TL;DR
Homocysteine is an amino acid, a building block of proteins, naturally produced in the body. It undergoes two main metabolic pathways: remethylation (requiring folate, vitamin B12, or betaine) and transsulfuration (requiring vitamin B6).
Biomarker for Cardiovascular Risk ▾: Elevated homocysteine is a risk factor for CVD, but not the sole predictor. It’s most useful when considered with other risk factors.
Causes of Hyperhomocysteinemia ▾: Elevated homocysteine levels can result from genetic factors, nutritional deficiencies (folate, vitamin B6, B12), lifestyle factors (smoking, alcohol), kidney disease, hypothyroidism, and certain medications.
Symptoms of Hyperhomocysteinemia▾: Often asymptomatic, but potential symptoms include weakness, fatigue, and neurological problems (though these are usually due to underlying conditions).
Diagnosis of Hyperhomocysteinemia ▾: Diagnosed through a blood test measuring homocysteine levels. Generally accepted normal range is less than 15 µmol/L
Treatment of Hyperhomocysteinemia ▾: Focuses on addressing underlying causes: vitamin supplementation, dietary adjustments, lifestyle modifications, and managing underlying conditions.
Complications of Hyperhomocysteinemia ▾: Increased risk of cardiovascular disease (heart attack, stroke), osteoporosis, potential neurological problems, and pregnancy complications.
*Click ▾ for more information
Introduction
Homocysteine is an amino acid, which is a building block of proteins. It’s naturally produced in the body during the breakdown of another amino acid called methionine. High homocysteine levels, a condition known as hyperhomocysteinemia, are associated with an increased risk of various health problems, particularly cardiovascular disease. This makes homocysteine an important biomarker, meaning it can help indicate an increased risk of certain health conditions.
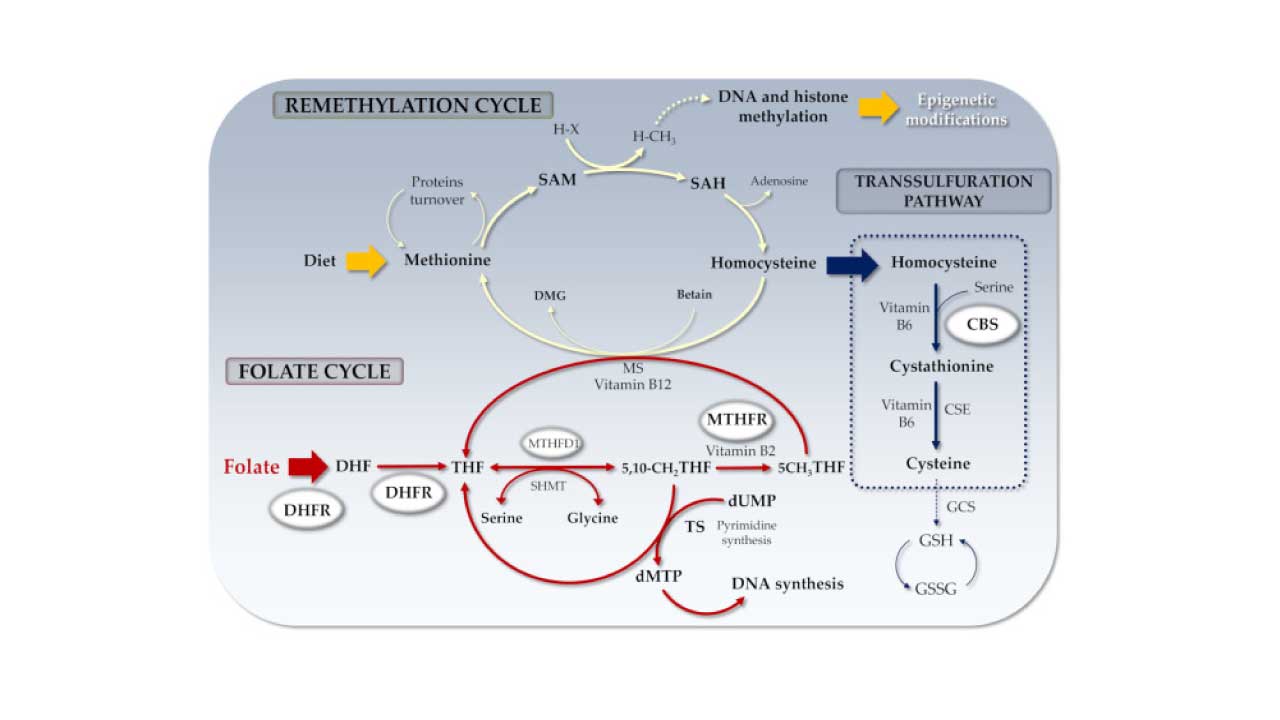
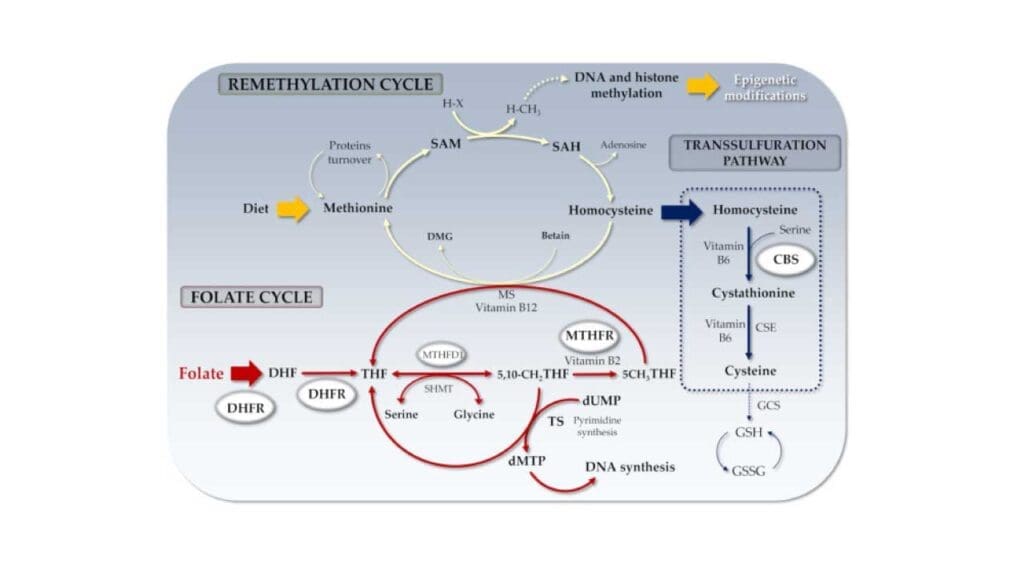
Homocysteine, a sulfur amino acid, is metabolized through two distinct pathways. In remethylation, it is converted back to methionine, a process dependent on folate, vitamin B12, or betaine. Alternatively, in transsulfuration, it is converted to cystathionine, a reaction requiring vitamin B6.
Homocysteine itself doesn’t have a known physiological function. Its significance lies in its role as an intermediate in the metabolism of other essential compounds. Elevated levels of homocysteine are primarily a risk factor for various health problems, particularly cardiovascular disease, rather than a direct cause of disease.
Homocysteine as a Biomarker for Cardiovascular Risk
Elevated homocysteine levels are considered an independent risk factor for cardiovascular disease (CVD), including heart attack, stroke, and peripheral artery disease. Studies have shown a correlation between higher homocysteine levels (hyperhomocysteinemia) and an increased risk of CVD events. Homocysteine testing, in conjunction with other risk factors (age, family history, smoking, blood pressure, cholesterol), can help assess an individual’s overall cardiovascular risk.
