TL;DR
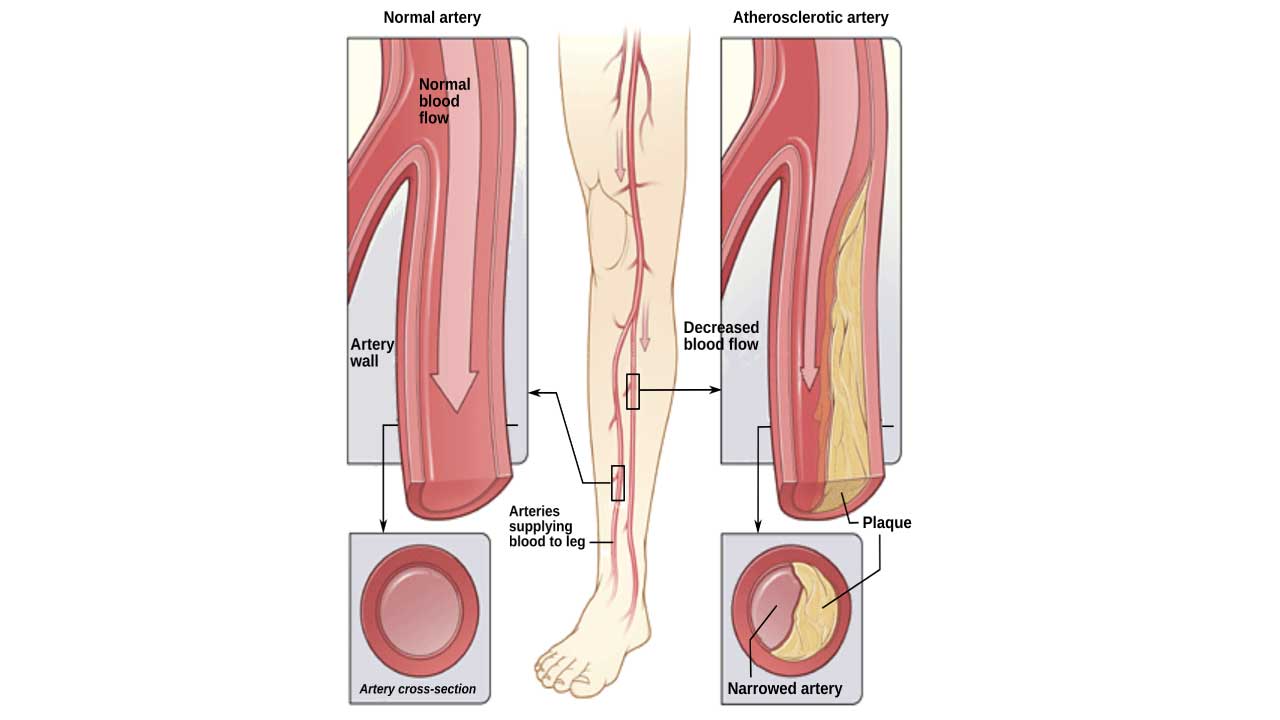
Peripheral artery disease (PAD) is the narrowing of arteries outside the heart, primarily in the legs, due to atherosclerosis.
- Cause ▾: Atherosclerosis (plaque buildup) is the main cause.
- Symptoms ▾: Intermittent claudication (leg pain with exercise), rest pain, non-healing wounds, and cold extremities.
- Risk Factors ▾: Smoking, diabetes, high cholesterol, and hypertension.
- Diagnosis ▾: Clinical examination (pulses), Ankle-Brachial Index (ABI), and imaging studies.
- Treatment ▾: Lifestyle changes, medications, and revascularization procedures.
- Prevention: Risk factor modification and healthy lifestyle.
*Click ▾ for more information
Introduction
Peripheral artery disease (PAD) is a specific type of peripheral vascular disease (PVD) that primarily affects the arteries. Specifically, peripheral artery disease (PAD) involves the narrowing or blockage of arteries, most commonly in the legs, due to atherosclerosis. This narrowing restricts blood flow to the extremities, leading to symptoms like intermittent claudication. Peripheral vascular disease (PVD) is a broad term encompassing any disorder affecting blood vessels outside the heart and brain, including both arteries and veins.
