TL;DR
Sjögren’s syndrome is a systemic autoimmune disease primarily targeting exocrine glands (dry eyes, mouth).
- Pathophysiology ▾: Lymphocytic infiltration, autoantibody production (anti-Ro/SSA, anti-La/SSB), genetic predisposition, and potential environmental triggers.
- Causes/Risk Factors ▾: Autoimmune dysfunction, genetics, female sex, age, other autoimmune diseases.
- Symptoms ▾: Dry eyes/mouth, joint pain, fatigue, potential systemic involvement (lungs, kidneys, nerves).
- Diagnosis ▾: Autoantibody tests, ocular/salivary tests, biopsy (focus score).
- Differential Diagnosis ▾: Dry eye syndrome, other autoimmune diseases, infections, lymphoma.
- Treatment ▾: Symptom relief (artificial tears, sialogogues), systemic therapies (hydroxychloroquine, immunosuppressants), and management of complications.
- Prognosis ▾: Chronic, variable; early diagnosis and management improve outcomes.
*Click ▾ for more information
Introduction
Sjögren’s syndrome is a systemic autoimmune disease characterized primarily by the immune system’s attack on the body’s moisture-producing glands, most notably the lacrimal and salivary glands, leading to dry eyes (xerophthalmia) and dry mouth (xerostomia). While these are the hallmark symptoms, Sjögren’s syndrome can also affect other parts of the body, causing a range of systemic manifestations, including joint pain, fatigue, and organ involvement.
Types of Sjögren’s Syndrome
- Primary Sjögren’s Syndrome: This form occurs independently, meaning it is not associated with any other underlying autoimmune disease. It is a standalone condition where the immune system primarily targets the exocrine glands.
- Secondary Sjögren’s Syndrome: In these cases, Sjögren’s syndrome is considered a secondary manifestation of the primary autoimmune disorder. This form develops in conjunction with another autoimmune disease, such as:
- Rheumatoid arthritis
- Systemic lupus erythematosus (SLE)
- Scleroderma
Impact on Patient Quality of Life
Sjögren’s syndrome, whether primary or secondary, can significantly diminish a patient’s quality of life. The constant dryness of the eyes and mouth can lead to:
- Physical Discomfort
- Eye irritation, pain, and potential corneal damage.
- Difficulty swallowing, speaking, and tasting food.
- Increased risk of dental caries and oral infections.
- Emotional Distress
- Chronic fatigue and pain can lead to depression and anxiety.
- Social limitations due to discomfort and symptoms.
- Functional Limitations
- Difficulty performing daily activities, such as reading, working, and socializing.
- Impact on dietary habits due to difficulty eating dry foods.
- Systemic complications
- When systemic manifestations occur, such as lung, kidney, or nerve involvement, quality of life can be further degraded.
It’s important to recognize that even “mild” cases of Sjögren’s can have a substantial impact on a person’s well-being. Therefore, comprehensive management that addresses both the glandular and systemic manifestations is essential.
Pathophysiology of Sjögren’s
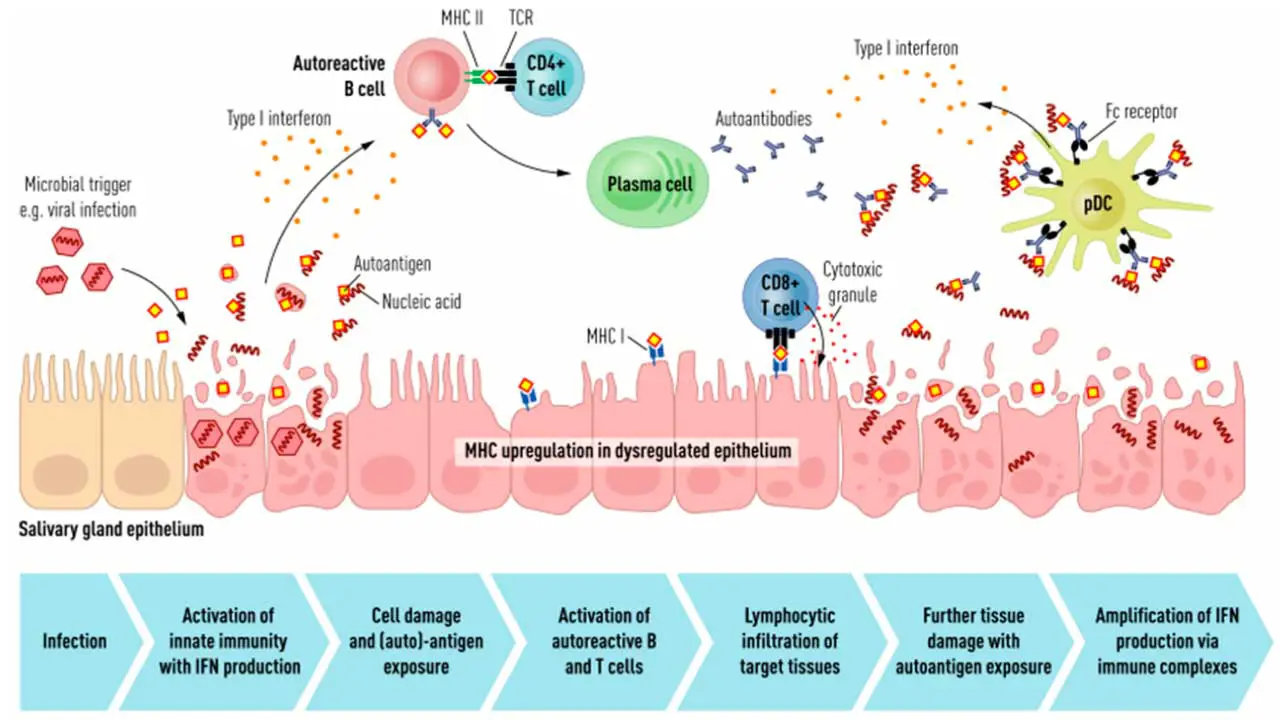
The core of Sjögren’s syndrome lies in a complex interplay of immune dysregulation, genetic susceptibility, and potentially environmental triggers, leading to the characteristic inflammation and destruction of exocrine glands.
Autoimmune Basis
