TL;DR
Iron deficiency anemia or IDA is caused by defective heme or hemoglobin synthesis due to the lack of iron.
Iron deficiency symptoms & signs ▾:
| General | Specific |
| Fatigue Weakness Pallor Headaches Dizziness or lightheadedness Shortness of breath Chest pain Palpitations Irritability Cold hands and feet Poor appetite in children and infants | Koilonychia Angular cheilosis Pica Sore tongues and papillary atrophy Paterson-Brown-Kelly or Plummer-Vinson syndrome |
- Age: Infants, children, elderly
- Dietary: Vegetarians without adequate iron intakes
- Drug History: Aspirin, NSAIDs
- Gastrointestinal Tract: Bleeding, gastric or bowel surgery
- Physiological: Pregnancy, frequent blood donors, breastfeeding
- Renal: Hematuria
- Reproduction: Menorrhagia
- Sex: Women especially women in childbearing age
- Dietary: Vegetarians, milk-fed infants, elderly
- Gastrointestinal Bleeding: Esophagitis, peptic ulcer, inflammatory bowel disease, malignancy of stomach and colorectal, renal / bladder tumors, hemorrhoids, NSAIDs etc
- Gastrointestinal Malabsorption: Atrophic gastritis, Helicobacter pylori gastritis, celiac disease, partial gastrectomy
- Physiological: Growth spurts (prematurity, adolescents), pregnancy, lactation
- Reproduction: Menorrhagia, postmenopausal bleeding
- Social: Hookworm infections (most common), poverty
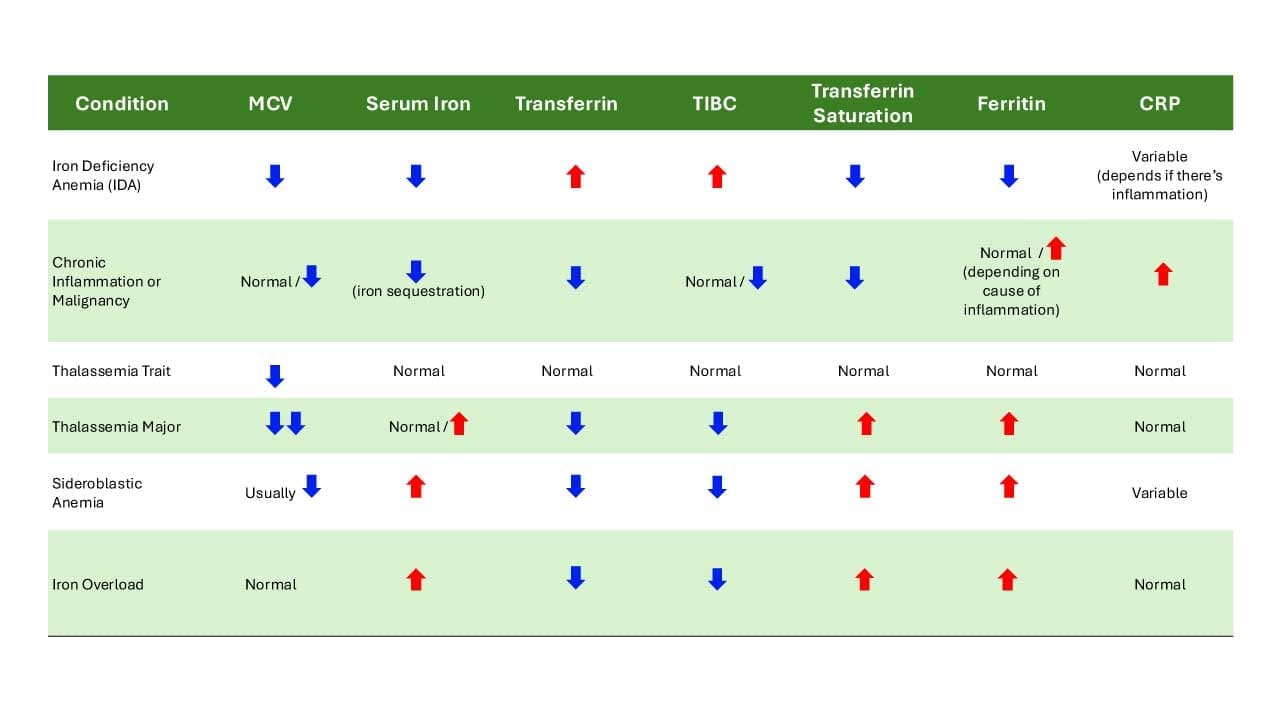
- Complete blood count: ↓ hemoglobin, ↓ mean cell volume and ↓ mean cell hemoglobin. Reticulocytes can be normal or increased depending on the severity of the anemia. White blood cell and platelet counts are generally within the normal range.
- Peripheral blood smear: Hypochromic, microcytic red cells, anisopoikilocytosis with numerous pencil-shaped cells.
