TL;DR
Vitamin K Deficiency Bleeding (VKDB) is a hemorrhagic disorder in newborns and infants (typically 0-6 months) caused by insufficient levels of vitamin K-dependent clotting factors, leading to spontaneous or traumatic bleeding.
- Causes: All newborns are physiologically deficient due to poor placental transfer, low liver stores, and a lack of established gut flora to produce Vitamin K2.
- Pathophysiology: Vitamin K is essential for the enzyme γ-glutamyl carboxylase (GGCX), which activates the clotting factors through γ-carboxylation. In deficiency, the liver produces inactive precursor factors called PIVKA (Proteins Induced by Vitamin K Absence or Antagonism), leading to coagulation failure.
- Classification ▾:
- Early (0 – 24 hrs): Associated with maternal drug use (e.g., anticonvulsants, antituberculars). Highly severe.
- Classical (2 – 7 days): Due to physiological deficiency and lack of prophylaxis. Presents as GI or mucosal bleeding.
- Late (2 wks – 6 mos): Most dangerous. Primarily affects exclusively breastfed infants without prophylaxis, often coupled with an underlying malabsorption disorder (e.g., cholestasis). Up to 50% present with devastating Intracranial Hemorrhage (ICH).
- Diagnosis ▾: Severely prolonged PT/INR and a prolonged or normal aPTT. Normal fibrinogen and platelet count and elevated levels of PIVKA-II.
- Treatment and Prevention ▾:
- Acute Bleeding: Immediate IV Vitamin K1 (1.0 mg) for rapid reversal (the “therapeutic diagnosis”). Fresh Frozen Plasma (FFP) is given for severe or life-threatening hemorrhage (like ICH) to immediately replace functional clotting factors.
- Prevention: Universal prophylactic IM injection of Vitamin K1 at birth is the global standard of care, offering reliable protection against all forms of VKDB.
*Click ▾ for more information
Introduction to Neonatal Coagulopathy and VKDB
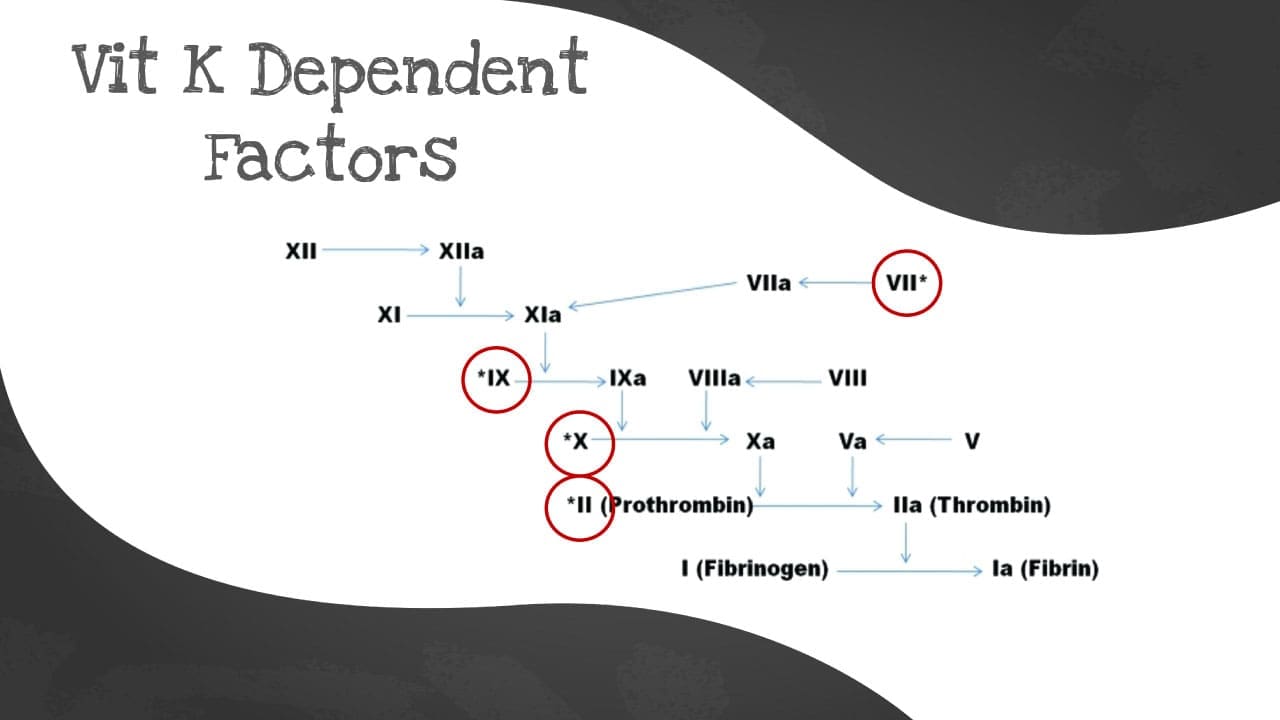
Vitamin K Deficiency Bleeding (VKDB), historically known as Hemorrhagic Disease of the Newborn (HDN), is a critical, yet largely preventable, coagulopathy in infancy. It results from the functional deficiency of the Vitamin K-dependent clotting factors (II, VII, IX, and X) and anticoagulant proteins (C and S). Despite universal prophylaxis recommendations, VKDB remains a global health concern, particularly where compliance with prophylactic measures is low. Understanding the unique hematologic profile of the neonate is essential to appreciate the necessity of intervention.
