TL;DR
The purpose of iron studies interpretation is to comprehensively assess the body’s iron status, diagnose iron deficiency or overload conditions, and differentiate them from other anemias or health issues that affect iron metabolism. Causes of highs and lows of the different iron parameters include:
- Serum Iron ▾
- Low Serum Iron Level
- Iron Deficiency Anemia (body is using iron faster than it can be absorbed or supplied)
- Anemia of Chronic Disease/Inflammation (iron is trapped in storage, not available in circulation)
- Malabsorption (e.g., celiac disease, gastric bypass surgery)
- Chronic blood loss (e.g., heavy menstruation, GI bleeding)
- Poor dietary intake
- High Serum Iron Level
- Hemochromatosis (genetic iron overload disorder)
- Repeated blood transfusions (introducing external iron)
- Excessive iron supplementation (oral or intravenous)
- Hemolytic anemias (red blood cells are breaking down, releasing iron)
- Liver disease (impaired iron storage and regulation)
- Acute iron poisoning
- Sideroblastic Anemia (iron is available but not incorporated into heme)
- Low Serum Iron Level
- Ferritin ▾
- Low Ferritin Level
- Iron Deficiency (depleted iron stores – most specific indicator)
- Chronic blood loss
- Poor dietary intake
- Malabsorption
- Pregnancy (increased iron demand)
- High Ferritin Level
- Iron Overload (e.g., Hemochromatosis, transfusional hemosiderosis)
- Inflammation or Infection (ferritin is an acute phase reactant, levels rise)
- Liver Disease (e.g., hepatitis, cirrhosis)
- Malignancies (e.g., lymphomas, leukemias)
- Certain autoimmune diseases (e.g., Adult Still’s disease, rheumatoid arthritis)
- Chronic alcohol abuse
- Metabolic Syndrome
- Low Ferritin Level
- Transferrin ▾
- Low Transferrin Level
- Inflammation/Infection (transferrin is a negative acute phase reactant, decreases in inflammation)
- Liver disease (impaired synthesis)
- Malnutrition/Protein deficiency
- Iron overload (body doesn’t need to produce as much iron-transporting protein)
- Nephrotic syndrome (protein loss in urine)
- High Transferrin Level
- Iron Deficiency Anemia (body tries to increase its capacity to bind available iron)
- Pregnancy (especially later stages)
- Oral contraceptive use (due to estrogen effects)
- Low Transferrin Level
- TIBC (Total Iron-Binding Capacity) ▾
- Low TIBC Level
- Anemia of Chronic Disease/Inflammation (less transferrin produced)
- Iron Overload (less need for iron binding capacity)
- Liver Disease (impaired protein synthesis)
- Malnutrition
- Nephrotic Syndrome
- High TIBC Level
- Iron Deficiency Anemia (more “empty seats” on transferrin to try and capture iron)
- Pregnancy (physiological increase)
- Oral contraceptive use
- Low TIBC Level
- Transferrin Saturation (%) ▾
- Low Transferrin Saturation
- Iron Deficiency Anemia (low serum iron, high TIBC means few binding sites are occupied)
- Anemia of Chronic Disease/Inflammation (low serum iron despite normal/high ferritin)
- IRIDA (Iron Refractory Iron Deficiency Anemia)
- High Transferrin Saturation
- Iron Overload (e.g., Hemochromatosis, transfusional iron overload – many binding sites occupied)
- Sideroblastic Anemia (iron is abundant but not utilized)
- Acute Iron Poisoning
- Hemolytic Anemias
- Low Transferrin Saturation
*Click ▾ for more information
Introduction
Iron studies (iron panel) are a valuable tool in interpretation of iron status and management of various iron disorders. Iron studies, also known as iron profile, are a group of blood tests used to assess iron status in the body. The iron studies interpretation help diagnose various iron-related conditions, including:
- Iron Deficiency Anemia: The most common type of anemia, characterized by a lack of red blood cells due to insufficient normal iron levels.
- Iron Overload: A condition where the body accumulates too much iron, which can damage organs.
- Conditions affecting iron absorption or utilization: Chronic inflammatory diseases, liver disease, and certain medications can all impact the normal iron levels.
Iron Cycle and Metabolism in the Body
Iron is a vital mineral that plays a crucial role in many bodily functions. It’s a key component of hemoglobin, the protein in red blood cells that carries oxygen throughout the body. Iron is also essential for energy production, DNA synthesis, and muscle function.
Iron metabolism is a tightly regulated process that ensures the body maintains adequate iron stores for vital functions while preventing iron overload, which can be toxic.
