TL;DR
Burkitt lymphoma (BL) is a highly aggressive (fast-growing) type of B-cell non-Hodgkin lymphoma.
- c-myc translocation: A hallmark genetic abnormality involving the c-myc oncogene, leading to uncontrolled cell growth. Other genetic abnormalities like mutations in ID3, TCF3, TP53 and complex karyotype can also contribute. TP53 mutations and complex karyotype are associated with poorer prognosis.
- EBV: The Epstein-Barr virus (EBV) is associated with BL, particularly in endemic (African) forms.
- Other factors: Malaria is a key environmental cofactor in endemic BL, impairing immune response and increasing B cell proliferation. Immunosuppression (e.g., HIV/AIDS) increases BL risk and can lead to atypical presentations.
- General symptoms: Fever, night sweats, weight loss (“B symptoms”).
- Endemic BL: Typically presents with jaw/facial bone tumors in children.
- Sporadic BL: Often presents with abdominal masses in children and adults.
- Immunodeficiency-associated BL: More likely to involve extranodal sites.
- Biopsy with histopathology (“starry sky” pattern) and immunohistochemistry (CD19, CD20, CD10, high Ki-67) is essential.
- Cytogenetic studies detect the c-myc translocation.
- Molecular studies may detect EBV and other genetic mutations.
- Imaging (CT, MRI, PET) is used for staging and assessing disease extent.
Treatment and Management ▾: Intensive chemotherapy regimens (e.g., CODOX-M/IVAC, Hyper-CVAD, DA-EPOCH-R) often combined with rituximab (immunotherapy) are the mainstays of treatment. Supportive care is crucial.
Prognosis ▾: While aggressive, BL is often highly treatable, especially in children. Prognosis is influenced by age, stage, treatment response, genetic abnormalities, immunodeficiency status, and access to healthcare.
*Click ▾ for more information
Introduction
Burkitt lymphoma (BL) is a highly aggressive (fast-growing) type of B-cell non-Hodgkin lymphoma. It is a fast-growing cancer of the lymphatic system, specifically affecting B lymphocytes. Burkitt lymphoma is known for its extremely rapid doubling time, meaning the tumor can double in size very quickly. This rapid growth contributes to its aggressive nature.
Burkitt lymphoma is a rare disease, accounting for about 1-2% of all non-Hodgkin lymphomas and is often associated with the Epstein-Barr virus (EBV). It occurs most often in children and young adults, but can also develop in adults. BL can develop in various locations throughout the body, including the jaw, abdomen, and central nervous system.
Pathogenesis of Burkitt Lymphoma
Epstein-Barr Virus (EBV) Infection
EBV primarily infects B lymphocytes. After infection, EBV can persist in B cells in a latent state, meaning the virus is present but not actively replicating. EBV expresses certain proteins that can disrupt the normal mechanisms controlling B cell growth and survival. These viral proteins can promote uncontrolled proliferation of B cells, increasing the risk of cancerous transformation.
EBV can exhibit different latency patterns in infected cells, with varying levels of viral gene expression. In Burkitt lymphoma, a specific latency pattern called latency I is commonly observed, where only a limited number of viral genes are expressed.
The association between EBV and Burkitt lymphoma varies among the different subtypes of Burkitt lymphoma.
- Endemic Burkitt Lymphoma: This form is most strongly associated with EBV, with nearly all cases showing EBV involvement.
- Sporadic Burkitt Lymphoma: This form has a weaker association with EBV, with only a fraction of cases showing EBV involvement.
- Immunodeficiency-associated Burkitt Lymphoma: This form has an intermediate association with EBV, with a portion of cases showing EBV involvement.
While EBV infection is an important factor, it’s usually not enough on its own to cause Burkitt lymphoma. Other factors, such as genetic abnormalities (like the c-myc translocation) and environmental factors (like malaria in endemic areas), also play crucial roles in Burkitt lymphoma development. These factors can work together with EBV to promote the uncontrolled growth of B cells and the development of Burkitt lymphoma.
Genetic factors
Genetic factors, particularly the translocation of the c-myc oncogene, play a crucial role in the development of Burkitt lymphoma (BL). c-myc is a proto-oncogene that normally regulates cell growth, proliferation, and differentiation. It codes for a transcription factor that controls the expression of many genes involved in these processes. In normal cells, c-myc expression is tightly controlled.
