Introduction
The prothrombin time (PT) test is a blood test that measures how long it takes for a blood clot to form. It is one of the most common blood tests performed in the world, and it is used to diagnose and monitor a variety of bleeding and clotting disorders.
The prothrombin time (PT) test works by measuring the amount of time it takes for prothrombin to be converted to thrombin. Prothrombin is a protein that is produced by the liver, and it is essential for blood clotting. Thrombin is an enzyme that converts fibrinogen to fibrin, which is the main component of blood clots.
The prothrombin time (PT) test is performed by mixing a sample of the patient’s blood with a reagent that contains tissue factor and calcium. Tissue factor is a protein that activates the coagulation cascade, which is the series of events that leads to blood clot formation. Calcium is also required for blood clotting.
The time it takes for a clot to form is measured in seconds. The normal range for the prothrombin time (PT) is 10 to 13 seconds. A prolonged prothrombin time (PT) indicates that it is taking longer for the blood to clot than normal. This can be caused by a variety of factors, including:
- Vitamin K deficiency
- Liver disease
- Kidney disease
- Certain medications, such as warfarin and heparin
- Bleeding disorders, such as hemophilia and von Willebrand disease
The prothrombin time (PT) test is a valuable tool for diagnosing and monitoring bleeding and clotting disorders. It is also used to monitor the effectiveness of blood thinners, such as warfarin.
Principle of Prothrombin Time (PT)
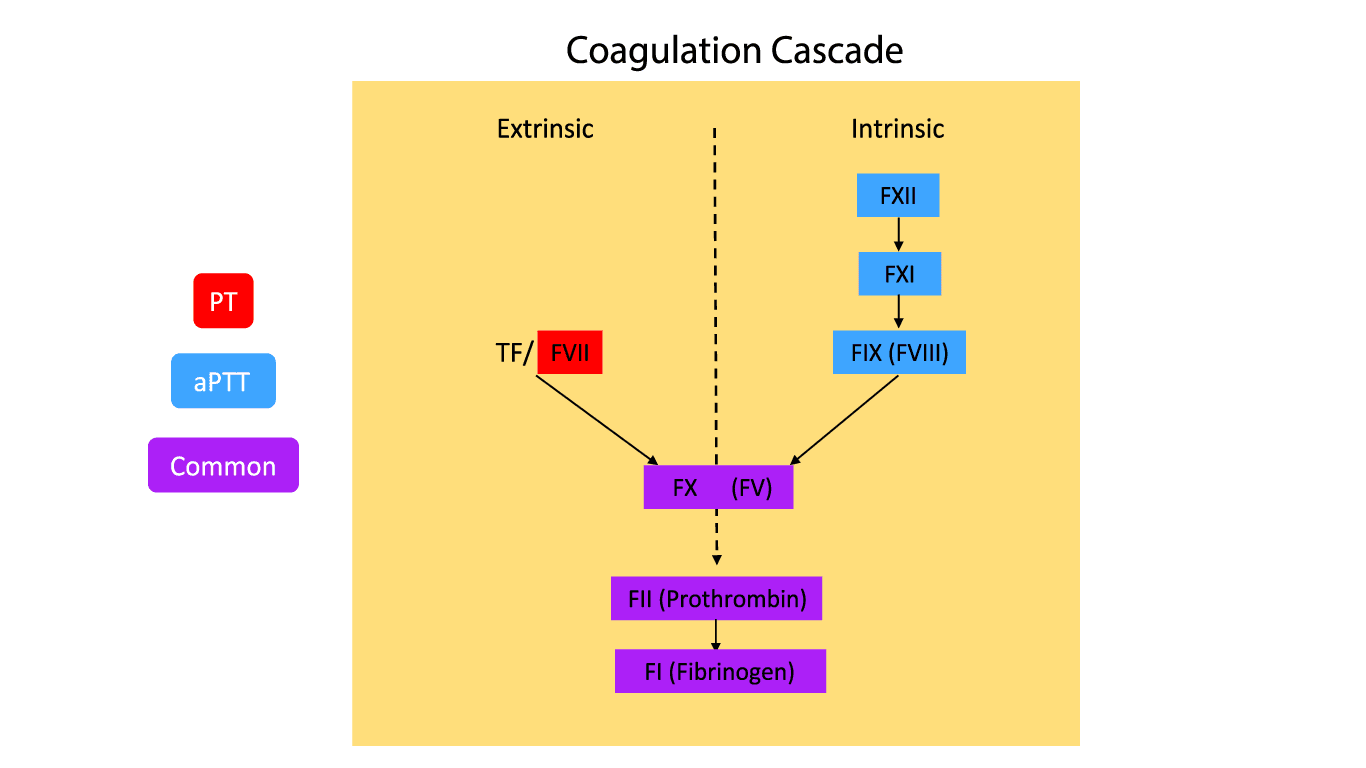
The prothrombin time (PT) test is based on the principle that the conversion of prothrombin to thrombin is the final step in the extrinsic coagulation pathway.
