Introduction
The activated partial thromboplastin time (aPTT) blood test measures how long it takes for a blood clot to form. It is one of the most common blood tests performed, and it is used to diagnose and monitor a variety of bleeding and clotting disorders.
The activated partial thromboplastin time (aPTT) blood test works by measuring the amount of time it takes for fibrinogen to be converted to fibrin. Fibrinogen is a protein that is produced by the liver, and it is essential for blood clotting. Fibrin is the main component of blood clots.
The activated partial thromboplastin time (aPTT) blood test is performed by mixing a sample of the patient’s blood with a reagent that contains a phospholipid and a contact activator. The phospholipid provides a surface for the coagulation factors to assemble on, and the contact activator activates the intrinsic coagulation pathway. The intrinsic coagulation pathway is one of two pathways that lead to blood clot formation.
The time it takes for a clot to form is measured in seconds. The normal range for the activated partial thromboplastin time (aPTT) blood test is 25 to 35 seconds. A prolonged activated partial thromboplastin time (aPTT) indicates that it is taking longer for the blood to clot than normal. This can be caused by a variety of factors, including:
- Disseminated intravascular coagulopathy (DIC)
- Other bleeding disorders
- Liver disease
- Certain medications, such as heparin and warfarin
The activated partial thromboplastin time (aPTT) blood test is a valuable tool for diagnosing and monitoring bleeding and clotting disorders. It is also used to monitor the effectiveness of blood thinners, such as heparin.
Principle of Activated Partial Thromboplastin Time (aPTT) Blood Test
Activated partial thromboplastin time (aPTT) blood test measures the plasma clotting time after the activation of contact factors (prekallikrein (high molecular weight kininogen [HMWK]) > kallikrein > FXII > FXIIa) without added tissue thromboplastin, indicating the overall efficiency of the intrinsic pathway.
Activated partial thromboplastin time (aPTT) blood test is performed by pre-incubating the plasma with a contact activator i.e. kaolin or elagic acid to activate the contact factors. This will produce factor XIIa, which cleaves factor XI to factor XIa. Calcium is absent during this phase to prevent coagulation.
After adding calcium, factor XIa activates factor IX, and coagulation proceeds. Phospholipid is added to allow the test to be performed on platelet-poor plasma. The aPTT assay depends on contact factors, factors VIII and IX, and reactions with factors X, V, prothrombin, and fibrinogen. It is also sensitive to the presence of circulating anticoagulants (inhibitors) and heparin.
Method differs slightly according to the manufacturer’s protocol.
Materials
- #Platelet poor plasma (PPP) of patient and control. PPP is prepared by centrifuging the peripheral blood at 2000 g for 15 minutes at room temperature.
- *Activator-phospholipid solution
- *0.025 mol/L calcium chloride (CaCl2)
- *Glass tubes 5 ml
- *Water bath
- Stopwatch
- Timer
- Pipettes 100 – 200 ul
- Pipette tips
*These items must be at 37°C.
#PPP must be kept at room temperature to prevent activation of factor VIII which may cause an inaccurate timing result.
