TL;DR
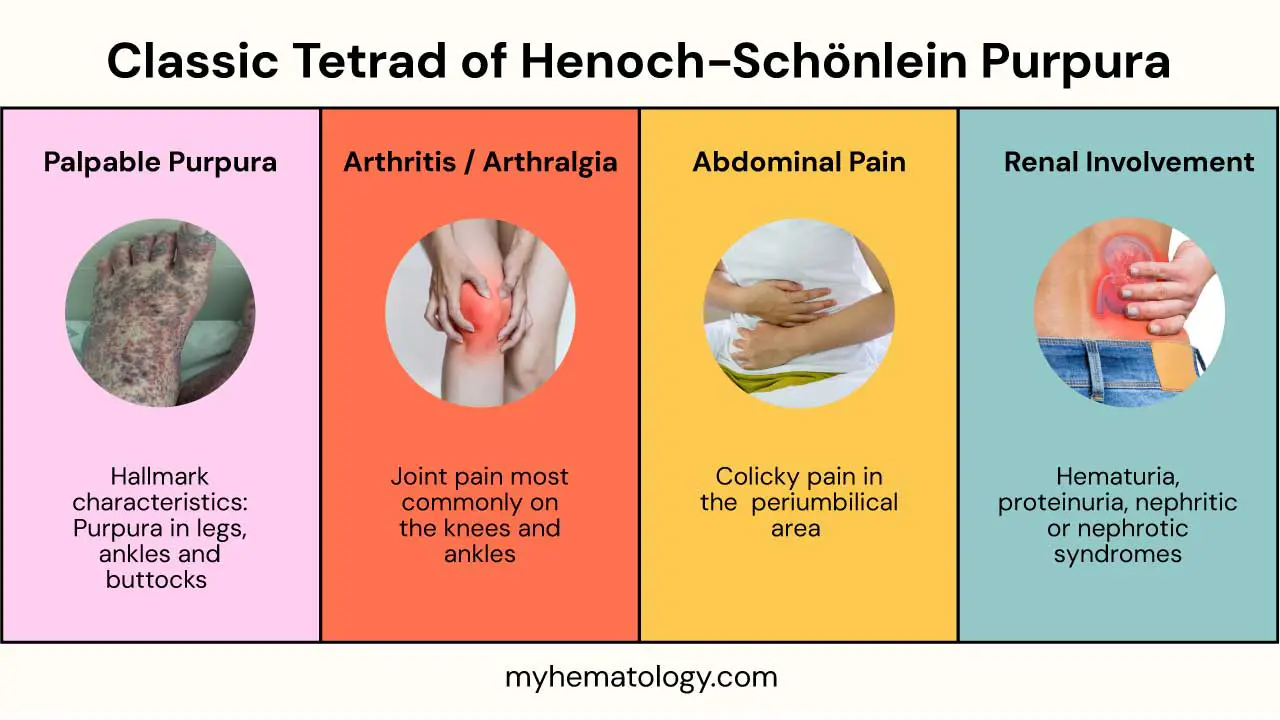
Henoch-Schönlein Purpura (HSP) is a systemic small-vessel vasculitis characterized by palpable purpura, arthritis/arthralgia, abdominal pain, and often kidney involvement.
- Causes ▾: Exact cause unknown; likely triggered by infections (e.g., upper respiratory), medications, or vaccinations, involving IgA antibody deposition.
- Pathophysiology ▾: Inflammation of small blood vessels due to IgA immune complex deposition in the skin, joints, gastrointestinal tract, and glomeruli of the kidneys.
- Symptoms ▾: Palpable purpuric rash (legs, buttocks), joint pain (knees, ankles), abdominal pain (colicky), and potential kidney involvement (hematuria, proteinuria).
- Investigation ▾: Primarily clinical diagnosis. Investigations may include urine analysis (for kidney involvement), blood tests (inflammatory markers), and rarely, skin or kidney biopsy.
- Treatment ▾: Mainly supportive care (pain relief, hydration). Severe gastrointestinal or kidney involvement may require corticosteroids. ACE inhibitors/ARBs for persistent proteinuria.
- Prognosis ▾: Generally good, with spontaneous resolution in most children within weeks. Long-term prognosis depends largely on the severity and persistence of kidney involvement.
