TL;DR
Immunotherapy is a type of cancer treatment that uses the body’s own immune system to fight cancer cells. It aims to boost the immune system’s ability to recognize and attack cancer cells.
Mechanisms ▾
- Checkpoint Inhibitors: Drugs that release the brakes on the immune system, allowing it to attack cancer cells more effectively.
- CAR-T Cell Therapy: T cells are engineered to recognize and attack specific cancer cells.
- Cancer Vaccines: Vaccines that stimulate the immune system to produce antibodies and T cells that target cancer cells.
- Cytokine Therapy: Cytokines are signaling molecules that boost the immune response.
Advantages ▾
- Targeted Therapy: Specifically targets cancer cells, minimizing damage to healthy tissues.
- Durable Response: Can induce long-lasting responses, even after treatment completion.
- Fewer Side Effects: Often has milder side effects compared to traditional treatments.
- Combination Therapy: Can be combined with other treatments to improve outcomes.
- Personalized Medicine: Can be tailored to individual patients.
Disadvantages
- Not Effective for All Cancers: May not be effective for all types of cancer.
- Side Effects: Can cause immune-related side effects.
- High Cost: Can be expensive, especially for newer treatments.
- Resistance: Cancer cells may develop resistance to immunotherapy.
*Click ▾ for more information
Introduction
Immunotherapy is a type of cancer treatment that uses the body’s own immune system to fight cancer. The immune system is a complex network of cells and organs that work together to protect the body from infection and disease.
Immunotherapy is a promising new approach to cancer treatment because it can be more targeted and have fewer side effects than traditional treatments.
Traditional Cancer Treatments: Surgery, Chemotherapy, and Radiation Therapy
Traditional cancer treatments have been the mainstay of cancer care for many years. These treatments include surgery, chemotherapy, and radiation therapy.
- Surgery involves removing cancerous tissue from the body. It is often used to treat localized cancers. However, surgery may not be an option for all cancers, especially those that have spread to other parts of the body.
- Chemotherapy uses drugs to kill cancer cells. Chemotherapy drugs can be administered intravenously, orally, or topically. While chemotherapy can be effective in treating many types of cancer, it can also have serious side effects, such as hair loss, nausea, and fatigue.
- Radiation therapy uses high-energy rays to kill cancer cells. Radiation therapy can be used to treat both localized and metastatic cancers. Like chemotherapy, radiation therapy can also have side effects, such as skin irritation and fatigue.
Limitations of Traditional Treatments
While traditional cancer treatments have made significant progress in improving patient outcomes, they also have limitations. These limitations include:
- Lack of Specificity: Traditional treatments often damage healthy cells along with cancer cells, leading to side effects.
- Drug Resistance: Cancer cells can develop resistance to chemotherapy drugs, making treatment less effective over time.
- Limited Effectiveness: Some cancers are resistant to traditional treatments, leaving patients with few options.
How Immunotherapy Works (Principle)
Immunotherapy is a type of cancer treatment that leverages the body’s own immune system to fight cancer. The immune system is a complex network of cells and organs that work together to protect the body from infection and disease. It comprises various components, including:
- T Cells: These cells play a crucial role in cell-mediated immunity, where they directly attack infected or cancerous cells.
- B Cells: These cells produce antibodies, which bind to foreign substances and mark them for destruction by other immune cells.
- Macrophages: Macrophages ingest and degrade dead cells, debris, tumor cells and foreign materials.
How Cancer Cells Evade the Immune System
Cancer cells often develop mechanisms to evade the immune system.
- Reduced expression of tumor antigens: Cancer cells may downregulate the expression of proteins that would normally be recognized by the immune system as foreign.
- Immune suppression: Cancer cells can release substances that suppress the activity of immune cells, making them less effective in attacking the tumor.
- Hiding from immune cells: Cancer cells can hide within tissues or form protective barriers that shield them from immune attack.
Mechanism of Immunotherapy
Immunotherapy aims to overcome these evasion mechanisms and stimulate the immune system to attack cancer cells.