The extrinsic coagulation pathway is activated by tissue factor, which is released from damaged tissues. Tissue factor activates factor VII, which in turn activates factor X. Factor X then activates factor IX, which in turn activates factor II (prothrombin). Prothrombin is converted to thrombin in the presence of calcium.
Thrombin is a protease that cleaves fibrinogen to fibrin. Fibrin is a protein that forms a mesh-like network that traps blood cells and other elements of the blood, forming a clot.
Method differs slightly according to the manufacturer’s protocol.
Materials
- #Platelet poor plasma (PPP) of patient and control. PPP is prepared by centrifuging the peripheral blood at 2000 g for 15 minutes at room temperature.
- *Thromboplastin
- *0.025 mol/L calcium chloride (CaCl2)
- *Glass tubes 5 ml
- *Water bath
- Stop watch
- Pipettes 100 – 200 uL
- Pipette tips
*These items must be at 37°C.
#PPP must be kept at room temperature to prevent activation of factor VIII which may cause an inaccurate timing result.
Protocol
This test must be performed in the water bath at all times apart from the observation of the clot formation step.
- Add 0.1 mL plasma of both patient and control into a test tube, respectively and label accordingly. Incubate for 1 – 3 minutes.
- Add 0.1 mL thromboplastin into each test tube. Incubate for 1 – 3 minutes.
- Get the stopwatch ready, add 0.1 mL CaCl2 and immediately start the timer.
- Gently mix the solution in the test tubes by tilting the test tubes to 45° angle and agitate lightly.
- Intermittently take the tubes out of the water bath to observe for the first sign of clot formation.
- Stop the timer and record the time at the first sign of clot formation.
- Test both patient and control plasma in duplicates and record the average time.
*Some manufacturers have added the thromboplastin reagent to CaCl2, thus step 3 can be omitted in such cases and just proceed with recording the time after step 2.
Interpretation
Prothrombin time (PT) reference range
| Parameter | Time | Unit |
| Rabbit thromboplastin | 11 – 16 | seconds |
| Human thromboplastin | 10 – 12 | seconds |
A prolonged prothrombin time (PT) indicates that it is taking longer for the blood to clot than normal. This can be caused by a variety of factors, including:
- Vitamin K deficiency
- Liver disease
- Kidney disease
- Certain medications or oral anticoagulation drugs, such as warfarin and heparin – vitamin K antagonists
- Factor VII, X, V or prothrombin deficiency or defect.
- Disseminated intravascular coagulation (DIC)
Isolated prolonged prothrombin time (PT) could indicate Factor VII deficiency while shortened PT could be found following treatment with rVIIa.
International Normalized Ratio (INR)
What is INR?
The International Normalized Ratio is a standardized blood test result calculated from the Prothrombin Time (PT). It is used primarily to monitor the effectiveness of anticoagulant medications, particularly warfarin.
How is INR Calculated?
INR =(Patient′s PT/Control PT)ISI
- The patient’s prothrombin time (PT) is a measurement in seconds of how long it takes the patient’s blood to clot.
- The control prothrombin time (PT) is the clotting time of a standard blood sample used by the laboratory.
- The International Sensitivity Index (ISI) is a value assigned by the manufacturer of the testing reagent to account for variations in the sensitivity of different reagents.
Function
The primary function of the International Normalized Ratio is to monitor the effectiveness of anticoagulant therapy, primarily warfarin. By maintaining the INR within a therapeutic range, the risk of blood clots (thrombosis) and excessive bleeding (hemorrhage) can be balanced.
