TL;DR
HELLP Syndrome is a serious pregnancy complication (0.2-0.9% of pregnancies) often linked to preeclampsia but definable by its own criteria.
- The HELLP Triad ▾: Characterized by Hemolysis (red blood cell breakdown), ELevated Liver enzymes (indicating liver damage), and LP Low Platelet count (increasing bleeding risk).
- Underlying Causes ▾: Not fully understood but involve blood vessel damage (endothelial dysfunction), abnormal placenta development, and activation of the clotting system.
- Clinical Presentation ▾: Common symptoms include right upper quadrant or epigastric pain, nausea, headache, fatigue, and sometimes visual changes.
- Diagnosis ▾: Relies on recognizing clinical symptoms like upper abdominal pain and confirming with specific blood tests (CBC, Liver Function Tests, Lactate Dehydrogenase). Severity is often graded using the Mississippi classification based on platelet levels.
- Differential Diagnosis ▾: Must be distinguished from other conditions like acute fatty liver of pregnancy, TTP/HUS, and gallbladder issues through careful evaluation.
- Definitive Treatment ▾: The only cure is delivering the baby and placenta, so management focuses on stabilizing the mother and monitoring the fetus until delivery is deemed necessary.
- Complications ▾: Can lead to life-threatening issues for the mother (e.g., liver rupture, DIC, stroke) and baby (e.g., preterm birth, fetal distress).
*Click ▾ for more information
Introduction
HELLP (Hemolysis, Elevated Liver enzymes, and Low Platelets) syndrome is recognized as a serious and potentially life-threatening complication that can occur during pregnancy or shortly after childbirth. This condition is characterized by a specific set of laboratory findings that indicate significant physiological stress in the affected individual.
The syndrome carries the potential for rapid deterioration in both maternal and fetal health, underscoring the critical need for prompt identification and effective management.
The incidence of HELLP syndrome is estimated to occur in 0.2% to 0.9% of all pregnancies.
However, it is more common in women who develop preeclampsia or eclampsia, occurring in 4% to 12% of pregnancies complicated by severe preeclampsia/eclampsia, and up to 15-20% of all cases of preeclampsia.
What is HELLP Syndrome?
The acronym HELLP stands for a constellation of three key findings:
- Hemolysis: The breakdown of red blood cells.
- ELevated Liver enzymes: Indicating liver damage.
- Low Platelet (LP) count: A decrease in the number of platelets in the blood (thrombocytopenia).
Essentially, HELLP syndrome is a serious condition that typically occurs during the later stages of pregnancy or sometimes shortly after childbirth. It is frequently considered a severe variant or complication of preeclampsia, a hypertensive disorder of pregnancy.
While often associated, HELLP syndrome can occur independently of the classic signs of preeclampsia (hypertension and proteinuria) in approximately 10 to 20% of cases. This absence of typical preeclamptic features can make the diagnosis of HELLP syndrome particularly challenging.
Pathophysiology and Risk Factors of HELLP Syndrome
The exact cause of HELLP syndrome remains unknown, but it is often considered a severe manifestation of preeclampsia. Several underlying mechanisms and risk factors have been identified that are believed to contribute to its development.
Underlying Mechanisms (Pathophysiology)
While the precise sequence of events is still being researched, the following processes are thought to play a significant role in the development of HELLP syndrome.
- Vasospasm and Endothelial Dysfunction: Similar to preeclampsia, widespread constriction of blood vessels (vasospasm) and damage to the inner lining of blood vessels (endothelial dysfunction) are thought to be primary events. This can lead to reduced blood flow to organs, including the liver and placenta.
- Abnormal Placentation: Issues with the development and function of the placenta, particularly inadequate trophoblastic invasion of the uterine spiral arteries early in pregnancy, may lead to placental ischemia (reduced blood supply). The ischemic placenta may then release factors that contribute to endothelial damage and systemic inflammation in the mother.
- Activation of the Coagulation System: Endothelial damage can trigger the activation of the coagulation cascade, leading to the formation of small blood clots (microthrombi) in the microvasculature of various organs, including the liver. This contributes to platelet consumption and the “LP” (low platelet count) component of HELLP.
- Microangiopathic Hemolysis: As red blood cells travel through the damaged and narrowed blood vessels with microthrombi, they can become fragmented or damaged, leading to hemolysis (the “H” in HELLP). This results in the characteristic schistocytes seen on the peripheral blood smear and elevated LDH and bilirubin levels.