- Lymphocytic Infiltration: The hallmark of Sjögren’s is the infiltration of lymphocytes (primarily T and B cells) into the exocrine glands, particularly the salivary and lacrimal glands. This infiltration leads to inflammation and progressive glandular damage, ultimately resulting in reduced secretion.
- T Cell-Mediated Damage: CD4+ T cells play a significant role in initiating and perpetuating the inflammatory process. These T cells release cytokines, such as interferon-gamma (IFN-γ) and interleukin-17 (IL-17), which contribute to the inflammatory cascade and glandular epithelial cell apoptosis (programmed cell death). Relating to the information provided previously, dendritic cells present antigens to the T cells, starting the activation process.
- B Cell Involvement and Autoantibody Production: B cells are also crucial, contributing to the formation of lymphoid follicles within the glands. They produce autoantibodies, most notably anti-Ro/SSA and anti-La/SSB, which are characteristic of Sjögren’s syndrome. While the exact pathogenic role of these autoantibodies is still debated, they are valuable diagnostic markers. B cells can also contribute to inflammation through cytokine production.
- Glandular Epithelial Cell Apoptosis: The inflammatory process leads to the destruction of glandular epithelial cells, further reducing secretory function. This apoptosis is mediated by various factors, including cytokines and Fas-FasL interactions.
Genetic Predisposition
- HLA Genes: A strong association exists between Sjögren’s syndrome and certain human leukocyte antigen (HLA) genes, particularly HLA-DRB1. Specific HLA alleles may influence the presentation of autoantigens and the activation of autoreactive T cells. These genetic factors contribute to an individual’s susceptibility to developing the disease.
- Non-HLA Genes: In addition to HLA genes, other genes involved in immune regulation may also contribute to Sjögren’s susceptibility. These genes may affect various aspects of the immune response, such as cytokine production, T cell activation, and B cell function.
Environmental Triggers
It is believed that genetic predisposition alone is not sufficient to cause Sjögren’s syndrome. Environmental factors, such as viral infections, may act as triggers in genetically susceptible individuals. Epigenetic modifications may also play a role.
- Epstein-Barr Virus (EBV): EBV is a common virus that has been implicated in several autoimmune diseases, including Sjögren’s syndrome. It’s hypothesized that EBV may trigger an abnormal immune response in genetically susceptible individuals.
- Other Viruses: Other viruses, such as hepatitis C virus (HCV), human T-cell lymphotropic virus type 1 (HTLV-1), and certain herpesviruses, have also been investigated as potential triggers. The idea is that viral infections can disrupt immune regulation, leading to autoimmunity.
Risk Factors of Secondary Sjögren’s Syndrome
- Sex: Being female is the most significant risk factor. The disease disproportionately affects women.
- Age: While it can occur at any age, it’s most frequently diagnosed in people over 40.
- Preexisting Autoimmune Diseases: Having another autoimmune disorder, such as rheumatoid arthritis, lupus, or scleroderma, increases the risk of developing secondary Sjögren’s syndrome.