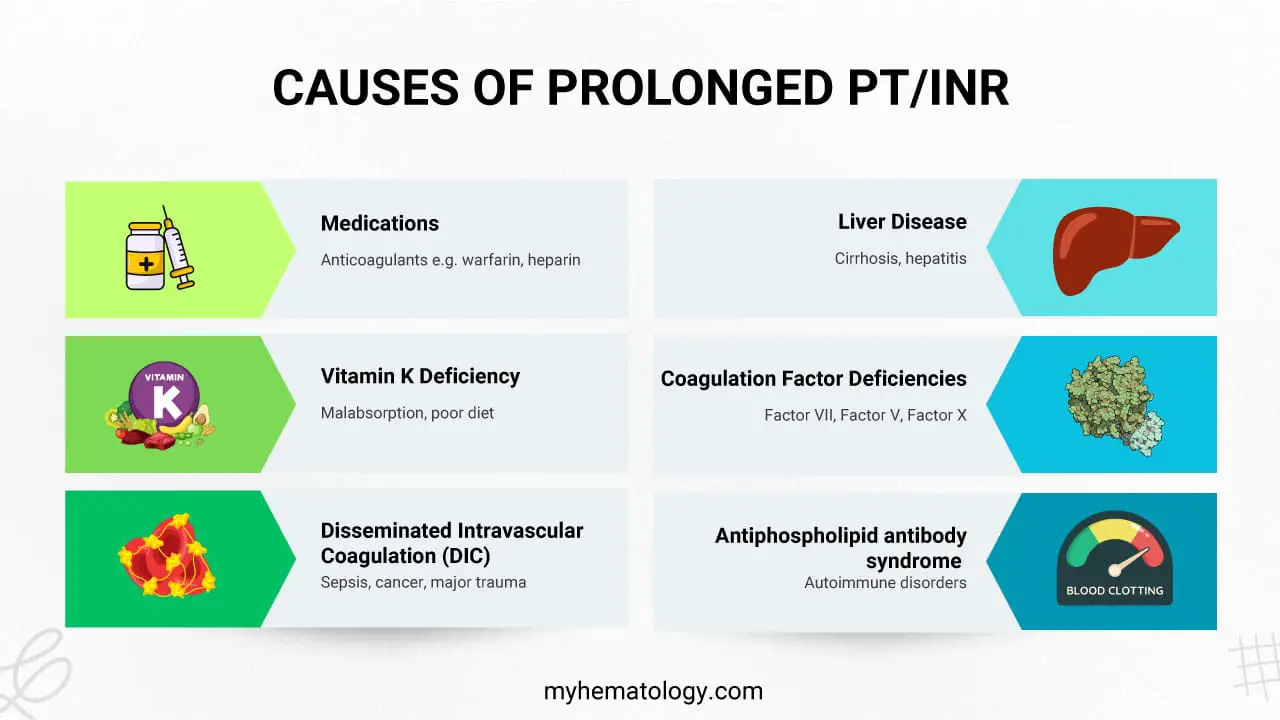
Prolonged PT/INR can be caused by:
- Anticoagulant medications
- Vitamin K antagonists (VKAs) like warfarin inhibit the production of clotting factors, leading to a gradual increase in PT/INR over several days.
- Heparins, direct factor Xa inhibitors, and direct thrombin inhibitors directly interfere with the clotting process, causing immediate increases in prothrombin time (PT) or aPTT (a related blood test).
- Liver dysfunction: The liver produces clotting factors and metabolizes warfarin, so liver disease can lead to prolonged PT/INR. However, this often indicates underlying clotting problems rather than excessive anticoagulation.
- Vitamin K deficiency: Reduced vitamin K availability, due to malnutrition, antibiotics, or malabsorption, can impair clotting factor production and prolong PT/INR.
- Disseminated Intravascular Coagulation (DIC): Widespread blood clotting consumes clotting factors, leading to prolonged PT/INR.
- Clotting factor deficiencies: Congenital or acquired deficiencies of clotting factors involved in the extrinsic pathway can prolong PT/INR.
- Antiphospholipid antibodies: In rare cases, these antibodies can interfere with clotting factor activity and prolong PT/INR, although a prolonged aPTT is more common.
Reference Range
The reference range for International Normalized Ratio varies depending on the clinical situation.
