TL;DR
Embolus or embolism is a moving blood clot or foreign object that travels through the bloodstream. When it lodges in a blood vessel, it can block blood flow and cause serious complications.
- Origin ▾: Often originates from a blood clot (thrombus) in a vein, but can also be caused by other foreign objects.
- Types ▾: Pulmonary embolism (PE) is the most common type, but others include cerebral, coronary, and mesenteric emboli.
- Complications ▾: Can lead to severe consequences like organ damage, stroke, and even death.
- Prevention ▾: Managing underlying risk factors for thrombosis, such as lifestyle changes and medical treatments, can help prevent emboli.
- Treatment ▾: Anticoagulant medications, thrombolytics, and in some cases, surgical intervention may be necessary to treat emboli.
Early detection and prompt treatment are crucial to prevent the severe consequences of embolism.
*Click ▾ for more information
Introduction
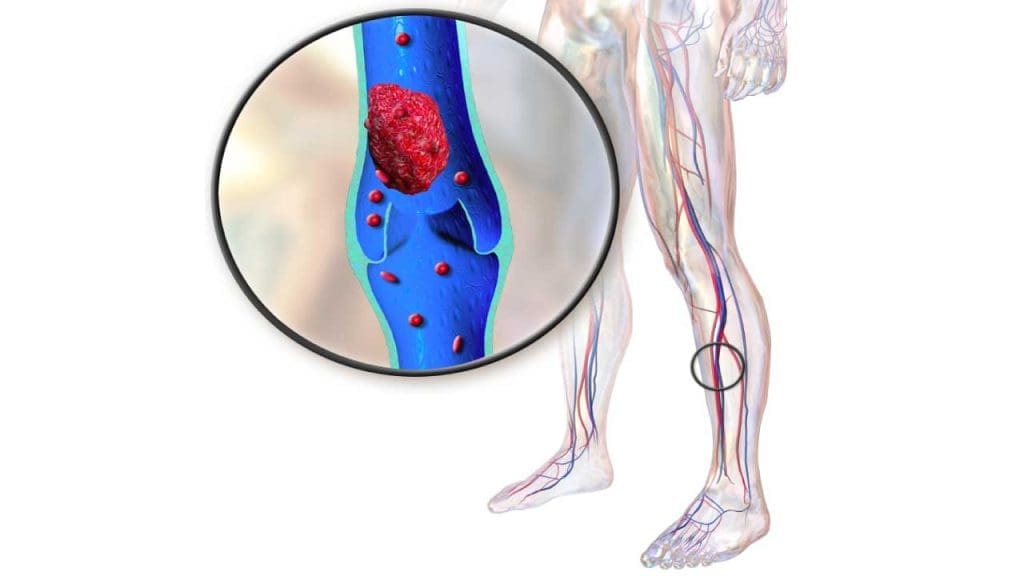
An embolus is a moving blood clot or other foreign object that travels through the bloodstream. When an embolus blocks a blood vessel, it can lead to serious complications. For instance, a blood clot that forms in a leg vein (deep vein thrombosis) can break off and travel to the lungs, causing a pulmonary embolism.
Thrombosis is the formation of a blood clot, or thrombus, within a blood vessel. This clot can partially or completely block blood flow, leading to serious health consequences.
The Formation of a Blood Clot
- Injury: When a blood vessel is damaged, platelets (cell fragments) gather at the site.
- Platelet Plug: Platelets stick together to form a temporary plug to stop bleeding.
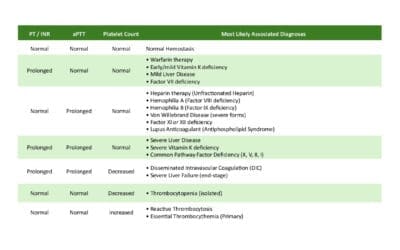
- Coagulation Cascade: A series of proteins in the blood plasma (clotting factors) are activated, leading to the production of fibrin, a protein that strengthens the platelet plug.
- Clot Formation: The fibrin traps red blood cells, creating a stable clot.
However, sometimes this process goes awry, and clots can form in inappropriate places or become too large.
Understanding Embolism
A blood clot or other foreign substance can travel through the bloodstream as an embolus, potentially blocking vital blood vessels.
How a Thrombus Becomes an Embolus
A blood clot (thrombus) can become an embolus when it breaks loose from its original location. This can happen due to factors like:
- Flow disturbances: Turbulence or changes in blood flow can dislodge a clot.
- Degradation: The clot itself may deteriorate, making it more likely to break apart.
- Underlying conditions: Certain medical conditions (e.g., atrial fibrillation) can increase the risk of clot formation and detachment.