*Click ▾ for more information
Introduction
Henoch-Schönlein Purpura (HSP), also known as IgA vasculitis, is a systemic small-vessel vasculitis characterized by the deposition of immunoglobulin A (IgA)-containing immune complexes in the skin, gastrointestinal tract, kidneys, and joints. This widespread inflammation of small blood vessels leads to the characteristic clinical manifestations of the disease.
Incidence
Henoch-Schönlein Purpura (HSP) is the most common systemic vasculitis in children, although it can affect individuals of all ages. The annual incidence of Henoch-Schönlein purpura in children is estimated to be between 10 to 20 cases per 100,000 children per year. Some studies report a slightly wider range, from 6 to 39 cases per 100,000 children annually, depending on the geographical location and study methodology.
The peak incidence occurs in children between the ages of 4 and 6 years, with the majority of cases (around 90%) occurring in children under the age of 10. It is less common in infants and young children.
Henoch-Schönlein purpura often shows a seasonal pattern, with a higher incidence during the fall and winter months and a decrease in the summer. This seasonality suggests a possible link to preceding respiratory infections, which are more common during these colder months.
Causes and Pathophysiology
While the exact cause of Henoch-Schönlein purpura (HSP) remains elusive in many cases, it is widely believed to be triggered by an abnormal immune response following various inciting factors. These potential triggers suggest that Henoch-Schönlein purpura (HSP) is likely a multifactorial disease in individuals with a genetic predisposition.
- Infections: Upper Respiratory Tract Infections (URTIs) is the most frequently reported preceding event, occurring in up to 50-75% of cases. Both viral (e.g., parvovirus B19, adenovirus, influenza, parainfluenza, Epstein-Barr virus) and bacterial (most notably, Streptococcus pyogenes) infections have been implicated. The latent period between the infection and the onset of Henoch-Schönlein purpura symptoms is typically 1-3 weeks. Less commonly, Mycoplasma pneumoniae, Helicobacter pylori, and even certain enteric pathogens have been associated with Henoch-Schönlein purpura (HSP).
- Medications: Certain drugs, such as some antibiotics (e.g., ampicillin), nonsteroidal anti-inflammatory drugs (NSAIDs), angiotensin-converting enzyme (ACE) inhibitors, and vaccines, have been reported as potential triggers in a minority of cases. However, a direct causal link is often difficult to establish.
- Vaccinations: While a temporal association between vaccinations (e.g., measles-mumps-rubella, influenza, hepatitis B) and Henoch-Schönlein purpura has been reported, a definitive causal relationship has not been consistently proven. The benefits of vaccination far outweigh the rare potential risk of triggering Henoch-Schönlein purpura (HSP).
- Insect Bites: Anecdotal reports suggest that insect bites might act as a trigger in some individuals.
- Other Less Common Triggers: Exposure to certain chemicals or allergens has been suggested in isolated cases. In a significant proportion of patients (up to one-third), no clear preceding trigger can be identified.
Pathophysiology
The hallmark of Henoch-Schönlein purpura (HSP) is a systemic inflammation of small blood vessels (vasculitis) characterized by the deposition of IgA-containing immune complexes.
The pathophysiology of Henoch-Schönlein purpura (HSP) centers around an aberrant immune response where the body produces an increased amount of immunoglobulin A (IgA), particularly a form with abnormal glycosylation.
This aberrantly glycosylated IgA1 is prone to forming immune complexes that then circulate in the bloodstream. These IgA-containing immune complexes deposit in the walls of small blood vessels throughout the body, most notably in the skin, gastrointestinal tract, kidneys, and joints.
This deposition triggers a cascade of inflammation within the vessel walls, leading to leukocytoclastic vasculitis, characterized by the infiltration of inflammatory cells and damage to the vessel lining.
The resulting increased vascular permeability allows red blood cells to leak out of the vessels, causing the characteristic palpable purpuric rash. Similarly, inflammation in the gastrointestinal tract leads to abdominal pain and potential bleeding, while in the kidneys, it can disrupt the filtration process, resulting in hematuria and proteinuria.
Ultimately, the widespread small-vessel inflammation driven by IgA immune complex deposition underlies the diverse clinical manifestations observed in Henoch-Schönlein purpura (HSP).