- Genetic Predisposition: A family history of Sjögren’s syndrome or other autoimmune diseases, as well as specific HLA gene variations, increases susceptibility.
- Hormonal Factors: The strong female predominance suggests hormonal influences, though the precise mechanisms are unclear.
- Potential Environmental Triggers: While not definitively proven, viral infections like Epstein-Barr virus (EBV) and certain environmental exposures are being investigated as potential triggers.
Clinical Manifestations

Sjögren’s syndrome presents with a wide range of clinical manifestations, affecting both exocrine glands and various systemic organs.
Classic Glandular Manifestations
- Xerophthalmia (Dry Eyes): Patients experience a gritty, sandy, or burning sensation in the eyes. They may have difficulty wearing contact lenses. Reduced tear production can lead to corneal abrasions, keratitis, and even corneal ulceration in severe cases. Light sensitivity (photophobia) is also common.
- Xerostomia (Dry Mouth): Patients complain of a dry, sticky feeling in the mouth. There is difficulty in swallowing dry foods, speaking for prolonged periods, and tasting food. Patients experience Increased risk of dental caries, oral candidiasis (thrush), and parotid gland enlargement. Cracked lips and oral fissures are common too.
Systemic (Extraglandular) Manifestations
- Musculoskeletal: Arthralgia (joint pain) and arthritis, often affecting the small joints of the hands and feet with myalgia (muscle pain) and fatigue.
- Respiratory: Dryness of the respiratory tract, leading to chronic cough and bronchitis. Interstitial lung disease (ILD) in some cases.
- Gastrointestinal: Dysphagia (difficulty swallowing) due to dry mouth and esophageal dysmotility. Also gastritis and other digestive issues.
- Renal: Interstitial nephritis, which can lead to renal tubular acidosis.
- Neurological: Peripheral neuropathy, causing numbness, tingling, and pain in the extremities and trigeminal neuropathy (pain in the face). In rare instances, central nervous system involvement may occur.
- Vascular: Raynaud’s phenomenon, causing color changes in the fingers and toes in response to cold or stress and vasculitis, which can affect various organs.
- Skin: Dry skin (xerosis) and purpura (small purple spots) due to vasculitis.
- Lymphatic System: Increased risk of lymphoma, particularly non-Hodgkin’s lymphoma.
- General Symptoms: Profound fatigue is a very common and often debilitating symptom. Fever can occur, especially with systemic involvement.
Laboratory Investigations
Diagnosing Sjögren’s syndrome involves a combination of clinical evaluation and laboratory investigations.
Autoantibody Testing
- Anti-Ro/SSA and Anti-La/SSB: These are the most characteristic autoantibodies associated with Sjögren’s syndrome. Their presence is a significant indicator of the disease. However, they are not always present, and their absence does not rule out Sjögren’s.
- Rheumatoid Factor (RF): RF is often positive in Sjögren’s syndrome, particularly in those with secondary Sjögren’s associated with rheumatoid arthritis. It’s not specific to Sjögren’s.
- Antinuclear Antibodies (ANA): ANA is frequently positive in Sjögren’s syndrome, indicating an autoimmune process. The ANA test by itself, is not specific to Sjogren’s. Further testing such as ENA testing refines the diagnosis.
Ocular Tests
- Schirmer’s Test: Measures tear production by placing filter paper inside the lower eyelid. A low tear production result suggests dry eyes.
- Ocular Surface Staining: Uses dyes to identify damage to the cornea and conjunctiva caused by dryness.
- Tear Break-Up Time (TBUT): Evaluates the stability of the tear film.
Salivary Gland Assessment
- Salivary Flow Rate: Measures the amount of saliva produced over a specific time. Reduced salivary flow indicates dry mouth.
- Salivary Gland Biopsy: A minor salivary gland biopsy (usually from the lip) is performed to examine the presence and extent of lymphocytic infiltration.
- Focus score: To quantify the degree of lymphocytic infiltration, a key feature of Sjögren’s syndrome. The focus score represents the number of lymphocytic foci (clusters of ≥50 lymphocytes) per 4 mm² of salivary gland tissue. A focus score of ≥1 is generally considered a significant finding in the context of Sjögren’s syndrome.
| Interpretation | Clinical Significance |
| No significant lymphocytic foci. | May indicate absence of Sjögren’s-related sialadenitis. |
| One or more lymphocytic foci per 4 mm². | Suggests the presence of focal lymphocytic sialadenitis, consistent with Sjögren’s syndrome, when combined with other clinical and laboratory findings. |
- Sialography or Salivary Scintigraphy: Imaging techniques to assess salivary gland function.
Other Investigations
- Complete Blood Count (CBC): May reveal abnormalities such as leukopenia (low white blood cell count).
- Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP): These are inflammatory markers that may be elevated.
- Comprehensive Metabolic Panel (CMP): To assess kidney and liver function.
- Imaging studies: Chest X-ray or CT scans may be used to look for lung involvement.
Differential Diagnosis
When considering a diagnosis of Sjögren’s syndrome, it’s essential to differentiate it from other conditions that can mimic its symptoms.
Dry Eye and Dry Mouth Syndromes
- Age-related Dryness: Natural decline in tear and saliva production with age. This is distinguished by the absence of systemic symptoms and autoantibodies.
- Medication-induced Dryness: Many medications (e.g., antihistamines, antidepressants, diuretics) can cause dry eyes and mouth. A thorough medication history is crucial.
- Dry Eye Disease (Keratoconjunctivitis Sicca): Isolated dry eye without systemic involvement. It lacks the systemic features and autoantibodies of Sjögren’s.
Other Autoimmune Diseases
- Rheumatoid Arthritis (RA): RA can cause secondary Sjögren’s syndrome. It is distinguished by the pattern of joint involvement and specific RA-associated autoantibodies (e.g., anti-CCP).
- Systemic Lupus Erythematosus (SLE): SLE can also cause secondary Sjögren’s. It is distinguished by other SLE manifestations (e.g., rash, renal involvement, hematologic abnormalities) and specific SLE autoantibodies (e.g., anti-dsDNA).
- Sarcoidosis: Sarcoidosis can cause salivary gland enlargement and dry eyes. It is distinguished by pulmonary involvement, lymphadenopathy, and characteristic granulomas on biopsy.
- Scleroderma (Systemic Sclerosis): Scleroderma can cause dry mouth, and other overlap syndromes. It is distinguished by skin thickening, Raynaud’s phenomenon, and specific scleroderma autoantibodies.
Infections
- Hepatitis C Virus (HCV) Infection: HCV can cause salivary gland involvement and sicca symptoms. It is distinguished by positive HCV serology and liver function abnormalities.
- HIV Infection: HIV can cause salivary gland enlargement and dry mouth. It is distinguished by positive HIV serology.
Lymphoproliferative Disorders
- Lymphoma: Sjögren’s syndrome increases the risk of lymphoma. Salivary gland enlargement and lymphadenopathy can mimic lymphoma. Biopsy and imaging are essential for differentiation.
Other Conditions
- Diabetes Mellitus: Can cause dry mouth and other neurological symptoms. It is distinguished by hyperglycemia and other diabetes-related manifestations.
- Neurological Disorders: Certain neurological conditions can cause facial nerve dysfunction which can lead to dry eyes.
- Fibromyalgia: Fibromyalgia shares symptoms of fatigue and musculoskeletal pain. It lacks the glandular involvement and autoantibodies of Sjögren’s.
Treatment and Management
The treatment and management of Sjögren’s syndrome focus on alleviating symptoms, preventing complications, and addressing any systemic manifestations. Because Sjögren’s syndrome is a chronic condition, management is typically long-term and tailored to the individual patient’s needs.
Symptomatic Relief of Glandular Manifestations
- Dry Eyes (Xerophthalmia)
- Artificial tears and lubricating eye drops: These are the mainstay of treatment, providing moisture and relief.
- Ophthalmic ointments: Used at night for more prolonged lubrication.
- Punctal plugs: Small devices inserted into the tear ducts to block drainage and conserve tears.
- Cyclosporine or lifitegrast ophthalmic solutions: These prescription eye drops can help reduce inflammation and improve tear production.
- Dry Mouth (Xerostomia)
- Artificial saliva substitutes: Sprays, gels, or lozenges can provide temporary relief.
- Sialogogues (e.g., pilocarpine, cevimeline): Medications that stimulate saliva production.
- Good oral hygiene: Regular dental checkups, fluoride treatments, and meticulous oral care are essential to prevent dental caries and oral infections.
- Sugar-free chewing gum or candies: Can stimulate saliva flow.
- Frequent sips of water.
- Humidifiers: Increase moisture in the air.
Management of Systemic Manifestations
- Musculoskeletal Symptoms (Arthralgia/Arthritis)
- Nonsteroidal anti-inflammatory drugs (NSAIDs): For pain relief.
- Hydroxychloroquine: Can help reduce joint pain and fatigue.
- Methotrexate or other disease-modifying antirheumatic drugs (DMARDs): For more severe joint involvement.
- Fatigue
- Lifestyle modifications: Regular exercise, adequate sleep, and stress management.
- Hydroxychloroquine: May improve fatigue.