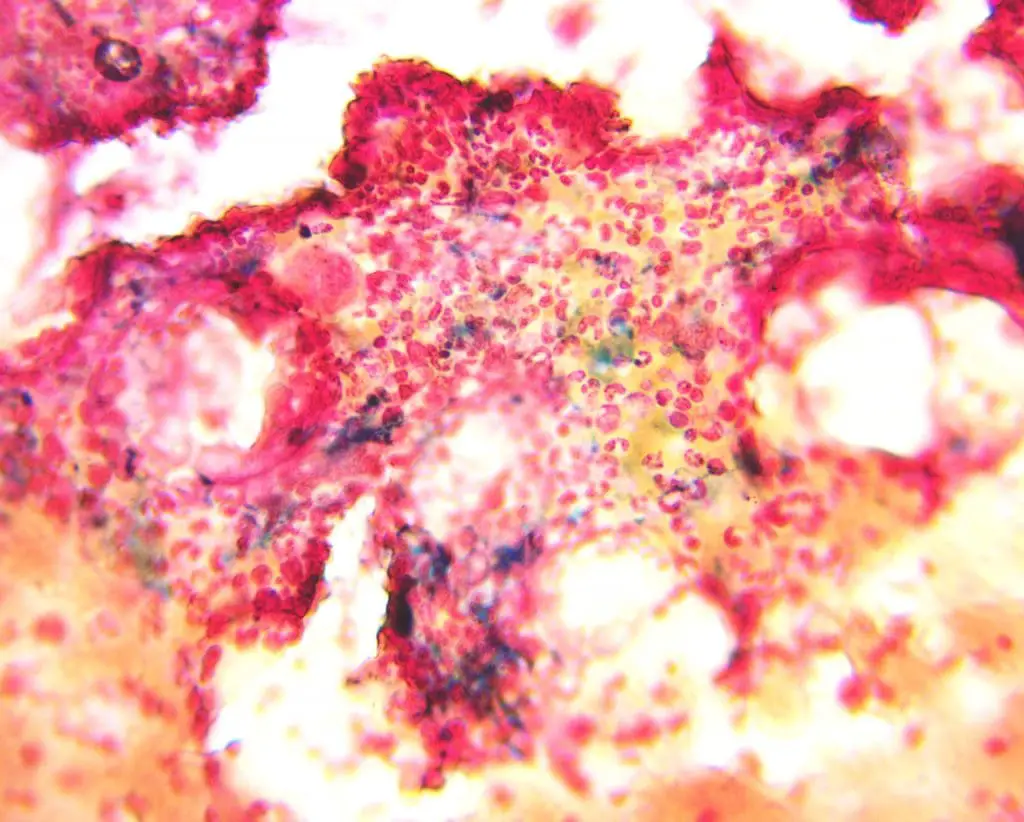
- Bone marrow smear: Perls’ Prussian blue stain will be negative if iron stores are absent.
- ↓ serum ferritin level (Reference range is 15 – 300 µg/dL).
- ↓ serum iron and transferrin saturation, and ↑ total iron binding capacity (TIBC).
- ↑ soluble transferrin receptor.
Iron deficiency treatment and management ▾:
- Treat the underlying cause and replenish the iron stores.
- Dietary and lifestyle changes.
- Iron therapy through oral ferrous iron salts and parenteral iron for those unable to absorb the oral iron.
- Transfusion of packed RBCs for those with significant acute bleeding or in danger of hypoxia or coronary insufficiency.
*Click ▾ for more information
What is iron deficiency anemia (IDA)?
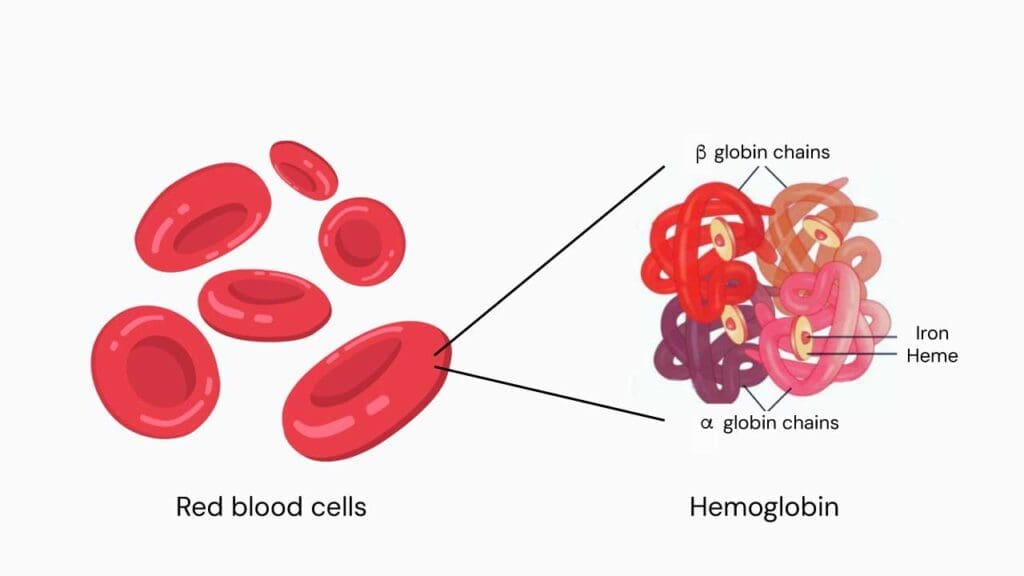
Iron deficiency anemia (IDA) is a type of hypochromic microcytic anemia, a red blood cell disorder, caused by defective heme or hemoglobin synthesis due to the lack of iron in our body.
Hemoglobin, the oxygen-carrying protein in red blood cells, is the primary molecule affected by iron deficiency. Iron is an essential component of heme, the non-protein portion of hemoglobin that binds oxygen. When iron levels are insufficient, heme synthesis is disrupted, leading to reduced hemoglobin production.
The decrease in hemoglobin production results in smaller and less hemoglobinized red blood cells, known as microcytic hypochromic erythrocytes. These cells have a diminished capacity to carry oxygen, leading to tissue hypoxia, a state of inadequate oxygen supply to body tissues.
Anemia is a public health problem that affects almost two billion people globally. Anemia is defined as when a person’s hemoglobin level falls below the reference range or a reduction in the hemoglobin concentration of the blood according to gender and age. Iron deficiency anemia (IDA) contributes to approximately 50% of the cause; the most common nutritional disorder in the world.
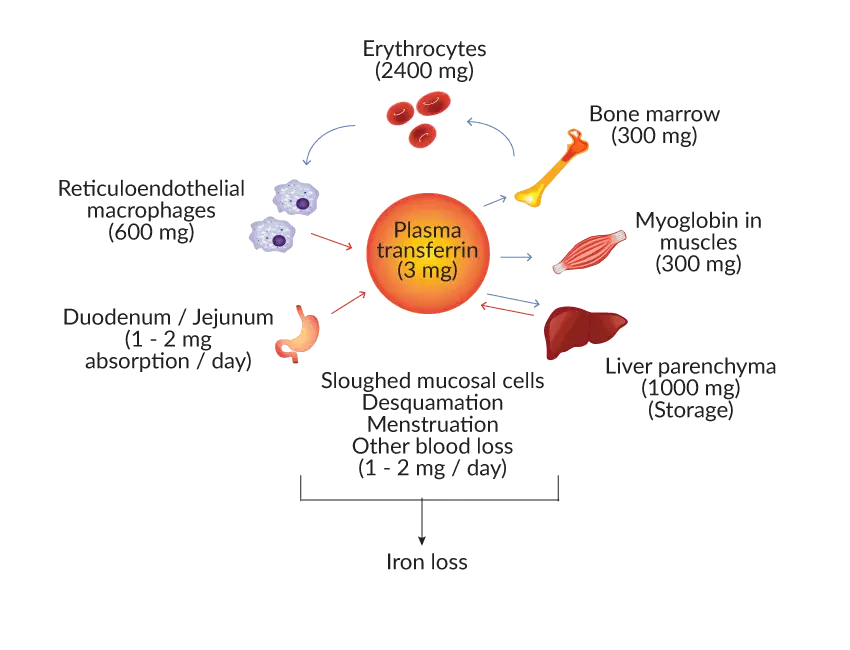
How is iron regulated in our body?
