TL;DR
Pernicious anemia is an autoimmune disease where the body attacks healthy stomach cells called parietal cells. This attack disrupts the production of intrinsic factor, a protein essential for vitamin B12 absorption.
Symptoms ▾: Fatigue, weakness, shortness of breath, tingling/numbness (especially in hands and feet), balance problems, cognitive decline, and glossitis (inflamed tongue).
Diagnosis ▾: Complete blood count (looking for macrocytosis, potential microcytosis, and pancytopenia), vitamin B12 level assessment, and sometimes additional tests like autoantibody markers and gastric investigations.
Treatment ▾: The primary treatment is vitamin B12 replacement therapy through injections (most effective), nasal spray, or oral tablets (depending on severity and individual needs).
Prognosis ▾: With early diagnosis and consistent treatment, the prognosis for pernicious anemia is generally good. Most people experience significant improvement in symptoms and maintain good health.
Other Important Points
- Pernicious anemia is associated with an increased risk of stomach cancer. Regular monitoring may be recommended.
- This condition can co-exist with other autoimmune diseases like type 1 diabetes or thyroiditis.
- A balanced diet remains important even with B12 replacement therapy.
Overall, pernicious anemia is a treatable condition. Early diagnosis and proper management ensure a good quality of life for individuals with this condition.
*Click ▾ for more information
Introduction
Pernicious anemia is an autoimmune disease where the body attacks the parietal cells found in the stomach lining. This attack cripples the production of intrinsic factor, a protein crucial for vitamin B12 absorption. The resulting B12 deficiency disrupts red blood cell production, leading to anemia. Additionally, B12 is vital for nervous system function, so the deficiency can also cause nerve damage and various neurological symptoms.
Pathogenesis
Intrinsic Factor and Absorption
Vitamin B12, also known as cobalamin, is a vital nutrient for red blood cell production and neurological function. However, dietary B12 isn’t readily absorbed by the body. This is where intrinsic factor comes in.
Intrinsic factor is a glycoprotein produced by the parietal cells in the stomach lining. It binds to dietary vitamin B12 in the stomach, forming an intrinsic factor-B12 complex. This complex then travels to the terminal ileum (lower part of the small intestine) where specific receptors recognize the intrinsic factor-B12 complex. The complex is then absorbed into the bloodstream, allowing B12 to be transported and utilized by the body.
Autoimmune Destruction and Deficiency
In pernicious anemia, the hallmark autoimmune attack targets parietal cells in the stomach lining, leading to a decline in intrinsic factor production and subsequent vitamin B12 deficiency. While the exact cause remains elusive, a potential mechanism involving gastric dendritic cells and autoreactive T lymphocytes is suggested.
- Gastric Dendritic Cells and Antigen Presentation: Gastric dendritic cells are specialized immune cells within the stomach lining. Their primary function involves antigen presentation – capturing and processing foreign or potentially harmful molecules, then presenting fragments (peptides) of these antigens to T lymphocytes for immune response evaluation.
- Apoptotic Parietal Cells and Misinterpretation: During normal stomach lining turnover, some parietal cells undergo programmed cell death (apoptosis). Dendritic cells might engulf fragments (peptides) derived from these apoptotic cells, including those originating from the proton/potassium ATPase, a protein abundantly expressed on the parietal cell surface.
- Presentation to T Lymphocytes: The dendritic cells then migrate to lymph nodes near the stomach (paragastric lymph nodes). Here, they present the acquired peptides to T lymphocytes. In individuals susceptible to pernicious anemia, a breakdown in immune tolerance might occur.
- Autoreactive T Cell Activation: Under normal circumstances, T cells would recognize these self-antigens (peptides from parietal cells) as harmless. However, in pernicious anemia, these presented peptides might be misinterpreted as foreign or threatening by some T cells. These T cells become activated, initiating an autoimmune response against healthy parietal cells.
- B Cell Activation and Antibody Production: Activated T cells can stimulate B lymphocytes (B cells), which are responsible for antibody production. This explains the presence of autoantibodies in many patients with pernicious anemia:
- Parietal Cell Antibody (PCA): Over 90% of patients have antibodies targeting parietal cells themselves.
- Intrinsic Factor Antibody (IFA): Around 50% of patients also have antibodies against intrinsic factor, further hindering vitamin B12 absorption.
Pernicious Anemia Symptoms and Signs
Pernicious anemia can cause a wide range of symptoms, but they often develop gradually and can be subtle at first. The severity of symptoms depends on the degree of vitamin B12 deficiency.