Limitations of Homocysteine as a Sole Predictor
While elevated homocysteine levels indicate an increased risk, the absolute risk increase may be relatively small for most individuals. It’s important to remember that elevated homocysteine is a risk factor, not a direct cause of CVD. Other factors, such as high blood pressure, high cholesterol, and smoking, play a more significant role in the development of CVD.
Homocysteine testing alone has limited predictive power for individual risk assessment. It’s most useful when considered in conjunction with other established risk factors. Elevated homocysteine levels can be influenced by various factors, including nutritional deficiencies, kidney disease, and certain medications. These confounding factors can complicate the interpretation of homocysteine levels as a predictor of CVD risk.
While studies have shown a correlation between elevated homocysteine and CVD risk, clinical trials investigating the benefits of homocysteine-lowering therapy in reducing CVD events have yielded mixed results.
Causes & Risk Factors of High Homocysteine Levels (Hyperhomocysteinemia)
High homocysteine levels can result from a combination of genetic, nutritional, and lifestyle factors:
Genetic Factors
- Methylenetetrahydrofolate reductase (MTHFR) enzyme: This enzyme is crucial for the remethylation of homocysteine back into methionine. Mutations in the MTHFR gene can reduce the enzyme’s activity, leading to decreased conversion of homocysteine and subsequent elevation of homocysteine levels.
- Cystathionine β-synthase (CBS) enzyme: This enzyme is involved in the transsulfuration pathway, converting homocysteine into cystathionine. Mutations in the CBS gene can significantly impair this pathway, leading to a dramatic increase in homocysteine levels. This condition is known as homocystinuria.
Nutritional Deficiencies
- Folate Deficiency: Folate is a B vitamin crucial for the remethylation of homocysteine. Insufficient folate intake or impaired folate absorption can lead to homocysteine buildup.
- Vitamin B6 Deficiency: Vitamin B6 is essential for the transsulfuration pathway of homocysteine metabolism. A deficiency can disrupt this pathway and contribute to elevated homocysteine levels.
- Vitamin B12 Deficiency: Vitamin B12 is also involved in the remethylation of homocysteine. Deficiency can impair this process and lead to increased homocysteine levels.
Lifestyle Factors
- Smoking: Smoking can increase homocysteine levels through various mechanisms, including oxidative stress and reduced vitamin B6 absorption.
- Excessive Alcohol Consumption: Heavy alcohol use can interfere with vitamin B6 metabolism and contribute to folate deficiency, both of which can elevate homocysteine levels.
