TL;DR
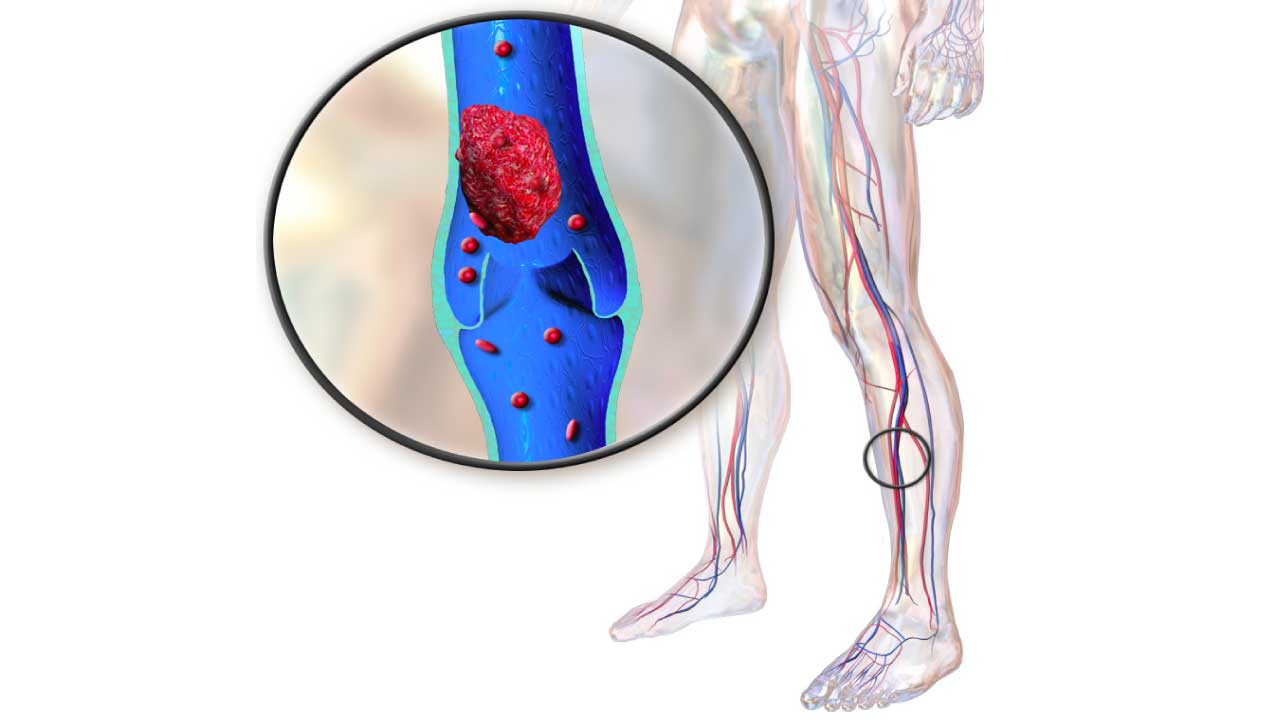
Deep vein thrombosis (DVT) is a blood clot (thrombosis) that forms in deep leg veins, often due to slow blood flow or injury.
Causes ▾: Slow blood flow (stasis), vessel wall damage, and hypercoagulability (increased clotting tendency).
Risks ▾: Sitting for long periods, surgery, pregnancy, certain medical conditions, smoking, obesity.
Deep Vein Thrombosis Symptoms ▾: Pain, swelling, redness, warmth in the affected leg due to blood clot in the leg (may be absent).
Complications ▾: Pulmonary embolism (PE) – potentially fatal blood clot in the lungs. Post-thrombotic syndrome (PTS) – chronic pain, swelling, skin changes.
Prevention ▾: Stay active, wear compression stockings, drink water, manage risk factors.
Treatment ▾: Anticoagulant medications, compression stockings, addressing underlying issues.
*Click ▾ for more information
Introduction
Deep vein thrombosis (DVT) is a serious medical condition characterized by the formation of a blood clot (thrombus) within a deep vein, a type of venous thrombosis, typically located in the legs (calf or thigh) (blood clot in legs) but also potentially occurring in the pelvis, arms, or other areas. These clots can partially or completely obstruct blood flow, leading to various complications.
Prevalence
Deep vein thrombosis (DVT) is a relatively common condition, affecting around 1-2 individuals per 1000 annually in developed countries. This translates to roughly 300,000 new cases per year in the United States alone. The risk of deep vein thrombosis (DVT) increases with age, with individuals over 60 years old being significantly more susceptible. Additionally, certain risk factors like surgery, prolonged immobility, certain medical conditions, and pregnancy can further elevate the risk.
Significance in Clinical Practice
Deep vein thrombosis (DVT) poses a significant challenge in clinical practice due to its potential for morbidity, mortality, and long-term complications.
Morbidity
- Pulmonary embolism (PE): The most feared complication of deep vein thrombosis (DVT) is PE, where a clot breaks off for example blood clot in the leg and travels to the lungs, potentially blocking blood flow and causing life-threatening respiratory distress. Up to 15% of untreated deep vein thrombosis (DVT) cases progress to PE.
- Post-thrombotic syndrome (PTS): This chronic condition arises in up to 40% of deep vein thrombosis (DVT) patients, leading to persistent leg pain due to blood clot in the leg, swelling, skin discoloration, and ulcers due to damaged veins and impaired blood flow.
- Chronic venous insufficiency: Left untreated, deep vein thrombosis (DVT) can cause long-term damage to the valves in the veins, leading to chronic venous insufficiency, characterized by deep vein thrombosis symptoms like persistent swelling, aching, and skin changes.
Mortality
- Direct deaths from deep vein thrombosis (DVT) occur due to massive PE, but the condition also indirectly contributes to mortality by increasing the risk of complications like heart failure and pneumonia.
- Mortality rates due to deep vein thrombosis (DVT) vary depending on factors like age, comorbidities, and access to timely treatment. However, estimates suggest the risk of death within 3 months of a deep vein thrombosis (DVT) diagnosis can be as high as 20-30%, highlighting its severity.
Economic Burden
- Deep vein thrombosis (DVT) represents a significant economic burden due to the costs associated with diagnosis, treatment, and management of complications. This includes hospital stays, medications, and long-term care for PTS and chronic venous insufficiency.