- For individuals not on anticoagulant therapy, a normal INR is typically between 0.8 and 1.2.
- For patients on warfarin, the target INR range is usually 2.0 to 3.0, but this can vary based on the specific medical condition.
- INR over 3.0 may pose a risk of excessive bleeding.
Advantages
- Standardization: The International Normalized Ratio provides a standardized measure of blood clotting time, allowing for consistent interpretation across different laboratories.
- Effective monitoring: It is an effective tool for monitoring the efficacy of warfarin therapy.
- Risk management: By maintaining the INR within the therapeutic range, the risk of both thrombosis and hemorrhage can be minimized.
Disadvantages
- Affected by other factors: Factors such as liver disease, vitamin K deficiency, and certain medications can influence INR results, complicating interpretation.
- Time-consuming: INR results can take several hours to obtain, limiting its usefulness in emergency situations.
- Potential for variability: There can be variability in INR results between different laboratories and even within the same laboratory.
Misuse
One common misuse of INR is requesting blood products unnecessarily. For example, some healthcare providers may order blood products for patients with elevated INR values without considering other factors such as the patient’s clinical condition, bleeding risk, and the specific INR level. This can lead to unnecessary blood product transfusions, increased costs, and potential complications.
Other Considerations
- INR and Pregnancy: INR monitoring is crucial during pregnancy for women on warfarin, as the drug can cross the placenta and affect the fetus.
- INR and Diet: Foods rich in vitamin K, such as green leafy vegetables, can affect INR levels. Consistent dietary intake is important for stable INR results.
- INR and Drug Interactions: Numerous medications can interact with warfarin and affect INR levels. It’s essential to consider all medications a patient is taking when interpreting INR results.
By understanding the intricacies of INR, healthcare providers can make informed decisions regarding anticoagulant therapy and minimize the risks associated with this treatment.
Frequently Asked Questions (FAQs)
What is PT and INR used for?
PT (Prothrombin Time) and INR (International Normalized Ratio) are blood tests primarily used to:
Monitor Anticoagulant Therapy
- Warfarin: INR is specifically used to monitor the effectiveness of warfarin, a blood-thinning medication. It helps ensure the patient is on the right dose to prevent blood clots without excessive bleeding.
Assess Blood Clotting Ability
- Bleeding disorders: Both prothrombin time (PT) and INR can help diagnose bleeding disorders by measuring how long it takes blood to clot.
- Liver function: Since the liver produces clotting factors, abnormal prothrombin time (PT) and INR values can indicate liver problems.
- Pre-surgery evaluation: These tests can be used to assess a patient’s clotting ability before surgery to determine the risk of bleeding.
In essence, prothrombin time (PT) and INR are important tools for managing blood clotting conditions and monitoring anticoagulant therapy.
What is the difference between PT/INR and aPTT?
PT/INR and aPTT are both blood tests that evaluate different parts of the blood clotting process.
PT/INR
- Measures the extrinsic and common pathways of the clotting cascade.
- Primarily used to monitor patients on warfarin (a blood thinner).
- INR is a standardized version of prothrombin time (PT) to allow for comparison of results across different laboratories.
aPTT
- Measures the intrinsic and common pathways of the clotting cascade.
- Primarily used to monitor patients on heparin (another blood thinner).
- More sensitive to deficiencies in clotting factors involved in the early stages of clotting.
What is the difference between a high and low PT/INR?
High PT/INR
A high PT/INR indicates that the blood is taking longer than normal to clot. This increases the risk of bleeding.
Potential causes of a high PT/INR
- Over-anticoagulation: Patients on warfarin (Coumadin) are particularly susceptible. This can occur if the dose is too high or if there are drug interactions.
- Liver disease: The liver produces clotting factors. Liver disease can impair this function, leading to prolonged PT/INR.
- Vitamin K deficiency: Vitamin K is essential for clotting factor production. Its deficiency can result in a high PT/INR.
- Disseminated Intravascular Coagulation (DIC): A complex condition where widespread clotting consumes clotting factors, leading to a paradoxical bleeding tendency.
Low PT/INR
A low PT/INR means the blood clots too quickly, increasing the risk of thrombosis (blood clot formation).
Potential causes of a low PT/INR
- Under-anticoagulation: Patients on warfarin might not be adequately protected from clots if their INR is too low.
