TL;DR
Lymphoma is a group of cancers affecting the lymphatic system, vital for immunity.
- Types ▾:
- Hodgkin Lymphoma ▾: Characterized by Reed-Sternberg cells, generally better response to treatment.
- Non-Hodgkin Lymphoma (NHL) ▾: Diverse group with various subtypes and prognoses (DLBCL, follicular, Burkitt, etc.)
- Common symptoms ▾: Swollen lymph nodes, fever, night sweats, fatigue & unexplained weight loss
- Risk factors ▾:
- Age (peaks in young adults and elderly)
- Weakened immune system (HIV/AIDS, organ transplants, autoimmune diseases)
- Previous infections (Epstein-Barr virus)
- Family history
- Obesity
- Smoking
- Diagnosis ▾: Biopsy is crucial to determine specific subtypes.
- Treatment ▾: Common modalities include chemotherapy, radiation therapy, immunotherapy, and stem cell transplantation
*Click ▾ for more information
Introduction
Lymphoma is a type of cancer that originates in the lymphatic system, a key part of the body’s immune system. It specifically begins when lymphocytes begin to grow and multiply uncontrollably.
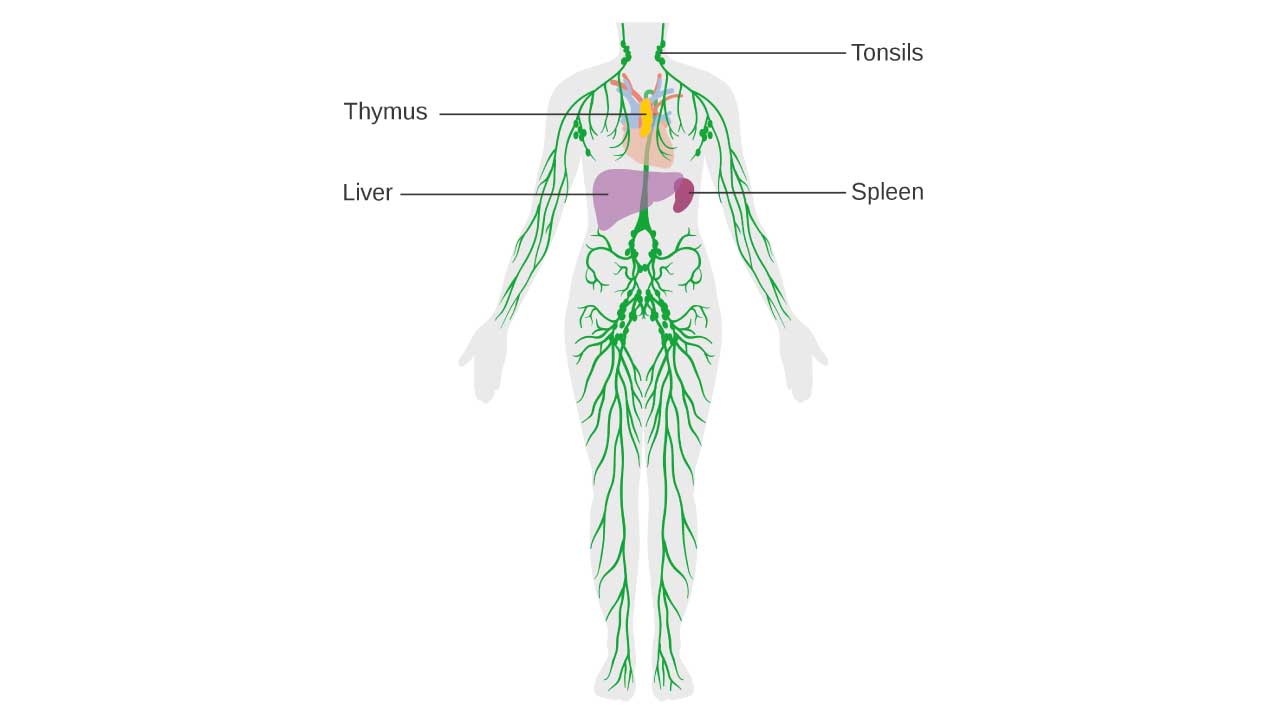
What is the lymphatic system and its role in immunity?
The lymphatic system is a network of vessels, tissues, and organs that play a crucial role in immunity. It acts as the body’s drainage system, collecting excess fluid and waste products from tissues and filtering them before returning them to the bloodstream.
Additionally, it plays a vital role in the immune system by:
- Producing lymphocytes: These are white blood cells, specifically B and T cells, that fight infections and diseases. The lymphatic system houses numerous lymph nodes, which are specialized structures where lymphocytes mature and multiply.
- Filtering out harmful substances: As lymph fluid flows through the lymphatic vessels, it passes through lymph nodes, where specialized immune cells trap and destroy bacteria, viruses, and other pathogens.
- Transporting immune cells: The lymphatic system provides a pathway for white blood cells to travel throughout the body, allowing them to reach sites of infection and inflammation.
- Drain excess fluid: It collects interstitial fluid that leaks from blood vessels and prevents tissue swelling.
Structure and Functions of the Lymphatic System
Vessels
Lymphatic vessels are responsible for transporting lymph fluid, a clear, watery substance resembling plasma. Unlike blood vessels, they have one-way valves to ensure fluid flows towards the heart. These tiny vessels begin blindly in tissues, collecting excess fluid. They merge into larger channels, eventually forming two main trunks: the thoracic duct (draining the left arm and most of the body below the diaphragm) and the right lymphatic duct (draining the right arm and head/neck region).
Lymph nodes are bean-shaped structures are scattered along the lymphatic vessels, acting as immune checkpoints. Inside, lymphocytes filter the lymph, trapping and destroying pathogens.
Organs
- Lymph nodes: Over 600 lymph nodes are strategically located throughout the body, with clusters in the neck, armpits, groin, and chest. Their size and activity can change based on immune response, causing “swollen lymph nodes” when fighting infection.
- Spleen: Located in the left upper abdomen, the spleen filters both blood and lymph, removing old red blood cells and debris while also housing immune cells.