- Hepatic Involvement: Microthrombi and reduced blood flow in the liver sinusoids can lead to liver cell damage and inflammation, resulting in elevated liver enzymes (the “EL” in HELLP). In severe cases, this can progress to hepatic hematoma or even rupture.
- Inflammatory Response: An exaggerated systemic inflammatory response is also believed to contribute to the endothelial damage and multi-organ dysfunction seen in HELLP syndrome.
- Genetic Predisposition: Some studies suggest a possible genetic predisposition to developing HELLP syndrome. For example, genes involved in the maternal immune response to pregnancy, such as TLR4 (Toll-like Receptor 4) and genes related to cytokine production (e.g., IL-6, TNF-alpha). An exaggerated inflammatory response is implicated in the pathogenesis of HELLP.
Risk Factors
Several factors have been associated with an increased risk of developing HELLP syndrome.
- Preeclampsia/Eclampsia: This is the most significant risk factor. Women with severe preeclampsia or eclampsia have a higher likelihood of developing HELLP syndrome. However, it’s crucial to remember that HELLP can occur in the absence of hypertension and proteinuria in up to 15-20% of cases.
- Previous History of HELLP Syndrome: Women who have had HELLP syndrome in a previous pregnancy have a significantly increased risk of recurrence in subsequent pregnancies (ranging from 16% to 52% in some studies).
- Multiparity: While seemingly counterintuitive, some studies have reported a higher incidence of HELLP syndrome in women who have had more than one previous pregnancy.
- Advanced Maternal Age: Women older than 35 years appear to have a higher risk.
- Family History: A family history of preeclampsia or HELLP syndrome may increase the risk.
- Underlying Medical Conditions: Pre-existing hypertension, diabetes, kidney disease, and autoimmune disorders (like antiphospholipid syndrome or systemic lupus erythematosus) may increase the risk.
- Obesity/Metabolic Syndrome: Obesity is considered a risk factor for preeclampsia and consequently may increase the risk of HELLP syndrome.
- Multiple Gestation: Carrying twins or other multiples increases the risk of hypertensive disorders of pregnancy, including HELLP syndrome.
- History of Poor Pregnancy Outcomes: Women with a history of other adverse pregnancy outcomes may be at higher risk.
Signs and Symptoms of HELLP Syndrome
The signs and symptoms of HELLP syndrome can be quite variable and sometimes mimic other conditions, making early recognition crucial. While the classic triad of Hemolysis, Elevated Liver enzymes, and Low Platelets is the defining characteristic, the clinical presentation can be subtle or rapidly progressive.
Common Symptoms
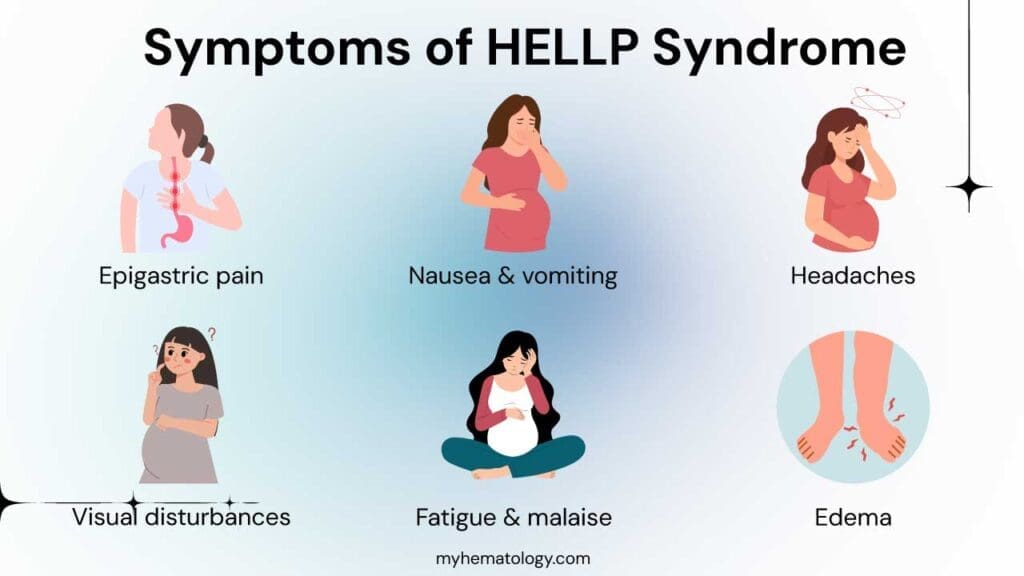
- Right Upper Quadrant (RUQ) or Epigastric Pain (around the upper middle abdomen): This is often the most prominent and characteristic symptom. It can range from mild discomfort to severe, continuous pain. The pain is typically located under the ribs on the right side, where the liver is situated, or in the upper central abdomen. It can sometimes be mistaken for heartburn, indigestion, or gallbladder issues.