Peripheral artery disease (PAD) is a significant public health concern due to its considerable prevalence and far-reaching impact. Affecting millions worldwide, its prevalence increases with age, particularly in individuals with established risk factors such as diabetes, smoking, and hypertension. Notably, peripheral artery disease (PAD) is often underdiagnosed, as many individuals remain asymptomatic, delaying crucial interventions. The impact of peripheral artery disease (PAD) extends beyond mere discomfort, significantly diminishing quality of life through symptoms like intermittent claudication, which limits physical activity and daily functioning.
Understanding peripheral artery disease (PAD) from a hematological standpoint is crucial because blood and its components play a fundamental role in the disease’s pathogenesis and progression.
Pathophysiology of Peripheral Artery Disease
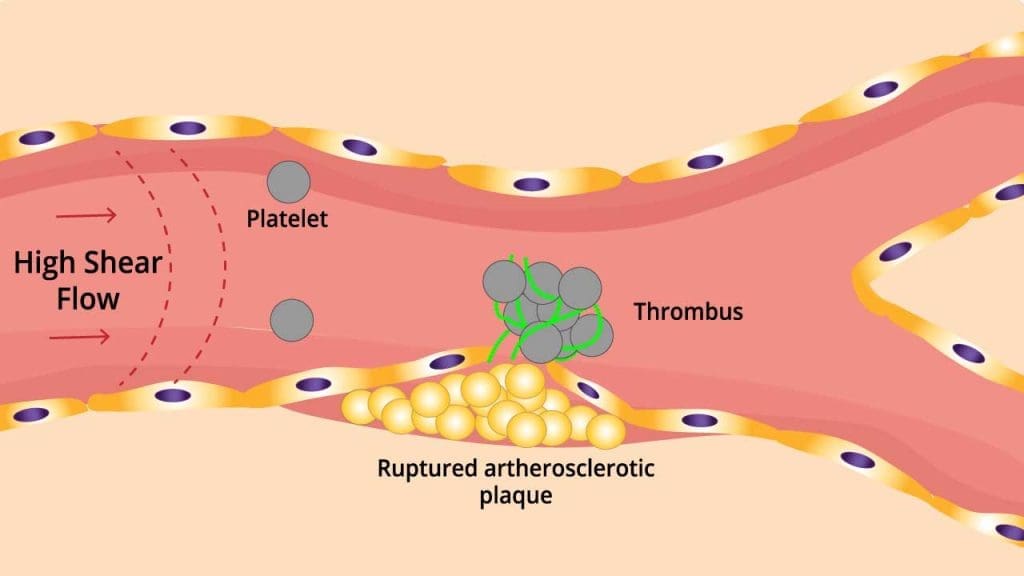
The pathophysiology of peripheral artery disease (PAD) primarily revolves around atherosclerosis, a chronic inflammatory process that leads to the narrowing and eventual blockage of peripheral arteries, most commonly in the lower extremities. This process begins with endothelial dysfunction, where the inner lining of the arteries becomes damaged due to risk factors like smoking, hypertension, hyperlipidemia, and diabetes. This damage allows low-density lipoprotein (LDL) cholesterol to accumulate in the arterial wall, triggering an inflammatory response.
Monocytes and T lymphocytes are recruited to the site, transforming into macrophages that engulf the accumulated LDL, forming foam cells. These foam cells, along with smooth muscle cells, contribute to the formation of atherosclerotic plaques. As these plaques grow, they narrow the arterial lumen, reducing blood flow. This reduced blood flow leads to ischemia, particularly during exertion, resulting in symptoms like intermittent claudication.
Furthermore, the plaque’s composition plays a critical role. Unstable or vulnerable plaques, characterized by a thin fibrous cap and a large lipid core, are prone to rupture.
Plaque rupture triggers platelet activation and aggregation, leading to thrombus formation, which can further obstruct blood flow or cause acute occlusion. Additionally, hematological factors such as increased platelet reactivity, hypercoagulability, and reduced red blood cell deformability exacerbate the ischemic process. In severe cases, chronic ischemia can progress to critical limb ischemia, characterized by rest pain, non-healing ulcers, and gangrene, ultimately threatening limb viability.
Other Causes (Less Common)
- Vasculitis: This involves inflammation of the blood vessels. Examples include:
- Buerger’s disease (thromboangiitis obliterans): Strongly associated with tobacco use.