Protocol
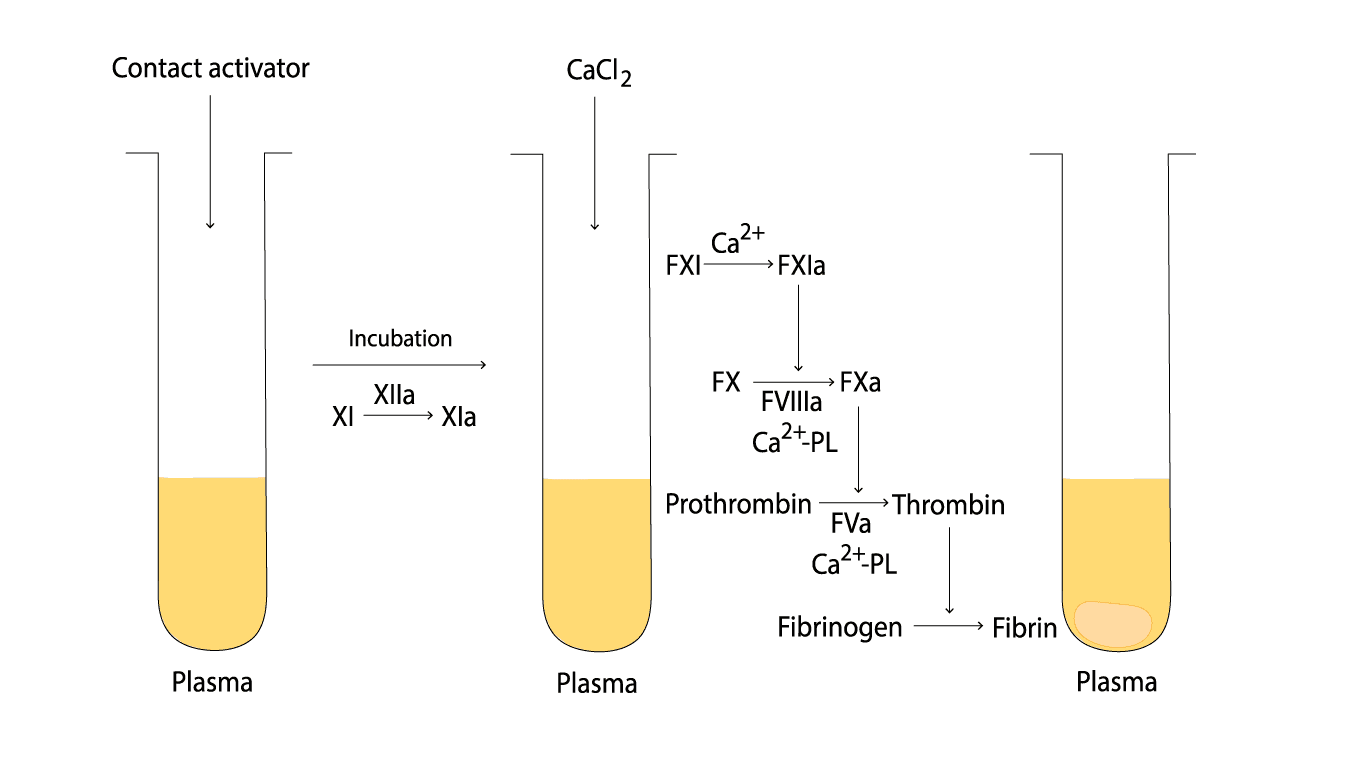
The addition of activator and phospholipid to the platelet-poor plasma initiates the intrinsic coagulation pathway. This pathway involves a series of enzymatic reactions, leading to the formation of thrombin, the enzyme responsible for converting fibrinogen to fibrin, the insoluble clot.
This test must be performed in the water bath at all times apart from the observation of the clot formation step.
- Add 0.1 mL plasma of both patient and control into a test tube, respectively and label accordingly. Have the timer set for 3 minutes.
- Add 0.2 mL of activator-phospholipid solution into each test tube and immediately start the timer.
- Incubate the tubes in the water bath for 3 minutes with occasional gentle agitation.
- Get the stopwatch ready, add 0.1 mL CaCl2 and immediately start the stopwatch.
- Gently mix the solution in the test tubes by tilting the test tubes to 45° angle and agitate lightly.
- Intermittently take the tubes out of the water bath to observe for the first sign of clot formation.
- Stop the timer and record the time at the first sign of clot formation.
- Test both patient and control plasma in duplicates and record the average time.
Interpretation
Reference range for activated partial thromboplastin time (aPTT) is 26 – 40 seconds.
Common Conditions of Prolonged aPTT
A prolonged activated partial thromboplastin time (aPTT) indicates that it is taking longer for the blood to clot than normal. This can be caused by a variety of factors, including:
Inherited Factor Deficiencies (Intrinsic Pathway)
The aPTT specifically measures the intrinsic and common pathways. Deficiencies in these factors will prolong the time it takes for a clot to form.