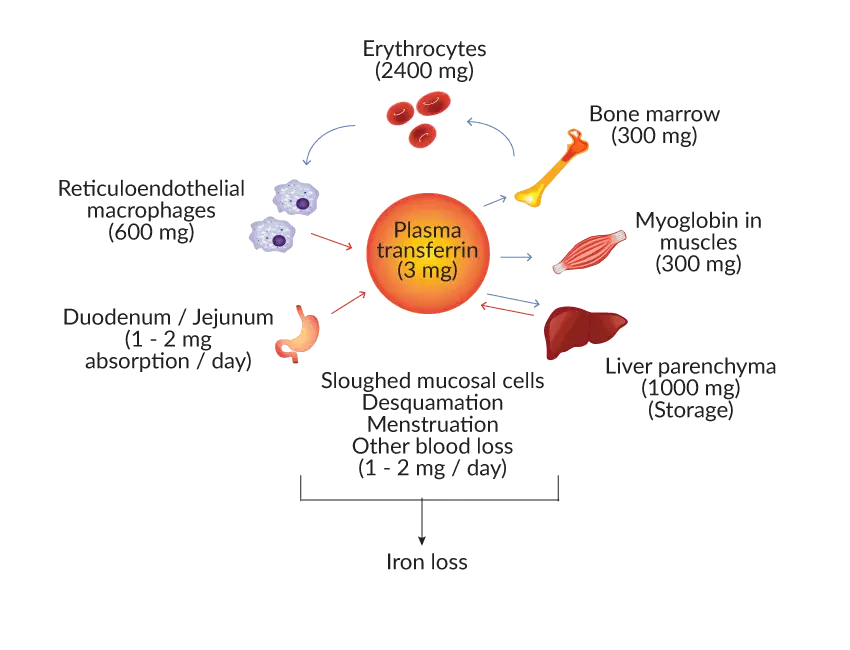
Absorption
Dietary iron from animal sources (heme iron) is absorbed more efficiently than iron from plant sources (non-heme iron). In the small intestine, stomach acid helps convert non-heme iron to a more absorbable form. Intestinal cells take up iron using specific transporters and regulate absorption based on body iron needs.
Transportation
Once absorbed, iron binds to transferrin, a protein in the bloodstream, for transport to various tissues.
Storage
Excess iron is stored in the liver, spleen, and bone marrow bound to ferritin, a protein complex.
Utilization
Bone marrow continuously releases iron for hemoglobin production in red blood cells. Hemoglobin is responsible for carrying oxygen throughout the body.
As red blood cells reach the end of their lifespan (around 120 days), they are broken down by macrophages in the spleen and liver. The iron from these degraded red blood cells is recycled back into the system for new hemoglobin synthesis.
Regulation
Hepcidin, a liver-produced hormone, plays a critical role in regulating iron absorption. High iron stores or inflammation lead to increased hepcidin production, which decreases iron uptake from the intestine.
Conversely, low iron stores or increased erythropoiesis (red blood cell production) stimulate hepcidin suppression to promote iron absorption.
Through this cyclical process, the body strives for iron homeostasis, maintaining a balance between iron absorption, storage, and utilization.
Components of Iron Studies Interpretation
A single iron test is generally insufficient for a proper diagnosis of iron disorders because each component of the iron studies (iron panel) reflects a different aspect of iron metabolism and their values are interdependent. Each component can be influenced by various factors beyond just iron status. Hence, the importance of accurate iron studies interpretation.
For example, serum iron levels can fluctuate throughout the day and are also affected by recent diet, making it an unreliable sole indicator. Ferritin, while the best indicator of iron stores, can be falsely elevated (high ferritin level) during inflammation (as it’s an acute phase reactant), potentially masking a true iron deficiency.
Similarly, transferrin and TIBC levels respond to the body’s need for iron but can also be influenced by conditions like liver disease or chronic inflammation.
Therefore, analyzing all these tests together as an iron panel in the iron studies interpretation allows healthcare providers to get a comprehensive and accurate picture of iron stores, transport, and utilization. This helps to differentiate between true iron deficiency, iron overload, and other conditions that might mimic iron imbalances due to underlying inflammation or disease.
