TL;DR
Heparin-induced thrombocytopenia is an immune-mediated reaction to heparin that causes thrombocytopenia and an increased risk of thrombosis.
- Type I: Non-immune, transient, mild thrombocytopenia.
- Type II: Immune-mediated, potentially serious, associated with thrombosis. (This is the clinically significant form.)
Pathogenesis ▾: Heparin binds to PF4, forming complexes. Antibodies (IgG) develop against these complexes. These antibodies then bind to platelet receptors, activating platelets. Platelet activation leads to consumption (thrombocytopenia) and thrombosis.
- Thrombocytopenia (usually 5-10 days after heparin exposure).
- Thrombosis (venous and arterial, including unusual sites).
- Skin necrosis at injection sites.
- Acute systemic reactions (fever, chills, flushing, chest pain).
- Platelet count monitoring.
- Anti-PF4-heparin antibody assays (ELISA, functional assays like SRA).
- Immediate cessation of all heparin.
- Alternative anticoagulation (DTIs: argatroban, bivalirudin; fondaparinux).
- Management of thrombosis (anticoagulation, thrombolysis if needed).
- Avoidance of platelet transfusions (generally).
- Long-term anticoagulation may be required.
- Lifelong avoidance of heparin.
*Click ▾ for more information
Introduction
Heparin-induced thrombocytopenia (HIT) is a serious complication of heparin therapy. It is an immune-mediated reaction that causes the body to attack its own platelets, leading to a decrease in platelet count (thrombocytopenia) and an increased risk of blood clots (thrombosis).
Heparin
Heparin is a medication that helps to prevent blood clots. It is a type of anticoagulant, also known as a blood thinner. Heparin acts as a catalyst by binding to antithrombin III. This binding induces a conformational change in antithrombin III, significantly enhancing its ability to inhibit several key proteins in the coagulation cascade. Primarily, the enhanced antithrombin III complex targets and neutralizes thrombin and factor Xa, two crucial enzymes that drive the formation of blood clots. By effectively inactivating these clotting factors, heparin indirectly prevents the conversion of fibrinogen to fibrin, a critical step in clot formation, thereby hindering the coagulation process. Essentially, heparin amplifies the natural anticoagulant action of antithrombin III, preventing excessive clot formation.
Types of Heparin-Induced Thrombocytopenia
Heparin-Induced Thrombocytopenia Type I
Heparin-induced thrombocytopenia type I is a non-immune-mediated reaction that occurs within the first few days of heparin therapy. It is usually mild and self-limiting, and the platelet count typically returns to normal despite continued heparin use. Heparin-induced thrombocytopenia type I is not associated with an increased risk of thrombosis.
Heparin-Induced Thrombocytopenia Type II
Heparin-induced thrombocytopenia type II is an immune-mediated reaction that typically occurs 5-10 days after the start of heparin therapy, although it can occur earlier in patients with prior exposure to heparin. It is caused by the formation of antibodies against heparin-platelet factor 4 (PF4) complexes. These antibodies activate platelets, leading to platelet consumption and thrombocytopenia. Heparin-induced thrombocytopenia type II is a potentially serious condition that can lead to life-threatening complications such as thrombosis.
The rest of this article will focus on HIT Type II, as it is the more clinically significant form of heparin-induced thrombocytopenia. .