Common manifestations include:
Hematologic (blood-related)
- Fatigue and weakness: This is a very common pernicious anemia symptom due to the reduced oxygen-carrying capacity of red blood cells caused by B12 deficiency. People with pernicious anemia may feel constantly tired and lack energy for daily activities.
- Pale skin: B12 deficiency can lead to a decrease in red blood cell production, resulting in pallor (pale skin, lips, and nail beds).
- Shortness of breath: This can occur due to anemia, as the body struggles to deliver enough oxygen to tissues.
Neurologic
- Paresthesias (tingling and numbness): This is a characteristic symptom of B12 deficiency and in pernicious anemia. It often starts in the hands and feet, progressing upwards towards the legs and arms. It’s caused by damage to the nerves due to lack of B12, which is essential for nerve function.
- Balance problems: As nerve function in the legs deteriorates, individuals with pernicious anemia may experience difficulty with balance and coordination, increasing the risk of falls.
- Cognitive decline: B12 deficiency can affect memory, concentration, and overall cognitive function. In severe pernicious anemia cases, confusion and dementia-like symptoms may develop.
- Depression: This can be a consequence of both physical symptoms like fatigue and the psychological impact of cognitive decline.
Gastrointestinal (may be absent)
- Diarrhea: B12 deficiency can affect the digestive tract lining, leading to diarrhea in some pernicious anemia individuals.
- Glossitis (inflamed tongue): A smooth, red, and painful tongue can be a sign of B12 deficiency in pernicious anemia.

Pernicious Anemia Laboratory Investigations
Diagnosing pernicious anemia often involves a combination of blood tests and, in some cases, additional investigations:
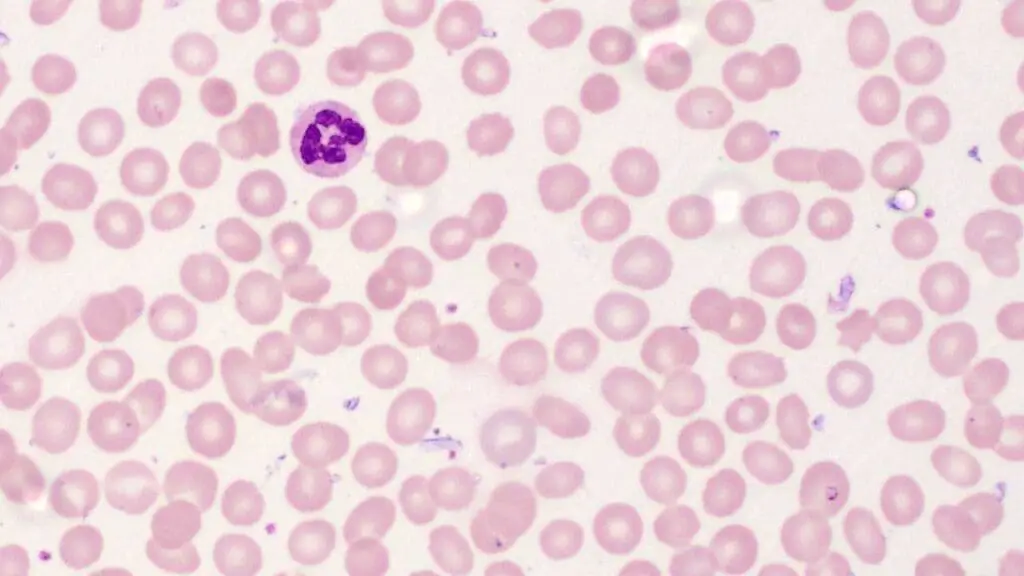
- Complete blood count (CBC)
- Macrocytosis: This is a hallmark finding in pernicious anemia, indicating enlarged red blood cells due to abnormal red blood cell production. Pernicious anemia is categorised under megaloblastic anemia disorders.
- Microcytic anemia (low MCV): This can be present if iron deficiency co-exists due to achlorhydria (lack of stomach acid) in pernicious anemia.
- Pancytopenia (reduction in all blood cell lines): This may occur in severe cases.
- Vitamin B12 levels
- Serum vitamin B12 assay measures the amount of B12 circulating in the blood. Low levels are indicative of deficiency.
- Indirect markers: Methylmalonic acid (MMA) and homocysteine levels can also be elevated in B12 deficiency.
