TL;DR
Granulocytes: Basophils are a type of granulocyte, a group of white blood cells characterized by their large granules.
- Allergic reactions: They play a crucial role in allergic reactions (type I hypersensitivity) by releasing histamine and other inflammatory mediators.
- Parasitic infections: Basophils are also involved in the immune response to parasitic infections.
- Inflammation: Basophils contribute to inflammatory processes in various conditions.
- Allergic conditions: Asthma, rhinitis, urticaria
- Hematological disorders: Chronic myelogenous leukemia
- Hypothyroidism: Decreased thyroid hormone production
- Infections: Parasitic infections
- Medications: Heparin, corticosteroids
- Acute infections: Increased neutrophils and inflammation
- Corticosteroid therapy: Suppresses basophil production
- Stress: Hormonal changes and immune system suppression
- Pregnancy: Hormonal fluctuations and immune system adjustments
Laboratory investigations ▾: Basophil counts, activation tests, and mediator measurements can be used to assess their function and involvement in diseases.
*Click ▾ for more information
Introduction
Basophils are a type of granulocyte, which are white blood cells characterized by their large, dark blue granules in their cytoplasm. They are the least common of the granulocytes, making up less than 1% of circulating white blood cells.
Overview of the Immune System
The immune system is a complex network of cells, tissues, and organs that work together to protect the body from harmful pathogens, such as bacteria, viruses, fungi, and parasites. It is made up of two main components: the innate immune system and the adaptive immune system.
Innate immune system: This is the body’s first line of defense against pathogens. It is non-specific, meaning it does not target a particular pathogen. The innate immune system includes physical barriers like the skin and mucous membranes, as well as cells such as neutrophils, macrophages, and natural killer cells.
Adaptive immune system: This is a more specific and slower-acting immune response. It is able to recognize and target specific pathogens. The adaptive immune system involves lymphocytes, including B cells and T cells. B cells produce antibodies that bind to specific antigens on pathogens, while T cells directly attack infected cells.