Pathogenesis of Heparin Induced Thrombocytopenia (Type II)
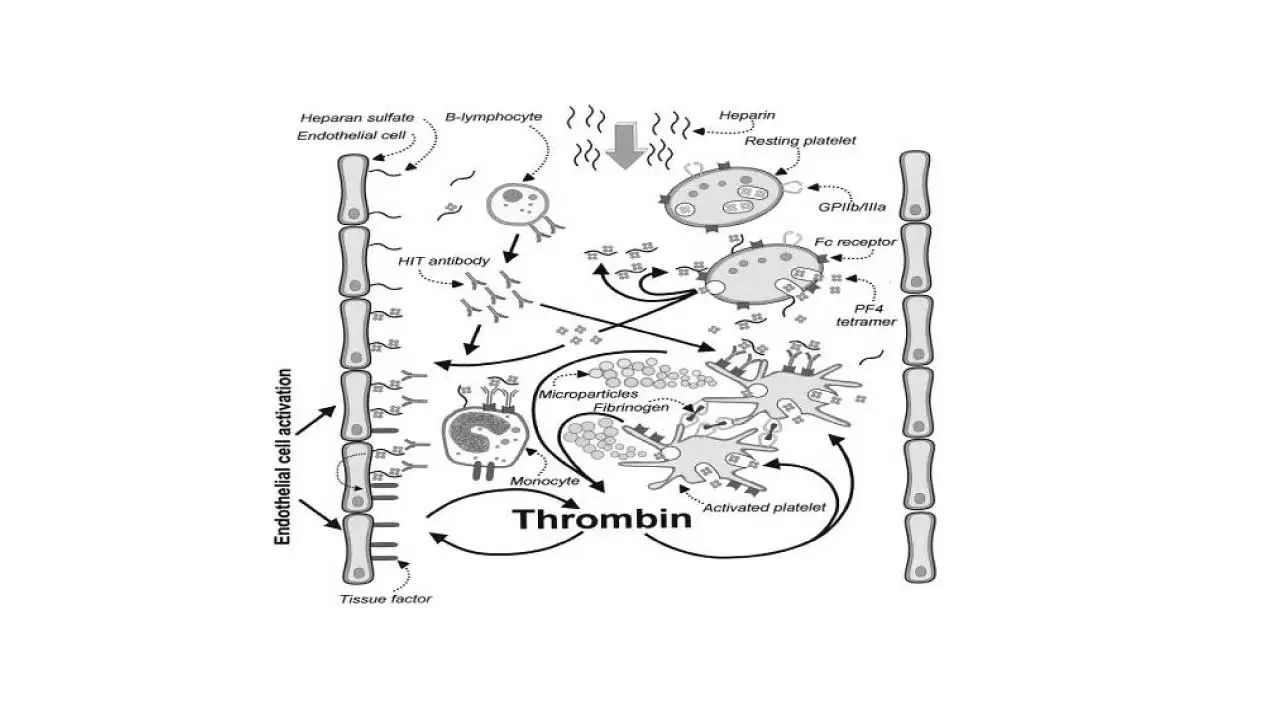
In heparin-induced thrombocytopenia (HIT), the pathogenesis involves a series of steps that lead to platelet activation and thrombosis. When heparin is administered, it binds to platelet factor 4 (PF4), a protein released from platelets. This binding creates PF4-heparin complexes. In some individuals, the PF4-heparin complexes trigger an immune response, leading to the production of IgG antibodies against these complexes. These anti-PF4-heparin antibodies bind to the FcγRIIa receptors on the surface of platelets. The binding of antibodies to platelet receptors causes platelet activation, leading to platelet aggregation and consumption. This results in a decrease in platelet count, known as thrombocytopenia. The activated platelets release procoagulant factors, which promote the formation of blood clots (thrombosis). This can lead to serious complications such as deep vein thrombosis, pulmonary embolism, and stroke.
In addition to platelet activation, endothelial damage may also play a role in promoting thrombosis in heparin-induced thrombocytopenia (HIT). The exact mechanisms by which endothelial damage contributes to HIT-associated thrombosis are not fully understood, but it is thought that it may involve the release of tissue factor and other procoagulant factors from damaged endothelial cells.
Signs and Symptoms of Heparin-Induced Thrombocytopenia (HIT)
Thrombocytopenia
The typical timing of platelet drop in heparin-induced thrombocytopenia is usually 5-10 days after heparin exposure. However, it is important to note that the degree of thrombocytopenia does not always correlate with the severity of thrombosis. In some cases, patients with heparin-induced thrombocytopenia may have a significant drop in platelet count but no signs or symptoms of thrombosis. In other cases, patients may have a relatively small drop in platelet count but develop serious thrombotic complications.
The reasons for this discrepancy are not fully understood, but it is thought that it may be related to the individual patient’s immune response to heparin. Some patients may produce more antibodies against heparin-platelet factor 4 (PF4) complexes than others. These antibodies can activate platelets, leading to platelet consumption and thrombocytopenia. However, they can also activate the coagulation cascade, leading to thrombosis.
The severity of heparin-induced thrombocytopenia can also be affected by other factors, such as the patient’s age, medical history, and other medications they are taking. It is important to note that even if a patient with heparin-induced thrombocytopenia does not have a significant drop in platelet count, they are still at risk for thrombosis. Therefore, it is important to monitor all patients receiving heparin for signs and symptoms of heparin-induced thrombocytopenia, even if their platelet count remains within the normal range. If heparin-induced thrombocytopenia is suspected, heparin should be discontinued immediately and an alternative anticoagulant should be started.