- Hemophilia A: Deficiency of Factor VIII.
- Hemophilia B (Christmas Disease): Deficiency of Factor IX.
- Hemophilia C: Deficiency of Factor XI (most common in Ashkenazi Jewish populations).
- Von Willebrand Disease (vWD): Since vWF acts as a carrier protein for Factor VIII, a severe deficiency in vWF can lead to secondary low levels of Factor VIII, prolonging the aPTT.
- Contact Factor Deficiencies: Deficiencies of Factor XII, Pre-kallikrein, or High Molecular Weight Kininogen (HMWK).
Acquired Inhibitors (Specific & Non-Specific)
- Lupus Anticoagulant (LA): An antiphospholipid antibody. This causes a “Biological Paradox”: it prolongs the aPTT in the test tube by interfering with reagents but is associated with a high risk of thrombosis in the patient.
- Specific Factor Inhibitors: Autoantibodies (usually IgG) against specific factors, most commonly Factor VIII (Acquired Hemophilia A). These are life-threatening and do not “correct” during a mixing study.
Pharmacological Causes (Anticoagulants)
- Unfractionated Heparin (UFH): The most common reason for a prolonged aPTT in hospitalized patients. It enhances Antithrombin III, which primarily inhibits Factors II and X (but also affects the intrinsic pathway).
- Direct Thrombin Inhibitors (DTIs): Drugs like Dabigatran, Argatroban, and Bivalirudin.
- DOACs: Direct Factor Xa inhibitors (Rivaroxaban, Apixaban) can prolong aPTT, though the effect is variable and the test is not used for monitoring.
Multiple Factor Deficiencies (Combined aPTT & PT)
If both the aPTT and PT are prolonged, the defect is likely in the Common Pathway (Factors X, V, II, I) or due to a global issue:
- Liver Disease: Reduced synthesis of nearly all clotting factors (except Factor VIII).
- Disseminated Intravascular Coagulation (DIC): Widespread activation of clotting consumes all factors and platelets.
- Vitamin K Deficiency: Affects the synthesis of Factors II, VII, IX, and X. Since IX is in the intrinsic pathway and X/II are in the common pathway, severe deficiency hits both tests.
- Warfarin (Supratherapeutic): While PT is more sensitive, very high doses of Warfarin will eventually prolong the aPTT.
Pre-Analytical Errors (The “False” Prolongation)
- Heparin Contamination: Often occurs when blood is drawn from a central line that was flushed with heparin.
- Inadequate Fill Volume: The 9:1 ratio of blood-to-citrate is crucial. If the tube is underfilled, there is excess citrate to bind the calcium in the test reagent.
- Polycythemia (Hematocrit >55%): High red cell mass means less plasma in the tube, resulting in an “over-anticoagulated” sample.
Differential Diagnosis Summary Table
| Isolated prolonged aPTT | Isolated prolonged PT | Both aPTT and PT prolonged |
| Heparin | Warfarin (early) | Liver Disease |
| Hemophilia A, B, C | Vitamin K Def (early) | DIC |
| Factor XII Deficiency | Factor VII Deficiency | Common Pathway (X, V, II, I) |
| Lupus Anticoagulant | Supratherapeutic Heparin/Warfarin |
Mixing Study
When an isolated prolongation of the aPTT is detected and pre-analytical errors have been ruled out, the clinician must determine the underlying mechanism. The primary diagnostic challenge is to distinguish between a quantitative deficiency (a lack of specific clotting factors) and the presence of a pathological inhibitor (a substance interfering with the clotting process).
This differentiation is achieved through a Mixing Study, the essential “gatekeeper” test in the coagulation lab.
How a Mixing Study Works
In this procedure, the patient’s plasma is mixed in a 1:1 ratio with “Normal Pooled Plasma” (NPP), which contains 100% of all necessary clotting factors. The aPTT is then repeated on this 50/50 mixture.