Overall, deep vein thrombosis (DVT) is a major public health concern with significant clinical and economic implications. Early diagnosis, prompt treatment, and preventive measures are crucial to reduce the burden of this potentially life-threatening condition.
Risk factors of Deep Vein Thrombosis (DVT)
Non-modifiable risk factors
- Age: Risk increases significantly with age, especially over 60 years old.
- Genetics: Certain inherited conditions can increase the risk of blood clotting, making deep vein thrombosis (DVT) more likely.
- Medical conditions: Certain medical conditions, like cancer, inflammatory bowel disease, and heart failure, can predispose individuals to deep vein thrombosis (DVT).
Modifiable risk factors
- Immobility and surgery: Prolonged periods of sitting or lying down (e.g., long flights, bed rest after surgery) can slow blood flow and increase clot formation leading to blood clot in the leg.
- Pregnancy and childbirth: Pregnancy and hormonal changes associated with it increase clotting risk. Postpartum period also carries an elevated risk.
- Oral contraceptives and hormone therapy: Certain types of birth control pills and hormone replacement therapy can increase the risk of deep vein thrombosis (DVT).
- Obesity and smoking: These factors contribute to inflammation and changes in blood vessel function, increasing clot risk.
- Travel and dehydration: Long journeys, especially by air, can lead to immobility and dehydration, contributing to deep vein thrombosis (DVT) risk especially blood clot in the leg.
Causes of Deep Vein Thrombosis (DVT)
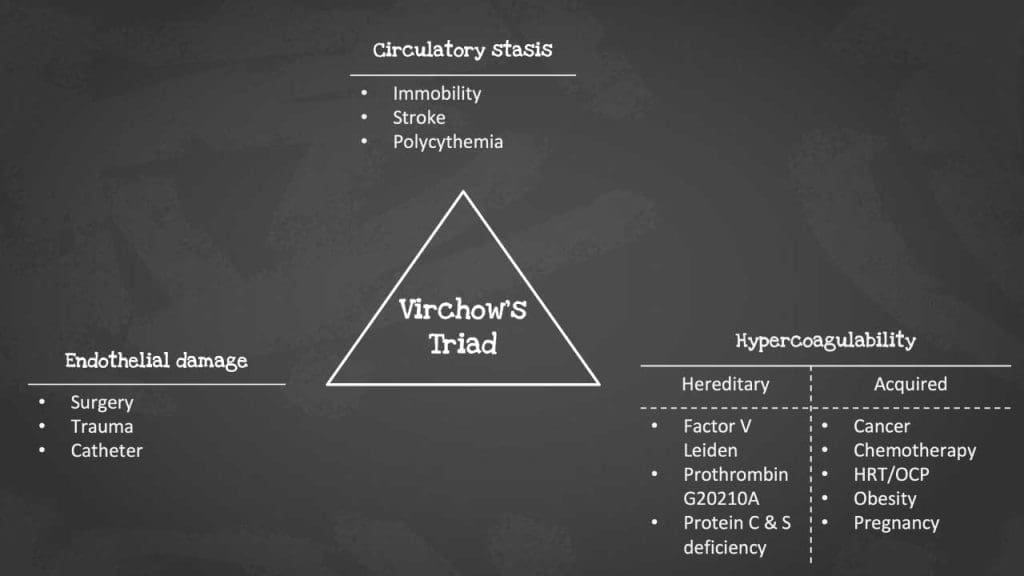
Deep vein thrombosis (DVT) is primarily caused by a combination of factors known as Virchow’s triad:
- Endothelial injury: Damage to the inner lining of a vein, caused by surgery, trauma, or inflammation, can trigger clot formation.
- Blood stasis: Slow or stagnant blood flow, due to immobility or certain medical conditions, allows clotting factors to accumulate and form a thrombus.
- Hypercoagulability: Certain conditions or genetic mutations can increase the blood’s tendency to clot, even with minimal stasis or injury.
Additional factors
- Catheters: Indwelling catheters inserted into veins can irritate the vessel wall and increase clotting risk.
- Varicose veins: Although not directly causing deep vein thrombosis (DVT), varicose veins can be a sign of underlying circulation problems that also contribute to deep vein thrombosis (DVT) risk.
Remember, the presence of one risk factor doesn’t guarantee deep vein thrombosis (DVT), but having multiple factors significantly increases the chances.
Pathophysiology of DVT
Understanding the underlying mechanisms, particularly Virchow’s Triad, is crucial for effective prevention and treatment.
Virchow’s Triad
This classic trio of factors forms the backbone of deep vein thrombosis (DVT) pathophysiology.
1. Endothelial Injury
- The endothelium, the smooth lining of blood vessels, acts as a barrier between blood and the vessel wall.
- Injury can occur due to:
- Surgery or trauma: Direct damage to the vein during procedures or accidents.
- Inflammation: Chronic inflammatory conditions like vasculitis can damage the endothelium.
- Chemical irritation: Catheters or medications can irritate the vessel wall.
- Genetic factors: Certain inherited conditions can weaken the endothelium, making it more susceptible to injury.
- Damaged endothelium loses its anti-thrombotic properties, exposing underlying tissues that trigger the clotting cascade. This cascade involves a series of proteins that activate each other, ultimately leading to the formation of fibrin, a mesh-like protein that forms the clot.
2. Blood Stasis
- Slow or stagnant blood flow allows clotting factors to accumulate and interact, increasing the risk of thrombus formation.
- This can occur due to:
- Immobility: Prolonged sitting or lying down, such as during long journeys or bed rest, reduces blood flow velocity leading to blood clot in the leg.
- Compression: Tight clothing or external pressure on veins can impede blood flow.
- Heart failure: Congestive heart failure can lead to blood pooling in the legs.
- Stasis disrupts the normal balance between pro-coagulant and anti-coagulant factors in the blood, tipping the scales towards clotting.
3. Hypercoagulability
- This refers to an increased tendency of the blood to clot, even in the absence of significant stasis or injury.
- It can be caused by:
- Genetic factors: Certain mutations can increase the production of clotting factors or decrease the production of anti-coagulant factors.
- Medical conditions: Cancer, inflammatory bowel disease, and pregnancy can all increase clotting risk.
- Hormonal changes: Oral contraceptives and hormone replacement therapy can elevate clotting factors.
- Hypercoagulability makes the blood more “sticky” and prone to forming clots even under normal conditions.
