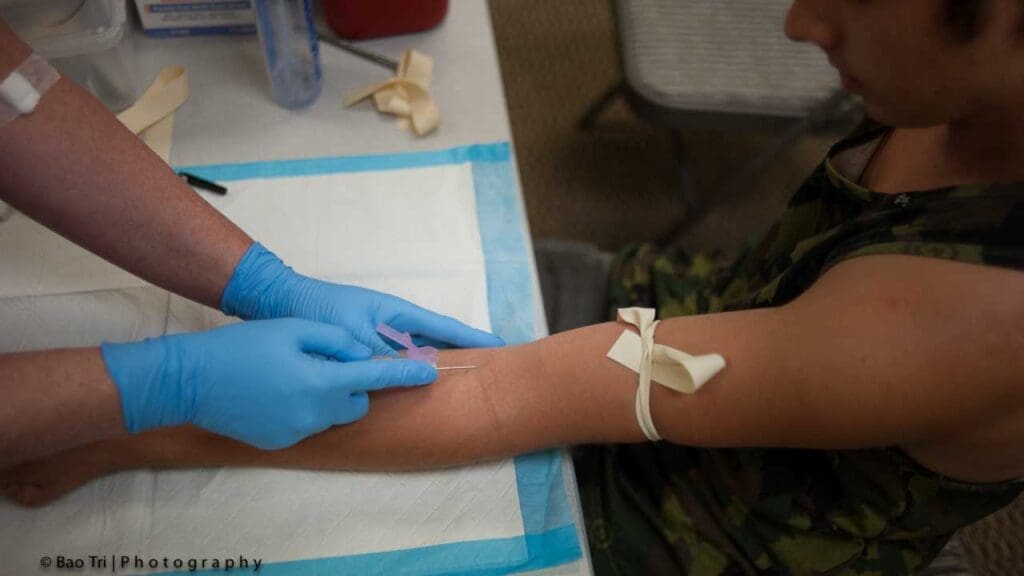
Phlebotomy is the process of drawing blood from a vein, typically in the arm, for various healthcare purposes. It encompasses the entire procedure, from preparing the patient and equipment to collecting, labeling, and processing the blood sample.
Role in Healthcare: Phlebotomy plays a crucial role in diagnosing and monitoring a wide range of medical conditions. Blood tests provide valuable information about:
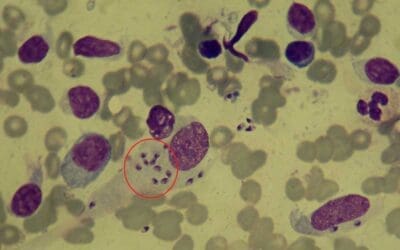
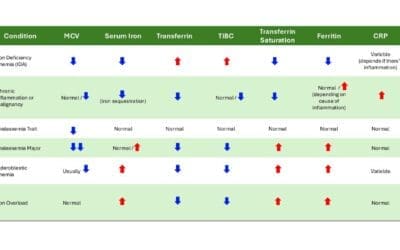
- Complete Blood Count (CBC): Evaluates red and white blood cells, hemoglobin, and platelets to assess overall health and identify potential infections or blood disorders.
- Chemistry Panels: Measure electrolytes, blood sugar, liver and kidney function, and other vital biochemical markers.
- Hormone Testing: Assesses hormone levels for thyroid function, fertility, and other conditions.
- Blood Typing and Crossmatching: Ensures blood compatibility for transfusions.
- Blood Cultures: Identify the presence of bacteria in the bloodstream to diagnose infections.
Importance of Proper Phlebotomy Technique
- Patient Safety: Minimizes discomfort, bruising, and risk of infection from improper needle handling or venipuncture in phlebotomy.
- Sample Integrity: Ensures accurate blood test results by avoiding contamination, hemolysis (red blood cell rupture), or clotting. Accurate results lead to proper diagnosis and treatment.
- Efficiency: Skilled phlebotomists can collect blood samples quickly and effectively, minimizing patient wait times and staff time spent on repeat procedures due to missed veins.
- Positive Patient Experience: A skilled and compassionate phlebotomist can make the phlebotomy process less stressful for patients, promoting better overall healthcare experiences.