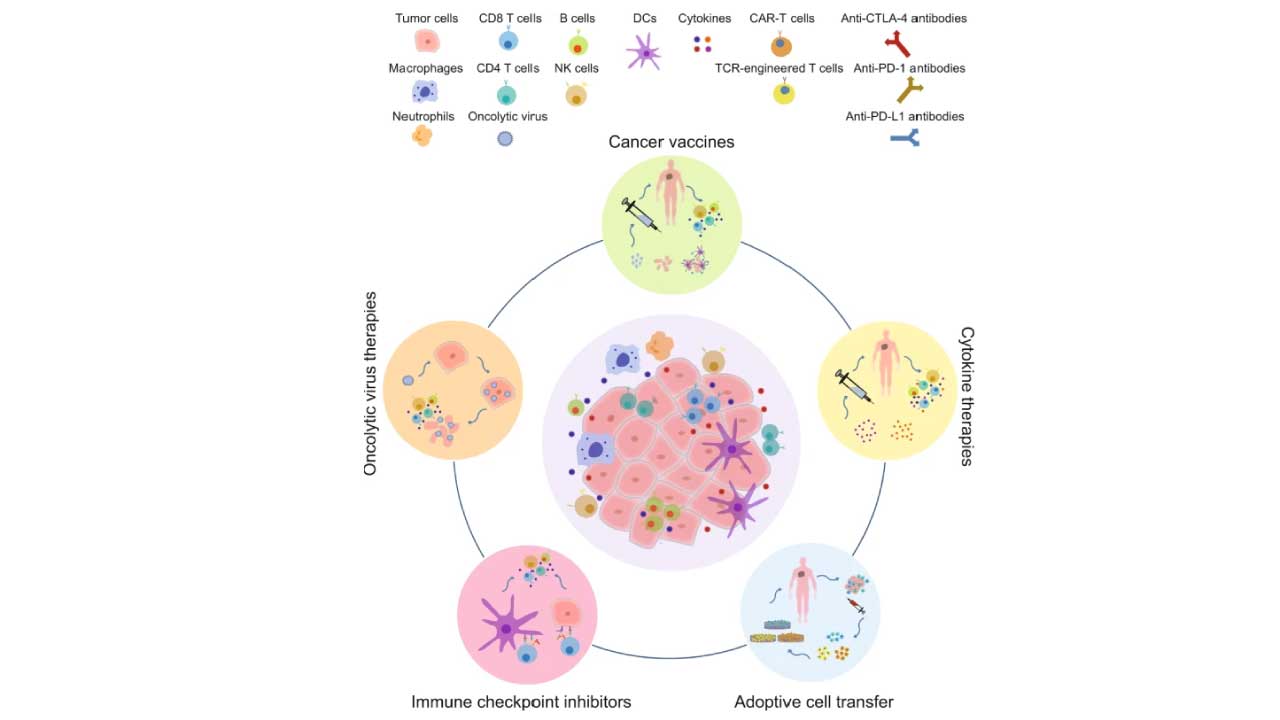
Checkpoint Inhibitors
The immune system has natural checkpoints to prevent it from attacking healthy cells. Cancer cells, however, can exploit these checkpoints to evade the immune response. Checkpoint inhibitors are drugs that target these checkpoints, releasing the “brakes” on the immune system and allowing it to attack cancer cells.
- PD-1/PD-L1 Inhibitors: PD-1 is a protein on T cells that can bind to PD-L1 on cancer cells, inhibiting the T cell’s activity. PD-1 inhibitors block this interaction, allowing T cells to attack cancer cells.
- CTLA-4 Inhibitors: CTLA-4 is another protein on T cells that can suppress their activity. CTLA-4 inhibitors block this protein, enhancing the T cell response against cancer.
CAR-T Cell Therapy
CAR-T cell therapy involves engineering a patient’s own T cells to recognize and attack cancer cells. This is done by genetically modifying T cells to express a chimeric antigen receptor (CAR), which binds to a specific antigen on cancer cells. The engineered T cells are then infused back into the patient’s body, where they can multiply and target cancer cells.
Cancer Vaccines
Cancer vaccines are designed to stimulate the immune system to recognize and attack cancer cells. They can be made from tumor cells, tumor antigens, or synthetic peptides. When administered, these vaccines trigger the immune system to produce antibodies and T cells that can target and destroy cancer cells.
Cytokine Therapy
Cytokines are signaling molecules that regulate the immune response. Cytokine therapy involves administering cytokines to boost the immune system’s ability to fight cancer. For example, interleukin-2 (IL-2) is a cytokine that can stimulate the growth and activity of T cells.