In Burkitt lymphoma, a chromosomal translocation typically occurs, involving the c-myc gene on chromosome 8 and an immunoglobulin gene (usually the heavy chain gene on chromosome 14). The most common translocation in Burkitt lymphoma is t(8;14)(q24;q32). The translocation leads to dysregulation of c-myc expression, resulting in its constitutive (always-on) activation in B cells. This uncontrolled c-myc expression drives excessive cell proliferation, a hallmark of Burkitt lymphoma. The affected B cells lose normal growth control and undergo rapid, uncontrolled division.
While the c-myc translocation is the hallmark genetic abnormality in Burkitt lymphoma (BL), other genetic alterations can also contribute to its development and progression.
Mutations in ID3
ID3 is a gene that encodes an inhibitor of DNA binding (ID) protein, which plays a role in cell differentiation and growth. Mutations in ID3 are found in a significant proportion of Burkitt lymphoma cases, particularly in sporadic Burkitt lymphoma. These mutations can disrupt the normal function of ID3, leading to uncontrolled cell growth and proliferation.
Mutations in TCF3
TCF3 is a gene that encodes a transcription factor involved in B cell development and differentiation. Mutations in TCF3 have been identified in some Burkitt lymphoma cases, and these mutations can also contribute to uncontrolled cell growth.
Mutations in Components of the SWI/SNF Complex
The SWI/SNF complex is a group of proteins that regulate gene expression by modifying chromatin structure. Mutations in genes encoding components of the SWI/SNF complex, such as ARID1A and SMARCA4, have been found in some Burkitt lymphoma cases. These mutations can disrupt the normal regulation of gene expression, contributing to BL development.
Other factors
Immunosuppression
Immunosuppression, particularly in the context of HIV/AIDS, has a significant impact on the development and behavior of Burkitt lymphoma (BL). Immunosuppression weakens the immune system’s ability to detect and eliminate cancerous cells, including those that could develop into Burkitt lymphoma. Immunosuppression can also lead to reactivation of latent EBV infection in B cells, increasing the risk of EBV-driven B cell proliferation and Burkitt lymphoma development.
Environmental factors
Environmental factors, particularly malaria in endemic regions, play a significant role in the development of Burkitt lymphoma (BL). Endemic Burkitt lymphoma is most common in equatorial Africa, where malaria is also highly prevalent. Chronic malaria infection is thought to be a crucial cofactor in the development of endemic BL.
Mechanisms of action
- Impaired immune response: Chronic malaria infection can impair the immune system’s ability to control B cell growth and EBV infection.
- Increased B cell proliferation: Malaria can stimulate B cell proliferation, increasing the pool of cells susceptible to EBV infection and malignant transformation.
- Cytokine dysregulation: Malaria can lead to dysregulation of cytokines, which are signaling molecules that play a role in immune responses and cell growth. This dysregulation can further contribute to B cell proliferation and Burkitt lymphoma development.
Clinical Features
Burkitt lymphoma (BL) is a fast-growing cancer with a variety of clinical presentations depending on the specific form of the disease. Symptoms can develop and progress rapidly.
General Symptoms
- Fatigue: Persistent tiredness and lack of energy
- Loss of appetite
- “B symptoms” are a common group of symptoms associated with lymphomas, including Burkitt lymphoma.
- Fever: Unexplained persistent or recurring fever
- Night sweats: Drenching sweats that soak clothes and bedding
- Weight loss: Unexplained loss of 10% or more of body weight over 6 months
Endemic Burkitt Lymphoma

Primarily affects children in equatorial Africa. The most common presentation is a rapidly growing tumor in the jaw or other facial bones, often causing swelling, pain, and loose teeth. Can also involve the abdomen, orbits (eye sockets), and other organs
Sporadic Burkitt Lymphoma
Occurs worldwide, affecting children and adults. The most common presentation is an abdominal mass, often in the ileocecal region (where the small and large intestines meet) or other parts of the gastrointestinal tract. Can also involve the ovaries, testes, and central nervous system.
Immunodeficiency-associated Burkitt Lymphoma
Occurs in individuals with weakened immune systems, such as those with HIV/AIDS or post-transplant patients. It is more likely to involve extranodal sites, such as the bone marrow, central nervous system, and gastrointestinal tract. Clinical features can vary depending on the specific site of involvement.
Laboratory Investigations
Diagnosing Burkitt lymphoma (BL) requires a combination of laboratory investigations to confirm the diagnosis and differentiate it from other conditions.
