TL;DR
Lead poisoning is a serious health concern, especially for children, caused by exposure to lead from various sources. Here’s a summary of the key points discussed:
- Sources of Exposure ▾: Common sources include lead-based paint (in older homes), contaminated soil and dust, lead in water pipes, and some imported products like toys and traditional remedies.
- How Lead Affects the Body ▾: Lead interferes with heme synthesis, disrupting red blood cell production and causing microcytic anemia. It’s also a neurotoxin, particularly harmful to developing brains.
- Symptoms ▾: Symptoms vary and can be subtle, especially with chronic exposure. In children, it can cause developmental delays, learning difficulties, and behavioral problems. In adults, it can lead to high blood pressure, joint pain, memory problems, and peripheral neuropathy.
- Diagnosis ▾: The most important test is a blood lead level (BLL) measurement. Other tests like CBC (looking for microcytic anemia and basophilic stippling) and erythrocyte protoporphyrin (EP/ZPP) can provide supporting evidence. There is no safe level of lead in blood, but reference values are used to identify higher exposure levels.
- Differential Diagnosis ▾: It’s important to differentiate lead poisoning from other conditions with similar symptoms, such as iron deficiency anemia, other heavy metal poisonings, ADHD, and certain neurological and gastrointestinal disorders.
- Treatment and Management ▾: The primary treatment is removing the source of exposure. Chelation therapy (using medications to bind and remove lead) is used for higher BLLs or symptomatic individuals. Supportive care and follow-up monitoring are also essential.
- Prevention ▾: Prevention is key and involves public health measures, education, occupational safety, and individual actions like testing homes, water, and toys for lead.
*Click ▾ for more information
Introduction
Lead, a naturally occurring heavy metal, has been utilized by humans for millennia due to its malleability, corrosion resistance, and low melting point. Its historical applications have been widespread, ranging from plumbing and construction in ancient civilizations to its use in paints, gasoline, and various industrial processes in more recent times. However, alongside its widespread use, the toxic effects of lead have been recognized for centuries. As early as the 2nd century BC, Greek physician Nicander documented symptoms suggestive of lead poisoning. Despite this early recognition, the widespread use of lead continued, leading to numerous instances of both acute and chronic poisoning throughout history.
Understanding lead poisoning remains crucial in modern medicine due to its continued prevalence, particularly in certain populations and regions. While significant efforts have been made to reduce lead exposure, cases still occur, and the long-term health consequences, especially in children, can be devastating. Lead’s toxicity affects multiple organ systems, but its impact on the hematological system is particularly significant and well-documented.
This article will focus specifically on the hematological effects of lead poisoning, exploring the mechanisms by which lead disrupts normal blood cell production and function, the resulting clinical manifestations, and the relevant laboratory investigations for diagnosis. We will also discuss the management and prevention strategies essential for mitigating the health burden of this preventable condition.
Definition of Lead Poisoning
Lead poisoning is defined as the presence of elevated levels of lead in the blood. While there is no known safe blood lead level, health organizations like the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) have established thresholds for intervention and public health action.
- World Health Organization (WHO): WHO states that a blood lead level of 5 µg/dL (micrograms per deciliter) or above is a cause for concern and requires action to reduce exposure.
- Centers for Disease Control & Prevention (CDC): The CDC uses a “reference level” to identify children with higher levels of lead in their blood compared to most U.S. children (97.5%). Currently, that level is 3.5 µg/dL. The CDC also recommends that pregnant women with a blood lead level (BLL) of 5 μg/dL or higher have their BLLs kept as low as possible. If their BLL is 10 μg/dL or higher, they should be removed from lead-exposed work areas.
Sources and Causes of Lead Exposure
Lead exposure can occur through various pathways, broadly categorized as occupational, environmental, and domestic.
Occupational Exposure
- Lead-related industries: Workers in industries that involve lead processing or use are at risk. This includes:
- Battery manufacturing and recycling
- Mining and smelting
- Construction and renovation (especially involving older buildings with lead paint)
- Plumbing
- Automotive repair (brake mechanics)
- Welding
- Exposure pathways: Lead can be inhaled as dust or fumes, or ingested through contaminated hands or food in the workplace.