- Takayasu arteritis: Affects large arteries, including the aorta and its branches.
- Fibromuscular dysplasia: This condition involves abnormal cell growth in the artery walls, leading to narrowing of the arteries.
- Trauma: Injuries to the arteries can cause damage that leads to narrowing or blockage.
- Blood clots (Thrombosis): Though often a consequence of atherosclerotic plaques, blood clots forming elsewhere can also cause blockages.
- Radiation exposure: Radiation can damage blood vessels, potentially leading to peripheral artery disease (PAD).
Risk Factors that contribute to atherosclerosis, and thus PAD:
- Smoking
- Diabetes
- High cholesterol
- High blood pressure
- Older age
- Family history of PAD, heart disease, or stroke
- Obesity
- A sedentary lifestyle
Signs and Symptoms of Peripheral Artery Disease
Peripheral artery disease (PAD) can manifest in a variety of ways, and it’s important to recognize that many individuals may be asymptomatic, particularly in the early stages. The severity of symptoms can vary widely depending on the degree of arterial blockage. It is important to note that people with diabetes may have less pain, because of diabetic neuropathy. Therefore, they may have severe peripheral artery disease (PAD) without having severe pain.
Key Symptoms
- Intermittent Claudication: This is the hallmark symptom of peripheral artery disease (PAD). It’s characterized by muscle pain or cramping in the legs (most commonly the calves), thighs, or buttocks that occur during exercise, such as walking. The pain is typically relieved by rest within a few minutes.
- Rest Pain: In more severe peripheral artery disease (PAD), pain may occur even at rest, particularly in the feet and toes. This pain is often worse at night and may be relieved by hanging the feet over the edge of the bed or sitting in a chair.
- Non-Healing Wounds: Reduced blood flow can impair the body’s ability to heal, leading to slow-healing or non-healing sores or ulcers on the feet and toes.
- Changes in Skin Appearance: The skin on the legs and feet may become:
- Cool to the touch.
- Pale or bluish in color.
- Shiny or smooth.
- Thin or fragile.
- Hair loss on the legs and feet can also occur.
- Weak or Absent Pulses: Diminished or absent pulses in the feet or legs are a significant sign of PAD.
- Other Symptoms:
- Numbness or tingling in the legs or feet.
- Weakness in the legs.
- Slow toenail growth.
- Erectile dysfunction (in men).

Fontaine and Rutherford Classification of PAD
The Fontaine and Rutherford classifications are two systems used to stage the severity of peripheral artery disease (PAD). They help clinicians assess the progression of the disease and guide treatment decisions.
Fontaine Classification
This is an older, simpler system that primarily focuses on the presence and severity of claudication.
| Stage | Description |
| I | Asymptomatic |
| IIa | Intermittent claudication > 200 meters |
| IIb | Intermittent claudication < 200 meters |
| III | Rest pain |
| IV | Tissue loss (ulcers or gangrene) |
Rutherford Classification
The Rutherford classification provides a more granular assessment of claudication severity. It incorporates objective findings, such as ankle-brachial index (ABI) values, in addition to subjective symptoms. It more accurately reflects the progression of PAD, particularly in the later stages. The Rutherford classification is more useful for clinical and research purposes.
| Grade | Category | Description |
| 0 | 0 | Asymptomatic |
| I | 1 | Mild Claudication |
| I | 2 | Moderate Claudication |
| I | 3 | Severe Claudication |
| II | 4 | Rest Pain |
| II | 5 | Minor Tissue Loss |
| III | 6 | Major Tissue 1 Loss |
Approach to PAD Diagnosis
Clinical examination
A thorough clinical examination is essential for the diagnosis and assessment of peripheral artery disease (PAD). It involves a combination of visual inspection, palpation, and non-invasive measurements.
Patient History
- Symptom Assessment
- Detailed inquiry about claudication: onset, duration, distance walked before pain, location of pain, and relief with rest.
- Presence of rest pain: location, severity, and factors that alleviate or exacerbate it.
- History of non-healing wounds, ulcers, or gangrene.
- Other symptoms: numbness, tingling, coldness, or color changes in the extremities.
- Risk Factor Evaluation
- Smoking history: duration and intensity.
- Diabetes mellitus: duration, control, and complications.