- Autoimmune markers
- Parietal cell antibody (PCA): Positive result suggests the presence of antibodies targeting parietal cells.
- Intrinsic factor antibody (IFA): Positive result indicates antibodies against intrinsic factor, further supporting pernicious anemia.
- Gastric investigations (may be done in some cases)
- Schilling test: A traditional test using radioactive B12 to assess absorption, but less commonly used now due to safety concerns with radioactivity.
- Endoscopy with biopsy: Allows visualization of the stomach lining and potential abnormalities. It can also obtain tissue samples to assess parietal cell function. Endoscopy may reveal signs of gastritis (inflammation of the stomach lining) in some cases. Biopsy analysis may show a decrease in the number of parietal cells, supporting the diagnosis of pernicious anemia.
Pernicious Anemia Treatment and Management
Fortunately, pernicious anemia is a treatable condition. The primary focus of treatment revolves around addressing the vitamin B12 deficiency and preventing future complications.
Vitamin B12 Replacement Therapy
This is the cornerstone of treatment. Vitamin B12 can be administered through various routes, depending on the severity of deficiency and individual needs.
- Injections (most common and effective): Intramuscular injections are the preferred initial approach, especially in cases with severe deficiency. They ensure optimal absorption of B12.
- Nasal spray: A convenient option, particularly for long-term maintenance therapy.
- Oral tablets: Less effective due to potential absorption issues in the gut, but may be suitable for maintenance therapy in some cases, especially if monitored closely.
Long-term Treatment
Pernicious anemia is a lifelong condition. Regular vitamin B12 replacement therapy is crucial to maintain healthy vitamin B12 levels and prevent complications. The frequency of injections or dosage of other forms may be adjusted based on individual response and B12 levels.
Monitoring Response to Treatment
Blood tests, including complete blood count (CBC) and vitamin B12 levels, are monitored regularly to assess response to treatment.
- Improvement in red blood cell count (normalization of MCV) is expected with successful treatment.
- Vitamin B12 levels should also reach and remain within the normal range.
Management of Neurological Complications
While B12 replacement can improve neurological symptoms, some damage may be irreversible.
- Supportive measures: Physical therapy or occupational therapy can help manage balance issues and improve daily function.
- Medications: Specific medications for managing nerve pain may be prescribed in some cases.
Additional Considerations
- Diet: Even with B12 replacement, a healthy diet rich in various nutrients is essential for overall health.
- Underlying Conditions: If pernicious anemia co-exists with other conditions like iron deficiency, those may also require treatment.
- Monitoring for Gastric Cancer: Individuals with pernicious anemia have a slightly increased risk of stomach cancer. Regular monitoring with endoscopy may be recommended by the healthcare professional.
Overall, the treatment approach for pernicious anemia aims to replenish vitamin B12 stores, address symptoms, prevent complications, and improve quality of life. The specific treatment plan will be tailored to the individual’s needs and monitored closely to ensure optimal outcomes.
Prognosis
The good news is that pernicious anemia, when diagnosed and treated promptly, has a generally favorable prognosis.
- Symptom Improvement: Early diagnosis allows for early intervention with vitamin B12 replacement therapy. This can lead to significant improvement in symptoms like fatigue, weakness, shortness of breath, and nerve-related issues (tingling, numbness, balance problems).
- Hematologic Recovery: With consistent B12 replacement, red blood cell production normalizes. This translates to a reversal of macrocytosis (enlarged red blood cells) on a complete blood count (CBC) and improved oxygen delivery throughout the body.
- Neurological Recovery: B12 replacement can reverse some neurological symptoms like paresthesias and improve cognitive function. However, it’s important to note that some nerve damage, especially in severe or long-standing cases, may be irreversible. Early diagnosis and treatment can help minimize the extent of such damage.
- Maintaining Good Health: Long-term vitamin B12 replacement therapy ensures that B12 levels remain within the normal range. This helps prevent future complications and allows individuals with pernicious anemia to live healthy and active lives.
Factors Affecting Prognosis
- Severity of Deficiency at Diagnosis: Early diagnosis and treatment generally lead to better outcomes. The longer someone has been deficient in B12, the higher the chance of some irreversible damage.
- Adherence to Treatment: Consistent B12 replacement therapy as prescribed is crucial for maintaining healthy B12 levels and managing symptoms effectively.
- Management of Co-existing Conditions: If pernicious anemia co-occurs with other health issues like iron deficiency or certain autoimmune diseases, addressing those conditions will also contribute to a better overall prognosis.