Signs and Symptoms of Henoch-Schönlein Purpura (HSP)

The classic presentation involves a tetrad of features, but patients may not always present with all four simultaneously.
The Classic Tetrad
Palpable Purpura
This is the hallmark cutaneous manifestation and is present in nearly all cases of Henoch-Schönlein purpura. The rash typically begins as small, red spots (petechiae) or raised bumps (papules) that quickly evolve into palpable purpura.
The purpura characteristically appears in gravity-dependent areas, such as the lower extremities (legs and ankles) and buttocks. It can also be found on the extensor surfaces of the arms and, less frequently, on the trunk and face.
The lesions may initially be reddish or purplish and can progress to a brownish color as the extravasated blood breaks down. They do not blanch (turn white) when pressed, indicating that the color is due to blood outside the vessels, not within them. The purpuric lesions can vary in size, ranging from a few millimeters to larger patches.
Arthritis or Arthralgia
Joint involvement is another common feature, affecting a significant proportion of patients. The most commonly affected joints are the knees and ankles, followed by the elbows and wrists. Smaller joints of the hands and feet can also be involved.
The joint pain can range from mild discomfort (arthralgia) to frank arthritis with swelling, tenderness, and limited range of motion.
The arthritis is often migratory and transient, meaning it can affect different joints at different times and usually resolves within days to weeks without causing permanent joint damage.
Abdominal Pain
Gastrointestinal involvement is a significant aspect of Henoch-Schönlein purpura and can be quite distressing. The abdominal pain is typically colicky (cramping and intermittent) in nature and can be severe. It is most commonly localized in the periumbilical or diffuse abdominal area.
The pain may occur before, during, or after the onset of the rash. It can be exacerbated by eating (postprandial). Nausea, vomiting, diarrhea, and even gastrointestinal bleeding (manifesting as melena or hematochezia) can occur.
In rare cases, serious complications like intussusception (telescoping of one part of the intestine into another) or bowel infarction can occur.
Renal Involvement
Kidney involvement is a major concern in Henoch-Schönlein purpura due to its potential for long-term sequelae. Clinically evident renal disease occurs in a significant proportion of patients, although subclinical involvement (detectable only through urine analysis) may be more common.
Manifestations:
- Hematuria: Blood in the urine, which can be microscopic (detected only under a microscope) or macroscopic (visible to the naked eye, making the urine appear pink or red).
- Proteinuria: Protein in the urine, indicating damage to the glomerular filtration barrier.
- Nephritic Syndrome: In more severe cases, patients may develop a nephritic syndrome characterized by hematuria, proteinuria, hypertension, and edema.
- Nephrotic Syndrome: Less commonly, a nephrotic syndrome (heavy proteinuria, hypoalbuminemia, edema) can occur.
Renal involvement usually appears within days to weeks of the onset of other symptoms but can sometimes occur later or even be the initial manifestation.
The severity of renal involvement is the primary determinant of long-term prognosis in Henoch-Schönlein purpura. Most patients have a benign course, but a small percentage may develop chronic kidney disease or end-stage renal disease.
Other Potential Signs and Symptoms
- Scrotal Involvement: In males, scrotal swelling and pain can occur due to vasculitis of the vessels supplying the scrotum. This can sometimes mimic testicular torsion and requires careful evaluation.
- Headache: Some patients may experience headaches.
- Fatigue: General malaise and fatigue are common during the acute phase of the illness.
- Neurological Manifestations: Although rare, neurological symptoms such as seizures or focal neurological deficits have been reported.
- Pulmonary Involvement: Pulmonary hemorrhage is a very rare complication.
Laboratory Investigations of Henoch-Schönlein Purpura (HSP)
While there isn’t a single definitive diagnostic lab test for Henoch-Schönlein purpura (HSP), certain investigations can help support the clinical diagnosis, assess the extent of organ involvement, and rule out other conditions.
Blood Tests
- Complete Blood Count (CBC): Typically, the platelet count is normal, which is crucial in differentiating Henoch-Schönlein purpura from thrombocytopenic purpuras like immune thrombocytopenia (ITP). The white blood cell count may be mildly elevated, reflecting the inflammatory process. Anemia is usually not present at the onset but can occur if there is significant gastrointestinal bleeding or chronic renal disease.