Blood tests
- Complete blood count (CBC): May show normal or elevated white blood cell count and decreased red blood cell count (anemia) or platelet count (thrombocytopenia).
- Liver and kidney function tests: May show abnormal results.
- Lactate dehydrogenase (LDH) levels: May show elevated lactate dehydrogenase (LDH) levels, a marker of cell damage and rapid cell turnover.
Imaging studies
Imaging studies play a crucial role in diagnosing and staging Burkitt lymphoma (BL). These studies help visualize the extent of the disease and identify any affected organs or tissues.
- Ultrasound: Often used as an initial imaging modality, especially for evaluating abdominal masses in children. It can reveal enlarged lymph nodes, abdominal masses, or involvement of organs such as the kidneys or ovaries.
- Computed tomography (CT) scan: Can detect enlarged lymph nodes in the chest, abdomen, and pelvis. It can also be used to identify involvement of organs such as the liver, spleen, and kidneys. It is also used to assess the extent of disease and help with staging.
- Magnetic resonance imaging (MRI): Can be useful for evaluating involvement of the central nervous system, bone marrow, or other soft tissues. It can provide more detailed information about tumor size and location compared to CT.
- Positron emission tomography (PET) scan: Uses a radioactive tracer to detect metabolically active cells, such as cancer cells. It can identify areas of increased metabolic activity, indicating the presence of lymphoma cells. It can also be useful for staging the disease and assessing response to treatment. PET/CT scan is increasingly used in the diagnosis and management of Burkitt lymphoma due to its ability to detect metabolically active tumor cells.
Biopsy
Biopsy of the lymph node is essential for diagnosis.
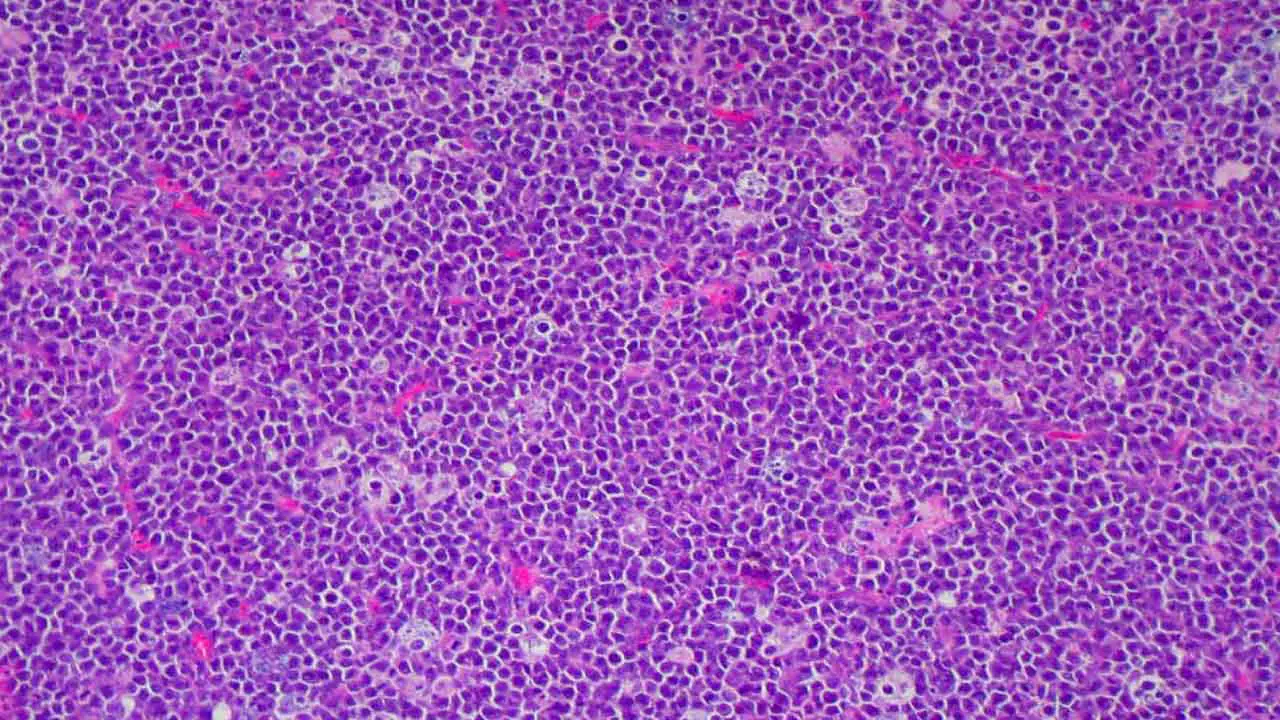
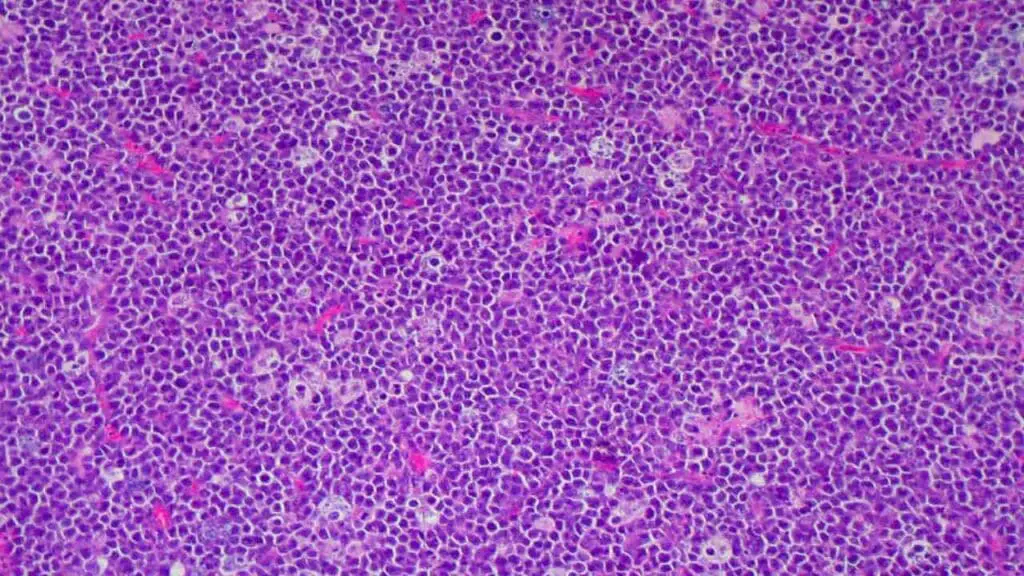
- Histopathology: Shows characteristic “starry sky” pattern with small, uniform lymphocytes and numerous tingible body macrophages