Mechanism of DVT
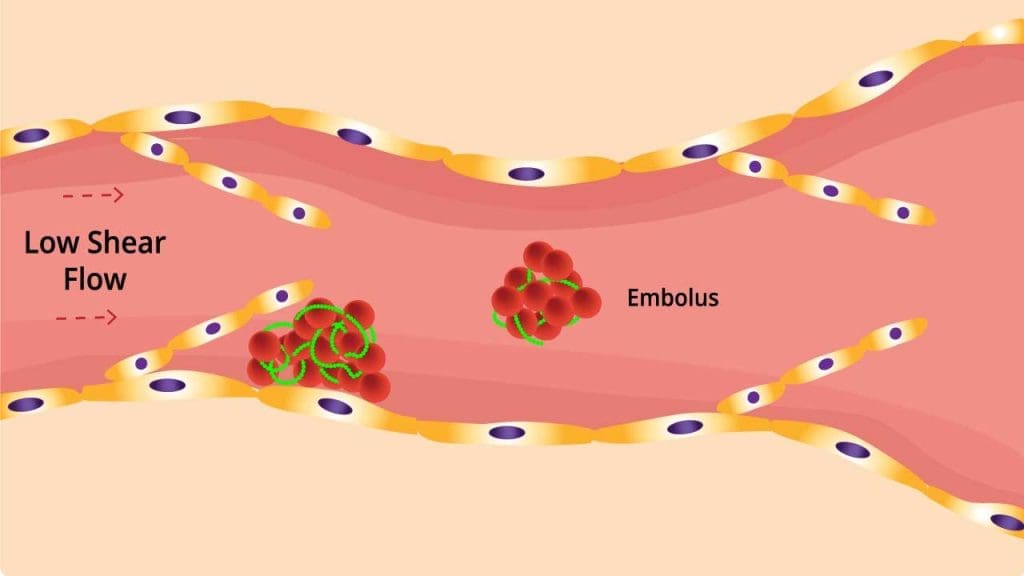
Deep vein thrombosis (DVT) poses a significant threat, often forming in areas where blood flow is compromised. While valves play a crucial role in propelling blood upwards against gravity, they can also become hotspots for deep vein thrombosis (DVT) development. This is due to several factors:
1. Reduced Blood Flow and Stasis: Valves create pockets downstream, where blood flow velocity decreases. This stasis allows blood components to accumulate, including clotting factors and red blood cells. This stagnant environment creates a perfect storm for clot formation.
2. Hypoxia and Endothelial Damage: The reduced blood flow also leads to lower oxygen levels (hypoxia) in these pockets. This can damage the inner lining of the vein (endothelium), further triggering the clotting cascade and creating a vicious cycle.
3. Local Hypercoagulability: As blood pools, activation products of the clotting system accumulate, creating a localized hypercoagulability state. This further increases the risk of clot formation within the valve pockets.
4. Viscous Blood and Clot Formation: Dehydration and elevated fibrinogen levels can thicken the blood (hyperviscosity), making it more prone to clotting. This viscous blood, combined with the other factors mentioned above, significantly increases the risk of thrombus formation.
5. Embolization and Pulmonary Embolism: Once a clot forms, it can break off and travel through the bloodstream as an embolus. This is particularly dangerous when it reaches the lungs, blocking blood flow and causing a potentially fatal condition called pulmonary embolism (PE).
Location-Specific Variations of DVT
Deep vein thrombosis (DVT) can occur in various locations, with each site presenting unique challenges and risk factors.
- Lower limb deep vein thrombosis (DVT) (most common): This primarily affects the deep veins of the calf and thigh, often triggered by immobility after surgery or prolonged sitting leading to blood clot in the legs.
- Upper limb deep vein thrombosis (DVT): Less common, typically associated with catheters, trauma, or certain medical conditions like breast cancer.
- Cerebral venous sinus thrombosis (CVST): Rare and life-threatening, affecting the dural sinuses of the brain. Can be caused by head injuries, infections, or hypercoagulable states.
- Splanchnic vein thrombosis (SVT): Affects veins within the abdomen, often associated with inflammatory bowel disease, abdominal surgery, or liver cancer.
- Portal vein thrombosis (PVT): Blocks the portal vein, responsible for draining blood from the intestines. Frequently linked to liver cirrhosis, infections, or tumors.
Understanding the specific risk factors and pathophysiology of deep vein thrombosis (DVT) at different locations is crucial for effective diagnosis, treatment, and prevention strategies.
Clinical Presentation and Deep Vein Thrombosis Symptoms
While deep vein thrombosis (DVT) often presents with classic symptoms, it can also manifest less obviously, requiring a high degree of clinical suspicion for timely diagnosis and intervention.
Typical Deep Vein Thrombosis Symptoms and Signs
- Pain: This is the most common deep vein thrombosis symptom, usually described as a throbbing or aching sensation in the affected leg, typically calf or thigh. It may worsen with standing, walking, or movement.
- Swelling: One leg, usually but not always the one with pain, appears swollen compared to the other due to blood clot in the leg. The swelling may involve the entire leg or just specific areas like the ankle or foot.
- Erythema (redness): The skin over the affected area may appear red or discolored, especially in lighter skin tones.
- Warmth: The affected area due to blood clot in the leg may feel warmer to the touch compared to the other leg.
- Tenderness: The area with pain and swelling may be tender to the touch.

Atypical Presentations
- Absence of deep vein thrombosis symptoms: Up to 30% of deep vein thrombosis (DVT) cases have no noticeable symptoms, particularly in individuals with underlying medical conditions or older adults.
- Swelling without pain: This can occur, especially in cases where the clot forms in deeper veins for example blood clot in the leg.
- Discoloration without swelling: Skin changes like reddish-brown patches or ulcers can develop, particularly in chronic cases or individuals with darker skin tones.
- Isolated calf pain: This can mimic muscle strain or other conditions, masking the underlying deep vein thrombosis (DVT).
- DVT in unusual locations: Upper limb DVT, CVST, SVT, and PVT can present with diverse symptoms depending on the affected site and may not involve pain or swelling in the legs.
Importance of Maintaining High Clinical Suspicion
- Atypical presentations and the absence of classic deep vein thrombosis symptoms can lead to delayed diagnosis and increased risk of complications.