Environmental Exposure
- Lead-based paint: A significant source, especially in homes built before 1978 (when lead paint was banned in the US). Deteriorating paint can create lead dust that children can inhale or ingest.
- Contaminated soil and dust: Lead from paint, gasoline (phased out in most countries), or industrial emissions can contaminate soil and household dust. Children playing in contaminated areas are at risk.
- Lead in water pipes: Older homes may have lead pipes or lead solder in copper pipes, which can leach lead into drinking water, especially if the water is acidic.
- Air pollution: Industrial emissions and past use of leaded gasoline have contributed to lead in the air, though levels have decreased significantly in many areas.
Domestic Exposure
- Imported products: Some imported products, such as toys, jewelry, traditional remedies, and certain food cans, may contain lead.
- Food contamination: Food can be contaminated through contact with lead-containing containers or during processing.
- Traditional remedies and cosmetics: Certain traditional medicines and cosmetics may contain lead.
- Hobbies: Activities like pottery (lead glazes), stained glass making, and gunsmithing can involve lead exposure.
Specific Risks for Children
Children are particularly vulnerable to lead poisoning due to:
- Increased absorption: Children absorb lead more readily than adults.
- Hand-to-mouth behavior: Young children often put their hands and objects in their mouths, increasing the risk of ingesting lead dust or contaminated items.
- Developing nervous system: Lead can have severe and irreversible effects on children’s developing brains and nervous systems.
Pathophysiology: The Hematological Impact of Lead
Mechanism of Lead Absorption, Distribution, and Storage in the Body
Lead can enter the body through three main routes:
- Ingestion: This is the most common route, especially for children who may ingest lead-contaminated dust, paint chips, or soil.
- Inhalation: Lead dust or fumes can be inhaled, particularly in occupational settings or areas with high air pollution.
- Dermal absorption: Although less efficient, lead can be absorbed through the skin, especially organic lead compounds.
Once lead enters the body, it undergoes a complex process of absorption, distribution, and storage.
Absorption
- Gastrointestinal tract: Lead absorption in the gut is influenced by factors like age (children absorb more), nutritional status (deficiencies in calcium, iron, or zinc increase absorption), and the chemical form of lead.
- Lungs: Inhaled lead particles can be directly absorbed into the bloodstream.
Distribution
- Blood: After absorption, lead enters the bloodstream and initially binds to red blood cells (RBCs). Approximately 99% of lead in the blood is found within RBCs, while the remaining 1% is in the plasma.
- Soft tissues: Lead is then distributed to various soft tissues, including the kidneys, liver, brain, and bone marrow. These organs initially accumulate higher concentrations of lead.
- Blood-brain barrier: Lead can cross the blood-brain barrier, posing a significant risk to the developing nervous system in children.
Storage
- Bones: Over time, the majority of lead is deposited and stored in bones, where it can remain for decades. Bones act as a reservoir for lead, and it can be released back into the bloodstream during periods of bone turnover, such as pregnancy, lactation, or osteoporosis.
Factors Affecting Lead Kinetics
- Age: Children absorb and retain lead more efficiently than adults.
- Nutritional status: Deficiencies in certain nutrients can increase lead absorption.
- Pregnancy and lactation: Lead stored in bones can be mobilized during pregnancy and lactation, exposing the developing fetus or infant.