Iron, a vital micronutrient, plays a pivotal role in various physiological processes, including oxygen transport, energy production, and DNA synthesis. Maintaining iron homeostasis, the balance between iron absorption, utilization, and storage, is essential for optimal health. This intricate process involves a complex interplay of specialized proteins, regulatory mechanisms, and target tissues.
Iron Absorption
Organic dietary iron is partly absorbed as heme and partly broken down in the gut to inorganic iron. Absorption occurs through the duodenum. Inorganic iron absorption is favored by factors such as acid and reducing agents like ferrireductase that keep iron in the gut lumen and in the Fe2+ rather than the Fe3+ state.
The protein DMT-1 is involved in transfers of iron from the lumen of the gut across the enterocyte microvilli. The amount of iron absorbed is partly regulated according to the body’s needs by changing the levels of DMT-1 according to the iron status of the duodenal villous crypt enterocyte. Heme is absorbed through a specific receptor HCP-1, exposed on the apical membrane of the duodenal enterocyte. Heme is then digested to release iron.
Iron Transport
Ferroportin at the basolateral surface controls the exit of iron from the cell into portal plasma. Hepcidin is also a major regulator by affecting ferroportin concentration. Low hepcidin levels in iron deficiency increase ferroportin levels and allow more iron to enter portal plasma. Another enzyme, hephaestin, converts Fe2+ to Fe3+ at the basal surface prior to binding to transferrin.
Iron Utilization
From our daily meal, the duodenum absorbs about 1 – 2 mg of dietary iron. It will then be carried by transferrin to be distributed into various compartments, mainly as functional iron, in which the iron is used to synthesize hemoglobin in the bone marrow. Additionally, iron is essential for various enzymatic processes, including DNA synthesis, energy production, and cellular respiration.
At the end of their life, red cells are broken down in the macrophages of the reticuloendothelial system (RES) and the iron is released from the hemoglobin, enters the plasma and is transported around the body in transferrins. Iron is also present in the muscle as myoglobin and in most cells of the body in iron-containing enzymes.
Iron Storage
Excess iron, not immediately required for utilization, is stored in specialized proteins, ferritin and hemosiderin. Ferritin, the primary iron storage protein, is found in the liver, spleen, and bone marrow, and it reversibly binds iron for long-term storage. Hemosiderin, an insoluble form of iron storage, is derived from ferritin degradation and is primarily found in macrophages.
Iron Loss
Apart from the iron cycle, approximately 1-2 mg iron is lost through sloughed mucosal cells, desquamation, menstruation and other causes of blood loss. Iron homeostasis is well-regulated to protect cells from iron-mediated oxidative stress. Unfortunately, there is no physiological pathway for iron excretion from the human body. Therefore, to avoid detrimental effects, iron homeostasis involves the interaction of different types of iron-binding proteins like iron storage protein, iron transport proteins and function proteins, so that iron is stored and transported in a safe state.
Iron Cycle
Clinical Manifestations of Iron Deficiency Anemia (IDA)
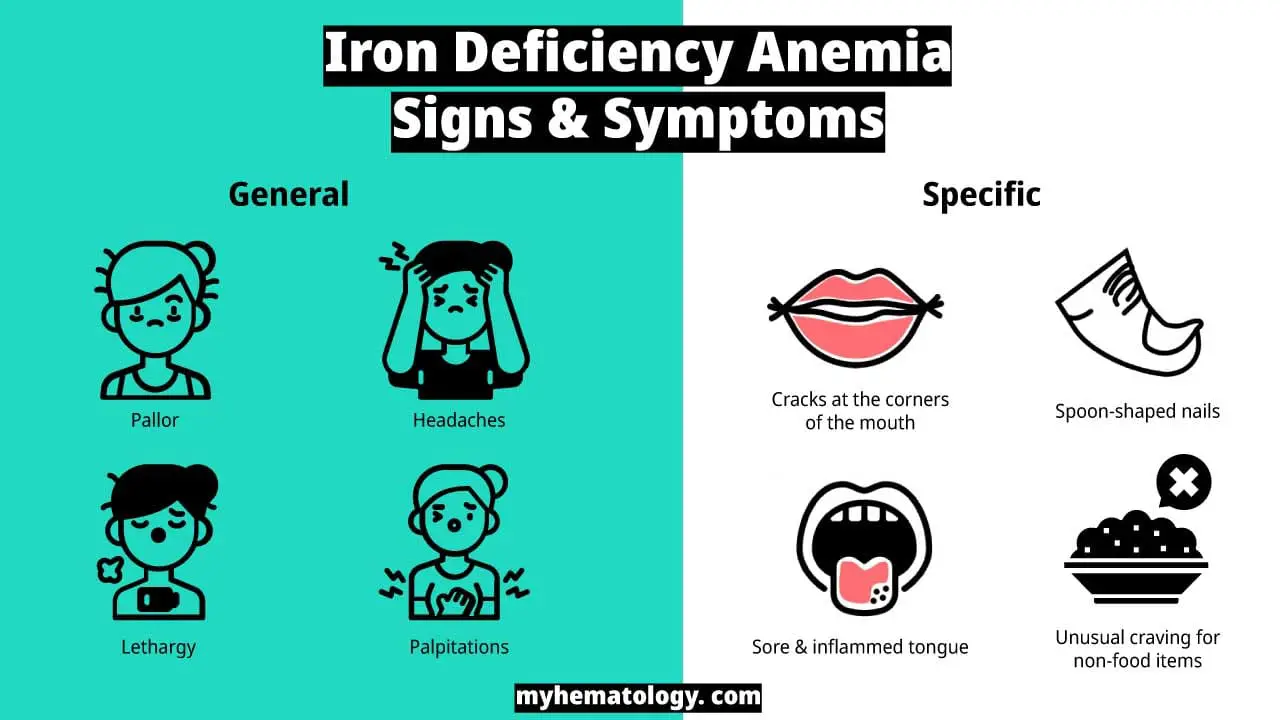
The clinical manifestations of iron deficiency anemia (IDA) can vary widely depending on the severity and duration of the deficiency. The symptoms often develop gradually and may go unnoticed in the early stages.