Thrombosis
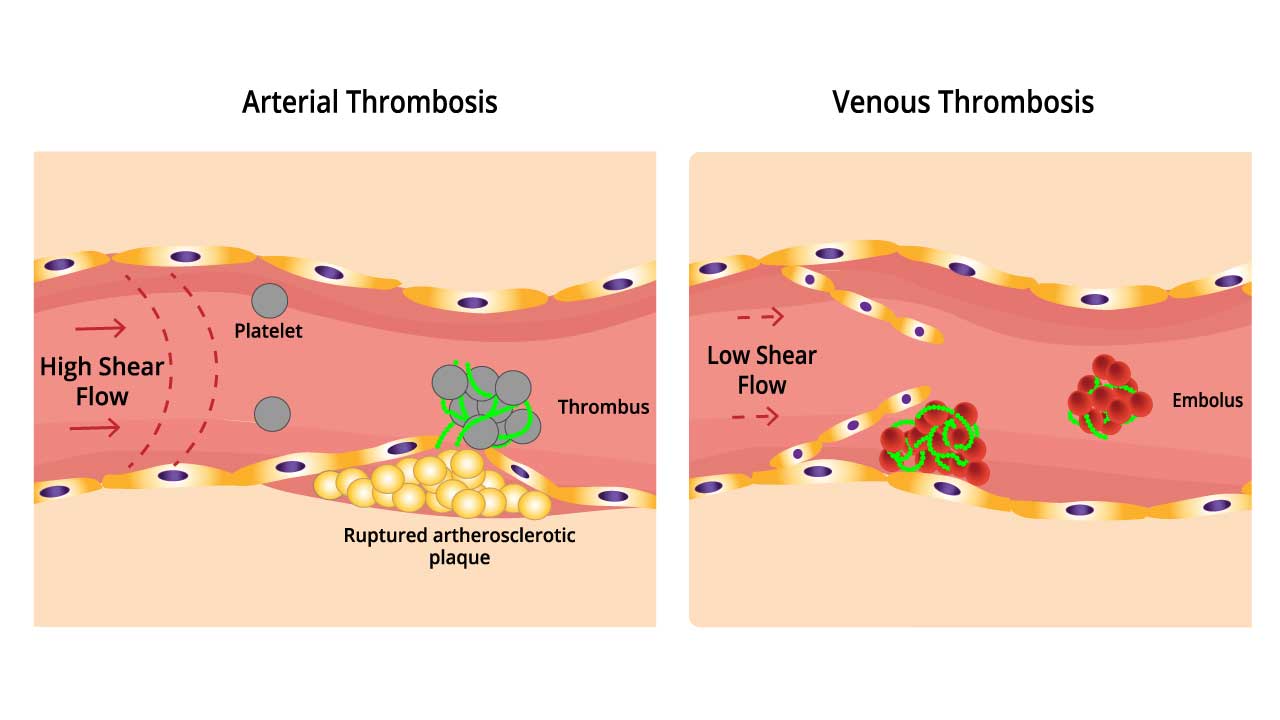
It is important to note that heparin-induced thrombocytopenia is primarily a thrombotic disorder, not a bleeding disorder, despite the low platelet count. In fact, the most common complication of heparin-induced thrombocytopenia is thrombosis, which can occur in both the veins and arteries.
Venous thrombosis is more common than arterial thrombosis in heparin-induced thrombocytopenia. The most common sites of venous thrombosis in heparin-induced thrombocytopenia are the deep veins of the legs (DVT) and the lungs (PE). However, venous thrombosis can also occur in other unusual sites, such as the mesenteric veins (mesenteric venous thrombosis) and the cerebral sinuses (cerebral venous sinus thrombosis).
Arterial thrombosis in heparin-induced thrombocytopenia can lead to serious complications such as limb ischemia, stroke, and myocardial infarction (heart attack). Limb ischemia occurs when blood flow to a limb is reduced, which can lead to pain, numbness, and even amputation. Stroke occurs when blood flow to the brain is interrupted, which can lead to permanent brain damage. Myocardial infarction occurs when blood flow to the heart is interrupted, which can lead to chest pain, shortness of breath, and even death.
heparin-induced thrombocytopenia is a serious condition that can lead to life-threatening complications. It is important to be aware of the signs and symptoms of heparin-induced thrombocytopenia so that it can be diagnosed and treated promptly.