Lead’s Interference with Heme Synthesis
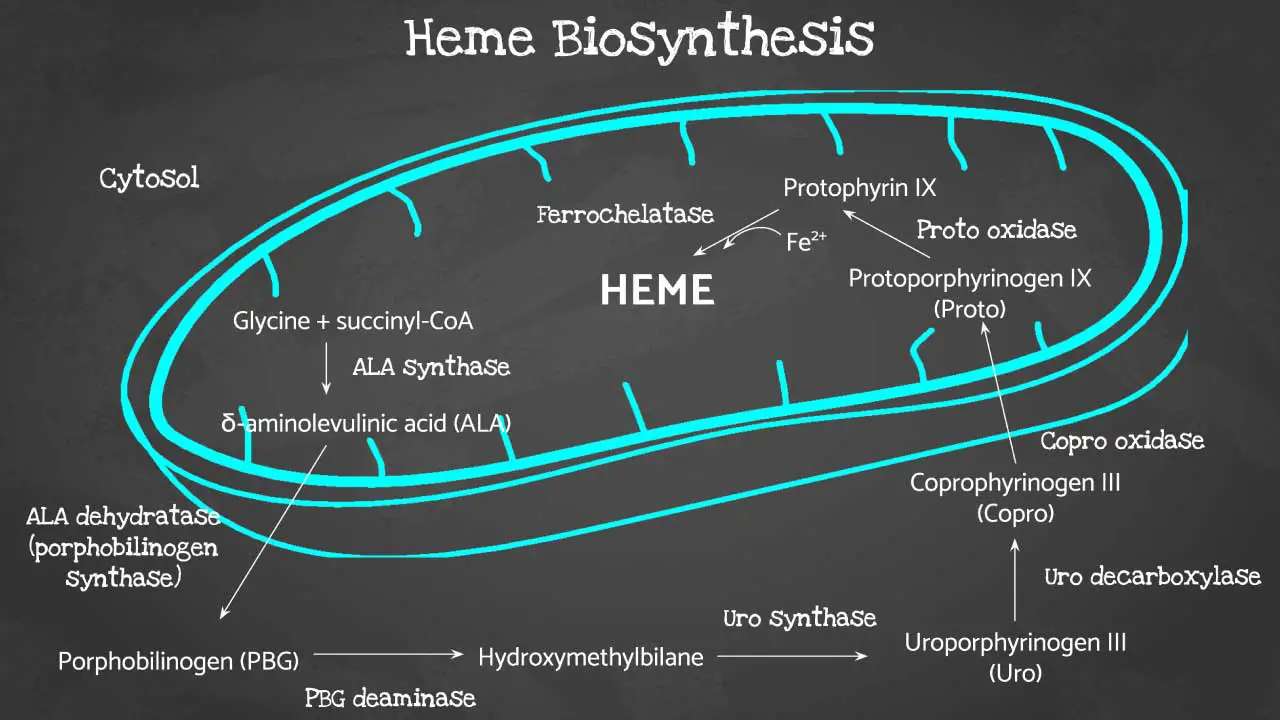
Lead exerts its toxic effects on the hematological system primarily by interfering with heme synthesis, the process by which red blood cells produce heme, a crucial component of hemoglobin that carries oxygen throughout the body. Lead disrupts this process by inhibiting several key enzymes in the heme synthesis pathway.
1. Inhibition of δ-aminolevulinic acid dehydratase (ALAD)
ALAD is an enzyme that catalyzes a crucial step in heme synthesis: the formation of porphobilinogen from δ-aminolevulinic acid (ALA). Lead strongly inhibits ALAD, leading to the accumulation of ALA in red blood cells, plasma, and urine. This inhibition is one of the earliest and most sensitive indicators of lead exposure.
2. Inhibition of ferrochelatase
Ferrochelatase is the enzyme responsible for the final step in heme synthesis: the insertion of iron into protoporphyrin to form heme. Lead inhibits ferrochelatase, thereby preventing the incorporation of iron into protoporphyrin. This leads to the accumulation of protoporphyrin in red blood cells, which can be measured as zinc protoporphyrin (ZPP) or free erythrocyte protoporphyrin (FEP).
Consequences of Lead’s Interference
- Decreased heme production: Inhibition of ALAD and ferrochelatase leads to a decrease in the overall production of heme.
- Impaired hemoglobin synthesis: Reduced heme availability impairs the synthesis of hemoglobin, the oxygen-carrying protein in red blood cells.
- Microcytic anemia: The impaired hemoglobin synthesis results in the production of smaller than normal red blood cells (microcytes), leading to microcytic anemia, a hallmark of lead poisoning.
- Accumulation of porphyrin precursors: The inhibition of enzymes in the heme synthesis pathway causes the accumulation of porphyrin precursors, such as ALA and protoporphyrin, which can have toxic effects on various tissues.