Interpreting the Results
- Correction: If the aPTT returns to the normal range, it indicates a Factor Deficiency (e.g., Hemophilia A or B). The 50% factor concentration provided by the normal plasma is sufficient to “correct” the clotting time.
- Failure to Correct: If the aPTT remains prolonged, it indicates the presence of an Inhibitor. This inhibitor is actively neutralizing the factors provided by the normal plasma. Common culprits include the Lupus Anticoagulant or specific factor antibodies (e.g., acquired Factor VIII inhibitor).
For a deep dive into the technical protocols, incubation periods, and complex inhibitor patterns, see our full guide on Manual APTT Mixing Studies.
Frequently Asked Questions (FAQs)
What is the difference between PT and aPTT?
PT (Prothrombin Time) and APTT (Activated Partial Thromboplastin Time) are both blood tests used to evaluate blood clotting ability. However, they assess different parts of the clotting process.
PT (Prothrombin Time)
- Measures the extrinsic and common pathways of the clotting cascade.
- Primarily used to monitor patients on warfarin (a blood thinner).
- Evaluates factors II, VII, and X, as well as fibrinogen.
aPTT (Activated Partial Thromboplastin Time)
- Measures the intrinsic and common pathways of the clotting cascade.
- Primarily used to monitor patients on heparin (another blood thinner).
- Evaluates factors XII, XI, IX, VIII, X, V, II, and fibrinogen.
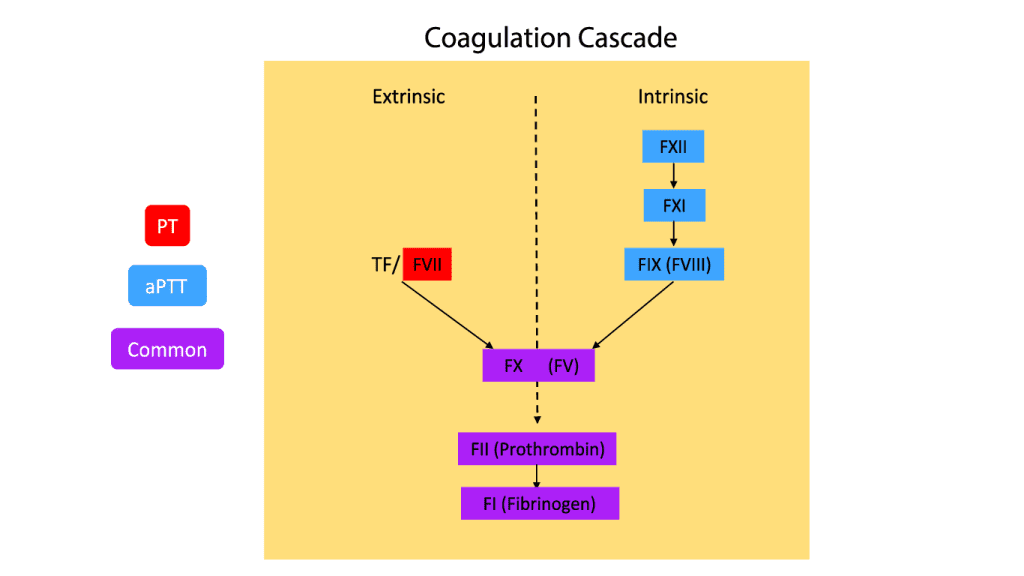
What are the coagulation factors related to aPTT?
The aPTT (Activated Partial Thromboplastin Time) test evaluates the functionality of several clotting factors involved in the intrinsic and common pathways of the coagulation cascade. These factors include:
- Factor I: Fibrinogen
- Factor II: Prothrombin
- Factor V
- Factor VIII
- Factor IX
- Factor X
- Factor XI
- Factor XII
By assessing the time it takes for blood to clot after adding specific reagents, the aPTT test helps identify deficiencies or abnormalities in these clotting factors.
What is a critical activated partial thromboplastin time (aPTT) level?
A critical activated partial thromboplastin time (aPTT) level is generally considered to be above 70 seconds. This indicates a significantly prolonged clotting time and carries a high risk of spontaneous bleeding.