Other Manifestations
While the most common manifestation of heparin-induced thrombocytopenia is thrombosis, there are other less common but still important manifestations that can occur.
Skin necrosis at heparin injection sites: This is a rare but serious complication of heparin-induced thrombocytopenia that can occur when heparin is injected subcutaneously. It is thought to be caused by the formation of thrombi in the small blood vessels of the skin. Skin necrosis typically presents as a painful, red or purple lesion at the injection site. In severe cases, it can lead to ulceration and gangrene.
Acute systemic reactions: These reactions can occur after an intravenous heparin bolus and are thought to be caused by the release of inflammatory mediators from activated platelets. Symptoms of acute systemic reactions can include fever, chills, flushing, chest pain, and shortness of breath. In rare cases, these reactions can be life-threatening.
4Ts Scoring System for Heparin-Induced Thrombocytopenia (HIT) Probability
The 4Ts scoring system is a clinical tool used to assess the likelihood of heparin-induced thrombocytopenia (HIT). It is a pretest probability assessment that helps clinicians determine whether further testing for heparin-induced thrombocytopenia (HIT) is necessary.
The 4Ts scoring system takes into account four clinical features of heparin-induced thrombocytopenia.
- Thrombocytopenia: The magnitude of the decrease in platelet count.
- Timing: The timing of the decrease in platelet count in relation to heparin exposure.
- Thrombosis: The presence of thrombosis or other complications of heparin-induced thrombocytopenia (HIT).
- Other causes: The likelihood of other causes for thrombocytopenia.
Each of these features is assigned a score of 0, 1, or 2, and the total score is used to categorize the patient’s probability of heparin-induced thrombocytopenia (HIT) as low, intermediate, or high.
The 4Ts scoring system is a valuable tool for clinicians because it can help them to
- Identify patients who are at high risk for heparin-induced thrombocytopenia (HIT) and require further testing.
- Avoid unnecessary testing in patients who are at low risk for heparin-induced thrombocytopenia (HIT).
- Make informed decisions about the management of patients with suspected heparin-induced thrombocytopenia (HIT).
| Feature | Score 0 | Score 1 | Score 2 |
| Thrombocytopenia | Platelet count < 10 x 109/L or fall <30% | Platelet count 10 -19 x 109/L or 30 – 50% fall | Platelet count ≥ 20 x 109/L or > 50% fall |
| Timing | Platelet fall ≤ day 4, no prior heparin | Consistent with days 5–10 fall, but not clear (e.g. missing platelet counts) orPlatelet fall after day 10, or ≤1 day if prior heparin < 30 -100 days ago | Platelet fall day 5-10, or ≤1 day if prior heparin < 30 days ago |
| Thrombosis | No thrombosis present | Thrombosis suspected or proven (new or progressive) | Proven thrombosis (new) or skin necrosis or post-heparin bolus acute systemic reaction |
| Other Causes | Other cause for thrombocytopenia definite | Other cause possible | No other cause apparent |
Interpretation
- Total Score 0-3: Low probability of heparin-induced thrombocytopenia (HIT)
- Total Score 4-5: Intermediate probability of heparin-induced thrombocytopenia (HIT)
- Total Score 6-8: High probability of heparin-induced thrombocytopenia (HIT)
It is important to note that the 4Ts scoring system is not a perfect tool. It is possible for patients with a low 4Ts score to have heparin-induced thrombocytopenia (HIT), and it is also possible for patients with a high 4Ts score to not have heparin-induced thrombocytopenia (HIT). However, the 4Ts scoring system is a useful tool that can help clinicians to assess the likelihood of heparin-induced thrombocytopenia (HIT) and make informed decisions about patient care.
Laboratory Investigations for Heparin-Induced Thrombocytopenia
Platelet Count Monitoring
Regular monitoring of platelet counts is essential in patients receiving heparin. A significant drop in platelet count, especially within the 5-10 day window after heparin initiation (or earlier with prior exposure), raises suspicion for heparin-induced thrombocytopenia (HIT).
Anti-PF4-Heparin Antibody Assays
- ELISA (Enzyme-Linked Immunosorbent Assay): This is a widely used screening test due to its high sensitivity. It detects antibodies (usually IgG) against PF4-heparin complexes. However, it’s important to note that ELISA has limitations in specificity, meaning a positive result doesn’t always confirm heparin-induced thrombocytopenia (HIT).