- Thymus: Situated in the chest, the thymus plays a crucial role in T lymphocyte development during childhood. It shrinks with age, but its function continues in the bone marrow.
Regional Breakdown
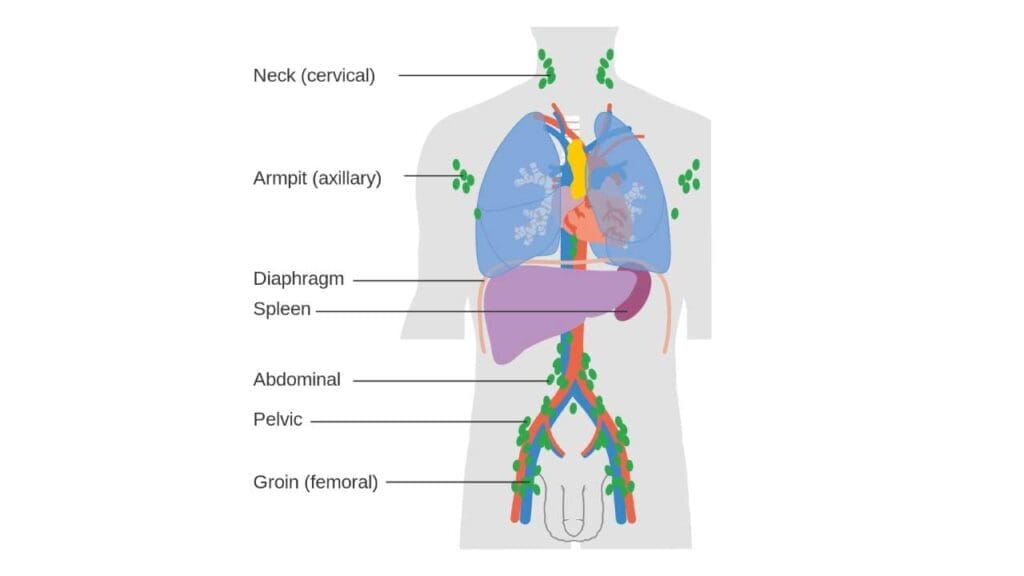
- Head and Neck
- Cervical lymph nodes: Located around the neck, they filter lymph fluid from the head, scalp, face, and ears. Swollen cervical lymph nodes can indicate infection, inflammation, or even lymphoma.
- Tonsils: These lymphoid tissues in the throat trap and destroy pathogens entering through the mouth or nose.
- Thymus: Located in the chest near the heart, it plays a vital role in T-cell development during childhood and adolescence.
- Chest
- Mediastinal lymph nodes: These nodes surround the heart and lungs, filtering lymph from the chest cavity and upper body.
- Spleen: This large organ filters blood and lymph, removing old red blood cells and producing immune cells.
- Thoracic duct: This large vessel collects lymph from the lower body and empties it into the bloodstream near the left collarbone.
- Abdomen and Pelvis
- Mesenteric lymph nodes: Located in the abdomen, they filter lymph from the digestive organs.
- Inguinal lymph nodes: Found in the groin area, they filter lymph from the lower limbs and genitals.
- Axillary lymph nodes: Situated under the armpits, they filter lymph from the arms and upper chest.
- Arms and Legs
- Superficial lymphatic vessels: These vessels run just below the skin, collecting lymph from tissues.
- Deep lymphatic vessels: Located deeper within the body, they drain lymph from muscles and other internal structures.
- Additional Components
- Lacteals: Tiny lymphatic vessels in the small intestine that absorb dietary fats and transport them to the lymphatic system.
- Peyer’s patches: Clusters of lymphoid tissue in the small intestine that help fight infections.
- Important Functions by Region
- Head and Neck: Protects against infections entering through the mouth and nose.
- Chest: Filters lymph from the lungs and heart, aiding in respiratory and cardiovascular health.
- Abdomen and Pelvis: Supports digestion by absorbing fats and filtering lymph from abdominal organs.
- Arms and Legs: Maintains fluid balance and fights infections in the limbs.
Functions Beyond Immunity
- Fat absorption: In the intestine, dietary fats are absorbed into tiny lymphatic vessels called lacteals and transported to the bloodstream.
- Wound healing: The lymphatic system plays a role in wound healing by transporting immune cells and removing debris.
Disorders and Dysfunction
Unfortunately, the lymphatic system isn’t immune to problems. Lymphedema, caused by blockage or damage to lymph vessels, leads to fluid buildup and swelling. Lymphoma, a cancer of lymphocytes, can disrupt the immune system and require specialized treatment.
Lymphoma vs Leukemia
Both lymphoma and leukemia are types of blood cancer, but they differ in their origin, spread, and specific types.