Definition of Vitamin K Deficiency Bleeding (VKDB)
Vitamin K Deficiency Bleeding (VKDB) is defined as a hemorrhagic disorder resulting from the functional deficiency of the Vitamin K-dependent coagulation factors – specifically, Factors II (Prothrombin), VII, IX, and X – as well as the natural anticoagulant Proteins C and S. The insufficient levels of these active clotting factors prevent the blood from forming a stable clot, leading to spontaneous, uncontrolled, and often life-threatening hemorrhage.
Historical Context and Nomenclature
Historically, this condition was universally known as the Hemorrhagic Disease of the Newborn (HDN). However, the nomenclature was officially updated to Vitamin K Deficiency Bleeding (VKDB) for reasons of clinical accuracy.
- Etiology: The new term clearly identifies the underlying deficiency of Vitamin K as the cause.
- Timing: The “Newborn” designation was misleading because a severe form of the disease – the Late VKDB – can occur well past the strict neonatal period (the first 28 days of life), manifesting between 2 weeks and 6 months of age. The term Vitamin K Deficiency Bleeding (VKDB) therefore offers a more accurate reflection of the entire at-risk timeline for infants.
The At-Risk Population
Crucially, all newborns are considered to be in a state of physiologic Vitamin K deficiency at birth. This is not a pathology but a normal developmental state resulting from three main limitations:
- Poor Placental Transfer: Vitamin K does not readily cross the placenta, leaving the fetus with minimal stores.
- Low Liver Reserves: The neonatal liver is immature and stores only small amounts of the vitamin.
- Sterile Gut: The intestinal flora, which eventually produces Vitamin K (menaquinon) in older children and adults, is not yet fully established in the newborn.
Because of this universal physiological vulnerability, prophylactic Vitamin K administration at birth is mandatory across the globe to protect the infant population from Vitamin K Deficiency Bleeding (VKDB).
Pathophysiology of Vitamin K and Coagulation
The pathology of Vitamin K Deficiency Bleeding (VKDB) is rooted in the disruption of the body’s final steps for activating coagulation factors, a process entirely dependent on adequate levels of Vitamin K.
The Role of Vitamin K
Vitamin K is a fat-soluble vitamin absorbed via dietary intake K1 and K2 and synthesized by intestinal bacteria (K2). It serves as a single, indispensable cofactor in the liver for the post-translational modification of specific proteins necessary for hemostasis.
The two clinically relevant forms are:
- Phylloquinone (Vitamin K1): The primary form obtained through diet (leafy green vegetables). This is the form used for prophylaxis.
- Menaquinones (Vitamin K2): Synthesized by bacteria in the gastrointestinal tract.
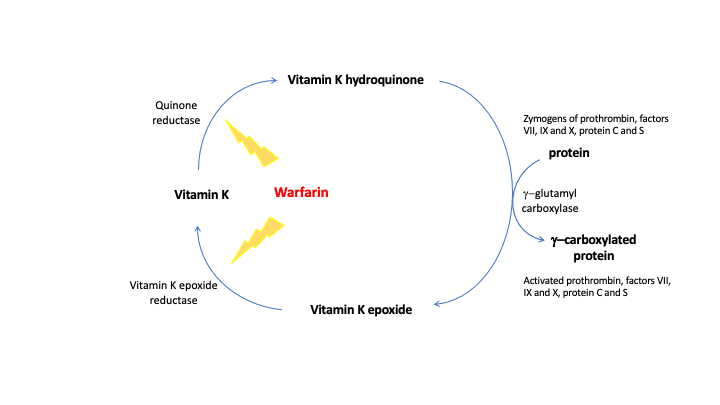
The key enzymatic reaction involving Vitamin K is its role as a cofactor for the enzyme γ-glutamyl carboxylase (GGCX).