Both the innate and adaptive immune systems work together to protect the body from infections. When a pathogen enters the body, the innate immune system responds first. If the pathogen is not eliminated by the innate immune system, the adaptive immune system is activated. The adaptive immune system is able to develop memory cells, which allow the body to quickly respond to future infections with the same pathogen.
Role of Granulocytes in Immune Responses
Granulocytes play a crucial role in immune responses by providing a rapid and effective first line of defense against pathogens. These white blood cells are characterized by their granules in their cytoplasm, which contain various enzymes and toxic substances that help to destroy invading microorganisms.
Key functions of granulocytes
- Phagocytosis: Granulocytes, particularly neutrophils, are capable of engulfing and destroying bacteria, fungi, and other foreign particles through a process known as phagocytosis. They use their granules to release enzymes that break down the engulfed material.
- Release of inflammatory mediators: Basophils and eosinophils play a vital role in allergic reactions and inflammation. They release various inflammatory mediators, such as histamine, prostaglandins, and leukotrienes, which help to recruit other immune cells to the site of infection or injury and promote tissue repair.
- Killing of parasites: Eosinophils are particularly effective at killing parasites. They release toxic substances that damage the parasite’s cell membrane.
- Regulation of immune responses: Granulocytes can also help to regulate immune responses by releasing factors that can either promote or suppress inflammation.
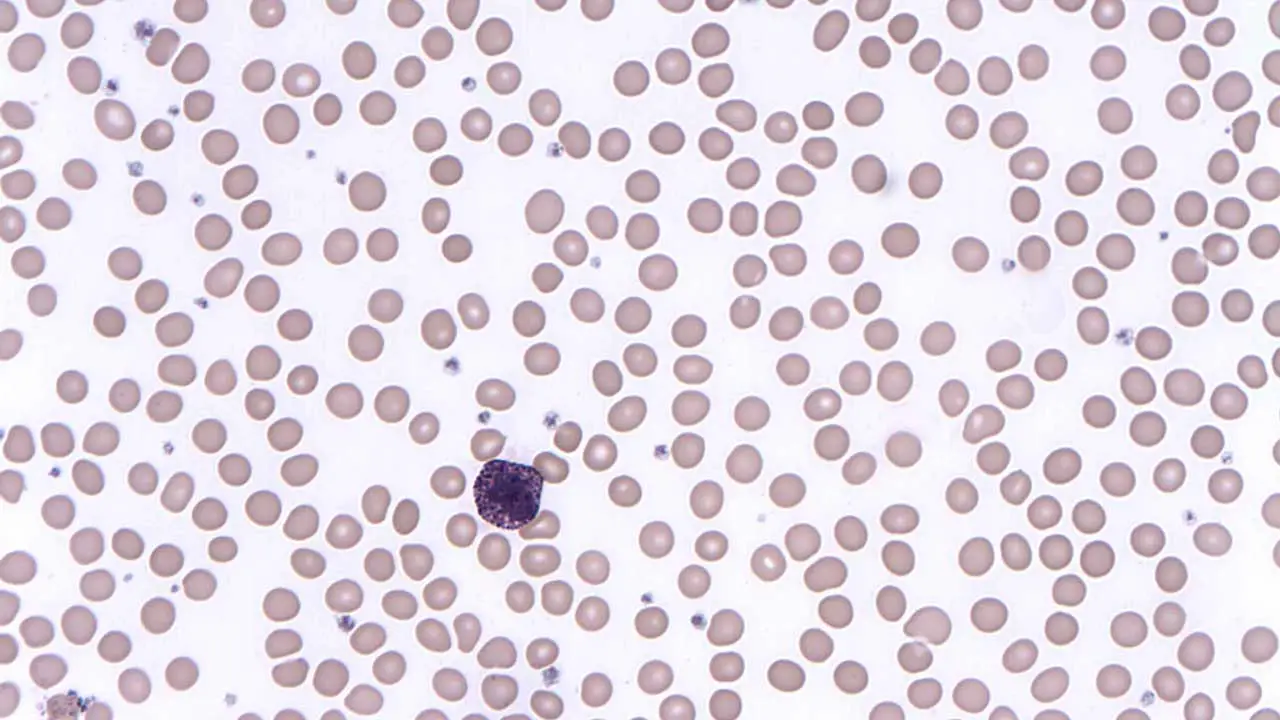
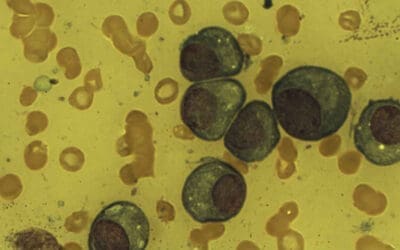
Morphology of Basophils
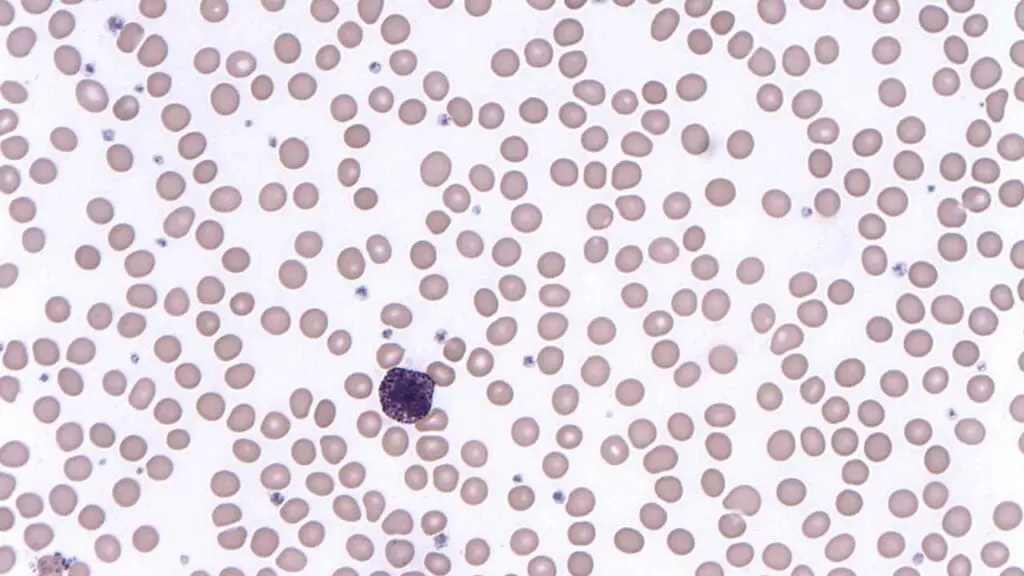
Nucleus: The nucleus is typically divided into two lobes, although it can sometimes appear as a single, horseshoe-shaped nucleus. The chromatin within the nucleus is condensed and stains dark blue or purple with Romanowsky-type stains.
Cytoplasmic Granules: Basophils are packed with numerous granules, often obscuring the nucleus. The granules in the cytoplasm are significantly larger than those found in neutrophils or eosinophils. These granules stain a dark blue or purple color due to their high content of histamine and other vasoactive substances.