Common Signs and Symptoms of Iron Deficiency Anemia (IDA)
- Fatigue and weakness: This is the most common symptom, as the body’s tissues are not receiving enough oxygen to function properly.
- Pale skin: The lack of hemoglobin, which gives blood its red color, can lead to a noticeable paleness, especially in the face, eyelids, and nail beds.
- Shortness of breath: With a reduced oxygen-carrying capacity, the body may struggle to get enough oxygen, leading to breathlessness, particularly during physical exertion.
- Dizziness or lightheadedness: Inadequate oxygen supply to the brain can cause these sensations.
- Headaches: Oxygen deprivation can also trigger headaches.
- Increased heart rate (tachycardia) or heart palpitations: The heart may pump faster to compensate for the lack of oxygen in the blood.
Specific Signs and Symptoms of Iron Deficiency Anemia (IDA)
In more severe or prolonged cases, additional, more specific signs and symptoms can develop:
- Tinnitus: A ringing, buzzing, or hissing sound in the ears.
- Brittle nails or koilonychia: The nails may become thin, brittle, and even take on a spoon-like, concave shape.
- Sore or swollen tongue (glossitis): The tongue may become inflamed, smooth, and pale.
- Cracks at the corners of the mouth (cheilosis): Painful sores or cracks can appear at the corners of the lips.
- Pica: An unusual craving to eat non-food substances such as ice, dirt, or paper. This is a classic, though uncommon, sign of iron deficiency.
- Restless legs syndrome (RLS): An uncontrollable urge to move the legs, often accompanied by uncomfortable sensations, which can be more severe at night.
- Hair loss: A noticeable increase in hair shedding can occur.
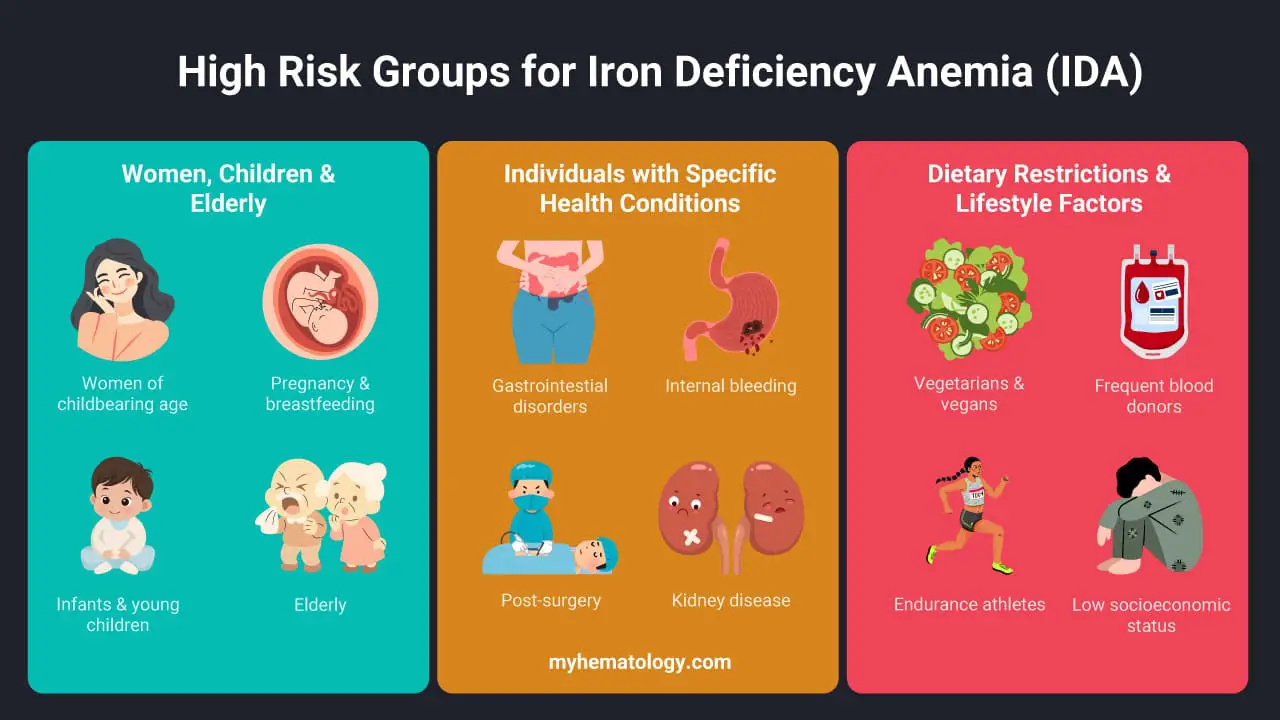
Am I at risk of iron deficiency anemia (IDA)?
High-risk groups for iron deficiency anemia (IDA) are typically those with increased iron needs, chronic blood loss, or impaired iron absorption. Here are the key groups most vulnerable:
Women and Children 👩👧
- Women of childbearing age: Due to regular blood loss from menstruation, women are at a significantly higher risk for iron deficiency anemia (IDA) than men. Heavy menstrual bleeding is a major risk factor.
- Pregnant and breastfeeding women: A pregnant person’s iron needs nearly double to support their increased blood volume and provide iron for the growing fetus. This demand can quickly deplete iron stores, leading to iron deficiency anemia (IDA). Iron is also passed to the infant during breastfeeding.