- Nausea and Vomiting: These gastrointestinal symptoms are very common and can be severe. They may be persistent and not relieved by typical remedies for morning sickness, especially if occurring in the late second or third trimester.
- Headache: Headaches can range from mild to severe and may be persistent. They can be similar to tension headaches or migraines and might not always be accompanied by visual disturbances as seen in eclampsia.
- Visual Disturbances: These can include blurred vision, flashing lights (scintillating scotoma), temporary loss of vision, or sensitivity to light (photophobia). These symptoms are more commonly associated with preeclampsia but can also occur in HELLP syndrome.
- General Malaise and Fatigue: Many women with HELLP syndrome report feeling unusually tired, weak, or generally unwell. This fatigue can be significant and out of proportion to the usual tiredness of late pregnancy.
- Swelling (Edema): While edema (swelling, particularly in the legs, ankles, and face) is a common symptom of preeclampsia, it may be less pronounced or even absent in some cases of HELLP syndrome, especially in “atypical HELLP.”
Less Common or Atypical Symptoms
- Shoulder Pain: This can occur due to diaphragmatic irritation from liver swelling or bleeding. The pain may radiate to the neck or shoulder.
- Jaundice: Yellowing of the skin and whites of the eyes (jaundice) is relatively rare in HELLP syndrome but can occur in severe cases of liver dysfunction.
- Hypertension: While HELLP syndrome is often associated with preeclampsia and hypertension, a significant portion of women (up to 15-20%) may have normal or only mildly elevated blood pressure (“normotensive HELLP”). This can make diagnosis more challenging.
- Proteinuria: Similarly, while protein in the urine is a hallmark of preeclampsia, it may be absent or less significant in some cases of HELLP syndrome.
- Flu-like Symptoms: Some women may initially experience vague flu-like symptoms such as malaise, fatigue, and general aches before the more specific symptoms of HELLP develop.
Importance of Recognizing Subtle Signs
It is crucial for medical professionals and pregnant women to be aware that HELLP syndrome can develop rapidly and may not always present with the classic triad of hypertension, proteinuria, and RUQ pain. Any pregnant or postpartum woman presenting with persistent RUQ or epigastric pain, severe nausea and vomiting, headache, visual changes, or unusual fatigue, especially in the late second or third trimester, should be evaluated for HELLP syndrome, even if their blood pressure is not significantly elevated and proteinuria is absent.
When to Suspect HELLP Syndrome
- Late second or third trimester of pregnancy.
- Postpartum period (usually within 48 hours, but can occur up to a week or more after delivery).
- Women with known preeclampsia or gestational hypertension who develop worsening symptoms.
- Women with the characteristic symptoms mentioned above, even without significant hypertension or proteinuria.
Laboratory Investigations in HELLP Syndrome
Laboratory investigations are crucial for confirming the clinical suspicion of HELLP syndrome and assessing its severity. These tests focus on identifying the hallmark features of the syndrome: Hemolysis, ELevated Liver enzymes, and LP Low Platelet count.
Hematological Tests (to assess Hemolysis and Platelet Count)
- Complete Blood Count (CBC) with Peripheral Blood Smear
- Hemoglobin and Hematocrit: May be normal initially, but a falling trend or levels below the normal range for pregnancy can indicate hemolysis. Severe anemia (hemoglobin < 8-10 g/dL, depending on gestational age) unrelated to blood loss is a significant finding.
- Platelet Count: This is a cornerstone of the diagnosis. A platelet count < 100,000 /µL is diagnostic for HELLP syndrome.
- Examination of the blood smear: Can reveal schistocytes (fragmented red blood cells), which are a characteristic finding of microangiopathic hemolysis, a key component of HELLP.
- Lactate Dehydrogenase (LDH): LDH is an enzyme found in many tissues, including red blood cells and the liver. Elevated LDH levels (≥ 600 IU/L, although some definitions use higher thresholds) indicate tissue damage, particularly the breakdown of red blood cells (hemolysis).
- Total and Indirect (Unconjugated) Bilirubin: Elevated bilirubin levels, particularly the indirect fraction, can result from the increased breakdown of red blood cells. A total bilirubin level ≥ 1.2 mg/dL is often used as a criterion for hemolysis in HELLP syndrome.