Comparison with Other Granulocytes
| Feature | Neutrophils | Eosinophils | Basophils |
| Nucleus | Multilobed (3-5 lobes) | Bilobed | Bilobed |
| Granules | Small, pale pink | Large, orange-pink | Large, dark blue |
| Function | Phagocytosis of bacteria and fungi | Killing of parasites and involvement in allergic reactions | Release of histamine and other mediators involved in allergic reactions |
Lifespan in Blood and Reference Range
Basophils have a relatively short lifespan in the bloodstream, typically ranging from 8 to 12 hours. This is in contrast to neutrophils, which have a lifespan of a few days, and eosinophils, which can survive for several weeks. The short lifespan of basophils reflects their role in immediate immune responses, particularly allergic reactions. They are rapidly mobilized to sites of inflammation and are consumed or degraded after fulfilling their function.
Normal Reference Range
Basophils are the least abundant granulocyte in peripheral blood, typically comprising less than 1% of the total white blood cell count.
The normal reference range can vary slightly between laboratories but generally falls within the following range:
- 0.01-0.1% of total white blood cells
- 20-50 cells/µL
Functions of Basophils
Role in Allergic Reactions (Type I Hypersensitivity)
Basophils are key players in type I hypersensitivity reactions, which are immediate allergic responses triggered by exposure to allergens. Upon activation by allergens, they release preformed granules containing histamine, a potent inflammatory mediator. Histamine causes vasodilation, increased capillary permeability, and contraction of smooth muscle, leading to the symptoms of allergic reactions such as sneezing, runny nose, watery eyes, and skin rashes.
Basophils also release other inflammatory mediators, including leukotrienes and prostaglandins, which contribute to the development and progression of allergic reactions.
Involvement in Parasitic Infections
Basophils and eosinophils often work together in response to parasitic infections. Both cell types release mediators that can damage parasites and promote inflammation.
Basophils may also play a role in regulating the immune response to parasites, helping to balance the body’s response to the infection.
Basopoiesis
Basopoiesis is the specialized process of basophil production and maturation, originating from hematopoietic stem cells in the bone marrow. These stem cells differentiate into common myeloid progenitors, which then commit to the basophil lineage under the influence of specific cytokines, primarily Interleukin-3 (IL-3), and possibly other growth factors. Unlike mast cells, which leave the bone marrow as progenitors and mature in peripheral tissues, basophils complete their maturation within the bone marrow before being released into the bloodstream as mature, circulating cells, maintaining a tightly regulated low count in healthy individuals.
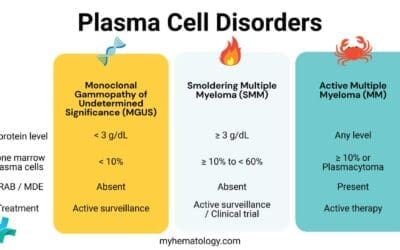
Causes of High Basophils (Basophilia)
Basophilia (high basophils) can be caused by various factors.
Allergic Conditions
- Asthma: Chronic inflammation of the airways often associated with basophilia.
- Rhinitis: Inflammation of the nasal mucosa often due to allergic reactions can lead to basophilia (high basophils).
- Urticaria: A skin condition characterized by hives, often due to allergic reactions can also be associated with basophilia.
Hematological Disorders
- Chronic myeloid leukemia (CML): A type of cancer characterized by the overproduction of white blood cells including basophils.
- Other myeloid disorders: Basophil counts can be abnormal in other hematological disorders, such as myeloproliferative syndromes and myelodysplastic syndromes.
Hypothyroidism
- Reduced metabolism: Hypothyroidism can lead to various metabolic changes including basophilia.
Infections
- Parasitic infections: Certain parasitic infections, such as helminthiasis (worm infections), can trigger basophilia as part of the immune response.
Medications
- Heparin: This anticoagulant medication can sometimes cause basophilia (high basophils) as a side effect.
- Corticosteroids: While typically used to suppress inflammation, corticosteroids can paradoxically cause basophilia (high basophils) in some individuals.
Causes of Low Basophils (Basopenia)
Basopenia can be caused by various factors.
Acute Infections
- Neutrophilia: During acute infections, there is often a surge in neutrophils, which are another type of granulocyte. This can lead to a relative decrease in basophils.
- Inflammation: The inflammatory response associated with acute infections can also affect basophil numbers.
Corticosteroid Therapy
- Anti-inflammatory effects: Corticosteroids are potent anti-inflammatory drugs that can suppress the production and release of basophils.
- Dosage and duration: The extent of basopenia induced by corticosteroids can depend on the dosage and duration of treatment.
Stress
- Hormonal changes: Stress can lead to the release of stress hormones, such as cortisol, which can influence basophil production and function.
- Immune system suppression: Chronic stress can also suppress the immune system, including basophil activity.
Pregnancy
- Hormonal changes: Hormonal fluctuations during pregnancy can affect basophil numbers.
- Immune system adjustments: The body’s immune system undergoes various adjustments during pregnancy, which can influence basophil counts.