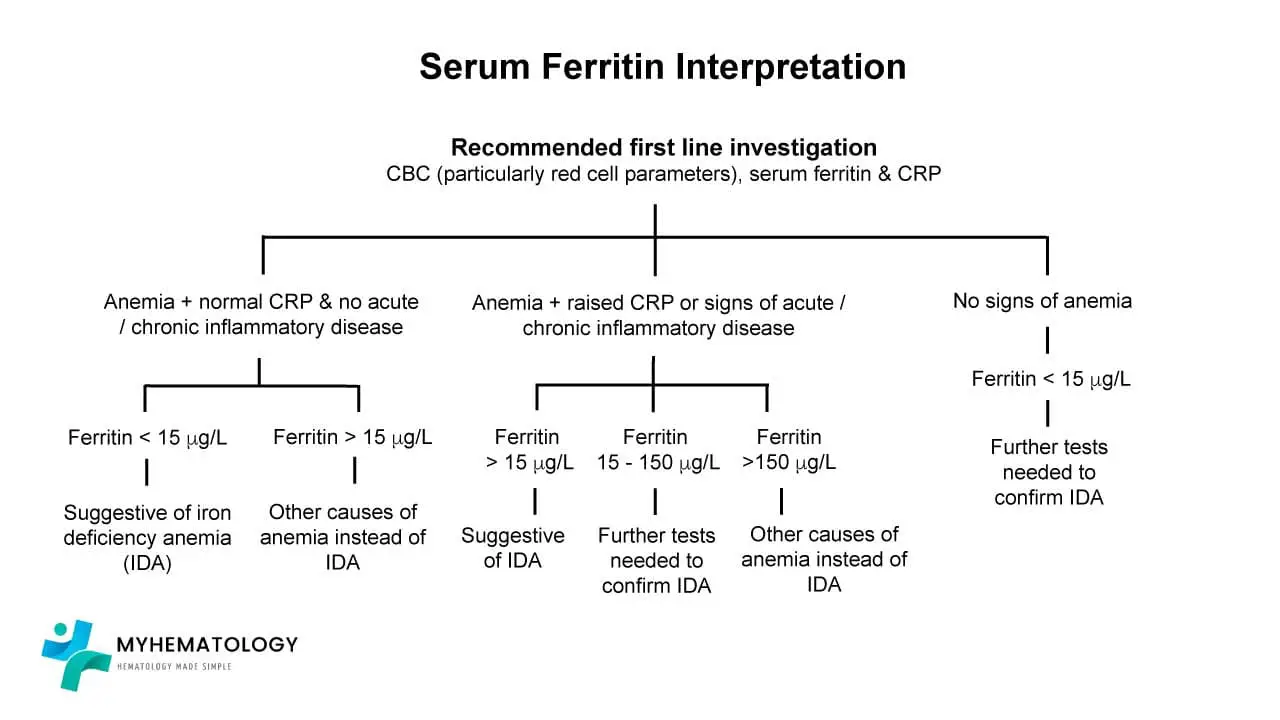
Serum Ferritin in Iron Studies Interpretation
Serum ferritin is a protein found in the blood and tissues that stores iron. Ferritin acts as the body’s major iron storage reservoir, with the highest concentrations found in the liver, spleen, and bone marrow.
Ferritin securely binds excess iron, preventing cellular damage from free iron and creating a reserve for hemoglobin production and other iron-dependent processes. Measuring serum ferritin levels as part of the iron studies interpretation provides an indirect assessment of total body iron stores.
Serum ferritin is a cornerstone test for assessing iron stores and diagnosing iron deficiency or overload. However, its interpretation requires consideration of other factors like inflammation and potential underlying medical conditions.
Expected Values (Iron Studies Reference Ranges)
Normal Range: Serum ferritin levels vary depending on age, sex, and ethnicity.
- Men: 30-300 µg/L (18.3-183 pmol/L)
- Women: 15-300 µg/L (9.2-183 pmol/L)
- Newborns: 25-200 µg/L (15.2-121 pmol/L)
- Children: Values may vary depending on age.
Importance in Iron Studies Interpretation
- High Ferritin level: A high ferritin level in the iron studies interpretation suggests iron overload from excessive dietary intake, chronic blood transfusions, or certain medical conditions like hemochromatosis (genetic disorder affecting iron absorption).
- Low Serum Ferritin: A low ferritin level is a strong indicator of iron deficiency, reflecting depleted iron stores and potentially leading to iron deficiency anemia. It can also be due to blood loss or conditions that limit iron absorption.
Advantages of Serum Ferritin in Iron Studies Interpretation
- Reliable Indicator of Iron Stores: Serum ferritin is a more reliable marker of total body iron stores compared to serum iron, which reflects circulating iron and can fluctuate significantly.
- Less Affected by Diurnal Variation and Inflammation: Unlike serum iron and transferrin, ferritin levels are less affected by diurnal variation and inflammation, making them a more stable measure for iron status assessment in the iron studies interpretation.
Limitations of Serum Ferritin in Iron Studies Interpretation
- Can Be Elevated in Chronic Inflammatory States: While generally a good indicator of iron stores, ferritin levels can be elevated (high ferritin level) in chronic inflammatory conditions (e.g., rheumatoid arthritis) even with iron deficiency. This is because inflammatory cells also store ferritin, leading to falsely high readings.
- Malignancy: Some cancers can also cause high ferritin level, so additional investigations might be needed to differentiate between iron overload and malignancy.
Serum Iron in Iron Studies Interpretation
Serum iron represents the amount of iron circulating in the bloodstream bound to transferrin, the main iron transport protein.
It reflects the iron available for immediate uptake by tissues, particularly the bone marrow for hemoglobin production.
