TL;DR
Vascular bleeding disorders encompass a diverse range of conditions marked by easy bruising and minor vessel bleeds.
Inherited Vascular Disorders ▾
- Hereditary hemorrhagic telangiectasia
- Connective tissue disorders e.g. Ehlers-Danlos syndromes and Pseudoxanthoma elasticum
- Giant cavernous hemangioma
Acquired Vascular Disorders ▾
- Simple easy bruising
- Senile purpura
- Purpura associated with infections
- Henoch-Schönlein syndrome
- Scurvy
- Steroid purpura
*Click ▾ for more information
Introduction
Vascular bleeding disorders are a group of medical conditions marked by easy bruising and spontaneous hemorrhage from capillaries and small blood vessels.
Physiology of Normal Hemostasis
The blood clotting cascade is a complex but crucial process that prevents excessive bleeding after injury. It involves a coordinated interplay between platelets, vessel wall components, and various clotting factors in the blood.
Key Players
- Platelets: These are small, disc-shaped cells that clump together to form a plug at the site of injury.
- Vessel Wall: When damaged, the vessel wall releases substances that activate platelets and clotting factors.
- Clotting Factors: These are proteins circulating in the blood that work in a cascade-like fashion to ultimately form fibrin, a mesh that stabilizes the platelet plug.
Key Pathways
There are two main pathways that initiate the clotting cascade:
- Intrinsic Pathway: This pathway is activated within the blood itself, triggered by contact with exposed collagen fibers from a damaged vessel wall. It involves a series of clotting factors (proteins) like factors XII, XI, IX, and VIII, ultimately leading to the activation of factor X.
- Extrinsic Pathway: This pathway is faster and is activated by tissue factor, a protein released by damaged tissues outside the bloodstream. Tissue factor directly activates factor VII, which then activates factor X.
Both pathways converge at the common pathway, where factor X is further activated. This leads to the formation of thrombin, the key enzyme that converts fibrinogen (soluble blood protein) into fibrin (insoluble mesh). Platelets, activated by the damaged vessel wall and clotting factors, adhere to the fibrin mesh, forming a strong clot that seals the wound..
Clot Breakdown
The body also has a counterbalancing system called the fibrinolysis. This system includes enzymes like plasmin, which break down fibrin clots once the bleeding has stopped. This prevents unnecessary clot formation that could block blood flow.
In essence, the clotting cascade is a tightly regulated process ensuring timely clot formation to stop bleeding while the fibrinolytic system maintains blood flow by dissolving clots when they are no longer needed.
Causes of Abnormal Bleeding
Abnormal bleeding can arise from various issues within the complex blood clotting system.
Platelet Abnormalities
- Quantitative deficiencies (thrombocytopenia): This refers to a low platelet count in the blood. Platelets are essential for forming an initial plug at the injury site. This can be caused by conditions like bone marrow problems, medications, or an enlarged spleen trapping platelets. Examples: Immune thrombocytopenia (ITP), bone marrow failure syndromes.
- Qualitative defects (dysfunctional platelets): Even with a normal platelet count, the platelets themselves might be malfunctioning and unable to clump together effectively. This can be due to genetic disorders or certain medications. Examples: Glanzmann’s thrombasthenia, Bernard-Soulier syndrome.
Vessel Wall Defects
- Hereditary disorders: Certain genetic conditions like Ehlers-Danlos syndrome weaken the blood vessel walls, making them more prone to rupture and bleeding.
- Acquired conditions: Deficiencies in vitamin C, essential for collagen production in blood vessel walls, can lead to increased fragility. Inflammatory conditions or medications like corticosteroids can also weaken vessels.
Coagulation Factor Deficiencies
- Inherited disorders: Hemophilia A, B, and von Willebrand disease are well-known examples where specific clotting factors are missing or dysfunctional due to genetic mutations.
- Acquired deficiencies: Liver disease can impair the production of clotting factors, and vitamin K deficiency can affect the activation of certain factors. Additionally, some medications like warfarin (blood thinner) deliberately reduce clotting factor activity.