- Hypertension: duration and treatment.
- Hyperlipidemia: lipid profile and treatment.
- Family history of PAD, coronary artery disease, or stroke.
- Other risk factors: obesity, sedentary lifestyle, and chronic kidney disease.
Physical Examination
- Skin Changes
- Color: pallor, cyanosis, or rubor (redness).
- Temperature: coolness of the extremities.
- Trophic changes: thin, shiny skin; loss of hair; thickened toenails.
- Presence of ulcers or gangrene: location, size, and characteristics.
- Leg Elevation and Dependency
- Elevation pallor: observe for pallor when the legs are elevated.
- Dependent rubor: observe for redness when the legs are dependent.
Palpation
- Peripheral Pulses
- Palpate the femoral, popliteal, dorsalis pedis, and posterior tibial pulses.
- Assess the strength of the pulses: graded on a scale of 0 (absent) to 3+ (bounding).
- Compare pulses between limbs.
- Capillary Refill Time
- Press on a toenail or fingertip and observe the time it takes for color to return.
- Prolonged capillary refill time indicates reduced blood flow.
Auscultation
- Arterial Bruits
- Listen for bruits (abnormal sounds) over the femoral and abdominal arteries.
- Bruits may indicate turbulent blood flow due to arterial stenosis.
Non-Invasive Measurements
- Ankle-Brachial Index (ABI)
- This is the most important non-invasive test for PAD.
- Measure systolic blood pressure in the brachial arteries and the ankle arteries (dorsalis pedis and posterior tibial).
- Calculate the ABI by dividing the ankle systolic pressure by the brachial systolic pressure.
- ABI interpretation:
- 1.0–1.4: Normal.
- 0.91–0.99: Borderline.
- ≤ 0.90: Diagnostic of PAD.
- <0.4: severe PAD
- 1.4: calcified vessels, common in diabetics, makes the ABI unreliable.
- Toe-Brachial Index (TBI)
- Useful in patients with calcified leg vessels, especially diabetics, where ABI is unreliable.
- Segmental Limb Pressures
- Measure blood pressure at different levels of the leg to localize the site of arterial stenosis.
- Duplex Ultrasonography
- Uses ultrasound to visualize blood flow and assess arterial stenosis.
- Exercise Testing
- Treadmill exercise testing can be used to assess claudication distance and severity.
Laboratory Investigations
Laboratory investigations play a crucial role in the assessment and management of peripheral artery disease (PAD), primarily by identifying risk factors, evaluating disease severity, and detecting associated comorbidities. While imaging studies are essential for visualizing arterial blockages, lab tests provide valuable information about the patient’s overall health and risk profile.
Complete Blood Count (CBC): Anemia can exacerbate PAD symptoms, while elevated white blood cell counts may indicate infection or inflammation. Platelets play a role in clot formation.
Coagulation Studies: To assess for hypercoagulability, which can contribute to thrombosis and embolic events.
- Tests:
- Prothrombin time (PT) and international normalized ratio (INR)
- Partial thromboplastin time (PTT)
- D-dimer.
- Expected Findings: These tests are generally within normal limits in PAD unless there’s a specific coagulation disorder or the patient is on anticoagulation therapy. D-dimer may be elevated in cases of acute thrombosis or embolism.
Lipid Profile: To assess for hyperlipidemia, a major risk factor for atherosclerosis.
- Tests:
- Total cholesterol
- LDL cholesterol (low-density lipoprotein)
- HDL cholesterol (high-density lipoprotein)
- Triglycerides
- Expected Findings: Elevated LDL cholesterol and triglycerides increase the risk of atherosclerosis. Low HDL cholesterol is also a risk factor.
Inflammatory Markers: To assess for systemic inflammation, which plays a role in atherosclerosis.
- Tests:
- C-reactive protein (CRP)
- Erythrocyte sedimentation rate (ESR)
- Expected Findings: Elevated CRP and ESR may indicate systemic inflammation, although they are not specific for PAD.
Blood Glucose and HbA1c: To assess for diabetes mellitus, a significant risk factor for PAD and a condition that often exacerbates it.
- Tests:
- Fasting blood glucose
- HbA1c (glycated hemoglobin)
- Expected Findings: Elevated fasting blood glucose or HbA1c indicates diabetes or impaired glucose tolerance. Poor glycemic control increases the risk of PAD and its complications.