- Immunohistochemistry: Shows specific markers for B cells (CD19, CD20, CD10) and a high proliferation rate (Ki-67)
Cytogenetic studies
Cytogenetic and molecular studies help confirm the diagnosis and provide prognostic information. Cytogenetic studies may show the characteristic t(8;14) translocation involving the c-myc gene and the immunoglobulin heavy chain gene. It may also show other variant translocations involving c-myc and other immunoglobulin genes.
Molecular studies
May show evidence of EBV infection in tumor cells (especially in endemic BL). May show mutations in ID3, TCF3, or other genes.
Others
- Bone marrow aspiration and biopsy: May show infiltration of the bone marrow by lymphoma cells if there is involvement of the bone marrow.
- Lumbar puncture and cerebrospinal fluid (CSF) analysis: May show lymphoma cells in the CSF if there is involvement of the central nervous system.
Treatment and Management
Burkitt lymphoma (BL) is an aggressive cancer, but it’s also highly responsive to treatment. The primary treatment approach is intensive chemotherapy, often combined with immunotherapy.
Chemotherapy
Burkitt lymphoma requires intensive chemotherapy regimens given in short, intensive cycles. These regimens typically include multiple chemotherapy drugs given in combination. Chemotherapy may also be given directly into the cerebrospinal fluid (intrathecally) to prevent or treat central nervous system involvement.
Commonly used drugs:
- Cyclophosphamide
- Doxorubicin
- Vincristine
- Methotrexate
- Cytarabine
- Ifosfamide
- Etoposide
Regimen examples:
- CODOX-M/IVAC
- Hyper-CVAD
- DA-EPOCH-R
Immunotherapy
Immunotherapy for Burkitt lymphoma uses rituximab. This monoclonal antibody targets the CD20 protein on B cells and is often added to chemotherapy regimens to improve outcomes.
Supportive Care
- Tumor lysis syndrome (TLS) prevention: Intensive chemotherapy can lead to TLS, a condition caused by the rapid breakdown of cancer cells. Careful monitoring and preventive measures, such as hydration and allopurinol, are crucial.