How Immunotherapy is Made
The manufacturing process for various immunotherapy treatments can vary significantly, but they generally involve complex procedures to ensure the safety and efficacy of the final product.
CAR-T Cell Therapy
CAR-T cell therapy involves a multi-step process.
- Leukapheresis: This process involves removing T cells from a patient’s blood. The patient’s blood is drawn, passed through a machine that separates out the T cells, and then returned to the patient.
- T Cell Activation and Expansion: The isolated T cells are then activated and expanded in a laboratory setting. This involves stimulating the T cells to divide and grow in large numbers.
- Genetic Engineering: The T cells are genetically modified to express a chimeric antigen receptor (CAR). This CAR is a protein that recognizes a specific antigen on cancer cells.
- Cell Expansion: The genetically modified T cells are further expanded in the laboratory to ensure a sufficient number of cells for infusion.
- Cell Infusion: The expanded CAR-T cells are infused back into the patient’s bloodstream, where they can target and kill cancer cells.
Checkpoint Inhibitors
Checkpoint inhibitors are typically monoclonal antibodies, which are proteins that can bind to specific targets. These antibodies are produced using recombinant DNA technology. The process involves:
- Gene Cloning: The gene encoding the desired antibody is cloned into a vector.
- Cell Culture: The vector is introduced into cells, which then produce the antibody.
- Antibody Purification: The antibodies are purified from the cell culture and formulated for administration.
Cancer Vaccines
Cancer vaccines can be produced using various methods, including:
- Whole-Cell Vaccines: These vaccines use whole tumor cells that have been inactivated or attenuated.
- Peptide Vaccines: These vaccines use short peptides that are derived from tumor antigens.
- DNA Vaccines: These vaccines use DNA that encodes tumor antigens.
- Viral Vector Vaccines: These vaccines use viruses to deliver tumor antigens into cells.
The manufacturing process for cancer vaccines involves:
- Antigen Preparation: The tumor antigen is isolated and purified.
- Vaccine Formulation: The antigen is formulated with an adjuvant, which helps to boost the immune response.
- Quality Control: The vaccine is tested for safety and efficacy before it is administered to patients.
Cytokines
Cytokines are proteins that regulate the immune response. They are produced using recombinant DNA technology, similar to the process used to produce monoclonal antibodies. The process involves:
- Gene Cloning: The gene encoding the desired cytokine is cloned into a vector.
- Cell Culture: The vector is introduced into cells, which then produce the cytokine.
- Cytokine Purification: The cytokine is purified from the cell culture and formulated for administration.
It’s important to note that the manufacturing process for each type of immunotherapy can vary depending on the specific product and the manufacturer. However, these general steps provide an overview of the key processes involved.
What Immunotherapy Treats
| Cancer Type | Type of Immunotherapy | Drug Name (Generic/Brand) |
| Melanoma | Checkpoint Inhibitor | Nivolumab, Pembrolizumab, Ipilimumab |
| Non-Small Cell Lung Cancer | Checkpoint Inhibitor | Nivolumab, Pembrolizumab, Atezolizumab, Durvalumab, Ipilimumab |
| Kidney Cancer | Checkpoint Inhibitor | Nivolumab, Pembrolizumab |
| Bladder Cancer | Checkpoint Inhibitor | Atezolizumab, Pembrolizumab |
| Head and Neck Cancer | Checkpoint Inhibitor | Pembrolizumab, Nivolumab |
| Liver Cancer | Checkpoint Inhibitor | Nivolumab, Pembrolizumab |
| Certain Blood Cancers (Leukemia, Lymphoma) | CAR-T Cell Therapy | Tisagenlecleucel, Axicabtagene ciloleucel |
Note: This is a simplified table and does not include all possible immunotherapy treatments for each cancer type. The specific treatment options may vary depending on the individual patient and the stage of their disease.