- Raynaud’s Phenomenon
- Avoidance of cold exposure.
- Calcium channel blockers: To improve blood flow.
- Interstitial Lung Disease (ILD):
- Corticosteroids.
- Immunosuppressants (e.g., azathioprine, mycophenolate mofetil).
- Renal Involvement
- Treatment of renal tubular acidosis.
- Corticosteroids or immunosuppressants in severe cases.
- Neurological Manifestations
- Medications for peripheral neuropathy (e.g., gabapentin, pregabalin).
- Corticosteroids or immunosuppressants for more severe neurological involvement.
- Vasculitis
- Corticosteroids.
- Immunosuppressants (e.g., cyclophosphamide, rituximab).
- Lymphoma Risk
- Regular monitoring for signs and symptoms of lymphoma.
- Prompt evaluation of any suspicious findings.
General Management and Lifestyle Modifications
- Hydration: Drink plenty of water throughout the day.
- Dietary Considerations: Avoid dry, spicy, or acidic foods that can irritate the mouth.
- Avoidance of Drying Medications: Review medications with a physician to identify and minimize the use of drugs that can cause dryness.
- Patient Education and Support: Provide information about the disease, management strategies, and available support groups.
- Regular Follow-up: Monitor disease activity and adjust treatment as needed.
Biologic Therapies
- In some cases of severe extraglandular involvement, biologic therapies such as rituximab may be used.
Prognosis
The prognosis for Sjögren’s syndrome varies depending on the severity of the disease and the extent of systemic involvement. While it’s a chronic condition, many individuals with Sjögren’s syndrome lead relatively normal lives with appropriate management.
General Prognosis
- Chronic but Stable: Sjögren’s syndrome is typically a chronic, slowly progressive disease. Many patients experience stable symptoms with periods of exacerbation and remission.
- Quality of Life: The primary impact is often on quality of life due to dry eyes and mouth, fatigue, and pain. Effective symptom management can significantly improve well-being.
- Systemic Involvement: The prognosis is more guarded in patients with significant systemic manifestations, such as interstitial lung disease, renal involvement, or vasculitis. These complications can lead to more serious health problems.
- Lymphoma Risk: Patients with Sjögren’s syndrome have an increased risk of developing lymphoma, particularly non-Hodgkin’s lymphoma. Regular monitoring is essential to detect any signs of lymphoma early.
Factors Affecting Prognosis
- Early Diagnosis and Treatment: Early diagnosis and management can help prevent complications and improve long-term outcomes.
- Severity of Glandular Involvement: The degree of dryness and glandular damage can impact quality of life.
- Presence of Systemic Manifestations: Systemic involvement, especially in major organs, can worsen the prognosis.
- Presence of certain autoantibodies: Some studies suggest that the presence of certain autoantibodies, and other biomarkers can help to predict which patients will develop systemic complications.
Long-Term Outlook
With proper management, most individuals with Sjögren’s syndrome can maintain a reasonable quality of life. Regular follow-up with a rheumatologist and other specialists is essential to monitor disease activity and adjust treatment as needed. Ongoing research is aimed at developing more effective therapies and improving the long-term outlook for patients with Sjögren’s syndrome.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- A. Björk, J. Mofors, M. Wahren-Herlenius., 2020, Journal of Internal Medicine, 287; 475–492.
- Seror R, Ravaud P, Mariette X, Bootsma H, Theander E, Hansen A, Ramos-Casals M, Dörner T, Bombardieri S, Hachulla E, Brun JG, Kruize AA, Praprotnik S, Tomsic M, Gottenberg JE, Devauchelle V, Devita S, Vollenweider C, Mandl T, Tzioufas A, Carsons S, Saraux A, Sutcliffe N, Vitali C, Bowman SJ; EULAR Sjögren’s Task Force. EULAR Sjogren’s Syndrome Patient Reported Index (ESSPRI): development of a consensus patient index for primary Sjogren’s syndrome. Ann Rheum Dis. 2011 Jun;70(6):968-72. doi: 10.1136/ard.2010.143743. Epub 2011 Feb 22. PMID: 21345815.
- Jonsson R. Disease mechanisms in Sjögren’s syndrome: What do we know? Scand J Immunol. 2022 Mar;95(3):e13145. doi: 10.1111/sji.13145. Epub 2022 Feb 1. PMID: 35073430.
- Bjordal O, Norheim KB, Rødahl E, Jonsson R, Omdal R. Primary Sjögren’s syndrome and the eye. Surv Ophthalmol. 2020 Mar-Apr;65(2):119-132. doi: 10.1016/j.survophthal.2019.10.004. Epub 2019 Oct 18. PMID: 31634487.