The Clotting Cascade: Ɣ-Carboxylation
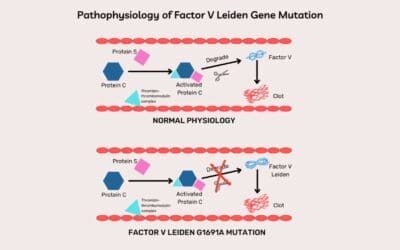
For the coagulation factors to become functionally active and capable of binding to calcium (a necessary step for initiating the clotting cascade), they must undergo a post-translational modification called γ-carboxylation.
This modification occurs when the GGCX enzyme uses Vitamin K to add a carboxyl group (COOH) to specific glutamic acid residues (Glu) on the precursor factors, converting them into γ-carboxyglutamic acid (Gla) residues.
This activation process is known as the Vitamin K Cycle:
- Activation: Vitamin K is oxidized (reduced to epoxide) during the carboxylation of the clotting factors.
- Regeneration: The oxidized Vitamin K (epoxide) must be converted back into its active form by the enzyme Vitamin K epoxide reductase (VKORC1). Anticoagulant drugs like warfarin work by inhibiting VKORC1, blocking the regeneration step.
The Vitamin K-Dependent Factors
The functionally relevant coagulation proteins requiring this γ-carboxylation for activity are:
- Pro-coagulant Factors: Factor II (Prothrombin), Factor VII, Factor IX, and Factor X (often called the 1972 group). A lack of active Factor VII causes an immediate prolongation of the PT (/INR).
- Anti-coagulant Factors: Protein C and Protein S. These factors are critical for regulating and shutting down the clotting cascade. When they are also deficient in Vitamin K Deficiency Bleeding (VKDB), the natural ability to control widespread coagulation is compromised, though the bleeding phenotype dominates.
Pathologic Mechanism
In an infant with Vitamin K Deficiency Bleeding (VKDB) who has a severe deficiency of active Vitamin K, the liver continues to synthesize the precursor proteins (Factors II, VII, IX, X) but cannot perform the necessary γ-carboxylation activation.
The body then accumulates high concentrations of these functionally inactive clotting factors. These inactive molecules are collectively known as PIVKA (Proteins Induced by Vitamin K Absence or Antagonism).
The most specific and frequently measured PIVKA is the precursor to Factor II (Prothrombin), called PIVKA-II or Des-gamma-carboxy prothrombin (DCP).
The presence of these inactive PIVKA means the entire clotting cascade is severely compromised, particularly the initiation (due to low Factor VII) and the final common pathway (due to low Factors II and X), leading to a failure to form a stable fibrin clot and resulting in spontaneous, potentially fatal, hemorrhage.