- Functional Assays (e.g., Serotonin Release Assay – SRA): These assays measure the ability of patient serum to activate platelets in the presence of heparin. They have higher specificity than ELISA and are considered the gold standard for heparin-induced thrombocytopenia (HIT) diagnosis. However, they are more complex, expensive, and may not be readily available in all labs.
Other Tests
Other tests like platelet aggregation studies or flow cytometry may be used in some cases, but their role in routine heparin-induced thrombocytopenia (HIT) diagnosis is limited.
Treatment and Management of Heparin-Induced Thrombocytopenia (HIT)
The treatment and management of heparin-induced thrombocytopenia (HIT) involves a multi-faceted approach, focusing on immediate cessation of heparin, alternative anticoagulation, and management of any thrombotic complications.
Immediate Cessation of Heparin
The first and most crucial step is to immediately discontinue all forms of heparin, including unfractionated heparin (UFH), low molecular weight heparin (LMWH), and even heparin flushes. Lifelong avoidance of heparin is essential to prevent recurrence of heparin-induced thrombocytopenia (HIT).
Alternative Anticoagulation
- Direct Thrombin Inhibitors (DTIs): These are the preferred anticoagulants in heparin-induced thrombocytopenia (HIT). Options include:
- Argatroban: Often preferred in patients with renal impairment.
- Bivalirudin: May be preferred in patients undergoing cardiac surgery.
- Fondaparinux: A synthetic pentasaccharide that inhibits factor Xa. It can be used as an alternative anticoagulant in some heparin-induced thrombocytopenia (HIT) cases.
- Other Options: In certain situations, other anticoagulants like danaparoid or direct oral anticoagulants (DOACs) may be considered, but their use in acute heparin-induced thrombocytopenia (HIT) might be less established.
Management of Thrombosis
- Treatment of Existing Thrombosis: If thrombosis is present (e.g., DVT, PE), it should be treated with appropriate anticoagulation therapy, often with a DTI initially.
- Thrombolysis: In severe cases of thrombosis, thrombolytic therapy (clot-busting medication) may be considered.
Other Considerations
- Avoidance of Platelet Transfusions: Generally, platelet transfusions are contraindicated in heparin-induced thrombocytopenia (HIT) as they can exacerbate thrombosis. However, in cases of severe bleeding, they might be considered cautiously.
- Warfarin: Warfarin should not be used as initial therapy in heparin-induced thrombocytopenia (HIT). It can be started later, once the platelet count has recovered and the patient is on a stable alternative anticoagulant.
- Monitoring: Regular monitoring of platelet counts is crucial until they recover.
- Long-Term Anticoagulation: After the acute phase, continued anticoagulation for several weeks or months is usually recommended to prevent further thrombotic events.
Risks of Future Heparin Exposure
- HIT recurrence: The most significant risk is the recurrence of heparin-induced thrombocytopenia (HIT), even with small amounts of heparin. This can lead to thrombocytopenia and thrombosis, with potentially life-threatening consequences.
- Rapid-onset HIT: In some patients, re-exposure to heparin can trigger a rapid and severe immune response (anamnestic response), leading to heparin-induced thrombocytopenia (HIT) within hours instead of the typical 5-10 days. This can be particularly dangerous due to the swiftness of the reaction.
Precautions for Patients with a History of HIT
- Strict avoidance of heparin: The cornerstone of management is lifelong avoidance of all forms of heparin, including UFH, LMWH, and even heparin flushes.
- Inform healthcare providers: Patients should inform all healthcare providers about their history of HIT to ensure heparin is not inadvertently administered. This includes doctors, nurses, dentists, and pharmacists.
- Medical alert bracelet or card: Wearing a medical alert bracelet or carrying a card indicating HIT can help prevent accidental heparin exposure in emergency situations.
- Alternative anticoagulants: If anticoagulation is necessary, alternative anticoagulants should be used instead of heparin. These include direct thrombin inhibitors (DTIs) like argatroban or bivalirudin, and fondaparinux.
- Careful consideration for cardiac surgery: In rare cases where heparin is absolutely necessary (e.g., during cardiac surgery), careful consideration and specialized protocols are required. This might involve using alternative anticoagulants during the procedure or, in specific situations, cautiously reintroducing heparin with close monitoring and specialized assays.
Differential Diagnosis
When considering a diagnosis of heparin-induced thrombocytopenia (HIT), it’s important to differentiate it from other conditions that can present with similar clinical features.