- Haptoglobin: Haptoglobin is a protein that binds free hemoglobin released during hemolysis. In HELLP syndrome, haptoglobin levels are typically low (< 25 mg/dL) due to increased consumption as it binds to the released hemoglobin. However, this test is not always readily available.
Liver Function Tests (LFTs) (to assess Elevated Liver Enzymes)
- Aspartate Aminotransferase (AST): AST is an enzyme found in the liver and other tissues. Elevated AST levels (≥ 70 IU/L, although some definitions use ≥ 40 IU/L for milder cases) indicate hepatocellular injury or damage.
- Alanine Aminotransferase (ALT): ALT is another liver enzyme that is more specific to the liver than AST. Elevated ALT levels (≥ 70 IU/L, with similar considerations for milder cases) also point towards liver cell damage. AST levels are often higher than ALT levels in HELLP syndrome.
- Alkaline Phosphatase (ALP): ALP is another liver enzyme, but its elevation is less specific to HELLP syndrome and can be elevated in normal pregnancy. While it might be mildly elevated, it’s not a primary diagnostic criterion for HELLP.
Coagulation Studies (to assess for Disseminated Intravascular Coagulation (DIC))
While HELLP syndrome itself is not primarily a coagulopathy, severe cases can sometimes be complicated by DIC. Therefore, coagulation studies may be performed to assess for this complication.
- Prothrombin Time (PT) and Activated Partial Thromboplastin Time (aPTT): These are usually normal or only mildly prolonged in HELLP syndrome. Significant prolongation suggests DIC.
- Fibrinogen: In DIC, fibrinogen levels can be low due to consumption.
- D-dimer: D-dimer is a marker of fibrinolysis (breakdown of blood clots). It is often elevated in HELLP syndrome and significantly elevated in DIC.
Renal Function Tests (to assess for associated kidney involvement)
While not part of the core HELLP criteria, kidney function can be affected, especially in the context of co-existing preeclampsia or severe disease.
- Serum Creatinine and Blood Urea Nitrogen (BUN): Elevated levels indicate impaired kidney function.
- Uric Acid: Often elevated in preeclampsia and may be elevated in HELLP syndrome.
Urinalysis (to assess for Proteinuria)
While not a diagnostic criterion for HELLP syndrome itself, proteinuria (protein in the urine) is a hallmark of preeclampsia. Its presence or absence can help in classifying the hypertensive disorder of pregnancy.
Mississippi Classification of HELLP Syndrome
The diagnosis of HELLP syndrome relies on a combination of clinical presentation and specific laboratory findings. While there isn’t a single universally accepted set of criteria, the Mississippi classification is a commonly used system to categorize the severity of HELLP syndrome based on platelet count and liver enzyme levels.
This system divides HELLP syndrome into three classes based on the lowest (nadir) platelet count achieved.
- Class 1 (Severe)
- Platelet count: ≤ 50,000 /µL
- Aspartate Aminotransferase (AST) or Alanine Aminotransferase (ALT): ≥ 70 IU/L
- Lactate Dehydrogenase (LDH): ≥ 600 IU/L (indicating hemolysis)
- Class 2 (Moderate)
- Platelet count: > 50,000 to ≤ 100,000 /µL
- AST or ALT: ≥ 70 IU/L
- LDH: ≥ 600 IU/L
- Class 3 (Mild)
- Platelet count: > 100,000 to ≤ 150,000 /µL
- AST or ALT: ≥ 40 IU/L
- LDH: ≥ 600 IU/L
Key Points about the Mississippi Classification
- Severity Grading: This classification helps to stratify the severity of HELLP syndrome, with Class 1 generally associated with higher maternal morbidity and a longer recovery time.
- Prognostic Value: It can provide some prognostic information regarding the risk of complications.
- Platelet Count Focus: The primary differentiating factor between the classes is the platelet count.
- Other Laboratory Findings: While the classification emphasizes platelet count and liver enzymes, evidence of hemolysis (elevated LDH, abnormal peripheral smear showing schistocytes, elevated bilirubin, low haptoglobin) is crucial for the diagnosis of HELLP syndrome across all classes.