| Feature | Lymphoma | Leukemia |
| Origin | Lymphatic system | Bone marrow |
| Affected cells | Lymphocytes | Various blood cells, including lymphocytes |
| Primary spread | Lymphatic system | Bloodstream |
| Main types | Hodgkin and Non-Hodgkin | Lymphocytic and Myelogenous |
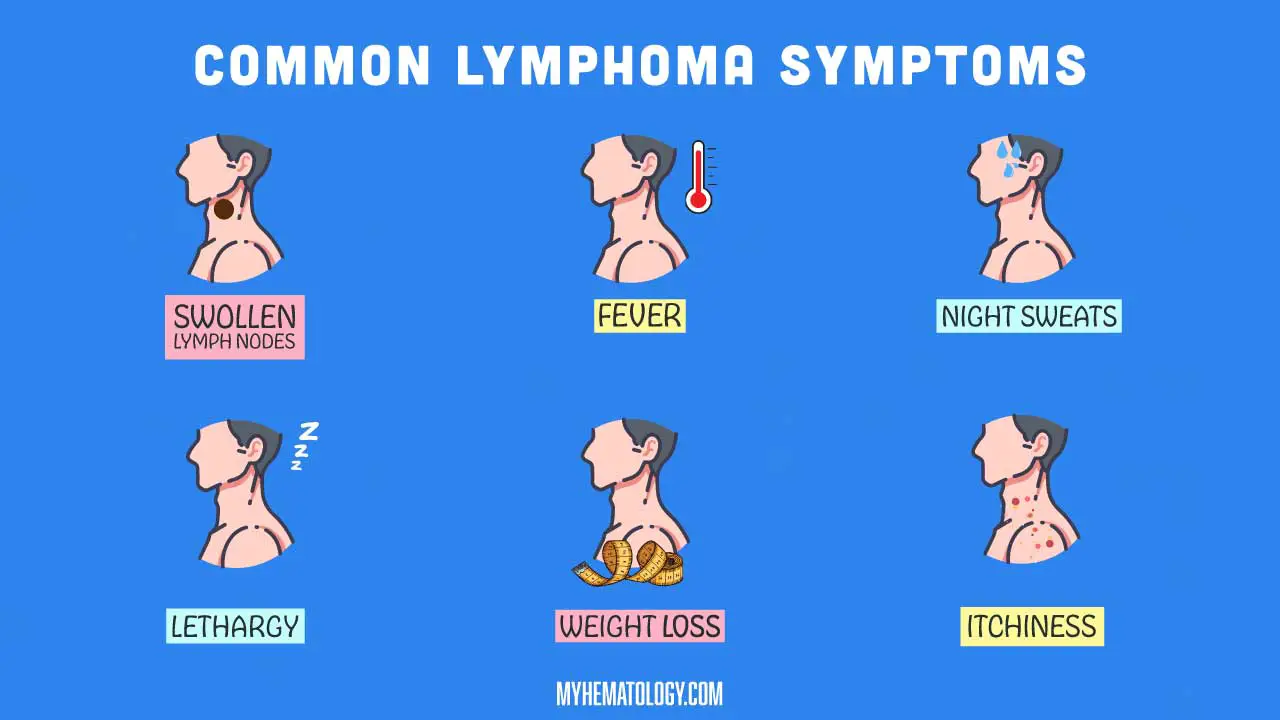
General Signs and Symptoms
- Swollen lymph nodes (lymphadenopathy): This is the most common symptom, occurring in both malignant and benign forms. Swollen nodes may be painless or tender, and can appear in the neck, armpits, groin, chest, or other areas.
- Fever: Unexplained fever that persists for several days or weeks.
- Night sweats: Drenching sweats at night, even in cool environments.
- Fatigue: Persistent tiredness and lack of energy are common symptoms.
- Unexplained weight loss: Losing weight without trying can be a warning sign.
- Itching: Some people experience persistent itching all over their body, but this is more common in certain malignant subtypes.
Red Flags Requiring Immediate Attention
- Rapidly enlarging lymph nodes: If a lymph node swells quickly or becomes noticeably larger within a short period.
- Night sweats that soak your clothes and sheets: While occasional night sweats can be unrelated, drenching sweats that happen every night often require investigation.
- Unexplained fever persisting for more than two weeks: A fever without an apparent cause, especially if accompanied by other lymphoma symptoms.
- Significant weight loss (10% or more of body weight) within a few months: While weight loss can have various causes, rapid and unexplained weight loss can be a red flag for several conditions, including lymphoma.
- Difficulty breathing or chest pain: These symptoms could indicate lymphoma affecting the lungs or chest cavity.
- Bone pain or persistent headaches: These can be signs of advanced lymphoma and merit investigation.
Risk Factors or Causes
While the cause of lymphoma remains complex, certain factors can increase the risk of developing it.
Age
Lymphoma exhibits two peaks in occurrence. The first occurs in young adults between 20-40 years old, especially for Hodgkin lymphoma. The second peak appears in the elderly population, over 60 years old, mainly affecting Non-Hodgkin lymphoma (NHL).
Weakened Immune System
- HIV/AIDS: Individuals with HIV/AIDS have a significantly higher risk of developing NHL due to a compromised immune system.
- Organ transplants: Medications to suppress the immune system after organ transplants increase the risk of certain types of NHL.
- Autoimmune diseases: Conditions like rheumatoid arthritis or lupus, where the immune system attacks the body’s own tissues, can slightly elevate the risk of lymphoma.
Previous Infections
- Epstein-Barr virus (EBV): This common virus is linked to an increased risk of developing certain NHL subtypes, like Burkitt’s lymphoma.
- Other infections: Less commonly, infections with Human T-cell lymphotropic virus (HTLV-1) or Helicobacter pylori (H. pylori) have been associated with specific lymphoma types.
Family History
Having a close relative (parent, sibling, or child) with lymphoma slightly increases individual risk. However, most cases are not considered hereditary.
Other Potential Factors
- Obesity: Recent research suggests a possible link between obesity and some NHL subtypes, but the exact mechanism is unclear.
- Smoking: Tobacco smoking is associated with an increased risk of developing certain NHL subtypes, potentially due to its immunosuppressive effects.
Types of Lymphoma
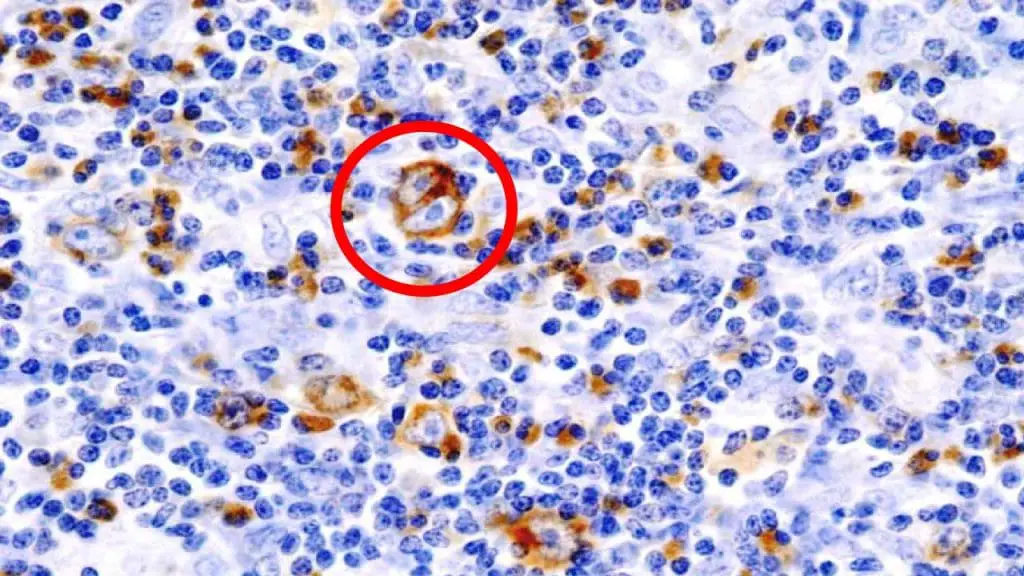
Hodgkin Lymphoma
Hodgkin lymphoma is characterized by the presence of Reed-Sternberg cells which are large abnormal lymphocytes. Hodgkin lymphoma can be further divided into classical (more common) and nonclassical subtypes.