- Kidney Disease: Kidney disease can impair the excretion of homocysteine, leading to its accumulation in the blood.
- Hypothyroidism: An underactive thyroid gland can affect homocysteine metabolism and contribute to elevated levels.
Medications
- Certain Medications: Some medications, such as methotrexate and anticonvulsants, can interfere with folate metabolism and increase homocysteine levels.
Symptoms of High Homocysteine Levels (Hyperhomocysteinemia)
High homocysteine levels (hyperhomocysteinemia) themselves often do not cause any noticeable symptoms. However, when high homocysteine levels (hyperhomocysteinemia) is severe or due to an underlying condition, some potential symptoms may include:
- General Weakness
- Fatigue
- Neurological Problems: These can vary and may include:
- Numbness or tingling: In the hands, feet, or other extremities.
- Cognitive difficulties: Such as memory problems or difficulty concentrating.
- Mood changes: Including depression or anxiety.
Laboratory Diagnosis of High Homocysteine Levels (Hyperhomocysteinemia)
Hyperhomocysteinemia is diagnosed through a simple homocysteine blood test.
The generally accepted normal range for total homocysteine levels in adults is less than 15 micromoles per liter (µmol/L).
- Moderate levels: 15-30 µmol/L
- Intermediate levels: 30-100 µmol/L
- Severe levels: Over 100 µmol/L
Treatment of High Homocysteine Levels (Hyperhomocysteinemia)
The treatment of high homocysteine levels (hyperhomocysteinemia) focuses on addressing the underlying causes.
Nutritional Approaches
- Vitamin Supplementation
- Folate: Often the first-line treatment. Folic acid supplements can significantly lower homocysteine levels.
- Vitamin B6 and B12: These vitamins also play crucial roles in homocysteine metabolism and are often supplemented alongside folate.
- Dietary Adjustments:
- Increase Folate Intake: Consume foods rich in folate, such as leafy green vegetables, citrus fruits, legumes, and fortified grains.
- Limit Alcohol Intake: Excessive alcohol consumption can interfere with vitamin B6 metabolism and contribute to folate deficiency.
Lifestyle Modifications
- Quit Smoking: Smoking can increase homocysteine levels and is a major risk factor for cardiovascular disease.
- Regular Exercise: Physical activity can improve overall cardiovascular health and may also help lower homocysteine levels.
- Maintain a Healthy Weight: Obesity can increase the risk of various health problems, including cardiovascular disease.
Addressing Underlying Conditions
- Treat Hypothyroidism: If an underactive thyroid is contributing to high homocysteine levels, treatment with thyroid hormone replacement therapy is essential.
- Manage Kidney Disease: If kidney disease is a factor, appropriate medical management of the kidney condition may help lower homocysteine levels.
Complications of High Homocysteine Levels (Hyperhomocysteinemia)
High homocysteine levels (hyperhomocysteinemia), if not addressed, can increase the risk of several health complications.
Cardiovascular Disease
- Atherosclerosis: Elevated homocysteine can contribute to the development of atherosclerosis, a condition where fatty substances build up within the artery walls, narrowing the blood vessels.
- Heart Attack: Atherosclerosis can lead to a heart attack by blocking blood flow to the heart muscle.
- Stroke: Atherosclerosis in the brain’s blood vessels can cause a stroke by disrupting blood flow to the brain.
- Peripheral Artery Disease: Atherosclerosis in the arteries of the legs and arms can restrict blood flow, leading to pain and discomfort, especially during exercise.
Pregnancy Complications
In pregnant women, high homocysteine levels may be associated with an increased risk of preeclampsia (a pregnancy complication characterized by high blood pressure and organ damage), miscarriage, and premature birth.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Hermann A, Sitdikova G. Homocysteine: Biochemistry, Molecular Biology and Role in Disease. Biomolecules. 2021 May 15;11(5):737. doi: 10.3390/biom11050737. PMID: 34063494; PMCID: PMC8156138.
- Finkelstein JD, Martin JJ. Homocysteine. Int J Biochem Cell Biol. 2000 Apr;32(4):385-9. doi: 10.1016/s1357-2725(99)00138-7. PMID: 10762063.
- Wijekoon EP, Brosnan ME, Brosnan JT. Homocysteine metabolism in diabetes. Biochem Soc Trans. 2007 Nov;35(Pt 5):1175-9. doi: 10.1042/BST0351175. PMID: 17956306.
- Bleich S, Hillemacher T. Homocysteine, alcoholism and its molecular networks. Pharmacopsychiatry. 2009 May;42 Suppl 1:S102-9. doi: 10.1055/s-0029-1214396. Epub 2009 May 11. PMID: 19434547.
- Temple ME, Luzier AB, Kazierad DJ. Homocysteine as a risk factor for atherosclerosis. Ann Pharmacother. 2000 Jan;34(1):57-65. doi: 10.1345/aph.18457. PMID: 10669187.
- Ferechide D, Radulescu D. Hyperhomocysteinemia in renal diseases. J Med Life. 2009 Jan-Mar;2(1):53-9. PMID: 20108491; PMCID: PMC5051482.