Differential Diagnosis
Several other conditions can present with overlapping signs and symptoms, making accurate and timely differentiation crucial for appropriate management.
| Differential Diagnosis | Key Similarities with HELLP | Key Differentiating Features |
| Acute Fatty Liver of Pregnancy (AFLP) | Late pregnancy onset, RUQ pain, nausea/vomiting, elevated liver enzymes, possible thrombocytopenia. | Pronounced jaundice, hypoglycemia, hyperammonemia, more significant coagulation abnormalities, less prominent hemolysis (lower LDH, fewer schistocytes), liver biopsy findings (microvesicular steatosis). |
| Thrombotic Thrombocytopenic Purpura (TTP) | Thrombocytopenia, microangiopathic hemolysis. | More prominent neurological abnormalities, often more severe renal impairment, fever, less marked liver enzyme elevation, severely reduced ADAMTS13 activity. |
| Hemolytic Uremic Syndrome (HUS) | Thrombocytopenia, microangiopathic hemolysis, possible renal involvement. | More prominent and often severe acute kidney injury, neurological abnormalities less consistent than TTP, typically occurs postpartum or associated with diarrheal illness (typical HUS). |
| Viral Hepatitis | Nausea/vomiting, RUQ pain, elevated liver enzymes, possible jaundice. | Lack of significant thrombocytopenia and hemolysis, positive viral serology, clinical context of viral exposure. |
| Gallbladder Disease | RUQ pain, nausea/vomiting. | Usually normal platelet count and LDH, less marked elevation in liver enzymes (ALP and bilirubin may be more elevated if obstruction), diagnosis often confirmed by abdominal ultrasound. |
| Pyelonephritis | Right flank/abdominal pain, nausea/vomiting. | Fever, urinary symptoms (dysuria, frequency), usually normal platelet count and liver enzymes, pyuria and bacteriuria on urine analysis, flank tenderness. |
| Systemic Lupus Erythematosus (SLE) Flare | Can involve hypertension, thrombocytopenia, liver abnormalities. | History of SLE, other systemic symptoms (rash, joint pain), positive autoimmune markers (ANA, specific antibodies), hemolysis may be present but microangiopathic hemolysis less typical. |
| Immune thrombocytopenia (ITP) | Thrombocytopenia. | Isolated thrombocytopenia without significant hemolysis or elevated liver enzymes, often occurs without other systemic symptoms or hypertension. |
Treatment and Management of HELLP Syndrome
The treatment and management of HELLP syndrome are complex and require a multidisciplinary approach involving obstetricians, maternal-fetal medicine specialists, anesthesiologists, hematologists, and neonatologists. The primary goal is to stabilize the mother and deliver the fetus and placenta, which is the only definitive cure for HELLP syndrome.
Immediate Goals
- Maternal Stabilization: Address acute complications and stabilize the mother’s condition. This includes managing hypertension, preventing seizures, correcting coagulation abnormalities, and optimizing fluid balance.
- Fetal Assessment: Continuously monitor fetal well-being to assess for any signs of distress.
- Definitive Treatment: Delivery of the fetus and placenta is the ultimate treatment to halt the progression of HELLP syndrome.
Maternal Stabilization Measures
- Antihypertensive Medications: Prompt control of severe hypertension (systolic blood pressure ≥ 160 mmHg or diastolic blood pressure ≥ 110 mmHg) is crucial to prevent maternal complications like stroke or placental abruption. Commonly used intravenous antihypertensive agents include labetalol, hydralazine, and nicardipine. Oral agents like nifedipine may be used for less severe hypertension. Blood pressure should be monitored frequently and titrated to maintain levels within a safe range.
- Magnesium Sulfate: Magnesium sulfate is the anticonvulsant of choice for preventing and treating eclamptic seizures. It is typically administered intravenously as a loading dose followed by a maintenance infusion. Even in the absence of overt seizures, magnesium sulfate is often given to women with HELLP syndrome due to the increased risk of eclampsia. Close monitoring for magnesium toxicity (e.g., loss of deep tendon reflexes, respiratory depression, decreased urine output) is essential.
- Fluid Management: Careful monitoring of fluid intake and output is crucial. Women with HELLP syndrome can be at risk for both fluid overload (leading to pulmonary edema) and hypovolemia (due to endothelial dysfunction and third-spacing of fluids). Intravenous fluids should be administered judiciously, often with crystalloids. Albumin may be considered in cases of severe hypoproteinemia.
- Blood Product Transfusion
- Platelet Transfusion: Indicated for very low platelet counts (< 20,000/µL), before cesarean delivery (typically aim for > 50,000/µL), or before other invasive procedures. The goal is to reduce the risk of bleeding.
- Packed Red Blood Cells (PRBCs): Transfused if there is significant anemia due to hemolysis or blood loss.
- Fresh Frozen Plasma (FFP) and Cryoprecipitate: May be considered if there are significant coagulation abnormalities or low fibrinogen levels, especially in the context of DIC (Disseminated Intravascular Coagulation).