What happens in vitamin K deficiency?
The vitamin K cycle is important for:
- Blood clotting: Vitamin K is required for the production of several clotting factors, which are essential for blood clotting.
- Bone health: Vitamin K is required for the binding of bone matrix proteins to calcium, which is essential for bone health.
- Other cellular functions: Vitamin K is also involved in other cellular functions, such as cell growth and differentiation.
Vitamin K deficiency can lead to a number of problems, including:
- Bleeding problems: Vitamin K deficiency can lead to bleeding problems, such as easy bruising, nosebleeds, and heavy menstrual periods.
- Bone problems: Vitamin K deficiency can lead to bone problems, such as osteoporosis and fractures.
- Other health problems: Vitamin K deficiency has also been linked to other health problems, such as heart disease and cancer.
Causes of Vitamin K Deficiency Bleeding (VKDB)
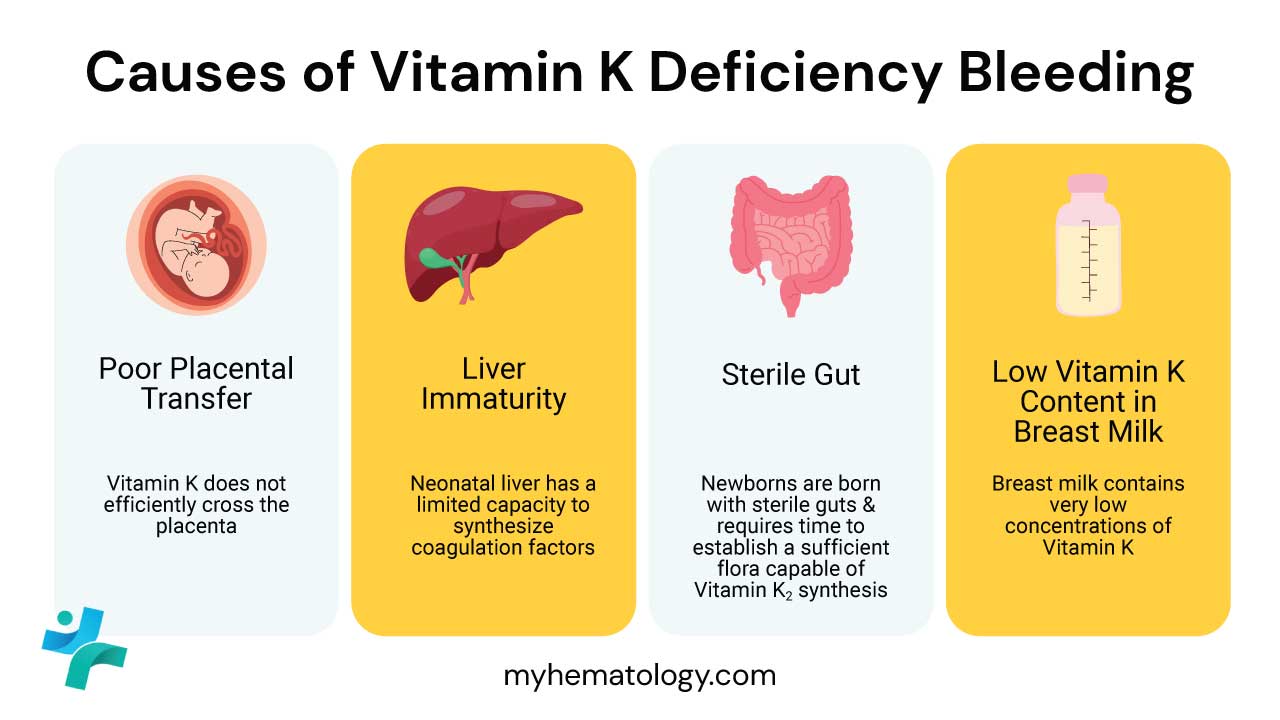
All newborns are considered vulnerable to Vitamin K Deficiency Bleeding (VKDB) due to multiple physiological factors that contribute to low Vitamin K status:
- Poor Placental Transfer: Vitamin K (a fat-soluble molecule) does not efficiently cross the placenta. Consequently, the fetus and neonate begin life with very limited Vitamin K stores.
- Low Reserves in the Neonatal Liver: Even with limited transfer, the neonatal liver has low capacity to store the vitamin, rapidly depleting any existing reserves.
- Lack of Established Gut Flora: In older children and adults, intestinal bacteria synthesize menaquinone (Vitamin K2), which contributes significantly to the body’s supply. The gut of a newborn is initially sterile and requires time to establish a sufficient flora capable of Vitamin K2 synthesis.
- Low Vitamin K Content in Human Breast Milk: While breast milk is the ideal nutritional source, its concentration of Vitamin K is significantly lower than that of commercial formulas. This places exclusively breastfed infants who do not receive prophylaxis at a higher, sustained risk of deficiency, particularly for Late VKDB.
Clinical Classification and Presentation of VKDB
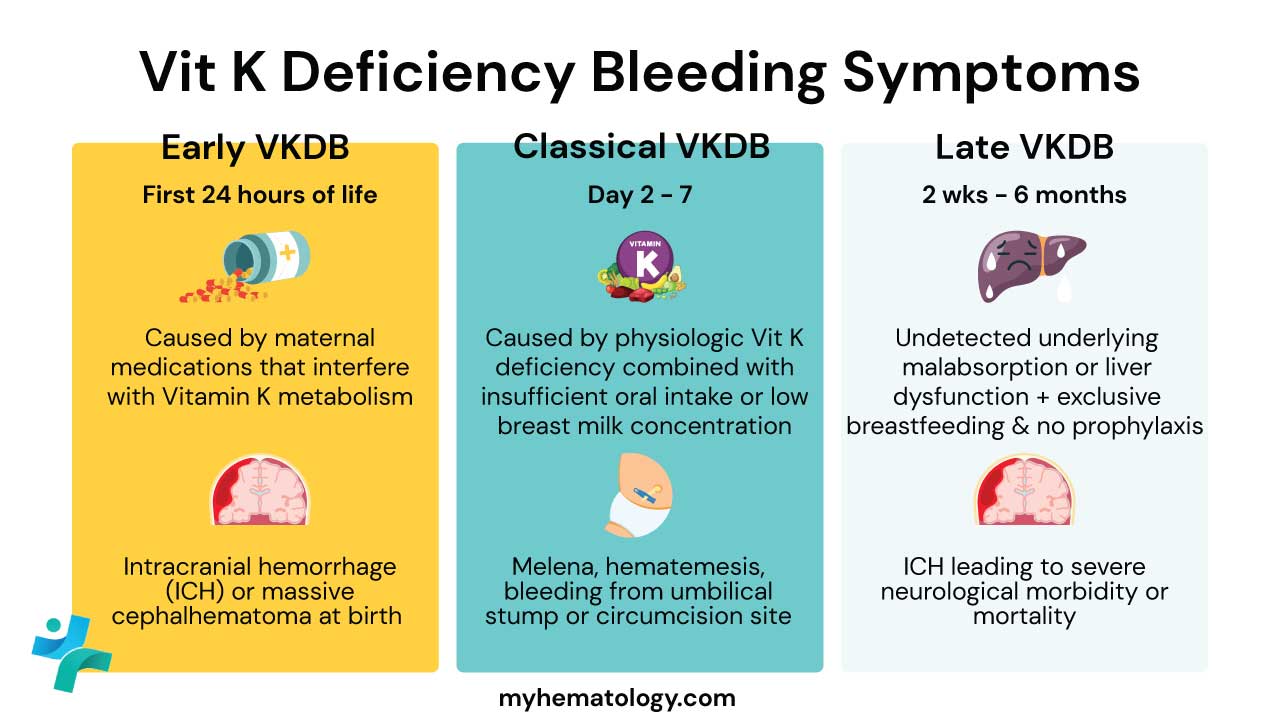
Vitamin K Deficiency Bleeding (VKDB) is categorized by the timing of bleeding onset relative to birth.