- Healthcare professionals need to maintain a high index of suspicion for DVT, especially in individuals with risk factors, even if they present with atypical features.
- Early diagnosis and treatment are crucial to prevent complications like pulmonary embolism (PE), post-thrombotic syndrome (PTS), and chronic venous insufficiency.
Additional Factors to Consider
- Age: Older adults are more likely to have atypical deep vein thrombosis symptoms.
- Comorbidities: Certain medical conditions can mask or modify deep vein thrombosis symptoms.
- Pregnancy: Pregnant women are at increased risk for deep vein thrombosis, and symptoms might be attributed to pregnancy-related changes.
Early diagnosis and treatment of DVT are crucial to prevent complications like pulmonary embolism (PE) and chronic venous insufficiency. Maintaining a high level of clinical suspicion is essential for identifying even atypical presentations and ensuring prompt intervention.
Differential diagnosis of DVT
Diagnosing DVT can be challenging because deep vein thrombosis symptoms can mimic other conditions.
Musculoskeletal conditions
- Muscle strain or tear: Often causes localized pain, tenderness, and swelling, but usually doesn’t involve warmth or erythema.
- Tendonitis: Inflammation of a tendon can cause pain and tenderness, but typically not swelling or warmth.
- Bursitis: Inflammation of a bursa (fluid-filled sac) can cause pain and swelling, but usually not redness or warmth.
- Arthritis: Can cause pain, swelling, and stiffness in joints, but not limited to the leg and usually affects both sides.
Other vascular conditions
- Superficial thrombophlebitis: Inflammation of a vein near the skin’s surface, causing redness, pain, and tenderness, but rarely involving deep veins.
- Varicose veins: Enlarged, bulging veins that can cause swelling and discomfort, but not typically associated with pain, warmth, or redness.
- Lymphedema: Chronic swelling due to impaired lymphatic drainage, often involving both legs and presenting with a characteristic pitting (indentations remain upon pressing).
- Peripheral artery disease (PAD): Narrowing of arteries in the legs, causing pain, fatigue, and skin changes, but not swelling or redness.
Other medical conditions
- Cellulitis: Skin infection causing redness, pain, and swelling, but often with fever and chills.
- Abscess: Localized collection of pus causing pain, swelling, and redness, but not warmth or leg-specific symptoms.
- Fracture: Can cause pain, swelling, and bruising, but typically with a history of trauma and localized tenderness.
- Lipedema: Abnormal fat accumulation in the legs, leading to swelling and discomfort, but usually not warmth, redness, or pain.
Laboratory Diagnosis of DVT
Laboratory tests play a crucial role in DVT diagnosis and management, providing valuable information beyond clinical symptoms and physical examination.
Types of Tests for DVT Diagnosis
- D-dimer test: This blood test measures a protein fragment released when a blood clot breaks down. While not diagnostic alone, a negative D-dimer test in a low-risk individual makes DVT highly unlikely. Conversely, a high D-dimer result warrants further investigation.
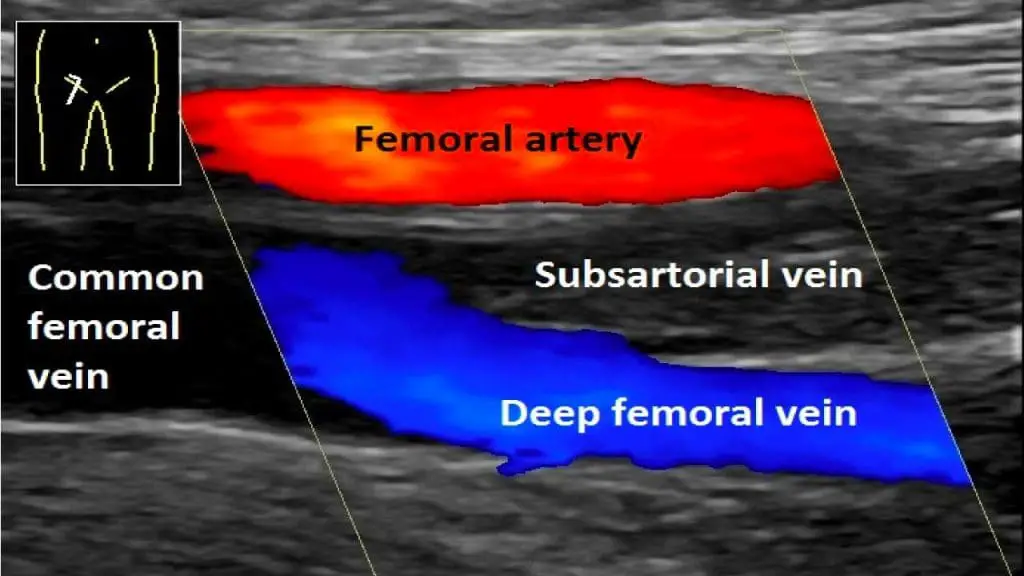
- Doppler ultrasound: This imaging technique uses sound waves to visualize blood flow in the veins. It is the gold standard for diagnosing DVT, providing information about the location, size, and extent of the clot.
- Venography: This X-ray technique involves injecting contrast dye into the veins to visualize them on images. It is less commonly used due to its invasiveness and being superseded by Doppler ultrasound in most cases.
Role in Assessing Co-morbidities
- Complete blood count (CBC): Can reveal abnormalities like anemia or infection, which might contribute to DVT risk.
- Kidney function tests: Impaired kidney function can affect blood clotting and influence treatment choices.
- Liver function tests: Liver dysfunction can impact clotting factors and require specific treatment considerations.
- Inflammatory markers: Elevated C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR) might suggest underlying inflammatory conditions that could contribute to DVT.
Role in Assessing Hypercoagulable States
- Genetic testing: Can identify inherited mutations that increase clotting risk, like Factor V Leiden or prothrombin gene mutation.
- Antiphospholipid antibody tests: These tests detect antibodies that can interfere with blood clotting, potentially leading to DVT.
- Protein C and S levels: These proteins are natural anticoagulants, and their deficiency can increase clotting risk.
- Homocysteine levels: High homocysteine levels may contribute to DVT risk, and testing can guide supplementation if needed.
Role of Laboratory Tests
- Diagnosis
- D-dimer test helps rule out DVT in low-risk patients with normal results.
- Abnormal D-dimer triggers further investigation with imaging tests.