- Basophilic stippling: Lead’s interference with heme synthesis also affects the maturation of red blood cells, leading to the formation of basophilic stippling, which are granules of ribosomal RNA in the cytoplasm of red blood cells.
Side Effects of Lead Poisoning (Symptoms of Lead Poisoning)
Lead poisoning can present with a wide range of side effects (symptoms), which can vary depending on the level and duration of exposure, as well as the age of the individual. In many cases, especially with chronic exposure, side effects of lead poisoning may be subtle and develop gradually, making diagnosis challenging.
Distinguishing Between Acute and Chronic Lead Exposure/Poisoning
Lead poisoning can manifest in two main forms, depending on the duration and intensity of exposure.
Acute Lead Exposure: This occurs from a short-term, high-level exposure to lead. Side effects of lead poisoning can appear relatively quickly and may include:
- Severe abdominal pain and cramping
- Vomiting
- Muscle weakness
- Seizures
- Encephalopathy (brain dysfunction)
Chronic Lead Exposure: This results from prolonged exposure to lower levels of lead over an extended period. Side effects of lead poisoning develop gradually and are often non-specific, making diagnosis challenging. Chronic lead exposure can lead to:
- Fatigue
- Abdominal pain and constipation
- Irritability
- Difficulty concentrating
- Memory problems
- Anemia
- Developmental delays in children
Acute poisoning is less common than chronic poisoning due to increased awareness and regulation of lead exposure sources. Chronic poisoning is more prevalent and poses a significant public health concern due to its insidious nature and long-term health consequences.
Common Side Effects (Symptoms ) of Lead Poisoning
In Children
- Developmental delays: Lead can impair cognitive development, leading to learning difficulties, lower IQ scores, and behavioral problems.
- Learning difficulties: Children with lead poisoning may have trouble with attention, memory, and academic performance.
- Irritability: Increased irritability, mood swings, and hyperactivity are common.
- Loss of appetite: Lead can cause a decrease in appetite and lead to weight loss.
- Abdominal pain: Stomachaches, constipation, and vomiting can occur.
- Fatigue and lethargy: Children may appear tired, sluggish, and have decreased energy levels.
- Hearing loss: In some cases, lead poisoning can affect hearing.
- Seizures: In severe cases of lead poisoning, seizures can occur.
- Pica: Children with lead poisoning may develop pica, a condition characterized by craving and eating non-food items like paint chips or dirt.
In Adults
- High blood pressure
- Joint and muscle pain
- Difficulties with memory or concentration
- Headache
- Abdominal pain: Similar to children, adults may experience abdominal pain, constipation, and nausea.
- Mood disorders: Irritability, depression, and anxiety can be associated with lead exposure.
- Reduced sperm count and abnormal sperm
- Miscarriage, stillbirth, or premature birth in pregnant women
It’s important to note that many of these symptoms are non-specific and can be caused by other conditions. Therefore, a blood lead level test is necessary to confirm a diagnosis of lead poisoning.
Laboratory Investigations
Blood lead level (BLL) measurement
This is the most important and direct test for diagnosing lead poisoning. It measures the amount of lead present in whole blood, usually expressed in micrograms per deciliter (µg/dL).
Children: The Centers for Disease Control and Prevention (CDC) uses a blood lead reference value of 3.5 µg/dL (micrograms per deciliter). This means that children with blood lead levels at or above 3.5 µg/dL have higher levels than 97.5% of U.S. children.
Adults: A blood lead level of 5 µg/dL or above is generally considered elevated and may require further evaluation and action, especially in occupational settings.
It’s crucial to ensure the accuracy of BLL measurements, as contamination can lead to falsely elevated results. Elevated capillary BLL results should be confirmed with a venous blood sample. Blood lead levels should always be interpreted in the context of the individual’s clinical history, potential sources of exposure, and other relevant factors.
Complete blood count (CBC)
CBC can provide indirect evidence of lead poisoning by revealing characteristic changes in red blood cells. Red blood cells are smaller than normal with low mean corpuscular volume (MCV). Mean corpuscular hemoglobin (MCH) will also be low.