- Corticosteroids for Fetal Lung Maturity: If the gestational age is less than 34 weeks and delivery can be safely delayed for at least 24-48 hours, a course of corticosteroids (betamethasone or dexamethasone) is typically administered to accelerate fetal lung maturation and reduce the risk of neonatal respiratory distress syndrome.
Fetal Considerations
If preterm delivery is anticipated, tests like amniocentesis for lecithin/sphingomyelin (L/S) ratio or lamellar body count may be considered if time allows. However, in many cases of HELLP, the need for prompt delivery outweighs the benefit of these tests.
- Consideration of Fetal Transfer: If the mother is in a hospital without adequate neonatal intensive care facilities for a preterm infant, transfer to a center with higher-level care may be necessary before delivery if the maternal condition allows for safe transfer.
Delivery
The only definitive treatment for HELLP syndrome is the delivery of the fetus and placenta. Once the placenta is removed, the maternal condition usually begins to improve, although this can take several days.
- Timing of Delivery: The decision on when to deliver depends on several factors, including:
- Gestational Age: Generally, if the gestational age is ≥ 34 weeks, delivery is usually recommended without delay after maternal stabilization.
- Maternal and Fetal Condition: In pregnancies < 34 weeks, if the maternal and/or fetal condition is unstable or deteriorating despite intensive management, immediate delivery is indicated regardless of fetal lung maturity. If the condition is stable, a 24-48 hour course of corticosteroids for fetal lung maturity may be considered before delivery.
- Severity of HELLP Syndrome: More severe classes of HELLP (Mississippi Class 1 and 2) often warrant earlier delivery.
- Route of Delivery
- Cesarean Section: Often necessary, especially for preterm deliveries, in cases of fetal distress, or if rapid delivery is required for maternal stabilization.
- Vaginal Delivery: May be considered in some stable term or near-term pregnancies, particularly if the cervix is favorable and there are no contraindications. However, this requires close monitoring and may not always be feasible.
Postpartum Management
- Close Monitoring: The mother needs close monitoring in the postpartum period, typically in an intensive care unit, for at least 24-48 hours or until her condition stabilizes and laboratory values begin to improve. This includes:
- Frequent blood pressure monitoring.
- Monitoring of urine output.
- Serial monitoring of laboratory values (platelet count, liver enzymes, LDH, bilirubin, renal function).
- Assessment for postpartum complications.
- Continuation of Magnesium Sulfate: Magnesium sulfate infusion is usually continued for 24 hours postpartum for seizure prophylaxis, even if the mother did not have seizures antepartum.
- Pain Management: Adequate pain relief is important.
- Monitoring and Management of Postpartum Complications: Be vigilant for complications such as:
- Disseminated Intravascular Coagulation (DIC).
- Acute Kidney Injury.
- Pulmonary Edema.
- Hepatic Hematoma or Rupture (rare but life-threatening).
- Postpartum Eclampsia.
- Infection.
- Postpartum Follow-up: Women who have had HELLP syndrome should have close postpartum follow-up to monitor their recovery and assess for any long-term sequelae, such as hypertension or cardiovascular disease.
Potential Complications of HELLP Syndrome
HELLP syndrome is a severe condition that carries significant risks for both the mother and the fetus. The complications can arise rapidly and can be life-threatening if not recognized and managed promptly.
Maternal Complications
- Eclampsia and Seizures: Women with HELLP syndrome are at an increased risk of developing eclampsia, characterized by seizures that are not attributable to other causes. This is a neurological emergency and can lead to hypoxia, aspiration, and maternal death.
- Disseminated Intravascular Coagulation (DIC): This is a serious condition where the body’s clotting system becomes overactive, leading to the formation of small blood clots throughout the vasculature. This can deplete clotting factors and platelets, paradoxically increasing the risk of severe bleeding from various sites (e.g., placenta, surgical wounds, IV sites).
- Acute Kidney Injury (AKI): Reduced blood flow to the kidneys due to vasospasm and endothelial dysfunction can lead to impaired kidney function, ranging from mild elevation in creatinine to severe AKI requiring dialysis.
- Pulmonary Edema: Fluid overload, capillary leak syndrome (due to endothelial damage), and impaired kidney function can contribute to fluid accumulation in the lungs, leading to shortness of breath and hypoxia.
- Placental Abruption: The sudden separation of the placenta from the uterine wall before delivery can occur more frequently in women with HELLP syndrome. This can lead to severe maternal hemorrhage and fetal distress or demise.
- Hepatic Hematoma or Rupture: Liver damage in HELLP syndrome can sometimes lead to the formation of a hematoma (collection of blood) within the liver tissue. In rare but catastrophic cases, this hematoma can rupture, causing massive intra-abdominal hemorrhage and requiring emergency surgery.