Laboratory Investigations
Several laboratory tests can be used to evaluate basophil function and count. These laboratory tests can be used in various clinical settings for:
Diagnose allergic conditions: Basophilia and positive BAT results can be indicative of allergic diseases such as asthma, rhinitis, and urticaria.
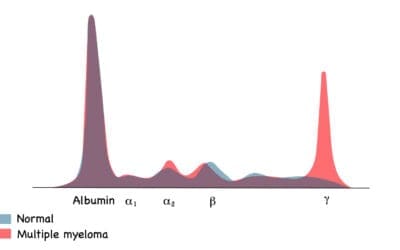
Evaluate hematological disorders: Basophil counts can be helpful in diagnosing certain hematological disorders, such as chronic myeloid leukemia.
Monitor treatment response: These tests can be used to monitor the response to treatment for allergic conditions or other disorders associated with abnormal basophil function.
Research: Laboratory investigations of basophils are also used in research to study the role of these cells in various immune responses and diseases.
Complete Blood Count (CBC) with Differential
A CBC with differential includes a count of all white blood cells, including basophils. The percentage of basophils in the total white blood cell count can be used to assess whether there is basophilia or basopenia.
Basophil Activation Test (BAT)
The BAT measures the ability of basophils to degranulate and release mediators in response to stimuli. It can be used to assess sensitivity to specific allergens by exposing basophils to these allergens in vitro.
Measurement of Basophil-Derived Mediators
- Histamine: Histamine is a key mediator released by basophils. Measuring histamine levels in the blood or other body fluids can provide insights into basophil activation.
- Tryptase: Tryptase is another mediator released by basophils. Measuring tryptase levels can also be helpful in assessing basophil activation, particularly in conditions such as mastocytosis.
Frequently Asked Questions (FAQs)
Can stress affect basophils?
Yes, stress can affect basophil counts, though the impact is generally more often associated with a decrease in basophils (basopenia) rather than an increase (basophilia), particularly during acute stress.
Do basophils increase with age?
Generally, no. Basophil counts do not significantly increase with age in humans to the point of causing basophilia. In fact, some studies, particularly in mice, suggest that while the absolute numbers of basophils in certain compartments like bone marrow and spleen might increase with age, their functionality (e.g., degranulation and cytokine production) can be impaired.
In humans, the normal reference range for basophils remains consistently low across adult age groups (typically 0.02 – 0.1 x 109/L, or 0-100 cells/mm3). While there might be minor fluctuations or individual variability, there’s no established trend of increasing basophil counts in healthy aging that would lead to a diagnosis of basophilia solely due to age. If an elderly person presents with basophilia, it would prompt the same investigation for underlying conditions (myeloproliferative neoplasms, allergies, chronic inflammation, hypothyroidism) as it would for a younger adult, rather than being dismissed as a normal age-related change.
Do basophils increase with allergies?
Yes, basophils can increase with allergies. Basophils are key immune cells involved in allergic reactions, and their activation and subsequent release of inflammatory mediators like histamine are central to allergic symptoms.
While a dramatic increase leading to clear basophilia (an absolute count above 0.1x 109/L or 100 cells/mm3) might not be seen in every mild allergic reaction, persistent or severe allergic conditions can indeed cause an elevation in basophil counts.
For example, chronic allergic conditions such as asthma, atopic dermatitis (eczema), and chronic allergic rhinitis can be associated with basophilia. In some cases, a rapid drop in circulating basophils (basopenia) might occur during an acute, severe allergic reaction like anaphylaxis as basophils quickly migrate from the blood into the affected tissues where they degranulate.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Goldberg S, Hoffman J. Clinical Hematology Made Ridiculously Simple, 1st Edition: An Incredibly Easy Way to Learn for Medical, Nursing, PA Students, and General Practitioners (MedMaster Medical Books). 2021.
- Keohane EM, Otto CN, Walenga JM. Rodak’s Hematology 6th Edition (Saunders). 2019.
- Blumenreich MS. The White Blood Cell and Differential Count. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 153.
- Poto R, Loffredo S, Marone G, Di Salvatore A, de Paulis A, Schroeder JT, Varricchi G. Basophils beyond allergic and parasitic diseases. Front Immunol. 2023 May 2;14:1190034. doi: 10.3389/fimmu.2023.1190034. PMID: 37205111; PMCID: PMC10185837.
- Karasuyama, Hajime et al. Multifaceted roles of basophils in health and disease. Journal of Allergy and Clinical Immunology, Volume 142, Issue 2, 370 – 380
- Miyake K, Ito J, Karasuyama H. Role of Basophils in a Broad Spectrum of Disorders. Front Immunol. 2022 May 27;13:902494. doi: 10.3389/fimmu.2022.902494. PMID: 35693800; PMCID: PMC9186123.