| VKDB Classification | Onset Timing | Etiology/Risk Factors | Clinical Presentation |
| Early VKDB | First 24 hours of life | Maternal ingestion of drugs that interfere with vitamin K metabolism (e.g., anticonvulsants like phenytoin, antitubercular drugs like isoniazid, some anticoagulants). | Often severe and life-threatening; typically presents as intracranial hemorrhage (ICH), intrathoracic, or intra-abdominal bleeding. |
| Classical VKDB | Day 2 – 7 | Physiologically low vitamin K stores at birth; Inadequate oral intake; Lack of prophylaxis. | Generally less severe; presents as superficial bleeding (umbilical stump, circumcision site), gastrointestinal bleeding (hematemesis, melena), or skin bruising. |
| Late VKDB | 1 week – 6 months (peak at 2–8 weeks) | Failure to receive prophylaxis at birth; Exclusive breastfeeding; Underlying cholestasis or malabsorption syndrome (e.g., Cystic Fibrosis, alpha1-antitrypsin deficiency) leading to impaired fat-soluble vitamin absorption. | Most dangerous form; 50%–80% present with severe intracranial hemorrhage (ICH), resulting in high mortality (up to 50%) and significant neurological morbidity. |
Laboratory Investigations and Diagnosis of VKDB
The diagnosis of Vitamin K Deficiency Bleeding (VKDB) is primarily clinical, supported by characteristic derangements in coagulation tests, and is often considered a “therapeutic diagnosis” given the rapid, dramatic reversal upon Vitamin K administration.
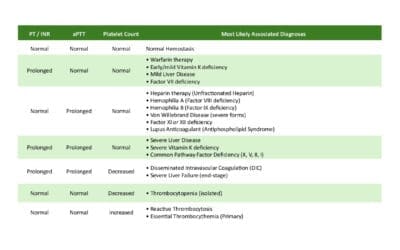
- Prothrombin Time (PT) and International Normalized Ratio (INR): Significantly Prolonged. The PT assesses the extrinsic and common coagulation pathways (Factors VII, X, V, II, I). Factor VII, which has the shortest half-life of all the Vitamin K-dependent factors, is the first to become functionally depleted. A highly elevated PT (and therefore a high INR) is the hallmark of Vitamin K Deficiency Bleeding (VKDB), reflecting this severe deficiency.
- Activated Partial Thromboplastin Time (aPTT): Prolonged or Normal. The aPTT assesses the intrinsic and common pathways. Since Factor IX (intrinsic) is Vitamin K-dependent, the aPTT may be prolonged. However, the PT/INR derangement is typically much more significant because Factor VII depletion is the primary driver of coagulopathy.
- Platelet Count, Fibrinogen, and D-dimer: Normal. These results are crucial for ruling out other critical neonatal bleeding disorders, particularly Disseminated Intravascular Coagulation (DIC). In DIC, the infant would typically exhibit thrombocytopenia (low platelets), hypofibrinogenemia (low fibrinogen), and highly elevated D-dimers (due to widespread clotting and fibrinolysis). Normal values for these three tests strongly point toward a primary coagulopathy like Vitamin K Deficiency Bleeding (VKDB).
- PIVKA-II (DCP): This test is highly sensitive and specific. Elevated levels of PIVKA-II (DCP), the inactive form of Factor II (Prothrombin), confirm that the coagulopathy is specifically due to a failure of the Vitamin K-dependent γ-carboxylation process.
- Cranial Imaging: Cranial Computed Tomography (CT) or Magnetic Resonance Imaging (MRI) is mandatory for any infant presenting with symptoms suggestive of Late VKDB (e.g., seizures, lethargy, bulging fontanelle) to confirm and localize a potential Intracranial Hemorrhage (ICH).