Peripheral blood smear
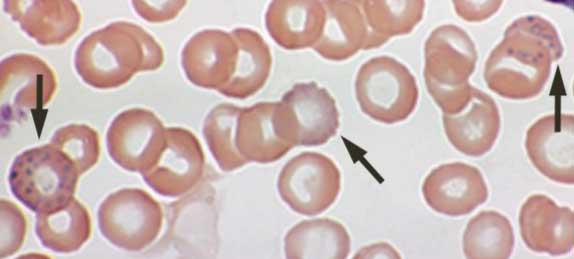
Hypochromic microcytic red blood cells can be seen in the peripheral blood smear. The presence of basophilic stippling in red blood cells on a peripheral blood smear is a characteristic but not specific finding in lead poisoning.
Erythrocyte Protoporphyrin (EP) or Zinc Protoporphyrin (ZPP) Measurement
While EP/ZPP levels can be elevated in lead poisoning, they can also be elevated in other conditions, such as iron deficiency anemia. Therefore, these tests are not as specific for lead poisoning as BLL measurement.
Other Tests
Renal function tests: Lead can affect kidney function, so tests like blood urea nitrogen (BUN) and creatinine may be performed.
X-ray fluorescence (XRF): This technique can be used to measure lead levels in bone, providing an estimate of cumulative lead exposure. However, it is not routinely used for diagnosis.
Differential Diagnosis
| Condition | Similarities to Lead Poisoning | Key Differences |
| Iron Deficiency Anemia | Microcytic anemia Fatigue Developmental delays (in children) | Low serum ferritin levels Responds to iron supplementation No basophilic stippling typically |
| Other Heavy Metal Poisonings (Arsenic, Mercury, Cadmium) | Neurological symptoms Gastrointestinal symptoms | Specific symptoms vary depending on the metal Different laboratory findings |
| Attention-Deficit/Hyperactivity Disorder (ADHD) | Behavioral problems Hyperactivity Difficulty concentrating | No microcytic anemia or basophilic stippling Normal blood lead levels |
| Learning Disabilities | Cognitive impairment Learning difficulties | No microcytic anemia or basophilic stippling Normal blood lead levels |
| Peripheral Neuropathies (Diabetic neuropathy, Vitamin deficiencies) | Numbness, tingling, weakness in extremities | Different underlying causes (diabetes, vitamin deficiency) Normal blood lead levels |
| Gastrointestinal Conditions (IBS, IBD) | Abdominal pain Constipation | Different gastrointestinal symptoms Normal blood lead levels |
| Other Causes of Developmental Delay | Developmental delays | Various underlying causes (genetic disorders, birth complications) Normal blood lead levels |
| Other Behavioral/Mood Disorders (Anxiety, Depression) | Irritability Mood swings | Different psychological symptoms Normal blood lead levels |
Treatment and Management of Lead Poisoning
The management of lead poisoning involves several key strategies aimed at reducing lead levels in the body and preventing further exposure.
Removal from the Source of Exposure
Identifying and eliminating the source: The most crucial step is to identify and eliminate the source of lead exposure. This may involve:
- Lead abatement in homes (removal or encapsulation of lead-based paint).
- Replacing lead pipes or plumbing fixtures.
- Improving workplace safety measures.
- Avoiding contaminated products or traditional remedies.
Environmental cleaning: Thorough cleaning of homes and other environments to remove lead dust is essential.
Chelation Therapy
Mechanism of action: Chelation therapy involves the use of medications called chelating agents that bind to lead in the blood and tissues, allowing it to be excreted in the urine.
Chelating agents: Several chelating agents are used in the treatment of lead poisoning, including:
- Succimer (Dimercaptosuccinic acid): An oral chelating agent commonly used for children with moderate lead poisoning.
- Edetate calcium disodium (CaNa2EDTA): Usually administered intravenously for higher lead levels or in cases where oral medication is not tolerated.
- Dimercaprol (British anti-Lewitsite): An intramuscular injection used in combination with EDTA for severe lead poisoning, especially in cases of encephalopathy.