- Stroke (Cerebrovascular Accident): Severe hypertension associated with HELLP can increase the risk of both ischemic and hemorrhagic strokes. Endothelial dysfunction might also contribute to vascular fragility. A recent search did not show a direct link between endothelial dysfunction and increased risk of hemorrhagic stroke in the general population, but in the context of HELLP with severe hypertension, this risk is plausible.
- Maternal Death: Although less common with timely and appropriate management, HELLP syndrome remains a significant cause of maternal morbidity and mortality due to the potential for these severe complications.
- Adult Respiratory Distress Syndrome (ARDS): A severe form of lung injury characterized by widespread inflammation and fluid buildup in the alveoli, leading to severe breathing difficulties.
- Aspiration Pneumonia: Vomiting, especially during a seizure, can lead to aspiration of stomach contents into the lungs, causing pneumonia.
- Blood Transfusion Reactions: Although rare, complications can arise from blood product transfusions required to manage anemia or thrombocytopenia.
Fetal and Neonatal Complications
Fetal and neonatal complications are primarily related to prematurity (often a consequence of the need for early delivery) and the intrauterine environment created by HELLP syndrome:
- Preterm Birth: Delivery is often necessary before term to save the mother’s life or prevent further deterioration. Prematurity is associated with numerous complications affecting all organ systems, including respiratory distress syndrome (RDS), necrotizing enterocolitis (NEC), intraventricular hemorrhage (IVH), and retinopathy of prematurity (ROP).
- Intrauterine Growth Restriction (IUGR): The placental dysfunction associated with preeclampsia and HELLP can impair fetal growth, leading to a baby that is smaller than expected for gestational age.
- Fetal Distress: The compromised placental function can lead to inadequate oxygen and nutrient supply to the fetus, resulting in fetal distress, which may necessitate emergency delivery.
- Oligohydramnios: Reduced amniotic fluid volume, which can be associated with placental insufficiency.
- Stillbirth: In severe and unmanaged cases, HELLP syndrome can lead to fetal demise in utero.
- Neonatal Morbidity Associated with Prematurity: Even if the baby survives, prematurity can lead to long-term neurodevelopmental disabilities and other health issues.
Long-Term Maternal Outcomes
Women who have experienced HELLP syndrome have an increased risk of:
- Recurrence in Subsequent Pregnancies: The risk of HELLP or preeclampsia in future pregnancies is significantly higher.
- Chronic Hypertension: HELLP syndrome can sometimes lead to the development of chronic hypertension.
- Cardiovascular Disease: Some studies suggest a long-term increased risk of cardiovascular events.
- Metabolic Syndrome and Diabetes: There may be an increased risk of developing these conditions later in life.
Frequently Asked Questions (FAQs)
What is the difference between HELLP and eclampsia?
HELLP syndrome is a severe pregnancy complication defined by hemolysis, elevated liver enzymes, and low platelet count, often occurring with preeclampsia but characterized by significant liver and blood abnormalities. Eclampsia, on the other hand, is the occurrence of seizures or coma in a woman with preeclampsia, representing a neurological emergency due to the seizures themselves. While both are serious and can coexist, HELLP is primarily diagnosed through specific laboratory findings indicating liver and blood damage, whereas eclampsia is defined by the presence of seizures in the context of preeclampsia.
Summary of key differences
| Feature | HELLP Syndrome | Eclampsia |
| Primary Finding | Hemolysis, Elevated Liver Enzymes, Low Platelets | Seizures or Coma |
| Hypertension | May or may not be present (often associated) | Typically present (pre-eclampsia) |
| Proteinuria | May or may not be present (often associated) | Often present (pre-eclampsia) |
| Key Symptoms | RUQ pain, nausea/vomiting, malaise, headache | Seizures, severe headache, visual disturbances, altered mental status |
| Main Danger | Liver hemorrhage/rupture, bleeding due to low platelets | Seizures, neurological complications, maternal death |
| Relationship to Preeclampsia | Often considered a severe variant of preeclampsia | A severe complication of preeclampsia |
| Diagnosis | Primarily based on specific laboratory findings | Based on the occurrence of seizures in the context of preeclampsia |
What does HELLP syndrome pain feel like?
HELLP syndrome pain is most commonly felt as right upper quadrant (RUQ) pain, located under the ribs on the right side of the abdomen where the liver is. It can also be experienced as epigastric pain, which is in the upper middle part of the abdomen, often described as being “below the breastbone.”