The entire phlebotomy procedure can be roughly divided into pre-phlebotomy procedure where preparations for the procedure is carried out and then the phlebotomy procedure itself which involves proper hand hygiene, patient positioning, vein selection, and venipuncture. Once enough blood is drawn, in post-phlebotomy procedure the sample is handled according to protocol and documenting everything in the patient’s medical record.
Pre-Phlebotomy Procedure
- Equipment
- Sterile Phlebotomy Tray: Containing needles of appropriate gauge and length, syringes if needed, various blood collection tubes specific to the tests ordered, and a tourniquet.
- Antiseptic wipes: For disinfecting the venipuncture site.
- Sterile gauze pads: For applying pressure after blood collection.
- Sharps container: For safe disposal of used needles and syringes.
- Specimen labels: To ensure proper identification of collected blood samples.
- Request form: The form requesting the type of tests ordered for the patient.
- Self-sealing plastic bags with a separate compartment for the request form: To prevent contamination of the forms in the event of leakage.
- Adhesive dressings: To cover the venipuncture site after blood withdrawal.
- Patient Identification: Verifying patient identity in phlebotomy is paramount to prevent errors. This requires using two patient identifiers, such as:
- Name (full legal name)
- Date of birth
- Medical record number (if applicable)
- Reviewing Lab Orders: Carefully review laboratory orders is essential in phlebotomy.
- The type of blood tests requested (e.g., complete blood count, blood chemistry panel).
- The number of blood tubes needed for each test.
- Any specific requirements for handling or processing the samples (e.g., maintaining samples on ice for specific tests).
- Patient Communication: Effective communication builds trust and reduces patient anxiety.
- Explain the phlebotomy procedure in a clear and concise manner.
- Address any questions or concerns the patient may have.
- Obtain informed consent, ensuring the patient understands the risks and benefits of the procedure.
- Acknowledge and address any anxieties the patient might have, such as fear of needles, by providing reassurance and a calming presence.
The Phlebotomy Procedure including Venipuncture
Following the thorough pre-procedure steps, the phlebotomy process itself involves several crucial steps to ensure patient safety, optimal blood collection, and proper sample handling.
5. Hand Hygiene and Gloves: Proper handwashing technique to prevent infection
- This is the cornerstone of infection control in phlebotomy. The phlebotomist must perform a thorough handwashing following World Health Organization (WHO) guidelines using an alcohol-based hand rub or soap and water. This eliminates transient and resident hand flora, significantly reducing the risk of transmitting pathogens to the patient and vice versa.
- Following thorough handwashing, put on well-fitting, non-sterile gloves.
6. Patient Positioning: Ensuring patient comfort and optimal vein visualization
- The patient’s comfort and safety are paramount. They are typically positioned in a comfortable chair with their arm supported on a stable surface. For optimal vein visualization, position the patient’s arm in a comfortable, extended position, with the hand in line with the wrist and elbow.
- The phlebotomist may ask the patient to clench and unclench their fist to improve vein filling.
7. Site Selection: Identifying suitable veins for venipuncture
- The most common site for venipuncture is the antecubital fossa, the area on the inner elbow where several veins are readily accessible.
- The preferred vein is the median cubital vein, known for being large, stable, and easily palpated. Alternative veins like the cephalic vein or basilic vein might be used for venipuncture if the median cubital vein is inaccessible. If these veins are not readily visible, clenching the patient’s fist can help make them more prominent.
- While visually identifying veins is ideal, feeling them (palpation) is also a valuable technique in venipuncture. Use your index finger to gently trace the path of the veins. Remember, arteries are bouncy and pulsate due to their thicker walls and elasticity. In contrast, thrombosed (clogged) veins feel firm and cord-like, rolling easily under your touch. If veins aren’t immediately visible, there are ways to make them more prominent. You can try massaging the arm from wrist to elbow to encourage blood flow, tapping the area lightly with two fingers, applying a warm washcloth for 5 minutes, or even lowering the patient’s arm to allow the veins to fill.
- For optimal comfort and safety, the basilic vein is generally avoided for venipuncture. It lies close to an artery and nerve, increasing the risk of accidental puncture. Additionally, avoid areas where veins branch out (divert) as this can make it trickier to draw blood and raise the chance of forming a blood clot (hematoma).
- Important Considerations for Venipuncture Location
- Arteries: Under no circumstances should a phlebotomist attempt venipuncture on an artery.