Considerations: The decision to use chelation therapy depends on the blood lead level, the presence of symptoms, and the individual’s age and health status. Chelation therapy can have potential side effects, so it’s essential to monitor patients closely during treatment.
Supportive Care
Nutritional support: Ensuring adequate intake of iron, calcium, and vitamin C can help reduce lead absorption and mitigate some of its effects.
Management of symptoms: Treatment may be needed to address specific symptoms, such as anemia, abdominal pain, or neurological issues.
Developmental and educational interventions: Children with lead poisoning may benefit from early intervention programs and educational support to address any developmental or learning difficulties.
Follow-up Monitoring
Regular blood lead level checks: After treatment, it’s essential to monitor blood lead levels regularly to ensure they are decreasing and to detect any rebound in lead levels.
Ongoing assessment: Continued monitoring of the individual’s health and development is crucial to address any long-term effects of lead exposure.
Prevention
Public health measures: Implementing public health programs to reduce lead exposure in the environment, such as lead abatement programs and regulations on lead in products.
Education and awareness: Educating the public about the sources and risks of lead exposure and promoting preventive measures.
Occupational safety: Implementing strict occupational safety measures to protect workers in lead-related industries.
Blood Lead Testing: While environmental remediation is crucial, it’s equally important to know your family’s blood lead levels, especially for young children. Even low levels of lead in the blood can have lasting effects on development. Simple and reliable blood lead testing kits are available for home use, providing a convenient way to monitor your family’s health. Early detection allows for prompt intervention and can help mitigate potential health risks. If you are concerned about lead exposure, talk to your doctor about getting tested or consider using a home blood lead test kit.
At-home Lead Tests: Lead can leach into drinking water from lead pipes, lead solder in copper pipes, and even some brass faucets and fixtures, especially in older homes. This contamination is often invisible – you can’t see, taste, or smell lead in water. Lead-based paint in older homes remains a significant source of exposure. If you live in a pre-1978 home, it’s crucial to test surfaces for lead, particularly areas that children may come into contact with, such as window sills, door frames, and painted toys. Lead paint on toys can pose a serious health risk to children, especially when they put toys in their mouths. While lead paint was banned in the United States in 1978, some older toys and imported toys may still contain lead. Easy-to-use lead testing kits are available for home use, allowing you to quickly identify potential hazards.
Frequently Asked Questions (FAQs)
What foods are high in lead?
While lead isn’t intentionally added to food, contamination can occur. Imported spices (like turmeric and chili powder) and candies, root vegetables and leafy greens grown in contaminated soil, food stored in improperly glazed pottery or lead crystal, and certain traditional remedies/cosmetics can have higher lead levels. Food regulations and monitoring help minimize risks, but choosing reputable sources and a varied diet further reduces potential exposure.
What is the most common source of lead poisoning?
The most common source of lead poisoning, particularly for children, is lead-based paint and lead-contaminated dust found in older homes. Lead-based paint was used extensively in homes built before 1978 (when it was banned in the US). Many of these homes still contain lead paint on walls, woodwork, and other surfaces. As lead paint deteriorates, it can chip, peel, or flake, creating lead-contaminated dust. This dust can settle on surfaces, and children can ingest it through hand-to-mouth contact or by putting contaminated objects in their mouths. Home renovation activities like sanding, scraping, or demolition can disturb lead paint and generate hazardous lead dust.
While other sources like contaminated water, soil, and certain imported products can contribute to lead exposure, lead-based paint and lead dust remain the most significant sources of lead poisoning, especially in children.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- https://www.who.int/news/item/27-10-2021-who-guidance-to-reduce-illness-due-to-lead-exposure
- https://www.cdc.gov/lead-prevention/php/data/blood-lead-surveillance.html
- Hon KL, Fung CK, Leung AK. Childhood lead poisoning: an overview. Hong Kong Med J. 2017 Dec;23(6):616-21. doi: 10.12809/hkmj176214. Epub 2017 Oct 13. PMID: 29026055.
- Walter K. What Is Lead Poisoning? JAMA. 2023 Mar 28;329(12):1040. doi: 10.1001/jama.2023.1543. PMID: 36897599.