Renal Function Tests: To assess for chronic kidney disease, which is a common comorbidity in PAD.
- Tests:
- Serum creatinine
- Estimated glomerular filtration rate (eGFR)
- Expected Findings: Elevated serum creatinine and decreased eGFR indicate impaired renal function.
Other Tests (When Indicated):
- Homocysteine: Elevated levels may be a risk factor for atherosclerosis.
- Lipoprotein(a): Elevated levels may be a risk factor for atherosclerosis.
- Genetic testing: In rare cases, to identify specific genetic predispositions.
- Autoimmune testing: When vasculitis is suspected.
Imaging Studies
Imaging studies are crucial in the diagnosis, localization, and assessment of the severity of peripheral artery disease (PAD).
They provide detailed anatomical and functional information that complements the clinical examination and laboratory findings.
Duplex Ultrasonography: Combines traditional ultrasound with Doppler ultrasound to visualize blood flow and assess arterial stenosis. It is mon-invasive, readily available, relatively inexpensive, and can be performed at the bedside.
- Uses:
- Detecting and localizing arterial stenosis or occlusion.
- Assessing the severity of stenosis.
- Evaluating blood flow patterns.
- Monitoring the progression of PAD.
- Post-intervention surveillance.
- Limitations: Can be limited by calcifications, obesity, and bowel gas.
Computed Tomographic Angiography (CTA): Uses CT scans with intravenous contrast to visualize the arterial system. It provides detailed anatomical images of the arteries, including calcifications.
- Uses:
- Diagnosing and localizing PAD.
- Planning revascularization procedures.
- Evaluating the extent of disease.
- Limitations: Requires intravenous contrast (risk of contrast-induced nephropathy), radiation exposure, and can overestimate stenosis due to calcifications.
Magnetic Resonance Angiography (MRA): Uses magnetic fields and radio waves to visualize the arterial system. Can be performed with or without intravenous contrast (gadolinium). It provides detailed anatomical images, excellent soft-tissue contrast, and can be performed without ionizing radiation (in non contrast enhanced versions).
- Uses:
- Diagnosing and localizing PAD.
- Planning revascularization procedures.
- Evaluating the extent of disease.
- Limitations: Can be limited by calcifications, patient claustrophobia, and the need for gadolinium contrast (risk of nephrogenic systemic fibrosis in patients with severe renal impairment).
Digital Subtraction Angiography (DSA): An invasive procedure that involves injecting contrast directly into the arteries through a catheter and taking real-time X-ray images. It provides the highest resolution images of the arteries and is considered the “gold standard” for diagnosing and planning revascularization.
- Uses:
- Definitive diagnosis of PAD.
- Planning and performing revascularization procedures (angioplasty, stenting).
- Evaluating the results of interventions.
- Limitations: Invasive (risk of complications), requires specialized equipment and expertise, and involves radiation exposure and contrast administration.
The choice of imaging modality depends on the clinical situation, patient risk factors, and available resources. Duplex ultrasonography is often the initial imaging test of choice. CTA or MRA is typically used for further evaluation and planning of revascularization. DSA is reserved for cases requiring intervention or when other imaging studies are inconclusive.
It is important to utilize the imaging modality that will gain the most pertinent information, while using the least invasive technique possible.
Treatment and Management of Peripheral Artery Disease
The treatment and management of peripheral artery disease (PAD) aim to alleviate symptoms, improve functional capacity, prevent disease progression, and reduce the risk of cardiovascular events. It involves a combination of lifestyle modifications, pharmacological therapy, interventional procedures, and surgical revascularization.
Lifestyle Modifications
- Smoking Cessation: This is the single most important intervention. Smoking significantly accelerates atherosclerosis and worsens PAD.
- Exercise Therapy: Supervised exercise programs, particularly treadmill walking, can improve claudication symptoms and increase walking distance. Regular exercise promotes collateral artery development, improving blood flow.
- Dietary Changes: A heart-healthy diet low in saturated and trans fats, cholesterol, and sodium is recommended. There must be an emphasis on fruits, vegetables, whole grains, and lean protein.
- Weight Management: Maintaining a healthy weight reduces the burden on the cardiovascular system and improves overall health.