- Genetic clotting disorders: These can lead to a hypercoagulable state.
- Certain medications: Some drugs can interfere with clotting mechanisms.
- Malignancy: Some cancers can be associated with a hypercoagulable state.
Clinical Significance
It is importat to interpret PT/INR results in the context of a patient’s clinical presentation. A high PT/INR might require a decrease in anticoagulant dosage, while a low PT/INR might necessitate an increase.
What are the symptoms of high INR levels?
A high INR indicates that the blood is taking longer to clot than normal. This can lead to excessive bleeding. Symptoms of a high INR may include:
- Easy bruising
- Nosebleeds
- Bleeding gums
- Heavy menstrual bleeding
- Blood in urine or stool
- Prolonged bleeding from cuts or injuries
- Vomiting blood or coffee-ground-like material
What INR is too high for surgery?
Generally, an INR of 1.5 or below is considered safe for most surgeries. However, the ideal INR level before surgery can vary depending on the type of surgery, the patient’s overall health, and the surgeon’s preference.
- < 1.5: Generally considered safe for most surgeries.
- 1.5 – 2.0: Might require careful evaluation and potential delay of surgery or administration of vitamin K to lower the INR.
- > 2.0: Significantly increases the risk of bleeding and might necessitate surgery postponement until the INR is lowered.
Glossary of Related Medical Terms
- Extrinsic Pathway: The coagulation route activated by tissue injury and the release of Tissue Factor (Factor III).
- Common Pathway: The final stage of coagulation where the intrinsic and extrinsic pathways meet, involving Factors X, V, II (Prothrombin), and I (Fibrinogen).
- International Sensitivity Index (ISI): A numerical value assigned by manufacturers to a batch of thromboplastin, indicating its sensitivity compared to an international standard.
- Thromboplastin: A reagent used in the PT test that mimics the body’s tissue factor to initiate the extrinsic pathway.
- Vitamin K Antagonist (VKA): A class of drugs (like Warfarin) that interfere with the recycling of Vitamin K, leading to the production of inactive clotting factors (II, VII, IX, X).
- Hemostasis: The physiological process that stops bleeding at the site of an injury.
- Hypoprothrombinemia: A deficiency of prothrombin (Factor II) in the blood, leading to a tendency to bleed.
Disclaimer: This protocol is intended for informational purposes only and may need to be modified depending on the specific laboratory procedures and patient circumstances. Always consult with a qualified healthcare professional for guidance. See additional information.
References
- Bain BJ, Bates I, Laffan MA. Dacie and Lewis Practical Haematology: Expert Consult: Online and Print 12th Edition (Elsevier). 2016.
- Saba HI, Roberts HR. Hemostasis and Thrombosis: Practical Guidelines in Clinical Management 1st Edition (Wiley-Blackwell). 2014.
- Dorgalaleh, A., Favaloro, E. J., Bahraini, M., & Rad, F. (2021). Standardization of Prothrombin Time/International Normalized Ratio (PT/INR). International journal of laboratory hematology, 43(1), 21–28. https://doi.org/10.1111/ijlh.13349
- Adcock, D. M., Moore, G. W., Kershaw, G. W., Montalvao, S. A. L., & Gosselin, R. C. (2024). International Council for Standardization in Haematology (ICSH) recommendations for the performance and interpretation of activated partial thromboplastin time and prothrombin time mixing tests. International journal of laboratory hematology, 46(5), 777–788. https://doi.org/10.1111/ijlh.14344
- Shikdar S, Vashisht R, Zubair M, et al. International Normalized Ratio: Assessment, Monitoring, and Clinical Implications. [Updated 2025 Feb 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507707/
- Zaidi SRH, Rout P. Interpretation of Blood Clotting Studies and Values (PT, PTT, aPTT, INR, Anti-Factor Xa, D-Dimer) [Updated 2024 Jun 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK604215/
- Poller, L., Ibrahim, S., Keown, M., Pattison, A., Jespersen, J., & European Action On Anticoagulation (2011). The prothrombin time/international normalized ratio (PT/INR) Line: derivation of local INR with commercial thromboplastins and coagulometers–two independent studies. Journal of thrombosis and haemostasis : JTH, 9(1), 140–148. https://doi.org/10.1111/j.1538-7836.2010.04109.x