- Feet: Blood collection from the feet is generally discouraged. If necessary, a healthcare provider’s explicit permission is required.
- Scarred or Burned or Inflamed Areas: Avoid areas with significant scarring or healed burns to prevent complications.
- Mastectomy: Do not draw blood from the arm on the same side as a mastectomy (breast removal surgery). Test results may be affected because of lymphedema.
- Hematomas (Blood Clots): Areas with visible blood clots (hematomas) should be avoided for venipuncture. It may cause erroneous test results. In the absence of a better option, collect the blood sample from an area below the blood clot (distal to the hematoma).
- Intravenous (IV) Lines: If an IV line is present, blood samples can be drawn from the arm below the IV insertion site, but never above it.
- Vascular Access Devices: Avoid drawing blood from an arm with a cannula (tube inserted into a vein for medication), fistula (surgical connection between an artery and vein), or vascular graft (transplanted blood vessel).
- Blood Transfusions: Wait 10-15 minutes after completing a blood transfusion before attempting blood collection from the same arm. Whenever feasible, draw blood from the arm opposite an IV to avoid potential dilution of the sample by fluids.
8. Venipuncture:
- Applying a tourniquet: The patient should make a fist without pumping the hand. Secure the tourniquet 4–5 finger widths above the chosen vein, then re-assess the vein. It helps to distend the vein, making it easier to locate and puncture. Apply the tourniquet comfortably snug, but not too tight. Limit its use to under two minutes to avoid hemoconcentration (increased blood cell concentration due to fluid loss). If necessary, wait two minutes before reapplying the tourniquet for another attempt.
- Disinfecting the venipuncture site: For routine blood draws (excluding blood cultures), cleanse the venipuncture site with a 70% alcohol swab in a circular motion for 30 seconds. Allow the alcohol to air dry completely for another 30 seconds before proceeding. This ensures proper disinfection and prevents discomfort during the needle insertion. Avoid touching the intended venipuncture site after cleaning.
- Performing venipuncture with proper needle insertion technique:
- Anchoring the Vein: Support the vein by firmly grasping the patient’s arm above the venipuncture site with your thumb. This helps stabilize the vein and prevent movement during needle insertion.
- Needle Angle and Entry: With the needle bevel facing upwards, hold it at a low angle (15-30 degrees) to the arm’s surface. Swiftly insert the needle through the skin and into the vein in a single smooth motion. Avoid excessive probing or forceful entry.
- Blood Flow Confirmation: A successful venipuncture will result in a visible flashback of blood into the tube attached to the needle. This confirms proper needle placement within the vein.
- Blood Collection: Maintain a secure hold on the needle hub and attach the first blood collection tube according to the required order of draw. Blood should flow freely into the evacuated tube.
- Blood collection and filling tubes in the correct order: Once proper blood flow is established, the blood collection tubes are filled in the correct order as per the laboratory requisition. Each tube contains specific anticoagulants or additives to preserve the blood components for different tests. In phlebotomy, maintaining a specific order of draw for blood collection tubes is essential to avoid cross-contamination of additives and ensure accurate test results.
- i. Blood Culture Bottle: This is drawn first to minimize contamination by skin flora or other additives.
- ii. Non-additive Tube (Serum or Plasma): This tube contains no additives and is used for tests requiring pure serum or plasma. It’s drawn before tubes with clotting activators to avoid premature clotting.
- iii. Sodium Citrate Tube (Light Blue Top): This tube contains sodium citrate as the anticoagulant. It’s used mainly for coagulation studies tests. Drawing it before clotting activator tubes minimizes the risk of residual activator affecting results.
- iv. Clot Activator Tube (Red Top): This tube contains a clot activator that accelerates clotting. It’s used for obtaining serum, the liquid portion of blood after clot formation.
- v. Serum Separator Tube (SST) (Red Speckled or Gold Top): These tubes contain a clot activator and a gel separator. The gel separates the serum from the red blood cells after clotting.
- vi. Sodium Heparin Tube (Light Green Top): This tube contains sodium heparin, an anticoagulant used for specific tests like blood gas analysis. Draw it after clotting tubes as heparin can interfere with some tests.
- vii PST (Plasma Separation Tube) (Light Green Top): These tubes contain a gel separator and may or may not contain an anticoagulant (lithium heparin). Used for specialized testing like blood banking or compatibility testing. Positioning depends on specific test requirements, but often drawn after heparin to avoid contamination.