WHO Bleeding Grades
The World Health Organization (WHO) bleeding scale is a standardized tool used by healthcare professionals to assess the severity of bleeding episodes in patients with suspected vascular bleeding disorders. It assigns a grade (0-4, with an additional grade 5) based on the type, location, and need for medical intervention for the bleeding.
| WHO Bleeding Scale Grade | Description of Bleeding | Examples |
| 0 | No bleeding | None |
| 1 | Petechiae or easy bruising | Tiny red/purple spots on skin, large bruises with minimal trauma |
| 2 | Mucous membrane bleeding | Nosebleeds (epistaxis), bleeding gums, blood in urine (hematuria), heavy menstrual bleeding (menorrhagia) |
| 3 | Gross blood loss (intramuscular or intraluminal) | Blood in vomit or stool, bleeding into joints (hemarthrosis), heavy vaginal bleeding after childbirth |
| 4 | Debilitating blood loss | Bleeding in the brain (intracranial hemorrhage), major bleeding after trauma requiring blood transfusion |
| 5 | Fatal bleeding | Life-threatening bleeding leading to death |
Purpura, Ecchymoses and Petechiae
Purpura, ecchymoses, and petechiae are all terms used to describe bleeding into the skin, but they differ based on the size of the bleeding area.
- Petechiae: These are the smallest and appear as tiny, pinpoint red or purple spots on the skin, usually less than 3 millimeters (mm) in diameter. They don’t blanch (turn pale) when pressed because the blood is trapped under the skin. Petechiae are often a sign of platelet dysfunction or fragile blood vessels.
- Purpura: These are larger than petechiae, ranging from 4 to 10 mm in diameter. They also appear as red or purple spots, but may be more irregular in shape compared to petechiae. Similar to petechiae, purpura doesn’t blanch with pressure. Purpura can be caused by platelet problems, weak blood vessels, or even certain medications.
- Ecchymoses: These are the largest of the three and are commonly known as bruises. They are typically larger than 1 cm (centimeter) in diameter and can vary significantly in size and color. Ecchymoses develop through stages, changing from red or purple to blue, green, yellow, and eventually fading away as the body reabsorbs the blood. Ecchymoses can be caused by injury, bleeding disorders, or even medications that thin the blood.
Here’s an analogy to visualize the size difference:
- Petechiae: Imagine a speck of pepper.
- Purpura: Think of the size of a lentil.
- Ecchymoses: Picture a large coin, like a quarter.
Clinical Differences: Platelets/Vessel Wall Bleeding vs. Coagulopathies
Knowing the type of bleeding disorder helps healthcare professionals narrow down the cause and choose the most appropriate diagnostic tests. For example, if a patient presents with easy bruising and normal clotting times, platelet function tests would be a priority. Conversely, if a patient has deep joint bleeds and prolonged clotting time, testing for specific clotting factor deficiencies would be crucial.
| Feature | Platelet/Vessel Wall Dysfunction | Coagulopathies (Coagulation Factor Deficiencies) |
| Bleeding Type | Typically superficial | Often deep, internal bleeding |
| Location | Skin (petechiae, purpura), mucous membranes (nosebleeds, gum bleeds) | Muscles, joints (hemarthrosis), internal organs (brain bleeds, gastrointestinal bleeds) |
| Onset | Spontaneous or after minor trauma | May occur spontaneously, but often triggered by surgery, injury, or childbirth |
| Bruising | Easy bruising, large bruises with minimal trauma | Bruising may be less common or absent |
| Blood Clot Formation | Clot formation at the injury site may be abnormal or delayed | Blood takes longer to clot |
| Laboratory Tests | * Normal clotting time (PT, aPTT) * Abnormal platelet function tests (bleeding time) | * Prolonged clotting time (PT, aPTT) * Specific factor deficiencies identified |
Inherited Vascular Bleeding Disorders
Hereditary Hemorrhagic Telangiectasia (HHT)

- Cause: Genetic mutations affecting genes involved in blood vessel formation resulting in vascular bleeding. These are autosomal dominant mutations.