It’s important to note that this is a general guideline, and specific critical values might vary slightly between laboratories.
Does activated partial thromboplastin time (aPTT) change with age?
Yes, activated partial thromboplastin time (aPTT) can change with age.
- Children: Generally have longer activated partial thromboplastin time (aPTT) values compared to adults due to lower levels of certain clotting factors.
- Adults: Activated partial thromboplastin time (aPTT) values tend to be relatively stable.
- Elderly: There’s some evidence suggesting that activated partial thromboplastin time (aPTT) might slightly increase with age, but this is less pronounced than the changes seen in children.
These are general trends and individual variations can occur. Other factors such as underlying health conditions, medications, and laboratory methods can also influence activated partial thromboplastin time (aPTT) blood test results.
Can aPTT be used to monitor Warfarin?
No. While a very high dose of Warfarin can slightly affect aPTT, the Prothrombin Time (PT/INR) is the standard and most sensitive test for monitoring Vitamin K antagonists.
Why does my aPTT remain high even after a mixing study?
If the aPTT does not “correct” after mixing the patient’s plasma with normal plasma, it suggests the presence of an inhibitor (like Lupus Anticoagulant or a specific factor antibody) rather than a simple deficiency.
What happens if the sample is contaminated with Heparin?
Heparin contamination (often from IV lines) will significantly prolong the aPTT. Labs often perform a Thrombin Time (TT) or use a heparin-neutralizing agent to confirm if the prolongation is due to heparin contamination.
Can aPTT be shortened (low)?
Yes. A shortened aPTT (e.g., <25 seconds) can occur in acute phase reactions (high Factor VIII levels), pregnancy, or certain advanced malignancies, indicating a potential hypercoagulable state.
Why is the aPTT used for Hemophilia screening?
Hemophilia A (Factor VIII) and Hemophilia B (Factor IX) are both part of the Intrinsic Pathway. Since aPTT specifically measures this pathway, it is the primary screening tool for these genetic disorders.
Glossary of Related Medical Terms
- Intrinsic Pathway: The part of the coagulation cascade involving factors XII, XI, IX, and VIII, initiated by contact with negatively charged surfaces.
- Contact Activators: Substances like Silica, Kaolin, or Ellagic Acid used in the reagent to trigger Factor XII.
- Phospholipids (Partial Thromboplastin): Reagents that provide a surface for the coagulation complexes to form, mimicking the role of platelets.
- Mixing Study: A procedure where patient plasma is mixed 1:1 with normal pooled plasma to identify the presence of inhibitors.
- Lupus Anticoagulant (LA): An antiphospholipid antibody that paradoxically prolongs the aPTT in the lab but increases clotting risk in the patient.
- Factor Inhibitor: An antibody (often IgG) that neutralizes a specific clotting factor, most commonly Factor VIII.
Disclaimer: This protocol is intended for informational purposes only and may need to be modified depending on the specific laboratory procedures and patient circumstances. Always consult with a qualified healthcare professional for guidance. See additional information.
References
- Bain BJ, Bates I, Laffan MA. Dacie and Lewis Practical Haematology: Expert Consult: Online and Print 12th Edition (Elsevier). 2016.
- Saba HI, Roberts HR. Hemostasis and Thrombosis: Practical Guidelines in Clinical Management 1st Edition (Wiley-Blackwell). 2014.
- Favaloro E. J. (2020). Coagulation mixing studies: Utility, algorithmic strategies and limitations for lupus anticoagulant testing or follow up of abnormal coagulation tests. American journal of hematology, 95(1), 117–128. https://doi.org/10.1002/ajh.25669
- Adcock, D. M., Moore, G. W., Kershaw, G. W., Montalvao, S. A. L., & Gosselin, R. C. (2024). International Council for Standardization in Haematology (ICSH) recommendations for the performance and interpretation of activated partial thromboplastin time and prothrombin time mixing tests. International journal of laboratory hematology, 46(5), 777–788. https://doi.org/10.1111/ijlh.14344