- viii. EDTA Tube (Lavender Top): This tube contains EDTA, an anticoagulant used for tests requiring whole blood, such as complete blood count (CBC) or blood smears. Drawn after heparin to minimize platelet clumping, which can affect CBC results.
- ix. ACD (Acid Citrate Dextrose) Tube (Pale Yellow Top): Contains anticoagulant citrate and dextrose for blood gas analysis. Draw it last due to its specific anticoagulant mix.
- x. Oxalate Tube (Gray Top): These tubes contain an anticoagulant (potassium oxalate or sodium oxalate) and are used for specific tests like glucose or lactate levels. Draw them last to minimize contamination.

9. Completion of Procedure:
- Releasing the tourniquet: After collecting enough blood, release the tourniquet first before removing the needle. However, some guidelines suggest doing this as soon as blood flows, but never leave it on for more than two minutes.
- Applying pressure to the puncture site: Gauze pad is applied with gentle pressure to the venipuncture site to stop any bleeding.
- Proper disposal of sharps: The used needle and any other sharps are disposed of safely in a designated sharps container to prevent accidental needle sticks and injuries.
10. Sample Handling: Labeling samples according to institutional protocols
- After collection, each blood tube is labeled with essential information such as the patient’s name, date of birth, time of collection, and any specific test requirements.
- This ensures proper identification and tracking of the samples throughout the testing process.
Post-Procedure
Following a successful blood draw, the phlebotomist performs a few crucial steps to ensure patient well-being and proper documentation.
11. Patient Care: Monitoring for bleeding or discomfort, providing post-procedure instructions
- Monitoring: The phlebotomist observes the venipuncture site for a few minutes to ensure bleeding has stopped. They may apply gentle pressure with a gauze pad for a short time.
- Discomfort: The patient might experience some slight discomfort or dizziness after the blood draw. The phlebotomist should inquire about their well-being and offer reassurance.
- Post-procedure instructions: The phlebotomist provides clear instructions to the patient, such as:
- Keeping the bandage on the venipuncture site for a recommended timeframe (usually a few minutes)
- How to monitor for any bleeding or swelling
- When to resume normal activities
- Contact information in case of any concerns
12. Documentation: Recording all relevant details of the procedure in the patient’s medical record
- Accurate documentation is essential for patient care and ensuring continuity of information. The phlebotomist will record details in the patient’s medical record, including:
- Date and time of blood draw
- Site of venipuncture
- Gauge and type of needle used
- Number and type of blood tubes collected
- Any complications encountered during the procedure (e.g., difficulty obtaining blood)
- Patient’s tolerance of the procedure
Additional Considerations
A. Troubleshooting: Addressing challenges during venipuncture
- Difficult Veins: If locating a suitable vein is challenging, the phlebotomist can utilize various techniques:
- Warm compress: Applying a warm compress to the area can help dilate veins, making them more visible.
- Arm positioning: Adjusting the patient’s arm position (e.g., having them clench and unclench their fist) can also improve vein visibility.
- Alternative sites: If the preferred veins are inaccessible, alternative sites like the hand or foot might be considered, but with proper authorization.
- Multiple Attempts: If a successful venipuncture isn’t achieved on the first try, phlebotomist protocols typically dictate a maximum number of attempts (often 2-3) before consulting a more experienced colleague or requesting a referral for a different blood draw method (e.g., venipuncture by a physician).
B. Special Situations
Pediatric Patients
- Minimize anxiety: Use a calm and friendly approach, explain the procedure in age-appropriate language, and allow parents or guardians to be present for comfort.
- Reduce pain: Consider topical anesthetics (with physician approval) for older children or use smaller needles appropriate for their size.
- Distraction techniques: Use toys, bubbles, or songs to distract younger children and divert attention from the procedure.
- Positioning: Support the child’s arm comfortably and choose a larger, more visible vein if possible.
Elderly Patients
- Fragile veins: Select larger veins in the arm or hand for easier access and minimize the number of attempts.
- Limited mobility: Assist the patient in assuming a comfortable position and provide support during the procedure.
- Medication review: Be aware of medications that might affect bleeding or clotting time.
- Hydration: Encourage adequate hydration before the blood draw to improve vein visibility.