The pain can vary in intensity from mild discomfort or tenderness to severe, continuous, and even sharp pain. Some women describe it as feeling like severe indigestion, heartburn, or a dull ache. It can sometimes radiate to the back or right shoulder.
What are the symptoms of low platelets in pregnancy?
While many pregnant women with low platelets (thrombocytopenia) may not experience any noticeable symptoms, especially in mild cases, some may develop signs related to an impaired ability to form blood clots. These symptoms can include easy or excessive bruising (purpura), superficial bleeding into the skin appearing as tiny reddish-purple spots (petechiae), often on the lower legs, prolonged bleeding from cuts, bleeding gums or nosebleeds, blood in the urine or stools, and unusually heavy menstrual flows (if occurring during or before pregnancy).
Is BP high in HELLP syndrome?
While HELLP syndrome is often associated with high blood pressure (hypertension), it’s important to know that blood pressure may not always be elevated in women with HELLP syndrome.
In fact, up to 15-20% of patients with HELLP syndrome do not have elevated blood pressure that meets the diagnostic criteria for preeclampsia (typically 140/90 mmHg or higher). This is sometimes referred to as “normotensive HELLP.”
Therefore, while hypertension is a common finding and HELLP is often considered a severe form of preeclampsia, the absence of high blood pressure does not rule out HELLP syndrome. The diagnosis relies on the characteristic laboratory findings of hemolysis, elevated liver enzymes, and low platelet count, along with the clinical presentation.
Why do platelets drop in HELLP syndrome?
The drop in platelets in HELLP syndrome (thrombocytopenia) is primarily due to increased consumption of platelets as they are activated and adhere to the damaged vascular endothelial cells lining the blood vessels. This widespread endothelial damage, a key feature of HELLP, triggers the activation of the coagulation cascade. Platelets are recruited to these damaged sites, leading to their aggregation and the formation of microthrombi (small blood clots) in the microvasculature, particularly in the liver. This increased utilization of platelets results in a lower circulating platelet count and a shortened platelet lifespan due to increased turnover.
Why is HELLP syndrome life threatening?
HELLP syndrome is life-threatening due to the potential for rapid progression and severe complications affecting multiple organ systems in both the mother and the baby. For the mother, the risks include liver hemorrhage or rupture, disseminated intravascular coagulation (DIC) leading to severe bleeding, acute kidney injury, pulmonary edema, placental abruption, stroke, and even death. For the baby, the main threats are premature birth (often necessitating early delivery to save the mother), intrauterine growth restriction, fetal distress due to placental insufficiency, and stillbirth. The combination of these potentially devastating complications underscores the critical need for prompt diagnosis and management of HELLP syndrome.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Jenkins J, Ferozuddin AA, Mourad J, Abdulla ZZ, Oviedo A. Incongruence of Hemolysis, Elevated Liver Enzyme, Low-Platelet Count Syndrome (HELLP) and Preeclampsia Criteria in Pregnancy: Implications for Medical Education and Obstetrics Training. Cureus. 2024 Aug 19;16(8):e67211. doi: 10.7759/cureus.67211. PMID: 39295684; PMCID: PMC11410063.
- Patel PB, Patel N, Hedges MA, Benson AE, Tomer A, Lo JO, Shatzel JJ. Hematologic Complications of Pregnancy. Eur J Haematol. 2025 Apr;114(4):596-614. doi: 10.1111/ejh.14372. Epub 2025 Jan 10. PMID: 39790057; PMCID: PMC11882378.
- Wallace K, Harris S, Addison A, Bean C. HELLP Syndrome: Pathophysiology and Current Therapies. Curr Pharm Biotechnol. 2018;19(10):816-826. doi: 10.2174/1389201019666180712115215. PMID: 29998801.
- Jiang Y, Chen LJ, Hu HH, Jin N, Lv SR, Fang C, Zhu CM, Yang MM, Xu D, Luo Q. Development a nomogram for predicting HELLP syndrome in women complicated with gestational hypertension. BMC Pregnancy Childbirth. 2025 Apr 10;25(1):418. doi: 10.1186/s12884-025-07546-8. PMID: 40211174; PMCID: PMC11987297.
- Nicolls S, Wang LQ, Koegl J, Lyons J, Van Schalkwyk J, Joseph KS, Lisonkova S. Twin Birth and Hemolysis, Elevated Liver Enzymes, and Low Platelets (HELLP) Syndrome: A Population-Based Study. J Obstet Gynaecol Can. 2025 Apr;47(4):102792. doi: 10.1016/j.jogc.2025.102792. Epub 2025 Feb 18. PMID: 39978767.