- Clinical features: Typically presents with painless, persistent swollen lymph nodes, fever, night sweats, and weight loss.
- Microscopic appearance: Reed-Sternberg cells are key, along with specific patterns of surrounding lymphocytes.
- Prognosis and treatment: Generally has better response rates to treatment compared to NHL, with various approaches depending on the subtype and stage.
Non-Hodgkin Lymphoma (NHL)
A vast and diverse category encompassing over 70 subtypes, each with distinct characteristics.
- Major Types
- Diffuse Large B-cell Lymphoma (DLBCL): An aggressive type with rapid growth, often requiring intensive treatment.
- Follicular Lymphoma: A slower-growing type, often managed with watchful waiting or less intensive therapy.
- Burkitt Lymphoma: Highly aggressive, requiring immediate and intensive therapy.
- T-cell Lymphoma: Represents about 10% of NHL cases, with diverse subtypes and varying prognoses.
- Clinical features: Symptoms vary depending on the specific subtype and can range from mild to severe.
- Microscopic appearance: No single defining feature, diagnosis relies on specific cell types, growth patterns, and immunohistochemistry.
- Prognosis and treatment: Varies greatly depending on the subtype, stage, and other factors. Treatments encompass chemotherapy, radiation, immunotherapy, and stem cell transplantation.
Comparison of Hodgkin and Non-Hodgkin Lymphoma
| Feature | Hodgkin Lymphoma (HL) | Non-Hodgkin Lymphoma (NHL) |
| Defining Cell | Characterized by the presence of Reed-Sternberg (RS) cells, which are large, abnormal lymphocytes that resemble owl eyes under a microscope. | Does not have Reed-Sternberg cells. This is the key distinction. |
| Origin of Cancer Cells | Almost always originates from B-lymphocytes. | Can originate from either B-lymphocytes (most common) or T-lymphocytes (less common). |
| Spread Pattern | Tends to spread in an orderly, contiguous fashion from one lymph node group to the next. | Spreads in a more unpredictable and non-contiguous way, often skipping lymph node groups. |
| Location | Usually begins in the upper body (e.g., in the lymph nodes of the neck, chest, or armpits). | Can start in lymph nodes anywhere in the body, and is more likely to originate in organs outside the lymphatic system. |
General Laboratory Investigations
A comprehensive evaluation of suspected lymphoma typically involves a combination of clinical presentation, physical examination, and various laboratory investigations.
Complete Blood Count (CBC)
- Anemia: Common due to bone marrow infiltration by lymphoma cells, leading to decreased RBC production.
- Leukocytosis: Elevated WBCs, often with an abnormal WBC morphology like atypical lymphocytes (abnormal appearance) suggestive of lymphoma.
- Thrombocytopenia: Less common, but may occur due to bone marrow involvement or other factors like splenomegaly.
Peripheral Blood Smear
Identification of abnormal lymphocytes suggestive of lymphoma based on size, shape, nuclear features, and presence of nucleoli (structures within the nucleus).
Lymph Node Biopsy
This procedure is considered the gold standard for diagnosing and classifying most lymphomas, alongside bone marrow aspiration and biopsy.
Flow Cytometry
Detection of a specific immunophenotype characteristic of a particular type of lymphoma.This helps differentiate between different types of lymphocytes and identify lymphoma cells based on their unique immunophenotype (marker expression pattern).
Bone Marrow Aspiration and Biopsy
Identification of abnormal lymphocytes in the bone marrow, confirming the diagnosis and providing information on the extent of involvement.
Lactate Dehydrogenase (LDH)
Elevated LDH might indicate a more aggressive disease course, but interpretation requires caution alongside other clinical findings.
Additional Tests
Depending on the specific clinical presentation and suspected type of lymphoma, additional investigations like cytogenetic analysis (chromosome abnormalities) or molecular testing (genetic mutations) might be employed for further characterization and prognostication.
Current Treatment Options
The battle against lymphoma involves a personalized strategy tailored to the specific type and stage of the disease.