Expected Values (Iron Studies Reference Ranges)
Normal Iron Levels
- Men: 60-170 mcg/dL (11-32 μmol/L)
- Women: 40-150 mcg/dL (7-27 μmol/L)
- Newborns: 100-250 mcg/dL (18-45 μmol/L)
- Children: Values may vary depending on age.
Importance in Iron Studies Interpretation
- Elevated Serum Iron: High serum iron in iron studies interpretation may suggest iron overload from excessive dietary intake or certain medical conditions. However, elevated levels can also be temporary due to recent iron supplementation or liver damage releasing stored iron.
- Low Serum Iron: Low serum iron in iron studies interpretation is a common finding in iron deficiency anemia, indicating insufficient iron for hemoglobin synthesis. It can also be due to blood loss, decreased iron absorption, or inflammatory conditions that sequester iron.
Limitations of Serum Iron in Iron Studies Interpretation
- Diurnal Variation: Serum iron levels fluctuate throughout the day, with higher levels in the morning and lower levels in the afternoon. This necessitates standardized blood draw times for accurate iron studies interpretation.
- Recent Iron Intake/Loss: Recent iron supplementation or blood loss can significantly alter serum iron levels, making iron studies interpretation challenging.
- Inflammation: Inflammatory conditions can decrease serum iron levels even with adequate iron stores, as iron gets trapped within macrophages.
Transferrin in Iron Studies Interpretation
Transferrin is an important component in the iron studies interpretation. Transferrin is a glycoprotein found in the blood plasma. It acts as the major iron transport protein in the body.
Transferrin is responsible for carrying iron from absorption sites in the intestines to tissues that need it. It primarily transports iron to the bone marrow for red blood cell production. Each transferrin binds to two iron atoms at specific binding sites.
Expected Values (Iron Studies Reference Ranges)
Normal Range: 250-370 mg/dL (28-42 μmol/L)
Importance in Iron Studies Interpretation
- Elevated Transferrin: High transferrin level in iron studies interpretation can occur in iron deficiency due to increased production to compensate for low iron stores and facilitate iron uptake. However, elevated transferrin can also be seen in situations unrelated to iron status, like pregnancy, malnutrition, or hormonal imbalances affecting transferrin synthesis.
- Low Transferrin: Low transferrin level in iron studies interpretation may indicate decreased production due to inflammation, liver disease, or protein deficiency. Low transferrin levels can limit iron transport capacity, even if iron stores are adequate.
Limitations of Transferrin in Iron Studies Interpretation
- Diurnal Variation: Similar to serum iron, transferrin levels can fluctuate throughout the day.
- Inflammation: Inflammatory conditions can decrease transferrin production, leading to falsely low transferrin levels and potentially misleading iron studies interpretations. Conversely, inflammation can suppress hepcidin, leading to increased iron release from stores and a temporary rise in transferrin saturation.
- Other Conditions: Pregnancy, hormonal changes, and malnutrition can affect transferrin levels, requiring consideration during interpretation.
Total Iron Binding Capacity (TIBC) in Iron Studies Interpretation
Total Iron Binding Capacity (TIBC) is a measure of the total amount of iron that transferrin can bind to.
It reflects the iron transport capacity of the blood plasma. Transferrin has two iron binding sites, and TIBC essentially represents the maximum amount of iron that transferrin can carry if all its binding sites are occupied.
TIBC is primarily used to calculate transferrin saturation, a more informative indicator of iron availability.
Expected Values (Iron Studies Reference Ranges)
Normal Range: TIBC levels typically range between 250-450 mcg/dL (45-81 μmol/L).
Importance in Iron Studies Interpretation
- High TIBC: A high TIBC in iron studies interpretation is often observed in iron deficiency. The body increases transferrin production to compensate for low iron stores and enhance iron uptake. However, high TIBC can also occur in conditions unrelated to iron status, such as pregnancy, malnutrition, or hormonal imbalances that stimulate transferrin synthesis.
- Low TIBC: A low TIBC in iron studies interpretation may indicate decreased transferrin production due to inflammation, liver disease, or protein deficiency. Low TIBC limits the total iron that can be transported, even if iron stores are adequate.
Limitations of TIBC in Iron Studies Interpretation
- Limited Diagnostic Value on its Own: TIBC reflects iron transport capacity but doesn’t directly assess iron stores or availability. It needs to be interpreted alongside other iron studies like serum iron and transferrin.
- Similar Factors Affecting Transferrin: Diurnal variation, inflammation, and other conditions that influence transferrin levels can also affect TIBC, potentially leading to misinterpretations in iron studies interpretation.
Transferrin Saturation in Iron Studies Interpretation
Transferrin saturation (TSAT) is a calculated value derived from serum iron and transferrin levels.
It expresses the percentage of transferrin binding sites occupied by iron, providing a more informative indicator of iron availability compared to individual measurements of serum iron or transferrin.
Expected Values (Iron Studies Reference Ranges)
Normal Range: Transferrin saturation typically falls within the range of 20-50%.