Comparison of Immunotherapy to Traditional Treatments
| Feature | Immunotherapy | Surgery | Chemotherapy | Radiation Therapy |
| Side Effects | Generally milder side effects, including fatigue, flu-like symptoms, and skin rashes. | Pain, bleeding, infection, and scarring at the surgical site. | Hair loss, nausea, vomiting, diarrhea, and bone marrow suppression. | Skin irritation, fatigue, and hair loss in the treatment area. |
| Effectiveness | Can be highly effective for certain types of cancer, especially those that are resistant to other treatments. | Highly effective for localized cancers, but less effective for metastatic disease. | Can be effective for many types of cancer, but can have limitations due to drug resistance. | Can be effective for both localized and metastatic cancers, but can damage healthy tissue. |
| Patient Experience | Generally well-tolerated, with fewer severe side effects than traditional treatments. | Invasive procedure with potential for pain and recovery time. | Can be physically and emotionally challenging due to side effects and treatment schedule. | Can be physically uncomfortable and may cause fatigue. |
Important Note: The specific side effects and effectiveness of each treatment can vary depending on the individual patient, the type of cancer, and the specific treatment regimen.
Managing Immunotherapy Side Effects
While immunotherapy offers promising results, it can sometimes lead to side effects. However, these side effects are often manageable with appropriate medical care.
Common Side Effects and Management Strategies
- Flu-like symptoms: These include fever, chills, fatigue, and muscle aches. Over-the-counter medications like acetaminophen or ibuprofen can help alleviate these symptoms.
- Skin rashes: Mild rashes can be treated with topical corticosteroids or antihistamines. Severe rashes may require systemic corticosteroids or other medications.
- Diarrhea: Anti-diarrheal medications, such as loperamide, can help control diarrhea. In severe cases, medications to reduce inflammation in the intestines may be necessary.
- Endocrine disorders: These can include thyroid dysfunction or adrenal insufficiency. Hormone replacement therapy may be required to manage these conditions.
- Pneumonitis: This is inflammation of the lungs. Corticosteroids are often used to treat pneumonitis.
Monitoring and Management
- Regular Check-ups: Regular doctor visits are essential to monitor for side effects and adjust treatment as needed.
- Blood Tests: Blood tests can help monitor organ function and identify potential problems early on.
- Imaging Studies: Imaging tests, such as CT scans or chest X-rays, may be used to assess organ damage.
Advantages and Disadvantages of Immunotherapy
| Feature | Advantages | Limitations |
| Specificity | Targets cancer cells specifically, minimizing damage to healthy tissues. | May not be effective for all cancer types. |
| Durability of Response | Can induce long-lasting responses, even after treatment completion. | Some cancers may develop resistance to immunotherapy over time. |
| Side Effects | Often has milder side effects compared to traditional treatments. | |
| Combination Therapy | Can be combined with other treatments, such as surgery, chemotherapy, and radiation therapy, to improve overall outcomes. | |
| Personalized Medicine | Can be tailored to individual patients based on their genetic makeup and tumor characteristics. | Requires advanced genetic testing and analysis, which may not be accessible to all patients. |
| Cost | Can be expensive, especially for newer treatments like CAR-T cell therapy. |
Frequently Asked Questions (FAQs)
At what stage of cancer is immunotherapy used?
Immunotherapy can be used at various stages of cancer. It’s increasingly being used as a first-line treatment for advanced cancers, such as metastatic melanoma and lung cancer. Additionally, it’s used to treat earlier-stage cancers, especially high-risk ones, to prevent recurrence.
Do you lose your hair with immunotherapy?
Generally, immunotherapy does not cause hair loss. Unlike chemotherapy, which often leads to hair loss, immunotherapy typically targets specific immune cells and doesn’t directly affect hair follicles.
However, in some rare cases, certain immunotherapy drugs may cause hair thinning or loss as a side effect.
What are good signs immunotherapy is working?
- Tumor Shrinkage: This is the most obvious sign of success. Regular imaging tests, such as CT scans or MRIs, can monitor tumor size and assess whether it’s shrinking or stabilizing.
- Improved Symptoms: As the tumor shrinks, symptoms related to the cancer may improve. This could include reduced pain, improved appetite, or increased energy levels.
- Increased Immune Response: Some immunotherapy treatments may cause flu-like symptoms, such as fever, fatigue, and muscle aches. While these can be unpleasant, they often indicate that the immune system is actively fighting the cancer.
- Changes in Tumor Markers: Certain blood tests, known as tumor markers, can measure levels of specific substances produced by cancer cells. A decrease in these markers may indicate that the treatment is effective.
What is the next step after immunotherapy?