- Symptoms:
- Characteristic small, dilated blood vessels (telangiectasia) on the lips, mouth, fingers, and mucous membranes.
- Recurrent nosebleeds are a common symptom, and other areas with telangiectasia may bleed as well.
- In severe cases, internal bleeding can occur in the lungs, gastrointestinal tract, or brain.
- Diagnosis: Based on clinical features and family history. Imaging studies may be used to identify internal lesions. Genetic testing to confirm the diagnosis is available.
- Treatment: No cure exists, but management focuses on controlling bleeding episodes. This can involve embolization, laser ablation to remove them, estrogens, tranexamic acid and iron supplementation. Thalidomide, lenalidomide and others have been used to reduce gastrointestinal bleeding and bleeding at other sites in severe cases.
Connective Tissue Disorders
Several connective tissue disorders involve mutations in genes responsible for collagen production and other structural components of blood vessels. This can lead to vessel wall weakness and increased bleeding risk. Here are two examples:
Ehlers-Danlos Syndrome (EDS): A group of inherited disorders affecting collagen with purpura due to abnormal platelet adhesion, hyperextensibility of the joints and hyperelastic friable skin. Some types of EDS (e.g., vascular EDS) can cause easy bruising, bleeding from mucous membranes, and problems with wound healing.
Pseudoxanthoma Elasticum (PXE): A rare disorder affecting elastic fibers in connective tissues. This can lead to fragile blood vessels that bleed easily, particularly in the skin, eyes, and gastrointestinal tract causing arterial hemorrhage and thrombosis.
- Diagnosis: Based on clinical symptoms like superficial bleeding and purpura following minor trauma, family history, and specific diagnostic criteria for each disorder. Genetic testing can confirm specific types of EDS and PXE.
- Treatment: There’s no cure, but management focuses on preventing injuries and controlling bleeding episodes. Physical therapy may help strengthen tissues, and medications or procedures might be used to address specific bleeding complications.
Giant Cavernous Hemangioma
- Cause: A rare vascular malformation where abnormal, dilated blood vessels form a large, sponge-like mass.
- Symptoms:
- May present with a painless lump or mass on the skin or within an internal organ.
- Depending on the location and size, symptoms can include pain, swelling, bleeding, or even organ dysfunction.
- Diagnosis: Imaging studies like ultrasound, MRI, or CT scan are used to identify the hemangioma.
- Treatment: Treatment options depend on the size, location, and severity of symptoms.
- Observation might be sufficient for small, asymptomatic hemangiomas.
- For larger or symptomatic cases, treatment options include surgery (when feasible), embolization (blocking blood flow to the hemangioma), or medication to shrink the mass.
Acquired Vascular Defects
While inherited disorders are a significant cause of vascular bleeding, many acquired factors can also weaken blood vessels and lead to easy bruising or abnormal bleeding under the skin.
Simple Easy Bruising
- Cause: A common benign disorder. The most common cause is unknown (idiopathic). Aging, sun damage, and medications like aspirin or blood thinners (anticoagulants) can also contribute.
- Symptoms: Easy bruising with minimal trauma is the main symptom. Petechiae or purpura might be present.
- Diagnosis: Usually based on clinical features and the absence of other medical conditions.
- Treatment: No specific treatment is needed for occasional easy bruising. Avoiding blood-thinning medications and using sun protection can be helpful.