Importance in Iron Studies Interpretation
- High Transferrin Saturation (Iron Overload): A TSAT above the normal range suggests a high proportion of transferrin is bound to iron, potentially indicating iron overload. This can occur due to excessive dietary iron intake, chronic blood transfusions, or certain medical conditions like hemochromatosis.
- Low Transferrin Saturation (Iron Deficiency): A TSAT below the normal range implies a low proportion of transferrin is occupied by iron, often seen in iron deficiency. This can be due to insufficient iron intake, impaired absorption, or increased iron losses.
Advantages of Transferrin Saturation in Iron Studies Interpretation
- Integrates Transferrin and Iron Levels: TSAT combines information from both transferrin (iron transport capacity) and serum iron (circulating iron) into a single value, providing a more comprehensive picture of iron availability compared to individual tests.
Limitations of Transferrin Saturation in Iron Studies Interpretation
- Affected by Factors Influencing Transferrin and Iron: Conditions that affect transferrin levels (inflammation, malnutrition, hormonal changes) and serum iron levels (diurnal variation, recent iron intake/loss) can also influence TSAT, potentially leading to misinterpretations.
- Not a Standalone Diagnostic Tool: TSAT is valuable but should be interpreted alongside other iron studies (iron panel) and clinical context for a definitive diagnosis.
Other Relevant Markers
Mean Corpuscular Volume (MCV)
The Mean Corpuscular Volume (MCV) is a measurement of the average size and volume of red blood cells (RBCs) in a blood sample. It’s reported in femtoliters (fL). MCV helps assess the overall health and maturity of red blood cells. It’s calculated from values included in a complete blood count (CBC) and isn’t technically part of the iron studies (iron panel) itself. However, MCV is often reported alongside iron studies interpretation because it provides valuable information for interpreting iron status.
Expected Values
Normal Range: MCV typically falls within the range of 80-100 fL.
- Microcytosis (Low MCV): An MCV value below 80 fL suggests microcytic red blood cells and is a strong indicator of iron deficiency anemia. However, other conditions like thalassemia can also cause microcytosis.
- Normocytosis (normal MCV): A normal MCV value suggests red blood cells are average size and isn’t specific to iron deficiency.
- Macrocytosis (high MCV) is not typically associated with iron deficiency anemia.
Limitations of MCV
- While a low MCV can suggest iron deficiency, it’s not diagnostic on its own. Other conditions, such as thalassemia (genetic blood disorder) or anemia of chronic diseases can cause microcytosis.
- MCV can be influenced by recent blood loss or bone marrow problems that affect red blood cell production.
C-Reactive Protein (CRP)
C-reactive protein (CRP) is a protein produced by the liver in response to inflammation in the body. It’s a sensitive marker of acute or chronic inflammatory processes. Higher CRP levels generally indicate the presence of inflammation.
Expected Values
Normal Range: CRP levels are typically considered:
- Low: Less than 1 mg/dL (less than 10 nmol/L)
- Moderately Elevated: 1-3 mg/dL (10-35 nmol/L)
- Highly Elevated: Greater than 3 mg/dL (greater than 35 nmol/L)
Importance in Iron StudiesInterpretation
CRP is not directly involved in iron metabolism, but its measurement can be crucial in iron studies interpretation because inflammation can affect the results of several iron tests:
- Serum Iron: Inflammation can lead to a decrease in serum iron levels even if iron stores are adequate. This is because iron gets trapped within macrophages during the inflammatory response.
- Transferrin: Inflammation can decrease transferrin production, leading to falsely low transferrin levels and potentially misleading interpretations of transferrin saturation. Conversely, acute inflammation might cause a temporary rise in transferrin synthesis.
- Ferritin: While generally a good indicator of iron stores, ferritin levels can be elevated in chronic inflammatory states (e.g., rheumatoid arthritis) even with iron deficiency. This is because inflammatory cells also store ferritin, leading to falsely high readings (high ferritin level).
Hepcidin
Hepcidin is a small peptide hormone produced primarily by the liver. It plays a crucial role in regulating iron absorption from the intestines and iron release from stores.
Hepcidin acts by binding to ferroportin, a protein on the surface of intestinal cells and macrophages that facilitates iron export into the bloodstream. When hepcidin levels are high, it binds to ferroportin, leading to its degradation and preventing iron export. Conversely, low hepcidin levels allow ferroportin to function normally, promoting iron absorption and release.
Importance in Iron Studies Interpretation
Hepcidin measurement is not routinely included in standard iron studies (iron panel) testing due to complexities in the test and ongoing research on its clinical utility. However, understanding its role can be helpful in iron studies interpretation.
- Increased Hepcidin: Can occur in response to inflammation, even with depleted iron stores. This is a protective mechanism to limit iron availability for bacterial growth. High hepcidin can contribute to iron deficiency by hindering intestinal iron absorption. High hepcidin levels can occur in iron overload conditions, but other factors might also contribute to increased hepcidin production (e.g., inflammation).