- Inflammatory Markers (Erythrocyte Sedimentation Rate – ESR and C-Reactive Protein – CRP): These markers of inflammation may be elevated, but their levels are often not dramatically high and are non-specific. They can support the presence of inflammation but do not confirm the diagnosis of Henoch-Schönlein purpura.
- Renal Function Tests (Blood Urea Nitrogen – BUN, Creatinine, Electrolytes):
These are essential for assessing kidney involvement. Elevated BUN and creatinine levels indicate impaired renal function. Electrolyte imbalances may also occur in cases of significant renal disease. These tests should be monitored regularly, especially if urinalysis shows abnormalities. - Serum IgA Levels: Serum IgA levels are often elevated in patients with Henoch-Schönlein purpura, particularly during the acute phase. However, elevated IgA is not always present and can be seen in other conditions. Therefore, a normal IgA level does not exclude the diagnosis of HSP, and an elevated level alone is not diagnostic.
- Streptococcal Serology (Antistreptolysin O – ASO titer): If there is a clinical suspicion of a preceding streptococcal infection (e.g., recent sore throat), an ASO titer may be checked. An elevated titer suggests a recent infection but does not confirm a causal link to HSP.
- Coagulation Studies (Prothrombin Time – PT, Activated Partial Thromboplastin Time – aPTT): These are usually normal in Henoch-Schönlein purpura, helping to distinguish it from other causes of purpura related to clotting disorders.
- Albumin Levels: Serum albumin levels may be decreased in cases of significant protein loss due to renal involvement (nephrotic syndrome).
Urine Analysis
This is a crucial investigation to assess for renal involvement. Urinalysis should be performed at the time of diagnosis and monitored regularly to track the course of renal involvement.
The presence of red blood cells in the urine (hematuria) (microscopic or macroscopic) is a common finding. The presence of protein in the urine (proteinuria) indicates glomerular damage. The degree of proteinuria can range from mild to nephrotic range. If proteinuria is detected on urinalysis, a 24-hour urine collection can quantify the amount of protein excretion, helping to assess the severity of renal involvement and guide management.
Urine sediment examination can reveal red blood cell casts, which are indicative of glomerular inflammation.
Stool Occult Blood Test
This test may be performed if the patient presents with significant abdominal pain or if there is suspicion of gastrointestinal bleeding (e.g., anemia, melena). A positive result indicates the presence of blood in the stool.
Biopsy (Skin or Kidney)
Skin Biopsy
A skin biopsy of a purpuric lesion can be helpful in confirming the diagnosis, especially in atypical presentations or when the diagnosis is uncertain.
- Histopathology: The characteristic finding is leukocytoclastic vasculitis, which involves inflammation of small blood vessels in the dermis with infiltration of neutrophils and fibrinoid necrosis.
- Direct Immunofluorescence (DIF): This technique can demonstrate IgA deposition in the walls of the dermal capillaries, which is a key diagnostic feature of Henoch-Schönlein purpura.
Kidney Biopsy
A kidney biopsy is typically reserved for patients with more severe or progressive renal disease (e.g., significant proteinuria, nephritic syndrome, rapidly declining renal function) to assess the severity and type of glomerular involvement, guide treatment decisions, particularly regarding the use of immunosuppressive agents and provide prognostic information.
The histopathological findings vary depending on the severity and stage of renal involvement but typically show mesangial proliferation and IgA deposition in the glomeruli, consistent with IgA nephropathy.
Imaging Studies
- Abdominal Ultrasound: This may be performed in patients with significant abdominal pain to evaluate for complications such as intussusception, bowel wall thickening, or free fluid.
- Renal Ultrasound: This can be used to assess the size and morphology of the kidneys, particularly if there is evidence of renal involvement. It can help rule out other causes of renal dysfunction.