Types of Emboli
While blood clots are the most common type of embolus, other foreign objects can also travel through the bloodstream, including:
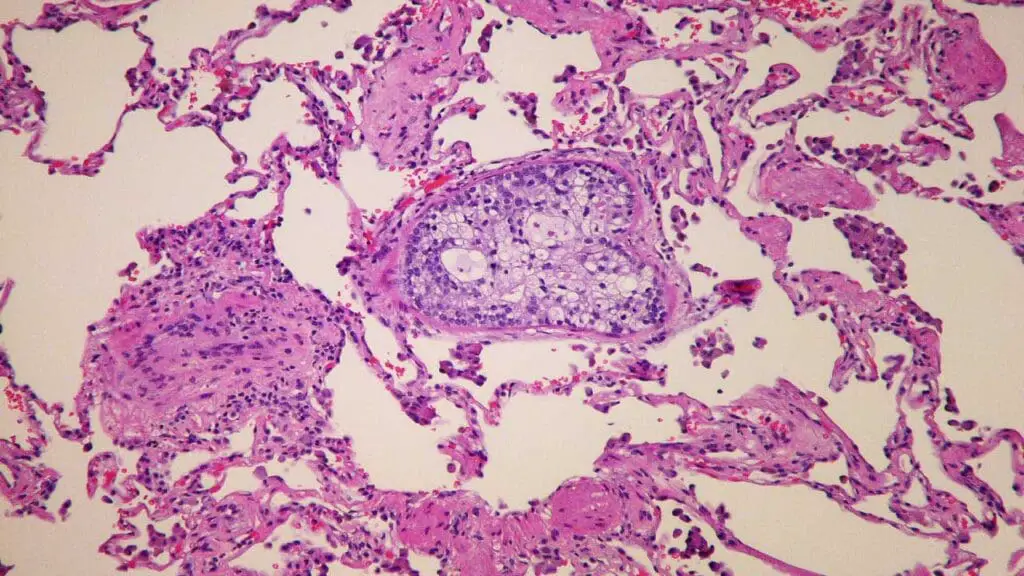
- Fat emboli: Fragments of fat tissue, often released after a severe injury or surgery, can enter the bloodstream.
- Air emboli: Air bubbles can enter the bloodstream, typically after trauma or medical procedures involving needles.
- Amniotic fluid emboli: Amniotic fluid can enter the bloodstream during childbirth, leading to a life-threatening condition.
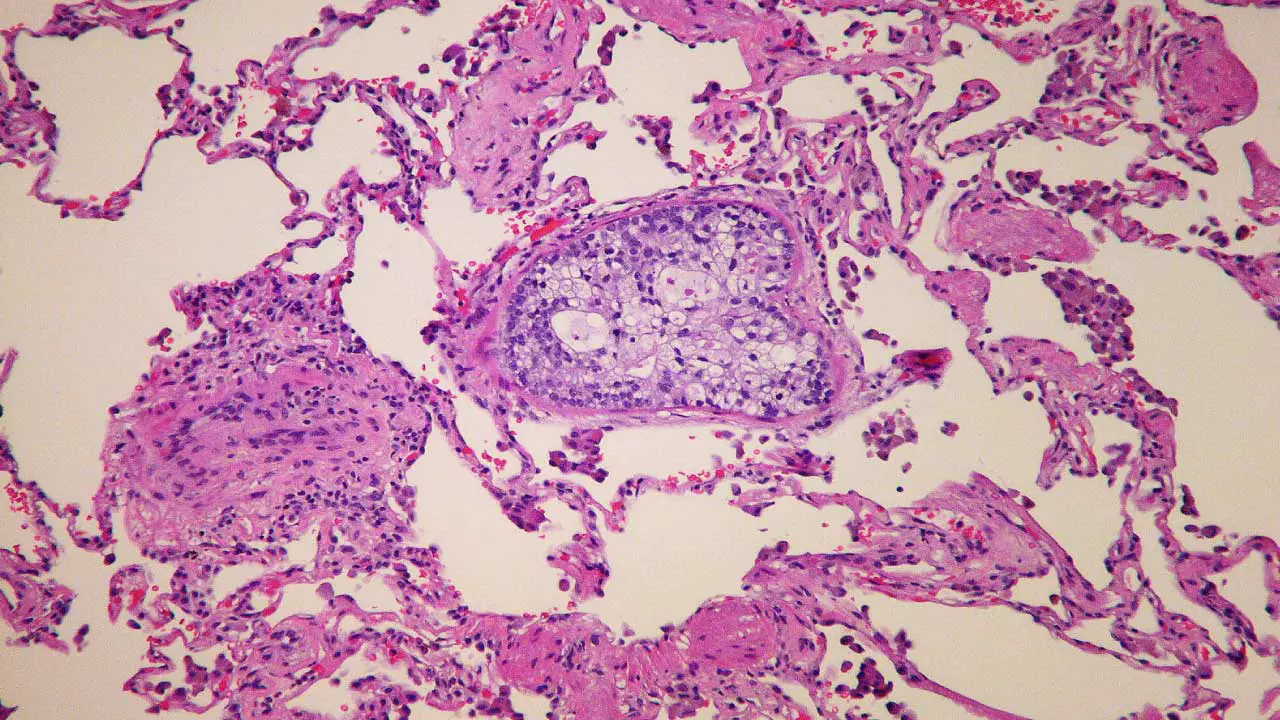
- Tumor emboli: Fragments of a tumor can break off and travel through the bloodstream, potentially spreading the cancer to other organs.