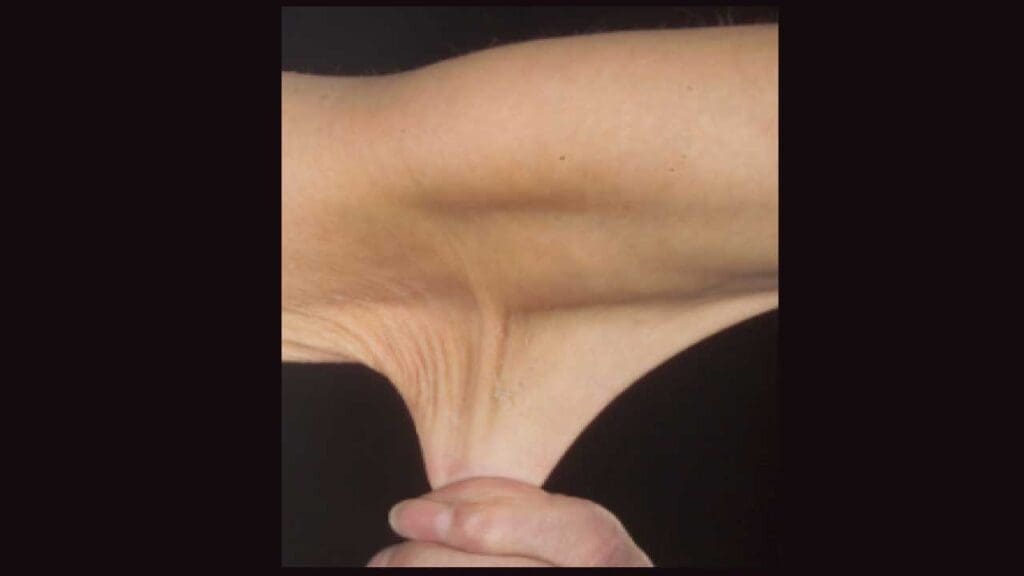
Senile Purpura
- Cause: Thinning and fragility of blood vessel walls due to aging.
- Symptoms: Purpuric lesions (red-purple patches) typically appear on the forearms and hands of elderly individuals.
- Diagnosis: Usually based on clinical features and age of the patient.
- Treatment: No specific treatment is needed unless bleeding is severe. Pressure dressings or topical vitamin K creams might be used.
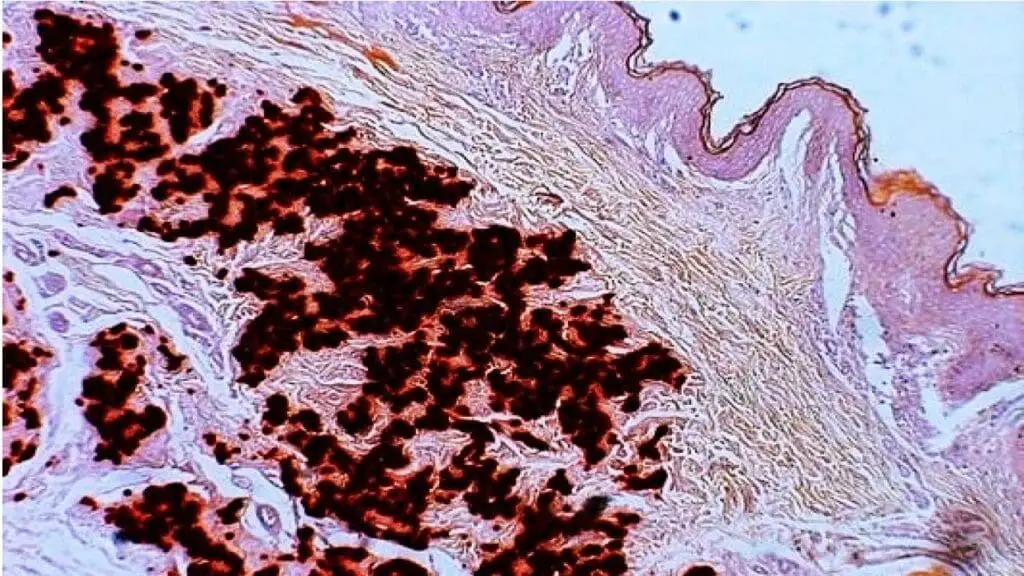
Purpura Associated with Infections
- Cause: Infections can damage blood vessels or cause platelet dysfunction, leading to purpuric lesions. Viral infections (mononucleosis) and bacterial infections (meningococcemia) are examples.