- Infection prevention: Chemotherapy can weaken the immune system, increasing the risk of infections. Preventive measures, such as antibiotics and antifungal medications, may be necessary.
- Nutritional support: Maintaining good nutrition is important during treatment. Nutritional support may be needed to address any nutritional deficiencies.
Treatment of Specific Burkitt Lymphoma Forms
- Endemic BL: Treatment is similar to other forms of BL, with intensive chemotherapy regimens being the mainstay of treatment.
- Sporadic BL: Treatment is also similar, with intensive chemotherapy regimens often combined with rituximab.
- Immunodeficiency-associated BL: Treatment needs to consider the patient’s underlying immunodeficiency. Antiretroviral therapy (ART) is crucial for HIV-associated BL, along with chemotherapy and rituximab.
Monitoring and Follow-up
- Response assessment: Regular imaging studies and other tests are done to assess response to treatment.
- Long-term follow-up: Long-term follow-up is important to monitor for any late effects of treatment or relapse.
Prognosis of Burkitt Lymphoma
Burkitt lymphoma (BL), while aggressive, has a generally favorable prognosis, especially with prompt and intensive treatment.
Factors Influencing Prognosis
| Factors | Favorable | Less Favorable |
| Age | Children & young adults | Older adults |
| Disease stage | Early (limited) | Advanced (widespread) |
| Treatment response | Complete remission | Residual disease / relapse |
| Genetic abnormalities | c-myc translocation only | TP53, complex karyotype |
| Immunodeficiency status | None | HIV/AIDS |
| Access to quality healthcare | Early diagnosis & prompt treatment | Delayed diagnosis or suboptimal treatmetn |
Overall Outlook
- High cure rates in children: With intensive chemotherapy, cure rates in children with BL are very high, often exceeding 90%.
- Good outcomes in adults: Adults with BL also have good outcomes with intensive treatment, with cure rates ranging from 70% to 80%.
- Improvements with rituximab: The addition of rituximab to chemotherapy regimens has further improved outcomes for both children and adults with BL.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- López C, Burkhardt B, Chan JKC, Leoncini L, Mbulaiteye SM, Ogwang MD, Orem J, Rochford R, Roschewski M, Siebert R. Burkitt lymphoma. Nat Rev Dis Primers. 2022 Dec 15;8(1):78. doi: 10.1038/s41572-022-00404-3. PMID: 36522349.
- Ferry JA. Burkitt’s lymphoma: clinicopathologic features and differential diagnosis. Oncologist. 2006 Apr;11(4):375-83. doi: 10.1634/theoncologist.11-4-375. PMID: 16614233.
- Schmitz R, Young RM, Ceribelli M, Jhavar S, Xiao W, Zhang M, Wright G, Shaffer AL, Hodson DJ, Buras E, Liu X, Powell J, Yang Y, Xu W, Zhao H, Kohlhammer H, Rosenwald A, Kluin P, Müller-Hermelink HK, Ott G, Gascoyne RD, Connors JM, Rimsza LM, Campo E, Jaffe ES, Delabie J, Smeland EB, Ogwang MD, Reynolds SJ, Fisher RI, Braziel RM, Tubbs RR, Cook JR, Weisenburger DD, Chan WC, Pittaluga S, Wilson W, Waldmann TA, Rowe M, Mbulaiteye SM, Rickinson AB, Staudt LM. Burkitt lymphoma pathogenesis and therapeutic targets from structural and functional genomics. Nature. 2012 Oct 4;490(7418):116-20. doi: 10.1038/nature11378. Epub 2012 Aug 12. PMID: 22885699; PMCID: PMC3609867.
- Quintana MDP, Smith-Togobo C, Moormann A, Hviid L. Endemic Burkitt lymphoma – an aggressive childhood cancer linked to Plasmodium falciparum exposure, but not to exposure to other malaria parasites. APMIS. 2020 Feb;128(2):129-135. doi: 10.1111/apm.13018. Epub 2020 Mar 4. PMID: 32133709.
- Atallah-Yunes SA, Murphy DJ, Noy A. HIV-associated Burkitt lymphoma. Lancet Haematol. 2020 Aug;7(8):e594-e600. doi: 10.1016/S2352-3026(20)30126-5. PMID: 32735838.
- Crombie J, LaCasce A. The treatment of Burkitt lymphoma in adults. Blood. 2021 Feb 11;137(6):743-750. doi: 10.1182/blood.2019004099. PMID: 33171490.