- Co-morbidity tests identify underlying conditions contributing to DVT risk.
- Management
- Serial D-dimer measurements can monitor treatment response and assess for recurrent DVT.
- Co-morbidity tests guide long-term management strategies for underlying conditions.
- Genetic testing can inform the need for long-term anticoagulant therapy.
- Prognosis
- Identifying co-morbidities and hypercoagulable states helps predict the risk of future DVT events.
Limitations
- No single laboratory test is definitive for DVT diagnosis.
- D-dimer test needs interpretation in the context of clinical presentation and risk factors.
- Genetic testing results may not always translate directly to individual risk.
Overall, laboratory tests are valuable tools for DVT diagnosis, risk assessment, and management. Combining them with clinical evaluation and imaging studies ensures a comprehensive approach to this potentially serious condition.
Treatment and Management of DVT
Treating DVT involves a multi-pronged approach to prevent clot growth, reduce the risk of complications, and ultimately prevent recurrence.
Antithrombotic Therapy
- Mainstay of treatment: Aims to prevent clot growth and extension, reducing the risk of complications like pulmonary embolism (PE).
- Types:
- Unfractionated Heparin (UFH): Given intravenously, often initially, due to its rapid action. Requires frequent monitoring of blood clotting time (aPTT).
- Low-molecular-weight heparin (LMWH): Effective alternative or follow-up to UFH. Can be injected subcutaneously (at home), offering convenience and predictable dosing. Examples: Enoxaparin, Dalteparin.
- Warfarin (Coumadin): Oral anticoagulant, requiring regular blood tests (INR) to monitor clotting time and adjust dosage.
- Direct oral anticoagulants (DOACs): Newer medications like Dabigatran, Rivaroxaban, Apixaban, offering oral administration without INR monitoring.
- Duration of therapy: Varies depending on severity, location of DVT, and risk factors.
- Typically 3-6 months for lower limb DVT.
- Longer duration or even lifelong therapy for high-risk individuals or recurrent cases.
- Monitoring: Regular blood tests to assess medication effectiveness and manage bleeding risk.
Mechanical Interventions
- Compression stockings: Apply graduated pressure to legs, improving blood flow and reducing swelling. Used long-term to prevent post-thrombotic syndrome and recurrence.
- Vena cava filter: A mesh device inserted into a major vein to prevent blood clots from traveling to the lungs. Used in specific situations, like high PE risk or contraindications to anticoagulants.
Addressing Underlying Risk Factors
- Manage conditions like obesity, diabetes, and high blood pressure.
- Stop smoking.
- Maintain a healthy weight and exercise regularly.
- Address hormonal factors, like oral contraceptives, if contributing to the risk.
Preventing Recurrence
- Long-term anticoagulant therapy may be needed for individuals with high recurrence risk.
- Regular follow-up with healthcare providers is essential.
Post-Operative and Rehabilitation Care
- Early ambulation after surgery or prolonged immobility is crucial to prevent DVT.
- Physical therapy can help improve leg strength and circulation.
- Lymphedema management may be necessary for cases with persistent leg swelling.
Remember: Choosing the optimal treatment approach for DVT involves individualized assessment by a healthcare professional, considering medical history, risk factors, and specific needs.
Complications and Prognosis of DVT
DVT, although treatable, can lead to serious complications if left untreated or if preventive measures are not properly implemented. Here’s a deeper dive into the key complications and their impact on prognosis:
Pulmonary Embolism (PE)
- Most feared complication of DVT, occurring when a clot breaks off and travels to the lungs, blocking blood flow.
- Symptoms: Sudden shortness of breath, chest pain, coughing (may be bloody), rapid heart rate, lightheadedness or fainting.
- Untreated PE can be fatal, emphasizing the importance of prompt diagnosis and intervention.
- Risk factors for PE include larger clot size, involvement of multiple veins, and lack of timely treatment for DVT.
Post-thrombotic syndrome (PTS)
- Develops in about 30-40% of DVT cases, even with treatment.
- Occurs due to damaged valves and impaired blood flow in the affected veins.
- Symptoms: Chronic leg pain, swelling, skin discoloration, itching, and leg ulcers in severe cases.
- Can significantly impact quality of life and daily activities.
- Early diagnosis and intervention are crucial to minimize long-term consequences.
Chronic venous insufficiency (CVI)
- Long-term consequence of DVT and PTS, characterized by persistent leg swelling and circulation problems.
- Can lead to skin changes, discomfort, and limited mobility.
- Prevention and early management of DVT and PTS are essential to avoid CVI.
Prognosis of DVT
- With prompt diagnosis and proper treatment, most DVT cases have a good prognosis. However, the presence of complications like PE and PTS significantly affects the long-term outlook.
- Mortality rate within 3 months of DVT can be as high as 20-30% if untreated, highlighting the importance of early intervention. Studies suggest that timely treatment with anticoagulants can reduce the risk of PE by up to 80%.
- Lifestyle modifications like maintaining a healthy weight, avoiding smoking, and exercising regularly can further improve prognosis and prevent recurrence.
Overall, prompt diagnosis, appropriate treatment, and preventive measures are crucial for a positive prognosis in DVT. Addressing underlying risk factors and adopting healthy habits play a vital role in reducing the risk of complications and ensuring long-term well-being.
DVT Preventive Strategies
Preventing DVT is crucial, especially for individuals with high risk factors. Here’s a breakdown of key preventive strategies:
Pharmacological Prophylaxis
- Involves administering medications to prevent blood clots particularly blood clot in the leg from forming.
- Primarily used for high-risk patients undergoing surgery, particularly those with prior DVT or other risk factors like advanced age, obesity, or immobility.
- Common medications include:
- Low-molecular-weight heparin (LMWH): Injected subcutaneously, offering convenient and effective prophylaxis.
- Direct oral anticoagulants (DOACs): Orally administered medications gaining popularity due to their convenience and potentially lower bleeding risk compared to LMWH.
- The choice of medication, dosage, and duration of prophylaxis depend on individual risk factors and the specific medical context.
Mechanical Measures
- Compression stockings: Apply graduated pressure to the legs, improving blood flow and reducing the risk of blood pooling. Effective in preventing DVT in high-risk situations like long-distance travel, pregnancy, or post-surgery. Different types and compression levels are available, requiring proper fitting for optimal effectiveness.