Other Causes of Thrombocytopenia
- Immune Thrombocytopenia (ITP): An autoimmune disorder causing platelet destruction. Differentiating factors include the absence of heparin exposure and often the presence of bleeding manifestations.
- Thrombotic Thrombocytopenic Purpura (TTP): A rare disorder with microangiopathic hemolytic anemia, thrombocytopenia, and neurological symptoms.
- Disseminated Intravascular Coagulation (DIC): Often associated with severe illness (sepsis, trauma), characterized by both thrombosis and bleeding due to consumption of clotting factors.
- Drug-Induced Thrombocytopenia: Various medications can cause thrombocytopenia. A careful medication history is crucial.
- Other Conditions: Infections, splenomegaly, and certain medical conditions can also lead to low platelet counts.
Other Causes of Thrombosis
- Deep Vein Thrombosis (DVT) or Pulmonary Embolism (PE) from other causes: These can occur due to various risk factors (surgery, immobility, cancer). Heparin-induced thrombocytopenia (HIT) is specifically linked to heparin exposure.
- Arterial Thrombosis: Conditions like atherosclerosis can cause arterial thrombosis, but HIT-related thrombosis often occurs in unusual locations or with a temporal relationship to heparin.
Prognosis and Complications
Heparin-induced thrombocytopenia (HIT) is a serious condition that can lead to several complications, primarily due to the increased risk of thrombosis.
Thrombosis
- Venous Thrombosis: Deep vein thrombosis (DVT) in the legs is a common complication, which can lead to pulmonary embolism (PE) if the clot travels to the lungs. Other less common sites include mesenteric veins (mesenteric venous thrombosis) and cerebral sinuses (cerebral venous sinus thrombosis).
- Arterial Thrombosis: This can lead to serious events like limb ischemia (reduced blood flow to a limb), stroke, or myocardial infarction (heart attack).
Limb Amputation
- Severe Ischemia: In cases of severe arterial thrombosis, reduced blood flow to a limb can lead to tissue damage and potentially require amputation.
Death
Both venous and arterial thrombosis can be life-threatening. PE can cause respiratory distress and death, while stroke or myocardial infarction can have fatal consequences.
Long-term prognosis for patients with HIT
The long-term prognosis for patients with heparin-induced thrombocytopenia (HIT) can vary depending on the severity of the condition and whether they develop thrombotic complications. With prompt recognition and treatment, many patients recover well from heparin-induced thrombocytopenia (HIT). Platelet counts usually return to normal, and the risk of further thrombosis decreases. However, there is a risk of recurrence if the patient is ever exposed to heparin again. Some patients may require long-term anticoagulation to prevent future thrombotic events, especially if they have had significant thrombosis related to heparin-induced thrombocytopenia (HIT).
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Lo GK, Juhl D, Warkentin TE, Sigouin CS, Eichler P, Greinacher A. Evaluation of pretest clinical score (4 T’s) for the diagnosis of heparin-induced thrombocytopenia in two clinical settings. J Thromb Haemost. 2006 Apr;4(4):759-65. doi: 10.1111/j.1538-7836.2006.01787.x. PMID: 16634744.
- Arachchillage DJ, Thachil J, Anderson JAM, Baker P, Poles A, Kitchen S, Laffan M; BSH Committee. Diagnosis and management of heparin-induced thrombocytopenia: Third edition. Br J Haematol. 2024 Feb;204(2):459-475. doi: 10.1111/bjh.19180. Epub 2023 Dec 28. PMID: 38153164.
- Hvas AM, Favaloro EJ, Hellfritzsch M. Heparin-induced thrombocytopenia: pathophysiology, diagnosis and treatment. Expert Rev Hematol. 2021 Apr;14(4):335-346. doi: 10.1080/17474086.2021.1905512. Epub 2021 Mar 30. PMID: 33736552.
- Dees DC. Heparin Induced Thrombocytopenia Testing. Clin Lab Med. 2024 Sep;44(3):541-550. doi: 10.1016/j.cll.2024.04.013. Epub 2024 May 30. PMID: 39089757.
- Arepally GM, Cines DB. Pathogenesis of heparin-induced thrombocytopenia. Transl Res. 2020 Nov;225:131-140. doi: 10.1016/j.trsl.2020.04.014. Epub 2020 May 15. PMID: 32417430; PMCID: PMC7487042.