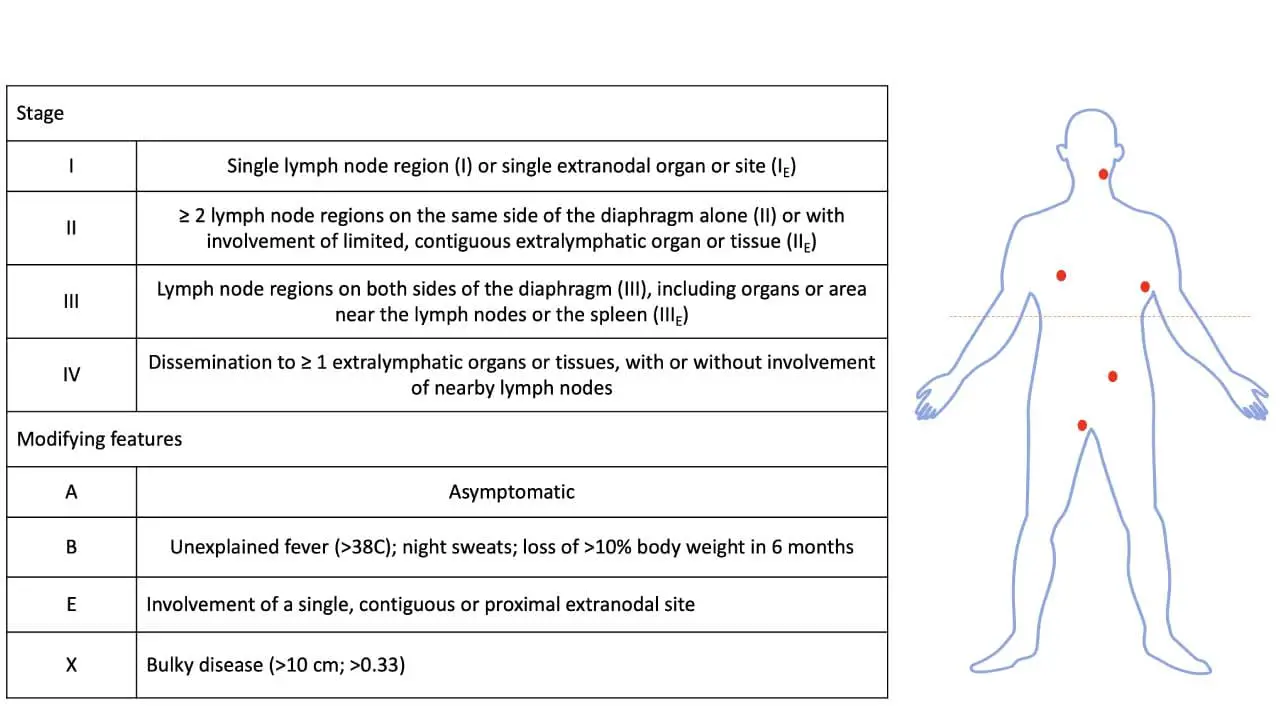
Staging and Type Guide Treatment
- Staging: This system categorizes lymphoma based on the extent of its spread, guiding treatment intensity and duration.
- Type: Different lymphoma types respond differently to specific therapies, influencing the chosen treatment approach.
Common Treatment Modalities
Chemotherapy
- Function: Uses powerful drugs to kill cancer cells throughout the body.
- Regimens: Different combinations of drugs are used depending on the type and stage of lymphoma. Common regimens include CHOP, R-CHOP, and ABVD.
- Side effects: Can vary but may include nausea, vomiting, hair loss, fatigue, and increased risk of infection.
Radiation therapy
- Function: Uses high-energy beams to target and kill cancer cells in specific areas.
- Applications: Often used in conjunction with chemotherapy, particularly for localized lymphoma or after surgery to remove affected lymph nodes.
- Side effects: Can include skin irritation, fatigue, and long-term effects on surrounding organs depending on the treated area.
Immunotherapy
- Function: Boosts the body’s immune system to recognize and attack cancer cells.
- Types: Targeted therapies like rituximab specifically target specific molecules on lymphoma cells, while other types help activate the immune system more broadly.
- Side effects: Can vary depending on the specific therapy, but may include infusion reactions, fatigue, and skin reactions.
Stem cell transplantation
- Function: Replaces damaged bone marrow with healthy stem cells, often after high-dose chemotherapy or radiation.
- Uses: Used in some aggressive lymphoma cases or when other treatments haven’t been successful.
- Considerations: Requires careful evaluation and carries significant risks of complications.
Supportive care measures
- Symptom management: Medications and other interventions to address symptoms like pain, fatigue, and nausea.
- Nutritional support: Ensuring proper nutrition to maintain strength and fight infection.
Emerging treatment options
The field of lymphoma treatment is constantly evolving, with new and promising options emerging all the time. Here are some exciting avenues currently being explored:
- Antibody-drug conjugates (ADCs): These drugs combine a monoclonal antibody that specifically targets cancer cells with a potent cytotoxic agent. This allows for targeted delivery of the chemotherapy, minimizing harm to healthy cells. Polatuzumab vedotin is an example already approved for some NHL subtypes, and several others are in clinical trials.
- Bispecific T-cell engagers (BiTEs): These molecules act as bridges, connecting T-cells (immune cells) to cancer cells, triggering the T-cells to destroy the lymphoma cells. Blinatumomab is an approved BiTE therapy for certain aggressive NHL types, and others are being studied for different subtypes.
- CAR T-cell therapy: This personalized approach involves engineering a patient’s own T-cells to recognize and attack their specific lymphoma cells. Several CAR T-cell therapies are showing promising results in clinical trials for NHL, and one (Kymriah) is already approved for certain situations.
- Immune checkpoint inhibitors: These drugs work by blocking molecules that dampen the immune system’s response, allowing it to better recognize and fight cancer cells. While not yet standard in lymphoma treatment, checkpoint inhibitors are showing promise in clinical trials for various subtypes.
- Targeted therapies: These drugs focus on specific mutations or pathways involved in lymphoma growth and survival. Several targeted therapies are already approved for specific NHL subtypes, and many more are being investigated in clinical trials.
- Gene therapy: This approach aims to correct genetic abnormalities contributing to lymphoma by introducing healthy genes or editing existing ones. While still in early stages, gene therapy offers potential for future personalized treatment options.
Prognosis and Survival Rates
Early diagnosis plays a critical role in improving lymphoma prognosis and survival rates. Prognosis and survival rates vary greatly between different lymphoma types, stages, and individual patient characteristics.
Hodgkin Lymphoma
Hodgkin lymphoma generally has better survival rates than NHL, with 5-year survival rates exceeding 80% for early-stage disease and over 50% for advanced stages with appropriate treatment. Prognosis further depends on specific subtypes, with classical type having better outcomes than nonclassical subtypes.
Non-Hodgkin Lymphoma (NHL)
Prognosis is highly diverse, depending on the specific subtype, stage, and other factors.
- Diffuse Large B-cell Lymphoma (DLBCL): An aggressive type with 5-year survival rates of around 70% for early-stage and 50% for advanced-stage disease with treatment.
- Follicular Lymphoma: A slower-growing type, with 10-year survival rates exceeding 90% for early-stage disease but requiring long-term management.
- Burkitt Lymphoma: A highly aggressive type with 5-year survival rates of 80-90% with intensive treatment, emphasizing the importance of early diagnosis and prompt intervention.
- T-cell Lymphoma: A diverse group with varying prognoses depending on the specific subtype. Some subtypes have favorable outcomes, while others are more challenging.