Differential Diagnosis of VKDB
| Condition | PT/INR | aPTT | Platelets | Fibrinogen | PIVKA}-II | Key Distinguishing Feature |
| Vitamin K Deficiency Bleeding (VKDB) | ↑ (High) | ↑ or Normal | Normal | Normal | ↑ (High) | Rapid and complete correction of PT/INR after Vitamin K administration. |
| Disseminated Intravascular Coagulation (DIC) | ↑ | ↑ | ↓ (Low) | ↓ (Low) | Normal | Consumption of coagulation factors and platelets; elevated D-dimer. |
| Severe Hepatic Failure | ↑ | ↑ | Normal or ↓ | ↓ (Low) | ↑ (High) | Elevated liver enzymes (AST/ALT); coagulopathy is often refractory to Vitamin K therapy. |
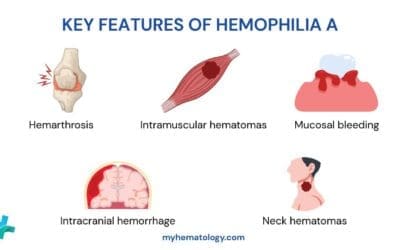
| Hemophilia A (Factor VIII Deficiency) | Normal | ↑ (High) | Normal | Normal | Normal | Isolated, severe prolongation of aPTT only. |
| Primary Thrombocytopenia | Normal | Normal | ↓ (Very Low) | Normal | Normal | Bleeding due to isolated platelet deficiency; coagulation times are normal. |
How do we treat VKDB?
The management of Vitamin K Deficiency Bleeding (VKDB) is a two-pronged strategy: immediate, aggressive treatment of the active bleeding episode, followed by universal prophylactic measures to prevent future occurrences.
Acute Management (Stopping the Bleed)
The primary goal is the rapid restoration of functional coagulation factors.
Immediate Vitamin K1 Administration
- Dose: 1.0 mg of Vitamin K1 (phylloquinone).
- Route: IV (Intravenous) is the preferred route in actively bleeding or critically ill infants (especially those with possible malabsorption) due to guaranteed and rapid uptake. IM (Intramuscular) can be used if IV access is delayed, but IV is faster and more reliable.
- Response: Vitamin K administration typically leads to a dramatic clinical and laboratory response, with PT and INR beginning to normalize within 2 – 4 hours and often correcting completely within 12 – 24 hours. This rapid correction is often considered the “therapeutic diagnosis” for Vitamin K Deficiency Bleeding (VKDB).
Coagulation Factor Replacement (For Severe Bleeding)
For active, life-threatening hemorrhage (e.g., confirmed or suspected intracranial hemorrhage (ICH), Vitamin K alone is often too slow. Immediate factor replacement is required to achieve rapid hemostasis.
- Fresh Frozen Plasma (FFP): FFP contains all active clotting factors (including Factors II, VII, IX, and X) and is the most common factor replacement used in pediatrics. It immediately replaces the missing functional factors.
- Prothrombin Complex Concentrate (PCC): PCC (a concentrated preparation of Factors II, VII, IX, and X) may be used in specialized settings for a more rapid, volume-sparing factor replacement, though FFP remains standard practice in many neonatal units.
Supportive and Specific Care
- Intracranial Hemorrhage: Requires immediate neurosurgical consultation, continuous neurological monitoring, and aggressive management of increased intracranial pressure.
- Volume Resuscitation: Management of hypovolemic shock if bleeding is massive.
Long-Term Prevention (Universal Prophylaxis)
Due to the devastating neurological morbidity associated with Late VKDB (primarily ICH), Vitamin K prophylaxis at birth is the universal standard of care across almost all developed nations.
- The Standard Regimen (IM Injection): All newborns receive a single IM injection of Vitamin K1 (0.5 – 1.0 mg) immediately after birth. The intramuscular dose provides a large, stable depot of Vitamin K that is slowly absorbed over several months, reliably bridging the period of physiological vulnerability (up to 6 months of age) and providing highly effective protection against all forms of Vitamin K Deficiency Bleeding (VKDB), especially the deadly Late VKDB.
- Oral Regimens (Less Common): In some countries, oral Vitamin K is offered. However, oral dosing is less reliable due to potential spitting, vomiting, and variable intestinal absorption, and requires multiple doses over several weeks/months. It is considered less effective than the IM dose, particularly in preventing late Vitamin K Deficiency Bleeding (VKDB). Oral administration, if chosen due to parental refusal of IM, requires meticulous adherence to the multi-dose schedule and careful monitoring for signs of late Vitamin K Deficiency Bleeding (VKDB), especially in exclusively breastfed infants.