- Infants and young children: This group has high iron requirements for rapid growth and development. Premature or low-birth-weight babies are especially at risk because they don’t have as much iron stored at birth. Toddlers who consume large amounts of cow’s milk may also develop iron deficiency anemia (IDA), as milk is low in iron and can interfere with its absorption.
Elderly
Anemia is a common condition in older adults, and while not all cases are due to iron deficiency, iron deficiency anemia (IDA) is a significant and frequent cause.
The risk factors in the elderly are often multi-faceted and different from those in younger adults. They include:
- Chronic Blood Loss: This is the most common cause of iron deficiency anemia (IDA) in older adults. It is frequently due to slow, often occult (hidden), gastrointestinal bleeding from conditions like ulcers, polyps, or, in some cases, colorectal cancer. The regular use of certain medications, such as aspirin and other NSAIDs, can also contribute to this.
- Nutritional Deficiencies: A poor or restricted diet is a common issue among the elderly due to a variety of reasons, including reduced appetite, difficulty with chewing or swallowing, or financial limitations. This can lead to an inadequate intake of iron-rich foods.
- Malabsorption Issues: Older adults are more likely to have conditions that impair iron absorption, such as celiac disease or H. pylori infection. Additionally, the use of certain medications, particularly proton pump inhibitors (PPIs) for acid reflux, can reduce stomach acid, which is necessary for iron absorption.
- Anemia of Chronic Disease (ACD): This is a separate type of anemia that is also very common in the elderly, often co-existing with iron deficiency anemia (IDA). Chronic inflammatory conditions (like rheumatoid arthritis), chronic kidney disease, or cancer can lead to the body’s inability to properly use stored iron, even if iron levels are technically sufficient. This can make diagnosis more complex, as inflammation can elevate ferritin levels, masking a true iron deficiency.
- Comorbidities: The elderly population often has multiple health conditions and takes various medications, many of which can contribute to the development of anemia.
Individuals with Specific Health Conditions 🤒
- People with gastrointestinal disorders: Conditions like celiac disease, inflammatory bowel diseases (Crohn’s disease, ulcerative colitis), and H. pylori infections can impair the small intestine’s ability to absorb iron.
- People with internal bleeding: Slow, chronic blood loss from conditions like peptic ulcers, colon polyps, or colorectal cancer can lead to iron deficiency anemia (IDA). Regular use of certain medications, such as aspirin and NSAIDs, can also cause gastrointestinal bleeding.
- Post-surgical patients: Individuals who have undergone major surgery, particularly gastric bypass or other bariatric procedures, may have reduced iron absorption due to changes in their digestive tract.
- Individuals with kidney disease: People on dialysis often lose blood during treatment, and their kidneys may not produce enough erythropoietin, a hormone needed to make red blood cells.
People with Dietary Restrictions and Lifestyle Factors 🥗
- Vegetarians and vegans: Iron from plant-based sources (non-heme iron) is not absorbed as efficiently by the body as iron from animal sources (heme iron). Therefore, those following these diets must carefully manage their intake of iron-rich plant foods and consider iron-fortified products.
- Frequent blood donors: Regular blood donation can deplete the body’s iron stores, as each donation removes red blood cells and the iron they contain.
- Endurance athletes: Intense physical training can lead to iron loss through sweat and a process called “march hemolysis,” where red blood cells are broken down due to the impact of rigorous exercise.
- People with low socioeconomic status: Food insecurity and limited access to a varied, nutrient-rich diet can contribute to chronic malnutrition and iron deficiency.
What are the stages of iron deficiency?
Iron deficiency anemia (IDA) develops progressively, with distinct stages characterized by varying levels of iron depletion and impact on red blood cell production.
Stage 1: Iron Depletion
- Iron stores: Depleted bone marrow iron stores (ferritin < 15 ng/mL)
- Red blood cells: Normal red blood cell production and indices (hemoglobin, MCV, MCH)
- Iron deficiency anemia (IDA) symptoms: Often asymptomatic, but fatigue may be present.
- Diagnostic tests: Low ferritin, normal transferrin saturation (TSAT), and increased transferrin receptor (TfR).
Stage 2: Iron-Deficient Erythropoiesis
- Iron stores: Further depletion of bone marrow iron stores, but still detectable.
- Red blood cells: Normal red blood cell count, but decreased hemoglobin production (microcytic carrier state). Hemoglobin may remain within normal range initially.
- Iron deficiency anemia (IDA) symptoms: Fatigue, pallor, and exertional dyspnea become more prominent.
- Diagnostic tests: Low ferritin, decreased TSAT (< 20%), and elevated TfR. Bone marrow aspirate may show microcytic precursors.
Stage 3: Iron Deficiency Anemia
- Iron stores: Severely depleted bone marrow iron stores (ferritin often < 10 ng/mL).
- Red blood cells: Decreased red blood cell count (anemia), microcytosis (MCV < 80 fL), and hypochromia (MCH < 27 pg).
- Iron deficiency anemia (IDA) symptoms: Severe fatigue, weakness, pallor, dyspnea at rest, cognitive impairment, and pica.
- Diagnostic tests: Confirmed anemia with microcytosis and hypochromia, low ferritin, decreased TSAT, and elevated TfR. Bone marrow aspirate confirms iron deficiency.
Laboratory Investigations for Iron Deficiency Anemia (IDA)
Diagnosing iron deficiency anemia (IDA) relies on a combination of clinical symptoms and specific laboratory investigations that assess red blood cell characteristics and the body’s iron stores. The most common and important tests include a complete blood count (CBC) and iron studies.