Nutrition and Lymphoma
While there isn’t a single “good” diet specifically for lymphoma, nutritional considerations play a crucial role in supporting patients throughout treatment and recovery.
Key Nutritional Challenges
- Increased energy needs: Treatment can increase metabolic demands, requiring adequate calorie intake.
- Side effects impacting nutrition: Nausea, vomiting, mouth sores, and diarrhea can hinder food intake and nutrient absorption.
- Weakened immune system: Proper nutrition is vital to support immune function and fight infections.
Dietary Recommendations
- Maintain a healthy weight: Being overweight or obese can increase the risk of certain cancers, including lymphoma. If you’re overweight or obese, losing weight gradually can be helpful.
- Boost your immune system: A healthy immune system can help your body fight off infection and potentially aid in recovery.
- Reduce inflammation: Inflammation can worsen some cancer symptoms and may play a role in cancer development.
- Manage side effects of treatment: Some cancer treatments can cause side effects like nausea, vomiting, and diarrhea. Eating a healthy diet can help manage these side effects.
- Eat plenty of fruits, vegetables, and whole grains: These foods are rich in vitamins, minerals, and fiber, which can help boost your immune system and reduce inflammation. Aim for at least five servings of fruits and vegetables per day.
- Choose lean protein sources: Lean protein sources, such as fish, poultry, beans, and lentils, can help you maintain muscle mass and strength during treatment.
- Limit unhealthy fats: Limit unhealthy fats, such as saturated and trans fats, and choose healthy fats, such as those found in avocados, nuts, and seeds.
- Limit added sugar and refined carbohydrates: Added sugar and refined carbohydrates can contribute to inflammation and weight gain. Limit sugary drinks, processed foods, and white bread.
- Stay hydrated: Drinking plenty of fluids throughout the day can help prevent dehydration, which is a common side effect of some cancer treatments.
Management of specific side effects of cancer treatment
- Nausea and vomiting: Ginger, bland foods, and anti-nausea medications can be helpful.
- Mouth sores: Soft, cool foods, sugar-free mouthwashes, and pain medication can offer relief.
- Diarrhea: BRAT diet (bananas, rice, applesauce, toast) and electrolyte replacement solutions might be recommended.
Individualized Approach
- Assess individual needs, preferences, and cultural considerations when providing dietary advice.
- Consult registered dietitians or nutritionists for personalized meal plans and guidance on managing side effects through diet.
- Monitor weight and nutritional status throughout treatment and adjust recommendations as needed.
Additional Considerations
- Specific dietary restrictions: Some treatments might require specific dietary restrictions, like avoiding certain foods or supplements.
- Complementary and alternative medicine (CAM): Discuss the potential risks and benefits of any CAM approaches related to diet with patients before they use them.
While diet alone cannot cure lymphoma, it plays a crucial role in supporting patients physically and emotionally during treatment.
Exercise and Lymphoma
While there isn’t a single “perfect” exercise program for all lymphoma patients, incorporating physical activity into their care plan offers numerous benefits and should be encouraged.
Benefits of Exercise in Lymphoma
- Improved physical fitness: Exercise helps maintain muscle mass, bone density, and cardiovascular health, which can be compromised during treatment.
- Reduced fatigue: Regular physical activity can combat fatigue, a common symptom in lymphoma patients.
- Improved mood and well-being: Exercise can reduce stress, anxiety, and depression, enhancing overall quality of life.
- Potential benefits for treatment response: Some studies suggest exercise might improve treatment response and reduce side effects.
Key Considerations
- Individualized approach: Assess each patient’s fitness level, limitations, and treatment side effects before recommending specific exercises.
- Start slowly and gradually progress: Begin with low-intensity, short-duration exercises and gradually increase intensity and duration as tolerated.
- Listen to the body: Encourage patients to rest when needed and avoid overexertion.
- Adapt exercises to limitations: Modify exercises to accommodate fatigue, pain, or other limitations.
- Safe exercise environments: Recommend activities in safe, clean spaces to avoid infections, especially during periods of neutropenia.
- Clear communication with the healthcare team: Collaborate with other healthcare professionals involved in the patient’s care to ensure exercise doesn’t interfere with treatment or recovery.
- Lymphedema: Avoid exercises that strain the affected area or restrict lymphatic flow. Consult a therapist for specific recommendations.
- Neutropenia: Opt for low-impact activities minimizing risk of injury and infection.
Suitable Exercise Types
- Aerobic activities: Brisk walking, swimming, cycling, dancing (moderate intensity, 30 minutes most days of the week).
- Strength training: Light weights, resistance bands, bodyweight exercises (2-3 times per week).
- Flexibility exercises: Stretching, yoga (gentle and adapted if needed).
Specific Considerations by Lymphoma Type
- Hodgkin lymphoma: Generally well-tolerated with exercise, but monitor for fatigue and adjust intensity accordingly.
- Non-Hodgkin lymphoma (NHL): Individualized approach based on specific subtype, stage, and treatment side effects.
- Lymphoma involving bone or joint pain: Low-impact activities like swimming or water aerobics might be preferred.
- Lymphoma affecting the chest: Monitor for shortness of breath or chest pain during exercise and adjust intensity if needed
Lymphoma and Hormonal Imbalance
While the link between lymphoma and hormonal imbalance is not straightforward and not always present, there are some connections between the two.
Potential Effects of Lymphoma on Hormone Levels
- Direct Disruption of Hormone-Producing Organs: In some cases, lymphoma can directly infiltrate and damage organs responsible for hormone production, such as the:
- Pituitary gland: Located in the brain, it regulates the production of many other hormones.
- Adrenal glands: Located above the kidneys, they produce various hormones, including cortisol and sex hormones.
- Gonads (ovaries and testes): These organs produce sex hormones like estrogen, progesterone, and testosterone.
- Indirect Effects through Cytokines: As mentioned previously, lymphoma cells release cytokines, which can have various effects on the body. Some cytokines can potentially:
- Interfere with hormone production by disrupting signaling pathways in hormone-producing cells.
- Alter the body’s sensitivity to hormones, affecting how they function despite normal production levels.