Overall, with early diagnosis, consistent treatment, and proper management of co-existing conditions, individuals with pernicious anemia can expect a good quality of life with minimal to no limitations.
The Link Between Pernicious Anemia and Other Autoimmune Diseases
Pernicious anemia is classified as an autoimmune disease where the body attacks healthy tissues. Interestingly, there’s a higher prevalence of pernicious anemia co-existing with other autoimmune conditions. Here’s why this association might occur:
- Shared Genetic Predisposition: Certain genes may increase susceptibility to developing multiple autoimmune diseases. These genes might influence how the immune system functions and targets specific tissues.
- Immune System Dysregulation: In autoimmune conditions, the immune system malfunctions and starts attacking healthy tissues. Pernicious anemia and other autoimmune diseases might share underlying mechanisms related to this dysregulation.
- Environmental Triggers: Some environmental factors, such as viral infections or exposure to certain chemicals, might trigger an autoimmune response. These triggers could potentially target different tissues in individuals with a genetic predisposition, leading to the development of multiple autoimmune conditions.
Examples of Autoimmune Diseases Associated with Pernicious Anemia
- Type 1 Diabetes: This condition is caused by the immune system attacking insulin-producing cells in the pancreas.
- Thyroiditis: This refers to inflammation of the thyroid gland, which can be caused by autoimmune processes.
- Addison’s Disease: This condition involves the destruction of adrenal glands by the immune system.
- Celiac Disease: This autoimmune disorder affects the small intestine and can interfere with vitamin B12 absorption, potentially contributing to deficiency.
Importance of Identifying Co-existing Conditions
- Recognizing the presence of other autoimmune diseases alongside pernicious anemia allows for a more comprehensive treatment approach.
- Regular monitoring for potential complications associated with these co-existing conditions can be implemented.
Frequently Asked Questions (FAQs)
What is the difference between pernicious anemia and B12 deficiency?
B12 deficiency is a broader term encompassing various causes of low vitamin B12 levels in the body. Pernicious anemia is a specific type of B12 deficiency caused by an autoimmune attack on stomach cells that produce intrinsic factor, a protein essential for B12 absorption. While both conditions share symptoms like fatigue and weakness, pernicious anemia has a distinct autoimmune cause. Not all B12 deficiencies are due to pernicious anemia, and other factors like dietary limitations or gut issues can also contribute.
Is pernicious anemia life threatening?
Pernicious anemia itself isn’t life threatening if caught early and treated effectively with vitamin B12 replacement therapy. However, left untreated, the B12 deficiency can lead to severe neurological complications and potentially heart problems. Additionally, people with pernicious anemia have a slightly increased risk of stomach cancer, so regular monitoring is crucial. With proper management, most people with pernicious anemia can live long and healthy lives.
Can pernicious anemia cause stomach cancer?
Pernicious anemia doesn’t directly cause stomach cancer, but it creates conditions that might increase the risk. The long-term lack of stomach acid (achlorhydria) caused by pernicious anemia can create an environment where pre-cancerous stomach lining changes can develop. Regular monitoring with endoscopy is recommended for people with pernicious anemia to detect any suspicious changes early and improve the chances of successful treatment.
How does pernicious anemia cause gastritis?
Pernicious anemia doesn’t directly cause gastritis (stomach inflammation). In fact, the autoimmune attack in pernicious anemia targets the parietal cells in the stomach that produce stomach acid. This lack of acid (achlorhydria) can irritate the stomach lining over time, but it’s not the typical inflammatory response seen in gastritis caused by infection or other factors.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Anemia: Diagnosis and Treatment (Willis, 2016).
- Management of Anemia: A Comprehensive Guide for Clinicians (Provenzano et al., 2018)
- Goldberg S, Hoffman J. Clinical Hematology Made Ridiculously Simple, 1st Edition: An Incredibly Easy Way to Learn for Medical, Nursing, PA Students, and General Practitioners (MedMaster Medical Books). 2021.
- Vaqar S, Shackelford KB. Pernicious Anemia. [Updated 2023 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK540989/10.1016/j.arr.2016.05.005. Epub 2016 May 17. PMID: 27223997; PMCID: PMC5114166.
- Health Quality Ontario. Vitamin B12 and cognitive function: an evidence-based analysis. Ont Health Technol Assess Ser. 2013 Nov 1;13(23):1-45. PMID: 24379897; PMCID: PMC3874776.