The next steps after immunotherapy depend on various factors, including the type of cancer, the stage of the disease, the patient’s response to treatment, and any side effects experienced. If the immunotherapy is successful, regular monitoring, continued therapy, or surveillance may be recommended. If the immunotherapy is not successful, alternative treatments, clinical trials, or supportive care may be considered.
What is the risk of death from immunotherapy?
While immunotherapy is generally safe, there is a small risk of severe side effects, which in rare cases can be fatal. 1 These side effects are often related to the immune system being overactivated. However, the overall risk of death from immunotherapy is low, and the benefits often outweigh the risks, especially for patients with advanced cancers.
Can cancer come back after immunotherapy?
Yes, cancer can come back after immunotherapy, even if the treatment was initially successful. This can happen due to various reasons, such as the presence of resistant cancer cells that were not eliminated by the immunotherapy, or the immune system gradually losing its ability to recognize and attack the cancer cells.
Regular monitoring and follow-up care are crucial to detect any recurrence early. If the cancer does return, additional treatment options, such as surgery, chemotherapy, radiation therapy, or further immunotherapy, may be considered.
How long can you stay on immunotherapy?
The duration of immunotherapy treatment can vary depending on several factors, including the type of cancer, the stage of the disease, the specific immunotherapy drug being used, and the individual patient’s response to treatment.
Typically, many people stay on immunotherapy for up to two years. However, this duration can be shorter or longer depending on the circumstances. Some patients may continue treatment indefinitely if they experience a sustained response and have minimal side effects.
Clinical trials are ongoing to determine the optimal duration of immunotherapy for different cancers and to identify patients who may benefit from shorter treatment courses.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Zhang, Y., & Zhang, Z. (2020). The history and advances in cancer immunotherapy: understanding the characteristics of tumor-infiltrating immune cells and their therapeutic implications. Cellular & molecular immunology, 17(8), 807–821. https://doi.org/10.1038/s41423-020-0488-6
- Esfahani, K., Roudaia, L., Buhlaiga, N., Del Rincon, S. V., Papneja, N., & Miller, W. H., Jr (2020). A review of cancer immunotherapy: from the past, to the present, to the future. Current oncology (Toronto, Ont.), 27(Suppl 2), S87–S97. https://doi.org/10.3747/co.27.5223
- Reck, M., Remon, J., & Hellmann, M. D. (2022). First-Line Immunotherapy for Non-Small-Cell Lung Cancer. Journal of clinical oncology : official journal of the American Society of Clinical Oncology, 40(6), 586–597. https://doi.org/10.1200/JCO.21.01497
- Onitilo, A. A., & Wittig, J. A. (2020). Principles of Immunotherapy in Melanoma. The Surgical clinics of North America, 100(1), 161–173. https://doi.org/10.1016/j.suc.2019.09.009
- Barsan, V., Ramakrishna, S., & Davis, K. L. (2020). Immunotherapy for the Treatment of Acute Lymphoblastic Leukemia. Current oncology reports, 22(2), 11. https://doi.org/10.1007/s11912-020-0875-2
- Meng, L., Collier, K. A., Wang, P., Li, Z., Monk, P., Mortazavi, A., Hu, Z., Spakowicz, D., Zheng, L., & Yang, Y. (2023). Emerging Immunotherapy Approaches for Advanced Clear Cell Renal Cell Carcinoma. Cells, 13(1), 34. https://doi.org/10.3390/cells13010034
- Ward Grados, D. F., Ahmadi, H., Griffith, T. S., & Warlick, C. A. (2022). Immunotherapy for Bladder Cancer: Latest Advances and Ongoing Clinical Trials. Immunological investigations, 51(8), 2226–2251. https://doi.org/10.1080/08820139.2022.2118606
- Bhatia, A., & Burtness, B. (2023). Treating Head and Neck Cancer in the Age of Immunotherapy: A 2023 Update. Drugs, 83(3), 217–248. https://doi.org/10.1007/s40265-023-01835-2
- Zheng, Y., Li, Y., Feng, J., Li, J., Ji, J., Wu, L., Yu, Q., Dai, W., Wu, J., Zhou, Y., & Guo, C. (2021). Cellular based immunotherapy for primary liver cancer. Journal of experimental & clinical cancer research : CR, 40(1), 250. https://doi.org/10.1186/s13046-021-02030-5