Specific Examples of Hormonal Imbalances in Lymphoma
- Hodgkin Lymphoma: This type of lymphoma can sometimes affect sex hormone production in both men and women, leading to:
- Men: Decreased testosterone levels, potentially resulting in decreased libido, erectile dysfunction, and muscle weakness.
- Women: Disruption of menstrual cycles, irregular periods, or even premature menopause.
- Estrogen-Receptor Positive Lymphomas: Certain types of lymphoma, particularly in women, can be estrogen-receptor positive. This means they can be fueled by the hormone estrogen, similar to some breast cancers.
Hormonal Imbalance as a Symptom
Hormonal imbalances can sometimes manifest as symptoms in individuals with lymphoma. These might include:
- Fatigue: A common symptom in both lymphoma and hormonal imbalances.
- Weight changes: Unexplained weight gain or loss can occur due to both conditions.
- Sleep disturbances: Night sweats, a potential symptom of lymphoma, can also be linked to hormonal fluctuations.
- Changes in mood and behavior: Hormonal imbalances can contribute to anxiety, depression, and other mood changes, which can be seen in both lymphoma patients and individuals with hormonal disorders.
Frequently Asked Questions (FAQs)
Is lymphoma a serious cancer?
Whether lymphoma is considered a “serious” cancer depends on several factors, particularly the specific type and stage of the disease. Here’s a breakdown to help you understand:
Lymphoma is a cancer, so inherently carries inherent risks and needs medical attention. However, it’s not a monolithic entity and encompasses diverse categories with varying levels of severity.
Generally
- Hodgkin lymphoma: Often considered less aggressive than NHL, with better survival rates. Early-stage Hodgkin’s typically has 5-year survival rates exceeding 80%, while even advanced stages have over 50% survival with proper treatment.
- Non-Hodgkin lymphoma (NHL): Prognosis varies greatly based on the specific subtype, stage, and other factors. Some types like DLBCL (aggressive) have 5-year survival rates around 70% for early stages, while others like follicular lymphoma (slower-growing) have 10-year survival rates exceeding 90% for early stages.
Therefore, “seriousness” depends on
- Type of lymphoma: Hodgkin lymphoma generally has better outcomes than aggressive NHL subtypes.
- Stage of the disease: Early stages have better prognoses than advanced stages.
- Individual factors: Age, overall health, response to treatment, and access to quality healthcare significantly impact outcomes.
While not all lymphomas are immediately life-threatening, it’s crucial to remember:
- Early diagnosis and treatment are vital for optimal outcomes in all cases.
- Lymphoma can be serious and requires medical expertise and intervention.
- Individual cases can vary significantly, and consultation with a healthcare professional for an accurate assessment based on your specific situation is critical.
Where does lymphoma usually start?
While lymphoma can potentially start anywhere in the body where there are lymphocytes (infection-fighting white blood cells), it most commonly arises in the lymphatic system. This network includes:
- Lymph nodes: Bean-shaped structures present throughout the body, including the neck, armpits, groin, chest, abdomen, and pelvis. These filter lymph fluid, trapping and eliminating harmful substances.
- Spleen: Located under the left ribs, the spleen filters blood and stores immune cells.
- Thymus: Situated behind the breastbone, the thymus matures T-cells, another type of white blood cell.
- Bone marrow: Found inside bones, the bone marrow produces various blood cells, including lymphocytes.
Specifically
- Hodgkin lymphoma: Often originates in the upper body lymph nodes like the neck or chest.
- Non-Hodgkin lymphoma (NHL): Can start in any lymph node but frequently involves those in the neck, chest, abdomen, or groin. Some rare NHL subtypes might primarily affect the skin, gastrointestinal tract, or other organs.
Is lymphoma painful?
Generally, lymphoma itself isn’t inherently painful. However, it can cause pain indirectly in a few ways:
- Swollen lymph nodes pressing on nerves: When enlarged lymph nodes push against nearby nerves, it can cause pain radiating to the affected area. This is more common in specific locations like the groin, chest, or abdomen.
- Bone involvement: If lymphoma spreads to the bones, it can cause bone pain, tenderness, and potential fractures.
- Other factors: In some cases, the specific type or stage of lymphoma might contribute to discomfort or pain due to other associated symptoms like fever or fatigue.
Here’s a breakdown of pain in different lymphoma types:
- Hodgkin lymphoma: Pain is less common, but some individuals might experience discomfort due to swollen nodes or other factors.
- Non-Hodgkin lymphoma (NHL): Pain can be more variable depending on the specific subtype and its location. Certain aggressive NHLs like Burkitt lymphoma might show more frequent pain due to rapid progression.
What are the signs of end stage lymphoma?
While the specific signs of end-stage lymphoma can vary depending on the individual and type of lymphoma, some common symptoms to watch out for include:
General
- Worsening of existing symptoms: Fatigue, night sweats, fever, and weight loss become more pronounced and persistent.
- Loss of appetite and difficulty eating: This can lead to further weight loss and weakness.
- Extreme fatigue and inability to perform daily activities: Even simple tasks become challenging.
- Confusion and changes in mental state: These can occur due to tumor progression or medication side effects.
- Increased pain and discomfort: This could be due to tumor growth pressing on nerves or organs.
- Difficulty breathing: If lymphoma affects the lungs or mediastinum, breathing problems can arise.
- Frequent infections: A weakened immune system makes individuals more susceptible to infections.
- Organ failure: In advanced stages, lymphoma can affect essential organs, leading to their failure.
Additional signs depending on the affected organs
- Abdominal pain or swelling: If lymphoma involves abdominal organs like the liver or spleen.
- Bone pain and fractures: If it spreads to the bones.
- Skin involvement: In rare cases, lymphoma can manifest as skin tumors or lesions.
What is natural killer lymphoma?
Natural killer (NK) lymphoma is a rare and aggressive type of non-Hodgkin lymphoma (NHL) that arises from natural killer (NK) cells, a type of lymphocyte involved in the immune system’s defense against viruses and tumors.
General Features
- Rarity: Accounts for less than 2% of all T-cell lymphomas and under 1% of all NHL cases.