Diagnosis of Henoch-Schönlein Purpura (HSP)
The diagnosis of Henoch-Schönlein purpura (HSP) relies heavily on recognizing the characteristic constellation of clinical findings. Several sets of diagnostic criteria have been proposed over the years, but the EULAR/PRES (European League Against Rheumatism/Paediatric Rheumatology European Society) criteria, revised in 2010, are widely used and provide a structured approach.
| Criterion | Description |
| Mandatory criterion | Palpable purpura with lower limb predominance |
| Minimum 1 out of 4 criteria | 1. Abdominal Pain: Diffuse or colicky pain, potentially with GI bleeding or intussusception. 2. Arthritis or Arthralgia: Acute onset of joint pain or arthritis (swelling, tenderness), any joint but commonly knees/ankles, transient and non-deforming. 3. Renal Involvement: Any hematuria and/or proteinuria occurring during the illness (excluding isolated proteinuria on routine exam). 4. Histopathology Showing IgA Deposition: Biopsy (skin or kidney) showing predominant IgA in small vessels without other vasculitis features. |
Differential Diagnosis of Henoch-Schönlein Purpura (HSP)
| Condition | Key Differentiating Features | Other Notable Features |
| Immune Thrombocytopenia (ITP) | Isolated thrombocytopenia, non-palpable petechiae/purpura, usually no other systemic symptoms. | Often follows viral infection, isolated low platelets. |
| TTP/HUS | Microangiopathic hemolytic anemia, thrombocytopenia, systemic illness, neurological (TTP) or renal (HUS) predominance. | Anemia with schistocytes, elevated LDH, often severe illness. |
| IgA Nephropathy | Primarily isolated hematuria (recurrent macroscopic or persistent microscopic) and proteinuria, systemic features less prominent or absent. | May be considered part of the same disease spectrum as Henoch-Schönlein purpura. |
| Systemic Lupus Erythematosus (SLE) | Wider range of systemic symptoms (malar rash, photosensitivity, serositis), purpura if present is not typically the palpable type of Henoch-Schönlein purpura. | Positive ANA and other autoantibodies, low complement levels. |
| Hypersensitivity Vasculitis | Palpable purpura often triggered by identifiable agent (infection, drug), but typically lacks prominent abdominal pain and IgA deposition on biopsy. | Often resolves with removal of the trigger. |
| ANCA-Associated Vasculitides | Systemic vasculitis with involvement of other organs (e.g., lungs, upper respiratory tract), positive ANCA antibodies. Palpable purpura can be present. | Upper respiratory symptoms (GPA), pulmonary-renal syndrome (MPA), positive ANCA. |
| Meningococcemia | Rapidly progressive petechial/purpuric rash, fever, headache, neck stiffness, altered mental status, systemic toxicity. | Positive blood cultures, often very ill appearance. |
| Rocky Mountain Spotted Fever | Fever, headache, maculopapular rash starting on extremities spreading centrally, history of tick exposure. | Geographic distribution, serological testing. |
| Acute Hemorrhagic Edema of Infancy | Large, painful ecchymotic lesions in infants, often on face/ears, edema, mild systemic symptoms, renal involvement rare. | Primarily affects infants. |
| Non-Accidental Injury | Bruises/purpura in unusual locations/patterns, inconsistent history, other signs of abuse/neglect. Palpability variable. | Social history and physical exam findings concerning for abuse. |
| Drug Reactions | Purpuric rash temporally related to drug exposure, may have other allergic-type symptoms. | History of new medication, resolution with drug discontinuation. |
Treatment and Management of Henoch-Schönlein Purpura (HSP)
The approach largely depends on the severity of the symptoms and the extent of organ involvement, particularly renal involvement. In most cases, Henoch-Schönlein purpura (HSP) is a self-limiting condition, and management focuses on supportive care and symptom relief.
Supportive Care
- Rest and Hydration: Ensuring adequate rest, especially during periods of significant pain or fatigue, is important. Maintaining good hydration is also crucial, particularly if there is gastrointestinal involvement or fever.
- Pain Management:
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): NSAIDs like ibuprofen or naproxen are often used to manage joint pain (arthritis/arthralgia) and mild abdominal pain. However, they should be used with caution due to the potential for gastrointestinal side effects and their possible impact on renal function, especially if there is pre-existing kidney involvement. Close monitoring is advisable.
- Acetaminophen (Paracetamol): Can be used for pain relief and fever control, especially if there are concerns about using NSAIDs.
Medications for Specific Manifestations
- Corticosteroids: Systemic corticosteroids (e.g., prednisone or prednisolone) may be considered for more severe symptoms, such as significant abdominal pain that doesn’t respond to NSAIDs, severe joint involvement limiting mobility, or severe scrotal pain and swelling.