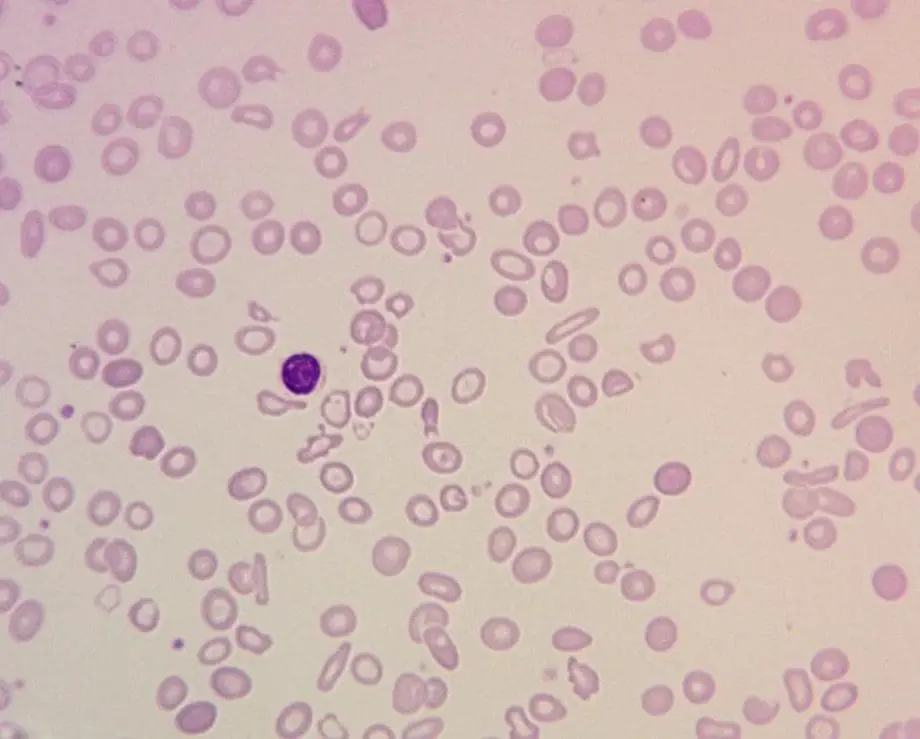
Complete Blood Count (CBC)
A CBC is a standard blood test that provides a detailed overview of the different cells in the blood, including red blood cells, white blood cells, and platelets. In iron deficiency anemia (IDA), a CBC typically reveals:
- Low Hemoglobin (Hb) and Hematocrit (Hct): These are the primary indicators of anemia. Hemoglobin is the protein in red blood cells that carries oxygen, and hematocrit is the percentage of red blood cells in the blood volume. Both will be below the normal reference range.
- Low Mean Corpuscular Volume (MCV): MCV measures the average size of red blood cells. In IDA, red blood cells are smaller than normal, a condition known as microcytic anemia. A low MCV is a key finding.
- Low Mean Corpuscular Hemoglobin (MCH) and Mean Corpuscular Hemoglobin Concentration (MCHC): These values measure the average amount and concentration of hemoglobin in red blood cells, respectively. Due to the lack of iron, the cells are pale, a condition known as hypochromic anemia, which is reflected in low MCH and MCHC values.
- High Red Cell Distribution Width (RDW): RDW measures the variation in the size of red blood cells. In IDA, the body produces red blood cells of various sizes (small and normal), leading to a higher-than-normal RDW. This is often one of the earliest signs of developing IDA.
Iron Studies
While the CBC points to the presence of anemia, iron studies are crucial to confirm that the anemia is due to iron deficiency. These tests measure the iron levels in the blood and the body’s iron stores.
- Transferrin Saturation (TSAT): TSAT is a calculation that shows the percentage of transferrin that is actually bound to iron. It is calculated as (Serum Iron ÷ TIBC) × 100. In IDA, with low serum iron and high TIBC, the TSAT is consequently low, typically less than 20%.
- Serum Ferritin: This is the most sensitive and specific test for diagnosing IDA and reflects the body’s total iron stores. A low serum ferritin level is the most reliable indicator of iron deficiency. However, because ferritin is an “acute phase reactant,” its levels can be falsely elevated in the presence of inflammation, infection, or liver disease, potentially masking an underlying deficiency.
- Serum Iron: This test measures the amount of iron circulating in the blood. In IDA, serum iron levels are typically low. However, this can fluctuate throughout the day and is not a reliable standalone marker.
- Total Iron-Binding Capacity (TIBC): TIBC measures the amount of transferrin available to carry iron in the blood. When iron levels are low, the body produces more transferrin in an attempt to absorb as much iron as possible. Therefore, TIBC is characteristically high in IDA.
Bone Marrow Biopsy
In certain complex or ambiguous cases, a bone marrow biopsy and subsequent staining with Perls’ Prussian blue stain is considered the “gold standard” for diagnosing iron deficiency anemia (IDA), such as in cases where a patient has both iron deficiency and a co-existing inflammatory condition (like chronic disease or infection), which can elevate serum ferritin and mask the underlying iron deficiency. While less common today due to the reliability of blood tests, this procedure provides a direct and definitive assessment of the body’s iron stores.
The key purpose of this stain in iron deficiency anemia (IDA) is to visually confirm the absence of iron stores.
- Normal Bone Marrow: In a healthy individual, the bone marrow contains visible, blue-staining iron deposits (hemosiderin) within macrophages and in the bone marrow particles. The pathologist can grade the amount of stainable iron present.
- Iron deficiency Anemia (IDA) Bone Marrow: In a patient with iron deficiency anemia (IDA), the bone marrow will show a complete absence of stainable iron. The macrophages will appear empty, and no blue deposits will be seen in the marrow particles. This finding confirms a state of absolute iron deficiency.
Iron Deficiency Anemia (IDA) Treatment & Management
The treatment and management of iron deficiency anemia (IDA) focus on three key pillars:
- Identifying and addressing the underlying cause of the deficiency
- Replenishing the body’s iron stores
- Monitoring the patient’s response to therapy.
Treating the Underlying Cause
This is the most critical and often overlooked step. Simply giving iron supplements without addressing the root cause will only provide a temporary solution, and the anemia will likely recur.
- For women with heavy menstrual bleeding: Treatments may include hormonal therapies like oral contraceptives to regulate and lighten periods, or in some cases, surgical options.
- For gastrointestinal blood loss: This is a common cause in men and postmenopausal women. The source of bleeding must be found and treated. This often involves an endoscopy (for the upper GI tract) or a colonoscopy (for the lower GI tract) to check for conditions like ulcers, polyps, inflammatory bowel disease, or in rare cases, cancer.
- For malabsorption issues: In conditions like celiac disease, strict adherence to a gluten-free diet is essential for the intestinal lining to heal and properly absorb iron.