- Ambulation: Regular movement, even just getting up and walking around every hour, helps prevent blood stasis and reduces clot formation risk. This is crucial for individuals at increased risk due to prolonged sitting or immobility.
Patient Education and Awareness
- Empowering individuals to understand their risk factors and recognize potential deep vein thrombosis symptoms is vital for early intervention.
- Educational initiatives can focus on:
- Identifying risk factors like medical conditions, lifestyle habits, and travel plans.
- Recognizing deep vein thrombosis symptoms like leg pain, swelling, redness, or warmth.
- Knowing the importance of seeking medical attention promptly if symptoms arise.
- Understanding preventive measures like compression stockings and ambulation.
Additional Strategies
- Maintaining a healthy weight and diet: Obesity increases DVT risk, so managing weight through healthy eating and exercise is crucial.
- Staying hydrated: Dehydration can thicken the blood and increase clot risk, so staying adequately hydrated is important.
- Avoiding smoking: Smoking damages blood vessels and increases clotting risk, so quitting is highly recommended.
- Managing chronic conditions: Effectively managing conditions like diabetes or high blood pressure can help reduce DVT risk.
- Avoid tight clothing: This can restrict blood flow and contribute to clot formation.
- Elevate your legs when resting or sleeping: This can help improve venous return and prevent blood pooling in the legs.
- Early ambulation after surgery: This is critical for reducing DVT risk, even if additional prophylactic measures are used.
- Pregnant women: Consult healthcare professionals for specific DVT prevention strategies during pregnancy and postpartum period.
- Travel recommendations: For long journeys, encourage frequent movement, staying hydrated, and wearing compression stockings if high-risk.
- Risk assessment tools: Healthcare professionals can utilize tools to assess individual DVT risk and guide prevention strategies.
Remember: DVT prevention is a multi-pronged approach. Combining pharmacological prophylaxis with mechanical measures, patient education, and healthy lifestyle habits can significantly reduce the risk of this serious condition.
Frequently Asked Questions (FAQs)
What is deep vein thrombosis?
Deep vein thrombosis (DVT) is a serious condition where a blood clot forms in a deep vein, most often in the legs (blood clot in the leg). This can happen due to several factors, like reduced blood flow from sitting for long periods, damage to the vein wall from surgery or injury, or an increased tendency for the blood to clot due to certain medical conditions or genetic factors.
What are the warning signs of deep vein thrombosis?
While DVT can sometimes be silent, there are key warning signs you shouldn’t ignore. Be on the lookout for these, especially if you have risk factors like prolonged sitting or recent surgery:
- Pain: Often throbbing or aching, typically in the calf or thigh, but can worsen with movement.
- Swelling: One leg, usually the one with pain, appears noticeably swollen compared to the other due to blood clot in the leg.
- Redness: Skin over the affected area may turn reddish or discolored, especially in lighter skin tones.
- Warmth: The affected area may feel warm to the touch compared to the other leg due to blood clot in the leg.
What causes deep vein thrombosis?
Deep vein thrombosis (DVT) forms due to a combination of factors working together, often referred to as Virchow’s triad:
1. Stasis (slow blood flow): This can occur from prolonged sitting or inactivity, such as during long flights or car rides, surgery with extended bed rest, or even certain medical conditions that lead to impaired circulation. When blood flows slowly, it becomes more likely to pool and clot.
2. Vessel wall damage: Injury or inflammation to the inner lining of a vein can make it more susceptible to clot formation. This damage can be caused by surgery, trauma, catheters, or certain medical conditions like vasculitis.
3. Hypercoagulability (increased clotting tendency): This can be inherited or acquired due to various factors like genetic mutations, pregnancy, hormonal changes, certain medications, smoking, dehydration, or some medical conditions. When your blood has a higher tendency to clot, it becomes more likely to form a thrombus even with less stasis or damage.
These factors can act independently or in combination to trigger DVT. Additionally, specific situations can increase the risk of DVT, like:
- Surgery: Particularly major surgeries or those involving the pelvis or legs.
- Pregnancy and postpartum period: Hormonal changes and pressure from the growing uterus can contribute to stasis and hypercoagulability.
- Cancer: Certain types of cancer and cancer treatments can increase clotting risk.
- Immobilization: Prolonged bed rest or wearing casts can lead to stasis.
How does DVT differ in presentation depending on its location (e.g., lower limb vs. upper limb)?
While the underlying causes of DVT remain the same regardless of location, its presentation can differ significantly depending on where the clot forms. Here’s a comparison of DVT in the lower limb (most common) vs. upper limb:
Lower limb DVT
- Deep Vein Thrombosis Symptoms
- More likely to present with classic deep vein thrombosis symptoms like pain, swelling, redness, and warmth in the affected leg, usually the calf or thigh.
- Pain can be throbbing or aching, worsening with movement or standing.
- Swelling can be significant and involve the entire leg or specific areas like the ankle or foot.
- Skin changes like redness or discoloration are more common.
- Diagnosis
- Doppler ultrasound is the gold standard diagnostic tool.
- D-dimer test can be helpful in ruling out DVT in low-risk individuals.
- Complications
- Pulmonary embolism (PE) is a major concern, where a clot travels to the lungs and blocks blood flow, potentially leading to respiratory distress and even death.
- Post-thrombotic syndrome (PTS) is a long-term complication characterized by chronic pain, swelling, and skin changes in the affected leg.
Upper limb DVT
- Deep Vein Thrombosis Symptoms
- Less common and often atypical, making diagnosis more challenging.
- Pain may be present, but it can be subtle or masked by other causes like muscle strain.
- Swelling may be limited to the arm or hand, and skin changes are less frequent.
- May cause arm heaviness, limited movement, or discoloration of the hand.
- Diagnosis
- Doppler ultrasound is still the preferred diagnostic tool, but venous duplex ultrasound or venography may be needed for confirmation.
- D-dimer test is less reliable due to lower prevalence of DVT in the upper limb.
- Complications
- PE is less common but still possible, especially if the clot extends into larger veins.
- Upper limb PTS is rare but can cause chronic arm swelling and pain.
Key differences
- Deep Vein Thrombosis Symptoms: Lower limb DVT typically presents with more classic and pronounced symptoms, while upper limb DVT can be more subtle and atypical.
- Diagnosis: Upper limb DVT may require additional imaging tests beyond Doppler ultrasound.