- Immunosuppressants: Immunosuppressive agents (e.g., azathioprine, mycophenolate mofetil, cyclophosphamide) are generally reserved for patients with severe or progressive renal disease (e.g., nephritic syndrome, significant proteinuria, declining renal function) that is not responding to corticosteroids alone. These medications are usually prescribed and monitored by a nephrologist.
- ACE Inhibitors or Angiotensin Receptor Blockers (ARBs): These medications may be used in patients with persistent proteinuria or hypertension related to renal involvement.
Management of Complications
- Intussusception: If intussusception occurs, initial attempts at non-surgical reduction (e.g., air or barium enema) may be tried. Surgical intervention is necessary if non-surgical methods fail or if there are signs of bowel ischemia or perforation.
- Gastrointestinal Bleeding: Management depends on the severity. Mild bleeding may resolve with supportive care. More significant bleeding may require blood transfusions or, rarely, endoscopic intervention if a specific bleeding site is identified.
- Severe Renal Disease: Management of severe renal involvement is complex and typically involves close collaboration with a nephrologist. This may include corticosteroids, immunosuppressants, and management of hypertension and fluid balance. In rare cases of end-stage renal disease, dialysis or kidney transplantation may be necessary.
Prognosis
The prognosis of Henoch-Schönlein Purpura (HSP) is generally very good, especially in children, which is the most commonly affected population. Most individuals experience a self-limiting illness with full recovery and no long-term sequelae. However, the course and potential complications can vary.
While most cases are a one-time event, recurrences of Henoch-Schönlein purpura (HSP) symptoms can occur in a minority of individuals (around 5-10%). These recurrences are usually milder and shorter in duration than the initial episode.
The most significant factor influencing long-term prognosis is the degree of kidney involvement (Henoch-Schönlein Purpura nephritis – HSPN). A small percentage of individuals, particularly adults and those with significant initial kidney disease (e.g., nephrotic syndrome, impaired kidney function), are at a higher risk of developing chronic kidney disease (CKD) in the long term. This can range from mild abnormalities to end-stage renal disease in rare cases.
Individuals who have experienced Henoch-Schönlein purpura (HSP), especially those with kidney involvement, often require long-term monitoring of their kidney function through regular urine tests and blood pressure checks. This helps to detect any signs of developing chronic kidney disease early.
Frequently Asked Questions (FAQs)
How long does Henoch-Schönlein purpura (HSP) take to heal?
The typical healing time for Henoch-Schönlein Purpura (HSP) is 4 to 8 weeks in most children.
Is Henoch-Schönlein purpura (HSP) itchy?
Yes, the rash associated with Henoch-Schönlein Purpura (HSP) can be itchy (pruritic) for some individuals, but it’s not the primary or most prominent symptom.
Does Henoch-Schönlein Purpura (HSP) get worse at night?
Medical literature on Henoch-Schönlein Purpura (HSP) doesn’t typically highlight a consistent pattern of symptoms worsening specifically at night. The symptoms tend to fluctuate throughout the day, often related to activity levels (e.g., joint pain might be worse after activity).
In summary, while some individuals with Henoch-Schönlein Purpura (HSP) might subjectively feel that their symptoms, particularly pain, are worse at night, this isn’t a universally reported characteristic of the disease. It’s more likely due to factors like reduced distraction, body positioning, or individual variations in pain perception.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Roache-Robinson P, Killeen RB, Hotwagner DT. IgA Vasculitis (Henoch-Schönlein Purpura) [Updated 2023 Sep 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537252/
- Bluman J, Goldman RD. Henoch-Schönlein purpura in children: limited benefit of corticosteroids. Can Fam Physician. 2014 Nov;60(11):1007-10. PMID: 25551129; PMCID: PMC4229160.
- Parums DV. A Review of IgA Vasculitis (Henoch-Schönlein Purpura) Past, Present, and Future. Med Sci Monit. 2024 Jan 28;30:e943912. doi: 10.12659/MSM.943912. PMID: 38281080; PMCID: PMC10832303.
- Hetland LE, Susrud KS, Lindahl KH, Bygum A. Henoch-Schönlein Purpura: A Literature Review. Acta Derm Venereol. 2017 Nov 15;97(10):1160-1166. doi: 10.2340/00015555-2733. PMID: 28654132.