- Symptoms: Purpura along with other symptoms of the underlying infection (fever, fatigue).
- Diagnosis: Clinical features, laboratory tests for infection (blood cultures), and sometimes a skin biopsy might be needed.
- Treatment: Treatment focuses on addressing the underlying infection with antibiotics or antivirals.
Henoch-Schönlein Purpura (HSP)
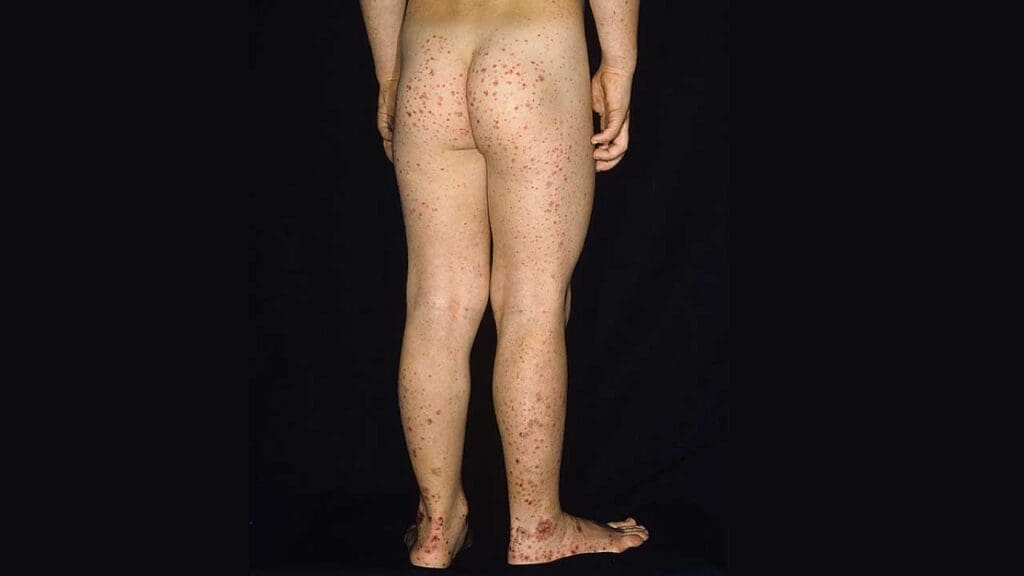
- Cause: The exact cause is unknown, but it is thought to be an autoimmune reaction triggered by an infection. This condition typically develops in children and often follows a recent upper respiratory tract infection. It involves an immune system reaction mediated by immunoglobulin A (IgA) that targets blood vessels (IgA-mediated vasculitis).
- Symptoms: Purpuric lesions on the buttocks and legs, along with joint pain, abdominal pain, and sometimes blood in the stool (hematuria).
- Diagnosis: Clinical features and laboratory tests might be used to rule out other causes.
- Treatment: Treatment is usually supportive with pain relievers and rest. Steroids might be used in severe cases.
Scurvy (Vitamin C Deficiency)
- Cause: Severe deficiency of vitamin C, which is essential for collagen formation (a building block of blood vessel walls).
- Symptoms: Easy bruising, bleeding gums, fatigue, and poor wound healing are classic signs.
- Diagnosis: Clinical features and blood tests to measure vitamin C levels.
- Treatment: Vitamin C supplementation is the mainstay of treatment. Bleeding symptoms usually improve quickly with adequate intake.
Steroid Purpura
- Cause: Long-term use of high-dose corticosteroids or Cushing’s syndrome can weaken blood vessels by causing abnormal vessel supportive tissue, leading to easy bruising, especially on the arms and legs.
- Symptoms: Easy bruising and petechiae are the main symptoms.
- Diagnosis: Usually based on medication use and clinical features.
- Treatment: The best approach is to minimize corticosteroid use if possible. Pressure dressings might be helpful for severe bruising.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.