- Parental Education: Crucial for informing parents about the severity of Vitamin K Deficiency Bleeding (VKDB) and the necessity of prophylaxis to ensure compliance.
Oral vs. Intramuscular (IM) Administration
The debate between oral (PO) and IM routes is a key area of discussion among healthcare professionals, particularly when addressing parental concerns:
| Feature | Intramuscular (IM) Prophylaxis | Oral (PO) Prophylaxis |
| Efficacy | Highest efficacy against all types (early, classic, and late VKDB). | Significantly less effective against Late VKDB, with failure rates reported due to non-compliance and malabsorption. |
| Dosing | Single 1.0 mg dose. | Requires a multiple-dose regimen (e.g., 2.0 mg at birth, 2.0 mg at 4 – 7 days, and 2.0 mg at 4 – 6 weeks. |
| Risk Factors | Not affected by breastfeeding or subclinical cholestasis. | Failure risk significantly increased by vomiting, diarrhea, or unrecognized cholestasis. |
| Safety | Requires injection, which is associated with momentary procedural pain. Association with childhood cancer has been debunked by extensive follow-up studies. | Avoids injection but depends on compliance for multiple doses over weeks. |
Prevention of Early VKDB
For mothers taking Vitamin K-inhibitory medications (e.g., certain anti-epileptics) during pregnancy, antenatal management may include administering oral Vitamin K1 to the mother in the weeks leading up to delivery, though data supporting this are mixed, and post-natal IM prophylaxis for the infant remains essential.
Frequently Asked Questions (FAQs)
What causes bleeding in a newborn?
The most common cause of bleeding in a newborn is vitamin K deficiency.
Newborns have limited vitamin K reserves at birth, and their gut bacteria, which produce vitamin K, are not yet fully developed. Without enough vitamin K, blood clotting can be impaired, leading to bleeding.
Other less common causes of bleeding in newborns include:
- Birth trauma: Injuries sustained during delivery can cause bleeding.
- Inherited clotting disorders: Some babies are born with inherited conditions that affect blood clotting.
- Platelet disorders: Problems with platelets, which help blood clot, can also cause bleeding.
- Infections: Certain infections can lead to bleeding.
- Liver disease: Liver problems can interfere with blood clotting.
Do breastfed babies need vitamin K?
Yes, breastfed babies need vitamin K. While breast milk is packed with nutrients, it doesn’t contain enough vitamin K to meet a newborn’s needs. Vitamin K is essential for blood clotting and preventing hemorrhagic disease of the newborn.
Why does vitamin K deficiency have normal bleeding time?
Vitamin K deficiency can have a normal bleeding time. This is because the bleeding time test primarily measures the function of platelets, which are not directly affected by lack of vitamin K.
What food is highest in vitamin K?
Vitamin K can be obtained from food and supplements. Good sources of vitamin K include green leafy vegetables, vegetable oils, and meats.
The recommended daily intake of vitamin K for adults is 120 micrograms for men and 90 micrograms for women. Pregnant and breastfeeding women need more vitamin K, 90 micrograms and 120 micrograms per day, respectively.
Most people can get enough vitamin K from their diet. However, some people may need to take a vitamin K supplement, such as people who are taking certain medications that interfere with the absorption of vitamin K.
Leafy green vegetables are generally the best source of vitamin K. Some of the highest vitamin K foods include:
- Kale
- Spinach
- Collard greens
- Swiss chard
- Turnip greens
- Mustard greens
- Broccoli
- Brussels sprouts
Other good sources of vitamin K include:
- Natto (a fermented soybean product)
- Sauerkraut
- Liver
- Eggs
- Avocado
- Kiwi
- Raspberries
It’s important to note that cooking can reduce the vitamin K content of some foods, so it’s best to consume them raw or lightly cooked whenever possible.
How to tell if you are vitamin K deficient?
Unfortunately, there are no specific symptoms of vitamin K deficiency that are easily recognizable. Often, the first sign is excessive bleeding or bruising.
However, if you have any of the following risk factors for vitamin K deficiency, you may be more susceptible:
- Newborn: Newborns have limited vitamin K reserves and may be at risk of deficiency.
- Malabsorption: Conditions that interfere with the absorption of nutrients from the intestines, such as celiac disease or Crohn’s disease, can lead to vitamin K deficiency.
- Liver disease: The liver plays a role in the activation of vitamin K. Liver damage can impair this process and lead to deficiency.
- Certain medications: Some medications, such as blood thinners and antibiotics, can interfere with vitamin K absorption or function.
- Intestinal surgery: Surgery that affects the small intestine can disrupt vitamin K absorption.
Who is likely to have vitamin K deficiency?