- Foot Care: Meticulous foot care is essential, especially for individuals with diabetes or severe peripheral artery disease (PAD). Individuals should regularly inspect their feet for any signs of injury or infection. Proper footwear is essential to prevent trauma.
Pharmacological Therapy
- Antiplatelet Agents: Aspirin or clopidogrel are used to reduce the risk of thrombotic events. These medications inhibit platelet aggregation and prevent clot formation.
- Lipid-Lowering Medications: Statins are used to lower LDL cholesterol levels and reduce the progression of atherosclerosis. They also have pleiotropic effects, such as improving endothelial function.
- Antihypertensive Medications: Controlling blood pressure is crucial to reduce the risk of cardiovascular events. Various classes of antihypertensive medications may be used.
- Medications to Improve Claudication Symptoms:
- Cilostazol: A phosphodiesterase inhibitor that improves walking distance by inhibiting platelet aggregation and promoting vasodilation.
- Pentoxifylline: Less effective, but sometimes used to improve blood flow.
- Management of Diabetes: Tight glycemic control is vital. Medications and lifestyle changes are used to achieve target blood sugar levels.
Interventional Procedures
- Angioplasty and Stenting: A minimally invasive procedure where a catheter with a balloon is inserted into the narrowed artery. The balloon is inflated to widen the artery, and a stent may be placed to maintain patency.
- Atherectomy: A procedure where plaque is removed from the artery using a catheter with a cutting device.
- Thrombolysis: Introduction of thrombolytic drugs into the affected artery to dissolve a clot.
Surgical Revascularization
- Bypass Grafting: A surgical procedure where a graft (either a vein or a synthetic graft) is used to bypass the blocked artery. This is typically reserved for severe peripheral artery disease (PAD) or when interventional procedures are not feasible.
- Amputation: In severe cases of critical limb ischemia with irreversible tissue loss, amputation may be necessary.
Management of Complications
- Wound Care: Aggressive wound care is essential for non-healing ulcers and gangrene. This may involve debridement, antibiotics, and specialized dressings.
- Infection Control: Prompt treatment of any infection.
- Pain Management: Management of pain is important for quality of life.
Follow-up and Surveillance
- Regular monitoring of symptoms, pulses, and ABI.
- Periodic lipid profile and blood glucose testing.
- Cardiovascular risk factor management.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Bierowski M, Galanis T, Majeed A, Mofid A. Peripheral Artery Disease: Overview of Diagnosis and Medical Therapy. Med Clin North Am. 2023 Sep;107(5):807-822. doi: 10.1016/j.mcna.2023.05.007. Epub 2023 Jul 3. PMID: 37541709.
- Gornik HL, Aronow HD, Goodney PP, Arya S, Brewster LP, Byrd L, Chandra V, Drachman DE, Eaves JM, Ehrman JK, Evans JN, Getchius TSD, Gutiérrez JA, Hawkins BM, Hess CN, Ho KJ, Jones WS, Kim ESH, Kinlay S, Kirksey L, Kohlman-Trigoboff D, Long CA, Pollak AW, Sabri SS, Sadwin LB, Secemsky EA, Serhal M, Shishehbor MH, Treat-Jacobson D, Wilkins LR; Peer Review Committee Members. 2024 ACC/AHA/AACVPR/APMA/ABC/SCAI/SVM/SVN/SVS/SIR/VESS Guideline for the Management of Lower Extremity Peripheral Artery Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2024 Jun 11;149(24):e1313-e1410. doi: 10.1161/CIR.0000000000001251. Epub 2024 May 14. PMID: 38743805.
- Fowkes FG, Aboyans V, Fowkes FJ, McDermott MM, Sampson UK, Criqui MH. Peripheral artery disease: epidemiology and global perspectives. Nat Rev Cardiol. 2017 Mar;14(3):156-170. doi: 10.1038/nrcardio.2016.179. Epub 2016 Nov 17. PMID: 27853158.
- Beckman JA, Schneider PA, Conte MS. Advances in Revascularization for Peripheral Artery Disease: Revascularization in PAD. Circ Res. 2021 Jun 11;128(12):1885-1912. doi: 10.1161/CIRCRESAHA.121.318261. Epub 2021 Jun 10. PMID: 34110904.