Iron Repletion
Once the cause is addressed, iron levels must be restored. There are two primary methods for this:
Oral Iron Supplementation
This is the first-line treatment for most patients with iron deficiency anemia (IDA). It is a simple, cost-effective, and effective way to replenish iron stores.
- Dosage and Formulation: The goal is to provide a high dose of elemental iron daily. Common formulations include ferrous sulfate, ferrous gluconate, and ferrous fumarate. Ferrous sulfate is the most widely used.
- Administration: To enhance absorption, it is often recommended to take iron supplements on an empty stomach with a source of vitamin C, such as a glass of orange juice. However, because iron can cause significant gastrointestinal side effects (e.g., nausea, constipation, stomach cramps), many patients may need to take it with food. Taking the supplement every other day may also improve absorption and reduce side effects.
- Duration: It is a long-term treatment. A patient’s hemoglobin level may begin to improve within a few weeks, but the full course of treatment can last for several months to a year or more to fully replenish the body’s iron stores (indicated by a normal ferritin level).
Intravenous (IV) Iron Therapy
This method delivers iron directly into the bloodstream and is reserved for specific situations.
- Indications: IV iron is used for iron deficiency anemia (IDA) patients who cannot tolerate oral iron due to severe side effects, have conditions that impair iron absorption (e.g., inflammatory bowel disease, celiac disease, gastric bypass surgery), or require rapid iron repletion (e.g., in late pregnancy, before major surgery, or in severe, symptomatic anemia).
- Benefits: IV iron is highly effective, can replenish iron stores much faster than oral supplements, and bypasses the gastrointestinal tract, eliminating side effects like nausea and constipation.
- Formulations: Newer formulations are safer and can be given in a single, large dose, making it a convenient option.
Monitoring and Follow-Up
Regular monitoring is crucial to ensure the treatment is working.
- Initial Follow-up: A patient’s hemoglobin and reticulocyte count (which measures new red blood cell production) are typically checked within a few weeks of starting treatment to confirm a positive response.
- Ongoing Monitoring: Once the hemoglobin level has normalized, treatment should continue for several more months to build up sufficient iron stores. A serum ferritin level is the best way to monitor this, with a goal of returning to a healthy range.
- Non-response to Therapy: If a patient’s hemoglobin and iron levels do not improve after a month or two of oral iron, a healthcare provider will investigate the reason, which may include poor patient adherence, undiagnosed malabsorption, or an underlying source of chronic bleeding. This may lead to switching the patient to IV iron or pursuing further diagnostic tests.
Blood Transfusion: In rare cases of very severe, symptomatic iron deficiency anemia (IDA) or when a patient is hemodynamically unstable (e.g., with a dangerously low hemoglobin level and signs of heart failure), a blood transfusion may be necessary to rapidly restore red blood cell volume and oxygen-carrying capacity. However, this is a short-term solution and does not correct the underlying iron deficiency.
What food is highest in iron?
The food sources with the highest iron content per serving are primarily animal-based, particularly organ meats and shellfish, because they contain heme iron, which is much more easily absorbed by the body than non-heme iron from plant sources.
Heme Iron Sources (Highest Bioavailability)
- Organ Meats: Liver (especially beef liver) is exceptionally high in iron.
- Shellfish: Clams, oysters, and mussels are some of the richest sources of iron, often with a high concentration per gram.
- Red Meat: Beef, lamb, and other red meats are excellent sources of heme iron.
- Poultry: The iron content is higher in the darker meat of chicken and turkey.
- Fish: Sardines and tuna are good sources of iron.
Non-Heme Iron Sources (Lower Bioavailability)
While non-heme iron is not as efficiently absorbed, these foods can still contribute significantly to the daily iron intake, especially when consumed with foods high in vitamin C, which enhances absorption.
- Fortified Cereals: Many breakfast cereals and grain products are heavily fortified with iron, making them one of the most common sources of iron in the average diet.
- Beans and Legumes: Lentils, soybeans, chickpeas, and other beans are a good source of non-heme iron.
- Nuts and Seeds: Pumpkin seeds and sesame seeds (tahini) are particularly rich in iron.
- Dark Leafy Greens: Spinach, Swiss chard, and kale contain iron, though their absorption can be hindered by compounds like oxalates.
- Tofu and Soy Products: Tofu and tempeh are good plant-based sources of iron.
- Dried Fruits: Dried apricots and raisins contain a notable amount of iron.
The amount of iron needed each day depends on factors like age, gender, and dietary habits. It’s recommended that people following a vegetarian or vegan diet consume about 1.8 times the iron of those who eat meat, due to the lower absorption rate of non-heme iron.
Iron-Rich Drinks
- Iron-fortified orange juice: Vitamin C in orange juice helps with iron absorption from plant-based sources.
- Prune juice: This naturally sweet juice is a good source of iron and other nutrients, but limit your intake due to its sugar content.
Foods to Avoid or Limit
While no foods directly interfere with iron absorption, some can hinder it if consumed in large quantities. These include:
- Coffee and tea: These beverages contain tannins, which can bind to iron and reduce its absorption. Space out your coffee or tea intake from iron-rich meals by at least an hour.
- Calcium-rich foods: Dairy products, calcium-fortified foods, and antacids can interfere with iron absorption if consumed close together. Avoid taking iron supplements with milk or calcium-rich foods.
- Whole-grain wheat products: While whole grains are nutritious, the phytates they contain can slightly reduce iron absorption. Soak or sprout grains before consuming to improve their digestibility and nutrient bioavailability.
Frequently Asked Questions (FAQs)
What is the main cause of iron deficiency anemia (IDA)?
The main cause of iron deficiency anemia (IDA) depends on several factors, including age, gender, and underlying health conditions. However, there are two main categories:
Blood loss
This is the most common cause of iron deficiency anemia (IDA) in adults and men. It can occur through various mechanisms.
- Gastrointestinal bleeding: This can be caused by ulcers, hemorrhoids, cancer, or chronic inflammation, such as Crohn’s disease.
- Heavy menstrual bleeding: Women with heavy periods are at increased risk of iron deficiency anemia (IDA).
- Blood donation: Frequent blood donation can deplete iron stores, especially if not replenished properly.