- Decreased Hepcidin: May be seen in iron deficiency anemia, promoting increased iron absorption to replenish iron stores. Low hepcidin can also occur in conditions with chronic blood loss or ineffective erythropoiesis (red blood cell production).
Limitations of Hepcidin Measurement in Iron Studies Interpretation
- Test Availability: Hepcidin testing is not widely available in clinical settings to be part of iron studies interpretation.
- Complex Interpretation: Hepcidin levels can be influenced by various factors beyond iron status, including inflammation, infection, and certain medications.
- Not a Standalone Diagnostic Tool: Hepcidin measurement is currently used for research purposes and not as a routine diagnostic test for iron disorders.
While not a direct test, understanding hepcidin’s role helps explain why iron studies interpretation might show seemingly contradictory results. For example, someone with iron deficiency anemia might have low serum iron but also elevated ferritin due to inflammation-induced hepcidin increase that traps iron in stores while limiting absorption.
There are no established reference ranges for hepcidin levels due to ongoing development of reliable assays.
Bone Marrow Iron Stores
Bone marrow is a major site for iron storage in the body. Iron is incorporated into ferritin, a protein complex, within bone marrow macrophages. This stored iron serves as a readily available reservoir for hemoglobin production in red blood cells.
Assessing bone marrow iron stores was historically considered the “gold standard” for evaluating the body’s iron status, particularly in cases where peripheral blood tests (like serum ferritin, TIBC, and transferrin saturation) yielded ambiguous results or were confounded by inflammation. This assessment involves a direct examination of the bone marrow.
Importance in Iron Studies (Iron Panel) Interpretation
In complex cases, particularly in patients with chronic inflammatory conditions or liver disease where serum ferritin might be misleading, bone marrow iron assessment can provide a clearer picture of true iron status compared to an iron studies interpretation.
It helps distinguish between:
- Absolute Iron Deficiency: Characterized by absent or markedly reduced iron stores in the marrow and a low percentage of sideroblasts.
- Anemia of Chronic Disease (Functional Iron Deficiency): Often presents with normal or even increased iron stores in the macrophages (trapped iron) but reduced iron in erythroblasts (impaired utilization), indicating that iron is present but not functionally available for erythropoiesis.
- Iron Overload (Hemochromatosis): Shows markedly increased iron stores in the marrow.
- Sideroblastic Anemias: Identified by the presence of abnormal ringed sideroblasts, where iron accumulates in the mitochondria of erythroblasts due to defects in heme synthesis.
Assessment of Bone Marrow Iron Stores
Bone Marrow Aspiration and Biopsy: This invasive procedure involves extracting a small sample of bone marrow for microscopic examination. The collected bone marrow aspirate smears or biopsy sections are then subjected to a special stain called Perls’ Prussian Blue stain.
This stain reacts with ferric iron (Fe3+) in the tissue, causing it to appear blue or black under a microscope.
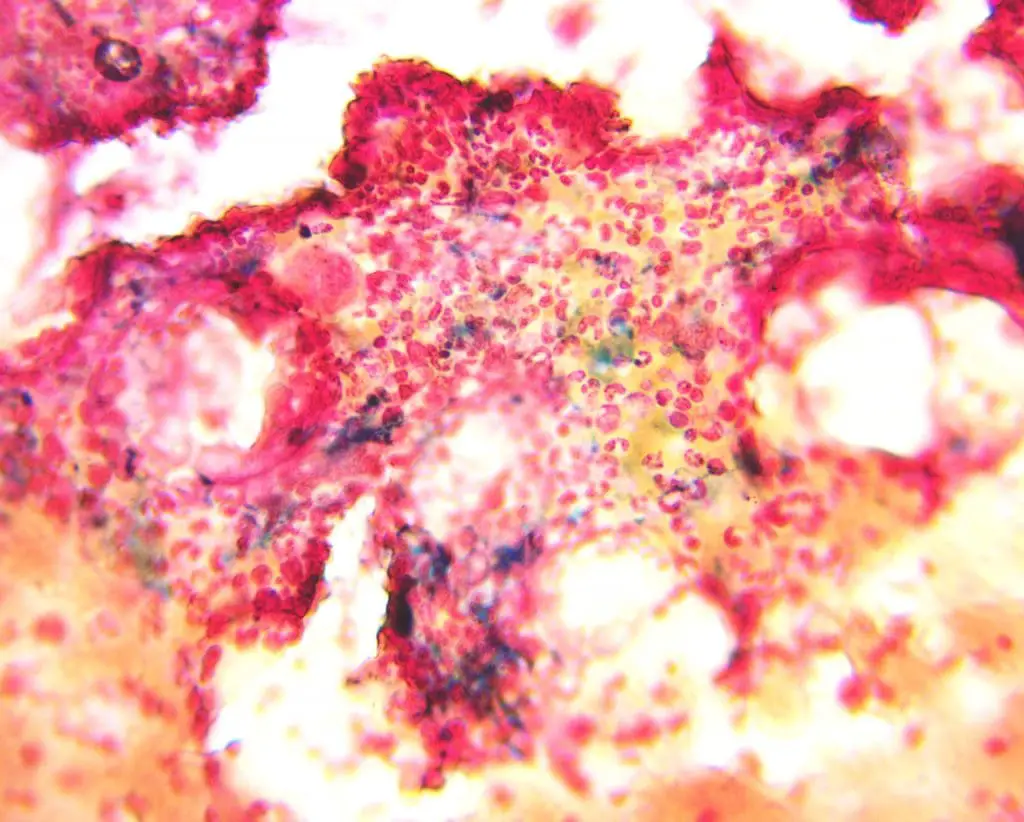
Limitations of Bone Marrow Iron Stain
- Invasiveness: It’s an invasive procedure that carries risks such as pain, bleeding, and infection. This limits its routine use and often reserves it for cases where less invasive tests are insufficient.