Patients with Disabilities
- Communication: Tailor your communication style to the patient’s needs. Use visual aids or written instructions if necessary.
- Accessibility: Ensure the phlebotomy chair or bed is adjustable and accommodates the patient’s physical limitations.
- Assistance: Offer assistance if needed for positioning or maintaining pressure on the venipuncture site after the draw.
- Respect and empathy: Maintain a respectful and patient demeanor throughout the procedure.
Patients with Blood Disorders
- Physician consultation: Consult the doctor for specific instructions regarding blood draw procedures for patients with bleeding disorders like hemophilia.
- Pressure application: Apply gentle but firm pressure for a longer duration (as directed by the physician) to ensure proper clotting after the needle is removed.
- Venipuncture site selection: Avoid areas with easy bruising or previous bleeding episodes.
- Documentation: Clearly document the patient’s blood disorder and any specific precautions taken during the procedure.
Immunocompromised Patients
- Aseptic technique: Meticulously adhere to aseptic technique using sterile supplies to minimize the risk of infection.
- Skin disinfection: Pay close attention to thorough skin disinfection at the venipuncture site.
- Sharps disposal: Ensure safe and proper disposal of sharps to prevent accidental needle sticks.
- Communication with healthcare team: Communicate any concerns or complications encountered during the blood draw to the healthcare team.
C. Safety Measures: Importance of universal precautions to prevent bloodborne pathogen transmission
Phlebotomists adhere to universal precautions, which assume all blood and body fluids are potentially infectious. This includes:
- Wearing personal protective equipment (PPE) like gloves, gowns, and eye protection during the procedure.
- Using sterile needles and single-use supplies.
- Proper disposal of sharps and biohazardous waste.
- Hand hygiene before, during, and after the procedure.
Following these precautions minimizes the risk of phlebotomists contracting bloodborne diseases and protects patients from potential contamination.
D. Quality Assurance: Maintaining proper standards for blood sample collection
Maintaining high-quality blood collection practices is essential for accurate test results. These practices include:
- Using properly labeled and dated tubes to ensure accurate sample identification.
- Following the recommended order of draw to prevent contamination between tubes.
- Maintaining proper storage and transport temperatures for blood samples.
- Regularly calibrating phlebotomy equipment to ensure accuracy.
Conclusion
Proper phlebotomy technique is more than just drawing blood. It’s a crucial skill that lays the foundation for accurate diagnoses and effective patient care.
- Accurate Sample Collection: The success of many medical tests hinges on the quality of the blood sample. Proper technique ensures minimal contamination, clotting, or hemolysis (red blood cell breakdown) in the sample, leading to reliable results for diagnosis and treatment decisions.
- Patient Comfort and Safety: Skilled phlebotomists minimize discomfort during the venipuncture procedure, reducing anxiety and potential complications like fainting or bruising. Universal precautions ensure safety for both patients and healthcare workers by preventing bloodborne pathogen transmission.
- Reduced Need for Re-draws: A successful first attempt at venipuncture translates to less stress for patients and a smoother workflow within the healthcare system. Proper venipuncture technique minimizes the need for repeat blood draws due to insufficient sample volume or compromised quality.
Comprehensive Training
Mastering proper phlebotomy technique requires comprehensive training especially in venipucture. This training equips phlebotomists with the necessary knowledge and skills to:
- Understand anatomy and physiology: Knowing the location and function of veins and arteries is crucial for safe and efficient blood collection.
- Perform sterile procedures: Following aseptic technique minimizes the risk of infection for both patients and healthcare workers.
- Communicate effectively: Clear communication with patients about the procedure and post-care instructions helps ease anxiety and ensures patient understanding.
- Troubleshoot challenges: Training equips phlebotomists with skills to handle situations like difficulty locating a vein or working with patients who have special needs.
Frequently Asked Questions (FAQs)
What are the two types/categories of phlebotomy?
Diagnostic Phlebotomy: This is the most common type. It involves drawing blood for various diagnostic tests to identify medical conditions, monitor existing ones, or assess overall health.
Therapeutic Phlebotomy: This type of phlebotomy uses blood removal as a treatment itself. It’s used for specific conditions like hemochromatosis (iron overload), polycythemia vera (excess red blood cells), or sickle cell disease. By removing some blood, these procedures aim to improve symptoms and prevent complications.