Inadequate iron intake or absorption
This is more common in infants, children, and pregnant women.
- Diet low in iron-rich foods: Meat, poultry, fish, beans, and leafy green vegetables are excellent sources of iron. Limited access to these foods can contribute to iron deficiency anemia (IDA).
- Malabsorption: Certain medical conditions, such as celiac disease or Crohn’s disease, can interfere with iron absorption from the gut.
- Increased iron requirements: During pregnancy, the body needs more iron to support fetal development. Infants and young children are also rapidly growing and require adequate iron intake.
Therefore, the main cause of iron deficiency anemia (IDA) can vary depending on individual circumstances.
What are the 4 common IDA symptoms?
While iron deficiency anemia (IDA) can present with a variety of symptoms, here are 4 common iron defiency anemia symptoms:
1. Fatigue and weakness: This is often the most noticeable iron deficiency anemia (IDA) symptom, and it can range from mild tiredness to feeling constantly exhausted. It occurs because the body’s tissues aren’t receiving enough oxygen due to the reduced number of healthy red blood cells.
2. Pale skin: Due to the lack of hemoglobin, which gives red blood cells their color and carries oxygen, the skin can appear pale or lackluster in iron deficiency. This may be most noticeable in the face, lips, and under the nails.
3. Shortness of breath: With fewer red blood cells transporting oxygen, the body has to work harder to deliver oxygen to the body’s tissues. This can lead to shortness of breath, especially during physical activity as a common iron deficiency symptom.
4. Dizziness or lightheadedness: As the body struggles to supply sufficient oxygen to the brain, a person may experience dizziness or lightheadedness, particularly when standing up quickly or changing positions in iron deficiency amemia (IDA).
How long does it take to correct iron deficiency anemia?
The time it takes to correct iron deficiency anemia (IDA) depends on several factors, including:
Severity of the deficiency: More severe iron deficiency anemia (IDA) cases with depleted iron stores will take longer to correct than mild cases.
Treatment method: Oral iron supplements usually take longer than intravenous (IV) iron to replenish stores.
Individual absorption and response: Different people absorb iron differently, and some may respond faster to treatment than others.
Underlying cause: If the underlying cause of the iron deficiency anemia (IDA) like blood loss, isn’t addressed, it can hinder iron stores from replenishing fully.
Here’s a general timeframe:
- Oral iron supplements: It can take 3-6 months to see significant improvement in red blood cell counts and iron deficiency anemia symptoms with oral iron supplements. However, iron stores may take longer to fully replenish, up to 12 months or more.
- IV iron: IV iron infusions can correct severe iron deficiency anemia symptoms much faster, sometimes within weeks. This is because it bypasses the gut and delivers iron directly into the bloodstream.
Factors that can slow down progress
- Skipping iron supplements or missing doses in iron deficiency anemia treatment.
- Having underlying conditions that affect iron absorption, like celiac disease or Crohn’s disease.
- Continuing to lose blood (e.g., heavy menstrual bleeding, ulcers).
- Taking medications that interfere with iron absorption, like antacids or calcium supplements.
When is the best time to take iron for anemia?
In general, most guidelines recommend taking iron supplements on an empty stomach, as food can reduce absorption. However, if you experience side effects, it’s okay to take them with food. Avoid taking iron supplements with calcium-rich foods like milk, yogurt, or antacids, as these can also interfere with absorption. Take iron supplements with a glass of water and avoid coffee or tea, which can further reduce absorption.
Are there test kits available to test for iron deficiency at home?
Yes, there are at-home iron test kits available. These kits typically measure ferritin, a protein that stores iron in your body.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Warner MJ, Kamran MT. Iron Deficiency Anemia. [Updated 2023 Aug 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448065/
- Safiri, S., Kolahi, AA., Noori, M. et al. Burden of anemia and its underlying causes in 204 countries and territories, 1990–2019: results from the Global Burden of Disease Study 2019. J Hematol Oncol 14, 185 (2021). https://doi.org/10.1186/s13045-021-01202-2.
- Goldberg S, Hoffman J. Clinical Hematology Made Ridiculously Simple, 1st Edition: An Incredibly Easy Way to Learn for Medical, Nursing, PA Students, and General Practitioners (MedMaster Medical Books). 2021.
- Garrison C. The Iron Disorders Institute Guide to Anemia: Understanding the Causes, Symptoms, and Healing of Iron Deficiency and Other Anemias (Cumberland House). 2009.
- Johansson A. Iron Deficiency Anemia Cookbook: Essential Diet Guide, 50 + Iron Rich Recipes and a 2-Week Diet Plan to Help Low Iron Levels. 2021.
- Cappellini, M. D., Musallam, K. M., & Taher, A. T. (2020). Iron deficiency anaemia revisited. Journal of internal medicine, 287(2), 153–170. https://doi.org/10.1111/joim.13004
- Lewkowitz, A. K., & Tuuli, M. G. (2023). Identifying and treating iron deficiency anemia in pregnancy. Hematology. American Society of Hematology. Education Program, 2023(1), 223–228. https://doi.org/10.1182/hematology.2023000474
- Elstrott, B., Khan, L., Olson, S., Raghunathan, V., DeLoughery, T., & Shatzel, J. J. (2020). The role of iron repletion in adult iron deficiency anemia and other diseases. European journal of haematology, 104(3), 153–161. https://doi.org/10.1111/ejh.13345
- DeLoughery, T. G., Jackson, C. S., Ko, C. W., & Rockey, D. C. (2024). AGA Clinical Practice Update on Management of Iron Deficiency Anemia: Expert Review. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association, 22(8), 1575–1583. https://doi.org/10.1016/j.cgh.2024.03.046
- Cappellini, M. D., Santini, V., Braxs, C., & Shander, A. (2022). Iron metabolism and iron deficiency anemia in women. Fertility and sterility, 118(4), 607–614. https://doi.org/10.1016/j.fertnstert.2022.08.014
- Leung, A. K. C., Lam, J. M., Wong, A. H. C., Hon, K. L., & Li, X. (2024). Iron Deficiency Anemia: An Updated Review. Current pediatric reviews, 20(3), 339–356. https://doi.org/10.2174/1573396320666230727102042