- Subjectivity: The grading of iron stores can be somewhat subjective, depending on the pathologist’s experience and the quality of the sample.
- Sampling Error: It’s a localized sample, and while generally representative, there’s a small chance of sampling error if iron distribution is uneven in the marrow.
- Cost and Time: It’s more costly and time-consuming than standard blood tests, as it requires a specialized procedure and expert interpretation.
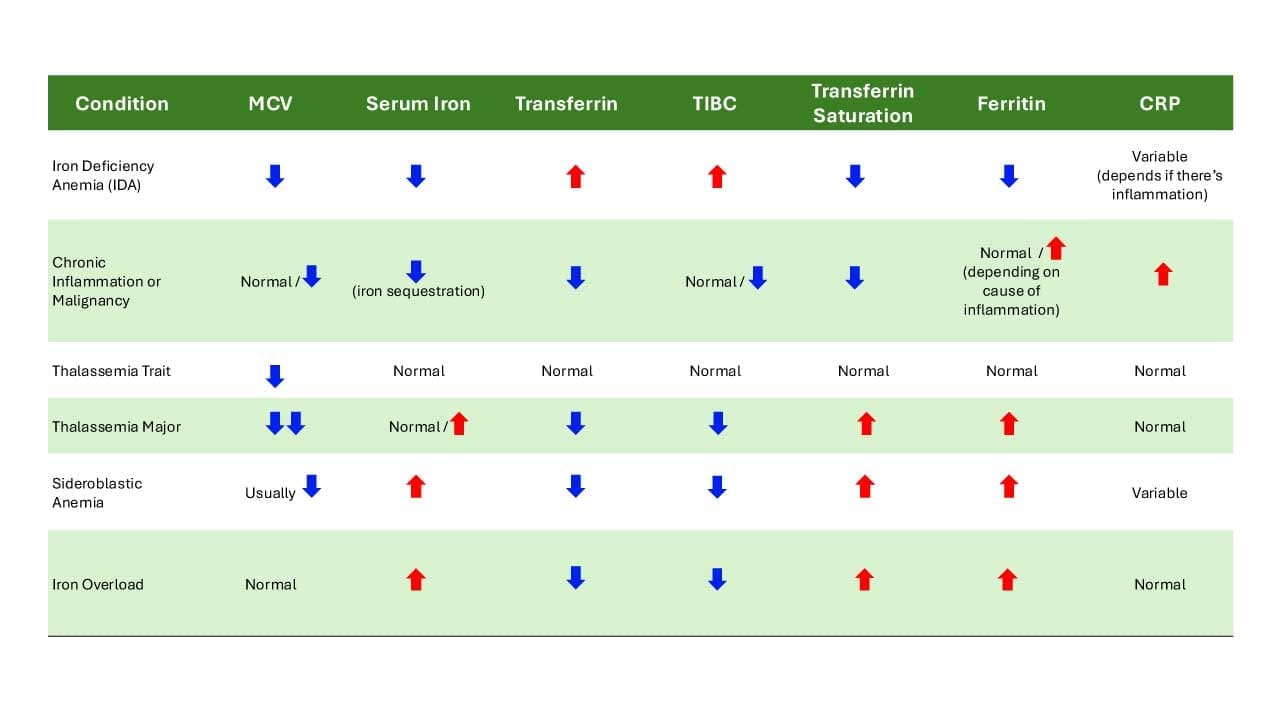
Iron Studies Interpretation Chart
Iron studies interpretation assess various markers to evaluate iron status and diagnose potential iron-related conditions.
Frequently Asked Questions (FAQs)
Do you need to fast before iron studies (iron panel) blood test?