- Complications: PE is a major concern for both, but its frequency is slightly lower in upper limb DVT.
- Prevalence: Lower limb DVT is significantly more common than upper limb DVT.
Beyond pain and swelling, what are some atypical deep vein thrombosis symptoms that healthcare professionals should be aware of?
While pain and swelling are often the most prominent deep vein thrombosis symptoms, healthcare professionals should be aware of several atypical presentations that can easily be missed:
1. Isolated Calf Pain: This is a common scenario, especially in younger individuals, where pain in the calf is attributed to muscle strain or other causes. However, it can be the only deep vein thrombosis symptom, particularly in smaller, deeper veins.
2. Swelling Without Pain: This can occur in older adults or individuals with underlying conditions like diabetes, where pain perception is diminished. Swelling in one leg, especially if it’s sudden or unexplained, warrants further investigation.
3. Discoloration Without Swelling: Skin changes like reddish-brown patches or ulcers can develop, especially in chronic cases or individuals with darker skin tones. These changes can be subtle and may not be immediately associated with DVT.
4. Neurological Symptoms: In rare cases, DVT in the upper limb can cause nerve compression, leading to numbness, tingling, or weakness in the arm or hand. This can be mistaken for other neurological conditions.
5. Fever and Respiratory Distress: While not typical, DVT can sometimes cause a low-grade fever or even respiratory problems if the clot extends into the inferior vena cava and affects blood flow to the heart and lungs.
6. Absence of Symptoms: Up to 30% of DVT cases, especially in older adults or individuals with co-morbidities, can be completely asymptomatic. This highlights the importance of maintaining a high index of suspicion and considering DVT in the differential diagnosis, even in the absence of classic deep vein thrombosis symptoms.
Additional factors to consider:
- Risk factors: Patients with known risk factors for DVT, such as recent surgery, immobility, pregnancy, or a history of blood clots, should be even more closely monitored for atypical presentations.
- Unilateral symptoms: While leg pain or swelling can occur due to other conditions, their unilateral nature (one leg only) should raise suspicion of DVT.
- Progressive symptoms: Any worsening of deep vein thrombosis symptoms, even if initially mild or atypical, requires prompt evaluation.
How does D-dimer testing aid in DVT diagnosis, and what are its limitations?
D-dimer is a protein fragment produced when blood clots break down in the body. While its presence doesn’t definitively diagnose DVT, it plays a crucial role in the diagnostic process. Here’s a breakdown of its advantages and limitations:
Advantages
- Non-invasive and readily available: Unlike imaging tests, D-dimer is a simple blood test, making it convenient and widely accessible.
- Rapid results: Results are usually available within a few hours, aiding in quick decision-making.
- High negative predictive value: If the D-dimer level is low, it’s highly unlikely that DVT is present, especially in low-risk individuals. This can help rule out DVT quickly and avoid unnecessary imaging tests.
- Useful in serial monitoring: D-dimer levels can be monitored over time to assess treatment response or detect recurrent clots.
Limitations
- Not diagnostic by itself: A high D-dimer level can be caused by other conditions besides DVT, such as infection, inflammation, or recent surgery. Therefore, it cannot be used as the sole basis for diagnosis.
- Variable sensitivity: D-dimer levels can be influenced by various factors like age, pregnancy, and underlying medical conditions, affecting its accuracy in specific patient groups.
- Limited value in high-risk patients: In individuals with high pre-test probability of DVT due to strong clinical suspicion or risk factors, a negative D-dimer result may not be reliable enough to rule out DVT.
Overall
D-dimer is a valuable tool for DVT diagnosis, particularly for ruling out the condition in low-risk patients with atypical deep vein thrombosis symptoms or when considering the risks and benefits of imaging tests. However, it’s crucial to remember its limitations and interpret results in conjunction with clinical history, physical examination, and other diagnostic tests for an accurate diagnosis.
What are the long-term risks and complications associated with untreated DVT?
Leaving a deep vein thrombosis (DVT) untreated can lead to serious and potentially life-threatening complications. Here are some of the key risks and long-term consequences to be aware of:
1. Pulmonary embolism (PE): This is the most feared and potentially fatal complication of DVT, occurring when a blood clot breaks off for example from the blood clot in the leg and travels to the lungs, blocking blood flow. Symptoms of PE can include sudden shortness of breath, chest pain, coughing up blood, rapid heart rate, and lightheadedness. It requires immediate medical attention and treatment to prevent death.
2. Post-thrombotic syndrome (PTS): This chronic condition develops in up to 40% of DVT patients, even with treatment. It occurs due to damage to the affected vein, leading to impaired blood flow and a variety of symptoms like leg pain, swelling, and skin discoloration, difficulty walking or standing for long periods or skin ulcers or sores in severe cases
3. Chronic venous insufficiency (CVI): This develops when valves in the leg veins are damaged, preventing proper blood flow back to the heart. It can lead to similar symptoms as PTS but without a history of DVT.
4. Increased risk of recurrent DVT: Once you’ve had DVT, you are at a higher risk of developing it again, especially if the underlying risk factors are not addressed.
5. Impaired quality of life: The chronic pain, swelling, and limitations caused by PTS and CVI can significantly impact a person’s quality of life, affecting their ability to work, exercise, and participate in daily activities.
Additional risks in specific cases:
- Pregnancy complications: Untreated DVT during pregnancy can increase the risk of miscarriage, preeclampsia, and other complications.
- Spread of infection: In rare cases, untreated DVT can lead to a serious infection called septic thrombophlebitis, requiring aggressive treatment with antibiotics.
How can compression stockings play a role in both preventing and managing DVT?
Compression stockings are valuable tools for both preventing and managing DVT in various ways.
For prevention
- Improve blood flow: They apply graduated pressure, highest at the ankle and decreasing towards the thigh. This helps squeeze the leg muscles, promoting better blood circulation and preventing blood from pooling in the veins, a key factor in DVT formation.
- Reduce vein size: The pressure helps compress the veins, minimizing their diameter and making it harder for blood to stagnate and clot.
- Support vein valves: Compression stockings can help support the function of one-way valves within the veins, ensuring blood flows upwards towards the heart instead of pooling downwards.
For management
- Reduce swelling and pain: After DVT diagnosis, compression stockings can significantly reduce swelling and pain in the affected leg by encouraging fluid drainage and improving circulation.