Certain individuals are more likely to have vitamin K deficiency than others. These include:
- Newborns: As mentioned earlier, newborns have limited vitamin K reserves and may be at risk of deficiency.
- People with malabsorption conditions: Conditions that interfere with the absorption of nutrients from the intestines, such as celiac disease or Crohn’s disease, can lead to vitamin K deficiency.
- Individuals with liver disease: The liver plays a role in the activation of vitamin K. Liver damage can impair this process and lead to deficiency.
- People taking certain medications: Some medications, such as blood thinners and antibiotics, can interfere with vitamin K absorption or function.
- Individuals who have undergone intestinal surgery: Surgery that affects the small intestine can disrupt vitamin K absorption.
- Individuals with certain dietary restrictions: People who follow a strict vegan or vegetarian diet if they do not consume enough vitamin K-rich foods or supplements.
Why is the INR so high in VKDB, and what is PIVKA-II?
The INR is extremely high because Vitamin K is required to activate Factor VII, which has the shortest half-life and rapidly declines. The PT/INR test is highly sensitive to Factor VII levels. PIVKA-II (Proteins Induced by Vitamin K Absence or Antagonism) is the inactive, under-carboxylated form of Prothrombin (Factor II). Its presence in high levels confirms the functional deficiency of Vitamin K.
Is the link between IM Vitamin K and childhood cancer still a concern?
No. The initial 1992 study suggesting a link has been extensively investigated by numerous larger, subsequent epidemiological studies which found no causal association between intramuscular Vitamin K prophylaxis and an increased risk of childhood leukemia or other cancers. This concern is considered thoroughly debunked by the current medical consensus.
Should formula-fed babies still receive Vitamin K prophylaxis?
Yes. While formula contains higher Vitamin K levels, the infant’s physiological deficiencies (low initial stores, sterile gut, immature liver) still place them at risk for early and classic Vitamin K Deficiency Bleeding (VKDB) during the first few days of life before adequate intake and gut colonization can occur. Prophylaxis is recommended for all newborns.
Glossary of Medical Terms
- Phylloquinone (K1): The natural form of Vitamin K found in plants; the form used in parenteral prophylaxis.
- Menaquinones (K2): The forms of Vitamin K synthesized by bacteria in the human gut.
- Gamma-Glutamyl Carboxylase (γ-GGC): The key hepatic enzyme requiring Vitamin K as a cofactor to activate clotting factors.
- PIVKA-II: Proteins Induced by Vitamin K Absence or Antagonism-II. Inactive precursor of Factor II (prothrombin); high levels are diagnostic of VK deficiency.
- Intracranial Hemorrhage (ICH): Bleeding within the skull (e.g., subdural, intraparenchymal); the most catastrophic complication of Late VKDB.
- Cholestasis: Impaired bile flow from the liver to the duodenum; leads to malabsorption of fat-soluble vitamins (A, D, E, K) and is a key risk factor for Late VKDB.
- Prothrombin Time (PT) / INR: A lab test measuring the extrinsic and common coagulation pathways; highly sensitive to Factor VII deficiency in VKDB.
- Parenteral: Administration of a substance by injection (e.g., intramuscularly or intravenously), avoiding the digestive tract.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Kher P, Verma RP. Hemorrhagic Disease of Newborn. 2023 Jun 26. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. PMID: 32644420.
- Ng E, Loewy AD. Guidelines for vitamin K prophylaxis in newborns. Paediatr Child Health 2018, 23(6):394–397.
- Goldberg S, Hoffman J. Clinical Hematology Made Ridiculously Simple, 1st Edition: An Incredibly Easy Way to Learn for Medical, Nursing, PA Students, and General Practitioners (MedMaster Medical Books). 2021.
- Keohane EM, Otto CN, Walenga JM. Rodak’s Hematology 6th Edition (Saunders). 2019.
- Sankar, M., Chandrasekaran, A., Kumar, P. et al. Vitamin K prophylaxis for prevention of vitamin K deficiency bleeding: a systematic review. J Perinatol 36 (Suppl 1), S29–S35 (2016). https://doi.org/10.1038/jp.2016.30
- Araki, S., & Shirahata, A. (2020). Vitamin K Deficiency Bleeding in Infancy. Nutrients, 12(3), 780. https://doi.org/10.3390/nu12030780
- Ceratto, S., Savino, F. Vitamin K deficiency bleeding in an apparently healthy newborn infant: the compelling need for evidence-based recommendation. Ital J Pediatr 45, 30 (2019). https://doi.org/10.1186/s13052-019-0625-y
- Schulte, R. et al. Rise in Late Onset Vitamin K Deficiency Bleeding in Young Infants Because of Omission or Refusal of Prophylaxis at Birth, Pediatric Neurology, Volume 50, Issue 6, 564 – 568.