Typically, you do not need to fast for iron studies (iron panel). However, it’s essential to check with your doctor or the laboratory where the test will be performed. Some healthcare providers might prefer a fasting sample for specific reasons, such as to minimize potential interference from food intake which can give false results in the iron studies interpretation.
How do I know if my iron is low again?
Recognizing the signs of low iron can be challenging as symptoms often overlap with other conditions. However, there are some common indicators:
- Fatigue and weakness: Feeling unusually tired or weak.
- Shortness of breath: Difficulty breathing, even with mild exertion
- Pale skin: A noticeable paleness in your skin, lips, and nail beds.
- Cold hands and feet: Often feeling chilly, even in warm environments.
- Headaches: Frequent or severe headaches.
- Dizziness or lightheadedness: Feeling faint or unbalanced.
What happens if ferritin is low?
Low ferritin level typically indicates iron deficiency. Ferritin is a protein that stores iron in the body, so low ferritin level means that the iron stores are depleted. Iron deficiency can lead to iron deficiency anemia. This condition occurs when the body doesn’t have enough red blood cells to carry oxygen efficiently.
Can you have low ferritin but not anemic?
Yes, it’s possible to have low ferritin level without being anemic.
Ferritin is a protein that stores iron in your body. A low ferritin level indicates that the iron stores are depleted, but it doesn’t necessarily mean you’re anemic yet. Anemia occurs when the body doesn’t have enough red blood cells to carry oxygen effectively.
This stage is often referred to as latent iron deficiency or iron deficiency without anemia. While there may be no anemia symptoms at this point, it’s important to address low ferritin level to prevent progressing to anemia.
What level of ferritin is concerning?
The definition of a “concerning” ferritin level can vary depending on individual factors such as age, sex, and overall health. However, general guidelines can provide some insight.
- Low ferritin level: Low ferritin level below the normal range can indicate iron deficiency. While exact values can vary by laboratory, a low ferritin level consistently below 15 ng/mL warrants further investigation.
- High ferritin level: High ferritin level significantly above the normal range can indicate iron overload, inflammation, or certain medical conditions. While normal ranges vary, a high ferritin level consistently above 400 ng/mL requires evaluation.
How long does it take to raise ferritin levels?
Typically, it takes around 3 months to significantly increase ferritin levels. However, this timeframe can vary depending on several factors, including:
- Severity of iron deficiency: The more depleted the iron stores are, the longer it may take to replenish them.
- Type of iron supplement: Oral iron supplements generally take longer to work compared to intravenous iron therapy.
- Underlying cause of low ferritin: Addressing the root cause of iron deficiency can also impact the time it takes to raise ferritin levels.
It’s important to note that while ferritin levels may take a few months to normalize, a person might start to feel improvements in energy and other symptoms within a few weeks of starting iron supplementation.
Regular blood tests will help monitor progress and ensure the treatment plan is effective.
Do iron supplements increase ferritin levels?
Yes, iron supplements can increase ferritin levels.
Ferritin is a protein that stores iron in the body. By increasing iron intake through supplements, the raw material is provided for the body to build up its iron stores. Over time, this will lead to an increase in ferritin levels.
However, it takes time for iron to be replenished in the body. There may not be an immediate increase in ferritin levels, and regular blood tests are necessary to monitor progress.
What is the root cause of low ferritin level?
Low ferritin level typically indicate iron deficiency, which can stem from various causes including inadequate iron intake, chronic blood loss (menstrual, gastrointestinal bleeding), impaired iron absorption due to conditions like celiac disease or inflammatory bowel disease, or increased iron demand during pregnancy or rapid growth.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- World Health Organization. Iron deficiency anemia: Assessment, prevention, and control of a global public health problem. World Health Organization; 2008.
- Short MW, Domagalski JE. Iron deficiency anemia: evaluation and management. Am Fam Physician. 2013 Jan 15;87(2):98-104. PMID: 23317073.
- Goldberg S, Hoffman J. Clinical Hematology Made Ridiculously Simple, 1st Edition: An Incredibly Easy Way to Learn for Medical, Nursing, PA Students, and General Practitioners (MedMaster Medical Books). 2021.
- Garrison C. The Iron Disorders Institute Guide to Anemia: Understanding the Causes, Symptoms, and Healing of Iron Deficiency and Other Anemias (Cumberland House). 2009.
- Kelly, A. U., McSorley, S. T., Patel, P., & Talwar, D. (2017). Interpreting iron studies. BMJ (Clinical research ed.), 357, j2513. https://doi.org/10.1136/bmj.j2513
- Fertrin K. Y. (2020). Diagnosis and management of iron deficiency in chronic inflammatory conditions (CIC): is too little iron making your patient sick?. Hematology. American Society of Hematology. Education Program, 2020(1), 478–486. https://doi.org/10.1182/hematology.2020000132
- Faruqi A, Zubair M, Mukkamalla SKR. Iron-Binding Capacity. [Updated 2024 May 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559119/