- Prevent post-thrombotic syndrome (PTS): Consistent use of compression stockings after DVT can significantly reduce the risk of developing PTS, a chronic condition with ongoing pain, swelling, and skin changes.
- Improve quality of life: By managing swelling and pain, compression stockings can help patients with DVT regain mobility, improve their quality of life, and participate more actively in daily activities.
Choosing the right stockings
- Compression level: Different levels of compression are available, recommended based on individual needs and the severity of DVT. Consult a healthcare professional for proper fitting and guidance.
- Type of stocking: Knee-high or thigh-high options are available, depending on the affected area and individual preferences.
- Comfort and fit: Stockings should be comfortable and fit well to be worn consistently for optimal effectiveness.
Important points
- Compression stockings are not a replacement for other DVT treatment, like anticoagulant medications.
- They should be used in conjunction with other preventive measures like maintaining a healthy weight, staying active, and avoiding sitting for prolonged periods.
- Regular monitoring and follow-up with a healthcare professional are crucial when using compression stockings for DVT management.
By understanding their role and using them correctly, compression stockings can be a valuable tool in both preventing and managing DVT, promoting better circulation, reducing symptoms, and improving overall well-being.
Can deep vein thrombosis be cured?
Deep vein thrombosis (DVT) itself isn’t necessarily “cured” in the traditional sense, but it can be effectively treated and managed to prevent further complications and improve quality of life. Here’s a breakdown:
Treating the Clot
- Anticoagulant medications: These medications, like warfarin or DOACs (direct oral anticoagulants), help prevent the clot from growing and new ones from forming. They’re typically taken for several months or even longer, depending on the severity of the DVT and individual risk factors.
- Compression stockings: As mentioned earlier, these stockings apply graduated pressure to improve blood flow and reduce swelling, promoting healing and preventing PTS.
- Thrombolysis or thrombectomy: In some severe cases, where the clot is large or life-threatening, minimally invasive procedures may be used to remove or break up the clot.
Managing Long-Term Effects
- Continuing anticoagulation: Depending on the initial cause and risk factors, some individuals may need to continue taking anticoagulants for a longer period or even indefinitely to prevent future clots.
- Lifestyle changes: Maintaining a healthy weight, exercising regularly, avoiding smoking, and staying hydrated are crucial for reducing the risk of recurrent DVT and improving overall health.
- Compression stockings: Consistent use of compression stockings can significantly reduce the risk of developing PTS and manage ongoing swelling and pain.
What is the survival rate of DVT?
The survival rate for DVT varies depending on several factors, including:
- Promptness of diagnosis and treatment: Early intervention is crucial for reducing the risk of complications, especially pulmonary embolism (PE), which can be life-threatening.
- Severity of the DVT: Larger clots or those involving major veins carry a higher risk of complications and potentially lower survival rates.
- Presence of underlying medical conditions: Individuals with co-morbidities like heart disease, lung disease, or cancer may have a higher risk of complications and lower survival rates.
- Age of the patient: Generally, younger individuals have a higher survival rate compared to older adults with DVT.
Here’s some information on DVT survival rates:
- Short-term survival: Studies report short-term survival rates for DVT ranging from 95% to 97% with prompt treatment, while the rate for PE can be around 77% to 94%.
- Long-term survival: Long-term survival rates for both DVT and PE range from 61% to 75%, depending on the factors mentioned above.
However, it’s important to remember that these are just general statistics, and individual outcomes can vary greatly.
Therefore, focusing solely on survival rates isn’t always the most helpful approach. It’s crucial to prioritize early diagnosis and treatment to minimize the risk of complications and improve the chances of a full recovery and good quality of life.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Saba HI, Roberts HR. Hemostasis and Thrombosis: Practical Guidelines in Clinical Management (Wiley Blackwell). 2014.
- DeLoughery TG. Hemostasis and Thrombosis 4th Edition (Springer). 2019.
- Keohane EM, Otto CN, Walenga JM. Rodak’s Hematology 6th Edition (Saunders). 2019.
- Kaushansky K, Levi M. Williams Hematology Hemostasis and Thrombosis (McGraw-Hill). 2017.
- Waheed SM, Kudaravalli P, Hotwagner DT. Deep Vein Thrombosis. [Updated 2023 Jan 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507708/
- Bates SM, Jaeschke R, Stevens SM, Goodacre S, Wells PS, Stevenson MD, Kearon C, Schunemann HJ, Crowther M, Pauker SG, Makdissi R, Guyatt GH. Diagnosis of DVT: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012 Feb;141(2 Suppl):e351S-e418S. doi: 10.1378/chest.11-2299. PMID: 22315267; PMCID: PMC3278048.
- Kearon C, Ageno W, Cannegieter SC, Cosmi B, Geersing GJ, Kyrle PA; Subcommittees on Control of Anticoagulation, and Predictive and Diagnostic Variables in Thrombotic Disease. Categorization of patients as having provoked or unprovoked venous thromboembolism: guidance from the SSC of ISTH. J Thromb Haemost. 2016 Jul;14(7):1480-3. doi: 10.1111/jth.13336. Epub 2016 Jun 7. PMID: 27428935.
- Su X, Yan B, Wang L, Cheng H, Chen Y. Comparative efficacy and safety of oral anticoagulants for the treatment of venous thromboembolism in the patients with different renal functions: a systematic review, pairwise and network meta-analysis. BMJ Open. 2022 Feb 21;12(2):e048619. doi: 10.1136/bmjopen-2021-048619. PMID: 35190410; PMCID: PMC8862458.
- Machin M, Younan H, Smith S, Salim S, Davies A, Shalhoub J. Systematic review on the benefit of graduated compression stockings in the prevention of venous thromboembolism in low-risk surgical patients. Phlebology. 2021;36(3):184-193. doi:10.1177/0268355520958590
- Kearon C, de Wit K, Parpia S, Schulman S, Spencer FA, Sharma S, Afilalo M, Kahn SR, Le Gal G, Shivakumar S, Bates SM, Wu C, Lazo-Langner A, D’Aragon F, Deshaies JF, Spadafora L, Julian JA. Diagnosis of deep vein thrombosis with D-dimer adjusted to clinical probability: prospective diagnostic management study. BMJ. 2022 Feb 15;376:e067378. doi: 10.1136/bmj-2021-067378. PMCID: PMC8845040.