- Aggressiveness: Characterized by rapid growth and spread, requiring prompt diagnosis and treatment.
- Association with Epstein-Barr virus (EBV): EBV infection is linked to the development of most NK lymphomas.
Subtypes
- Extranodal NK/T-cell lymphoma, nasal type (ENKL): Most common subtype, primarily affecting the nose, sinuses, and upper respiratory tract.
- Nodal NK/T-cell lymphoma (NNKL): Less common subtype, originating in lymph nodes throughout the body.
- Aggressive NK-cell leukemia (ANKL): Rare subtype involving the blood and bone marrow.
Symptoms
- Can vary depending on the subtype and affected location.
- Common symptoms for ENKL include nasal blockage, nosebleeds, facial swelling, and pain.
- NNKL might present with enlarged lymph nodes, fever, night sweats, and weight loss.
- ANKL symptoms resemble those of acute leukemia, including fatigue, bruising, and infections.
Diagnosis
- Requires a combination of tests, including biopsy of affected tissue, blood tests, and imaging studies like CT scans or PET scans.
- Immunophenotyping to identify specific markers on the lymphoma cells helps confirm the diagnosis.
Treatment
- Depends on the subtype, stage, and patient’s overall health.
- Often involves intensive chemotherapy regimens, sometimes combined with radiation therapy.
- Immunotherapy and stem cell transplantation might be considered in specific cases.
Prognosis
- Variable depending on various factors, with ENKL generally having a better prognosis than NNKL and ANKL.
- Early diagnosis and treatment are crucial for better outcomes.
Are lymphoma lumps movable?
Yes, lymphoma lumps are typically movable under the skin, which is one of the ways they can be distinguished from other types of lumps. Here’s a breakdown of the characteristics of lymphoma lumps:
- Movable: They tend to move slightly when pressed gently with your fingers. This is because they are not firmly attached to underlying tissues.
- Smooth and round: They usually have a smooth and round shape.
- Usually painless: While not always the case, lymphoma lumps are generally painless or cause minimal discomfort when touched.
- Often appear in the neck, armpit, or groin: These are common areas where lymph nodes are located, and swollen lymph nodes are a frequent symptom of lymphoma.
However, it’s important to remember that:
- These are just general characteristics, and there can be variations. Some lymphoma lumps might be firm or slightly adherent to surrounding tissues.
- Not all movable lumps are lymphoma. Other conditions can also cause movable lumps.
Why does lymphoma cause itching?
While the exact reason behind itching in lymphoma isn’t fully understood, there are two main theories:
1. Cytokine release
- The immune system releases various chemicals called cytokines to fight infections and inflammation.
- In lymphoma, some types of abnormal lymphocytes (white blood cells) may release excessive amounts of specific cytokines that can irritate nerve endings in the skin, leading to itching.
- This theory aligns with the observation that itching is more common in Hodgkin lymphoma, which tends to involve more pronounced lymphocyte activation compared to other lymphoma types.
2. Disruption of the skin barrier
- Lymphoma can affect the skin’s natural balance and barrier function in several ways:
- Direct infiltration: Lymphoma cells can directly infiltrate the skin, disrupting its structure and function.
- Indirect effects: The disease process or some treatments can damage the skin, making it drier and more susceptible to irritation and itching.
- This theory might explain why itching can sometimes occur in areas not directly affected by lymphoma cells.
Additional factors
- Individual sensitivity: Some individuals might be more susceptible to itching than others, regardless of the underlying cause.
- Psychological factors: Stress and anxiety, which can be common experiences when dealing with cancer, can sometimes worsen itching sensations.
Remember
- Itching can be a symptom of various conditions, not just lymphoma.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. WHO Classification of Tumours, Revised 4th Edition, Volume 2. 2017.
- Eichenauer DA, Aleman BMP, André M, Federico M, Hutchings M, Illidge T, Engert A, Ladetto M; ESMO Guidelines Committee. Hodgkin lymphoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2018 Oct 1;29(Suppl 4):iv19-iv29. doi: 10.1093/annonc/mdy080. PMID: 29796651.
- Adler EM. Living with Lymphoma: A Patient’s Guide (Johns Hopkins Press Health Books (Paperback)). 2016.
- Leukemia & Lymphoma Society (LLS)
- Che Y, Ding X, Xu L, Zhao J, Zhang X, Li N, Sun X. Advances in the treatment of Hodgkin’s lymphoma (Review). Int J Oncol. 2023 May;62(5):61. doi: 10.3892/ijo.2023.5509. Epub 2023 Apr 7. PMID: 37026506; PMCID: PMC10147096.
- Katsin M, Dormeshkin D, Meleshko A, Migas A, Dubovik S, Konoplya N. CAR-T Cell Therapy for Classical Hodgkin Lymphoma. Hemasphere. 2023 Nov 16;7(12):e971. doi: 10.1097/HS9.0000000000000971. PMID: 38026793; PMCID: PMC10656097.
- Denlinger N, Bond D, Jaglowski S. CAR T-cell therapy for B-cell lymphoma. Curr Probl Cancer. 2022 Feb;46(1):100826. doi: 10.1016/j.currproblcancer.2021.100826. Epub 2021 Dec 25. PMID: 35012754; PMCID: PMC9284423.
- Sehn LH, Herrera AF, Flowers CR, Kamdar MK, McMillan A, Hertzberg M, Assouline S, Kim TM, Kim WS, Ozcan M, Hirata J, Penuel E, Paulson JN, Cheng J, Ku G, Matasar MJ. Polatuzumab Vedotin in Relapsed or Refractory Diffuse Large B-Cell Lymphoma. J Clin Oncol. 2020 Jan 10;38(2):155-165. doi: 10.1200/JCO.19.00172. Epub 2019 Nov 6. PMID: 31693429; PMCID: PMC7032881.
- Minson A, Tam C, Dickinson M, Seymour JF. Targeted Agents in the Treatment of Indolent B-Cell Non-Hodgkin Lymphomas. Cancers (Basel). 2022 Mar 1;14(5):1276. doi: 10.3390/cancers14051276. PMID: 35267584; PMCID: PMC8908980.