It’s important to note that not all emboli cause symptoms, and some may be absorbed by the body without causing harm. However, when an embolus lodges in a vital organ, it can have serious consequences.
The Dangers of Embolism
Pulmonary Embolism (PE)
- Most common type of embolism: PE occurs when a blood clot (embolus) travels from a vein, often in the leg (DVT), to the lungs.
- Life-threatening: PE can block blood flow to the lungs, leading to shortness of breath, chest pain, and potentially, death.
- Symptoms: Sudden onset of shortness of breath, chest pain, coughing (may bring up blood), rapid heart rate, lightheadedness, or fainting.
Deep Vein Thrombosis (DVT) and Its Link to PE
- Common source of PE: DVT is a frequent precursor to PE. When a blood clot forms in a deep vein, especially in the leg, it can break loose and travel to the lungs.
- Risk factors for DVT: Surgery, prolonged immobility, obesity, pregnancy, and certain medical conditions can increase the risk of DVT and, consequently, PE.
Other Types of Embolism
- Cerebral Embolism: A clot that travels to the brain can cause a stroke.
- Coronary Embolism: A clot that travels to the heart can lead to a heart attack.
- Mesenteric Embolism: A clot that travels to the intestines can cause severe abdominal pain and tissue damage.
- Renal Embolism: A clot that travels to the kidneys can lead to kidney failure.
Long-Term Consequences of Embolism
- Pulmonary embolism: Even if a PE is treated successfully, it can cause long-term damage to the lungs.
- Deep vein thrombosis: Untreated or recurrent DVT can lead to post-thrombotic syndrome, a condition characterized by pain, swelling, and skin changes in the affected leg.
- Other embolisms: The long-term consequences can vary depending on the organ affected and the severity of the blockage.
It’s important to note that early detection and treatment of thrombosis and embolism are crucial to prevent severe complications.
Prevention
Early detection of thrombosis and embolism is crucial to prevent serious complications. Symptoms like leg pain, swelling, shortness of breath, and chest pain should be taken seriously and prompt medical attention sought.
Risk Factors for Thrombosis
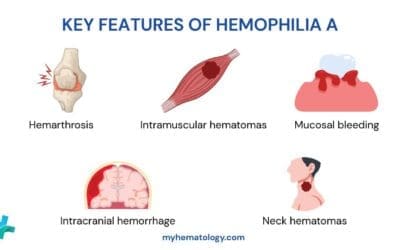
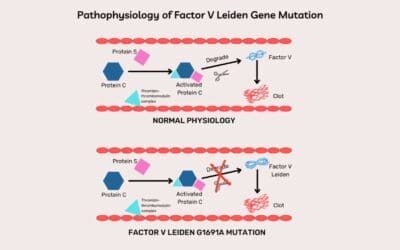
- Inherited Factors: Genetic conditions like Factor V Leiden, prothrombin gene mutation, and protein C/S deficiencies can increase the risk.
- Acquired Factors:
- Lifestyle: Smoking, obesity, sedentary lifestyle
- Medical Conditions: Cancer, pregnancy, inflammatory bowel disease, heart disease
- Medications: Hormonal therapy, birth control pills, certain medications for medical conditions
- Surgery and Immobilization: Prolonged periods of inactivity, especially after surgery, can increase the risk thrombosis which may lead to the formation of an embolus.
Lifestyle Changes to Prevent Clot Formation
- Regular Exercise: Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Healthy Diet: Eat a balanced diet rich in fruits, vegetables, and whole grains.
- Hydration: Drink plenty of fluids to stay hydrated.
- Weight Management: Maintain a healthy weight to reduce strain on your veins.
- Smoking Cessation: Smoking damages blood vessels and increases the risk of thrombosis.
- Limit Alcohol Consumption: Excessive alcohol intake can increase the risk of blood clots.
Treatment for Thrombosis and Embolism
- Anticoagulant Medications: These medications help prevent blood clots from forming and can break down existing clots. Common types include warfarin, dabigatran, rivaroxaban, and apixaban.
- Thrombolytics: In severe cases, medications like alteplase can be used to dissolve blood clots.
- Compression Stockings: These can help improve blood flow in the legs and reduce the risk of DVT.
- Catheter-Directed Interventions: In some cases, procedures using catheters can remove clots or embolus or restore blood flow.
- Surgery: In rare cases, surgery may be necessary to remove a large clot or repair damaged blood vessels.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Saba HI, Roberts HR. Hemostasis and Thrombosis: Practical Guidelines in Clinical Management (Wiley Blackwell). 2014.
- DeLoughery TG. Hemostasis and Thrombosis 4th Edition (Springer). 2019.
- Keohane EM, Otto CN, Walenga JM. Rodak’s Hematology 6th Edition (Saunders). 2019.
- Kaushansky K, Levi M. Williams Hematology Hemostasis and Thrombosis (McGraw-Hill). 2017.