What are the 3 main phlebotomy procedures used today?
While phlebotomy can be broken down into various steps, the 3 main procedures used today based on the type of blood draw are:
- Venipuncture: This is the most common procedure, involving drawing blood from a vein in the arm using a needle and evacuated tube system. It’s used for a wide range of diagnostic tests, blood transfusions, and some therapeutic procedures.
- Capillary Puncture: This procedure uses a small lancet to prick a fingertip, heel, or earlobe to collect a small blood sample. It’s typically used for tests requiring a smaller volume like blood sugar monitoring, newborn screening, or allergy testing.
- Arterial Puncture: This is a less common procedure used in critical care settings to draw blood directly from an artery. Due to the risks involved, it’s only performed by specially trained personnel and for specific purposes like blood gas analysis or monitoring during surgery.
What are the 3 types of phlebotomy needle?
There isn’t a universal classification for phlebotomy needles based on type, but here are 3 ways to categorize them based on their key characteristics.
- By Design
- Conventional Hypodermic Needle: This is a basic needle with a bevel (angled tip) and a hub for connection to a syringe or tubing. It’s less commonly used in modern phlebotomy due to the need for separate needle insertion and blood collection steps.
- Butterfly Needle (Winged Infusion Set): This needle has a short, thin needle with flexible wings on either side. It’s ideal for patients with fragile veins or those who might have difficulty holding still, as the wings provide stability during insertion.
- By Gauge: Gauge refers to the inner diameter of the needle, with a higher number indicating a smaller diameter. Common phlebotomy needle gauges include:
- Large Gauge (18-21 gauge): Used for collecting larger blood volumes or for patients with easily accessible veins.
- Medium Gauge (22-23 gauge): Most commonly used for routine blood draws, offering a balance between blood flow and patient comfort.
- Small Gauge (25-27 gauge): Used for pediatric patients, elderly patients with fragile veins, or situations requiring minimal blood volume.
- By Collection System
- Single Sample Needle: This is a basic needle used with a syringe for a single blood draw.
- Vacutainer Needle: This needle is designed for use with a vacuum tube system, allowing for multiple blood samples to be collected in separate tubes without needing to change the needle.
What is the difference between phlebotomy and venipuncture?
Phlebotomy and venipuncture are often used interchangeably, but there’s a subtle difference between them.
- Phlebotomy: This is the broader term encompassing the entire process of drawing blood for various purposes. It includes techniques like venipuncture, capillary puncture (fingerstick), and even heel pricks in newborns. Phlebotomy also involves tasks beyond blood collection itself, such as preparing the necessary equipment, labeling samples, and ensuring proper disposal of sharps.
- Venipuncture: This is a specific technique within phlebotomy that focuses solely on drawing blood from a vein, typically in the arm. It involves inserting a needle into a vein to collect a blood sample for diagnostic tests, blood transfusions, or some therapeutic procedures.
What is the most common complications of phlebotomy?
The most common complications of phlebotomy are generally minor and temporary. Here are the top 3:
- Hematoma: This is a collection of blood that escapes from the vein and forms a bruise at the venipuncture site. It typically occurs due to difficulty locating a vein or applying insufficient pressure after needle removal.
- Pain and Discomfort: While phlebotomy is a minimally invasive procedure, some patients might experience discomfort during needle insertion or throbbing after the blood draw. Following proper technique and using appropriate needle size helps minimize this.
- Vasovagal Reaction: This is a reflex response to the stress of the procedure, causing lightheadedness, dizziness, or even fainting. It’s more common in patients with anxiety or fear of needles. Creating a calm environment and having patients lie down during the draw can help reduce the risk.
It’s important to note that more serious complications like nerve damage or infection are rare when proper aseptic technique is followed by trained phlebotomists.
References
- WHO Guidelines on Drawing Blood: Best Practices in Phlebotomy. Geneva: World Health Organization; 2010. 2, Best practices in phlebotomy. Available from: https://www.ncbi.nlm.nih.gov/books/NBK138665/
- https://pathlabs.ufl.edu/client-services/specimen-shipping/blood-collection-process-venipuncture/
- https://webpath.med.utah.edu/TUTORIAL/PHLEB/PHLEB.html
- https://www.phlebotomyusa.com/blog/phlebotomy/a-step-by-step-guide-to-phlebotomy-procedure/